There are currently two scheduled course offerings available for Modalities and Pelvic Function: Philadelphia PA in April 6-7 and Manchester NH in August 24-25. If neither of these work for your location or schedule then consider hosting! The hosting requirements and interest form can be found on the Host a Course page.
The new Modalities and Pelvic Function - Pelvic Health Clinical Toolkit is an in-person two-day continuing education course targeted to pelvic health clinicians covering frequently used modalities in pelvic health, including biofeedback and EStim. This course was designed to answer the clinician’s need to understand how to choose and access the right tools, both for in-clinic care and for patient self-care application.
One of the course co-creators, Mora Pluchino shared “This class will be unlike one you've taken before. The H&W curriculum team sat down and thought about how we could make this the most interactive, hands-on, and practical course while still staying evidence-based and professional. This will be an in-person learning opportunity with 2 days of lab, demonstration, and interactive learning opportunities. If there is a modality that exists in pelvic health, it will likely have a debut here. This class is made for anyone who wants to learn to apply modalities in the variety of uses possible for pelvic health!"
Biofeedback and electrical stimulation are covered in this course, as are introductions to understanding tools such as shockwave, dry needling, real-time ultrasound, laser, and electrotherapies. With hands-on lab time and learning modules grouped into tools specific to pelvic health conditions such as bowel dysfunction and sexual health challenges, practitioners will have the opportunity to trial various tools and applications that previously may have only been available as an image in a presentation.
When our popular Pelvic Function Level 1 course, which introduces participants to the world of pelvic health, was transitioned to a satellite lab course one of the content pieces that was left out was the modalities focus - simply because the equipment was too difficult to ship to multiple satellite locations around the country. Herman & Wallace is thrilled to announce that not only have we solved this issue, but designed a way for clinicians to learn about dozens of modalities in an environment that allows the clinician to move beyond theoretical and soundly into the practical delivery of a variety of technologies and tools.
Current Medical Technologies will be in-person with us as we design this learning experience and will be available to answer your questions about products and clinical set-up. The interactive environment has been designed to be stimulating and allow the clinician to apply a variety of learning strategies including tactile opportunities to try things on themselves or a lab partner. This is a unique course that provides a foundational understanding of technology and tools, clinical practice research, and recommendations in an in-person environment. Many equipment providers have been generous in providing sample products for trial and even some giveaways to take home!
We believe this Modalities course is so foundational to our skillset in pelvic health that we have added it to our core Pelvic Function Series. This course is intended to be taken after Pelvic Function Level 1 and can be taken at any point following the introductory course as you work your way through the PF Series. If you’re wondering “When should I take this course?” the answer is “as soon as you can!”
This article is contributed by faculty members Tiffany Lee and Jane Kaufman. Their course, Biofeedback for Pelvic Floor Muscle Dysfunction, is scheduled for December 4-5, 2021 provides a safe space for clinicians to learn and practice this valuable tool.
Rarely do practitioners see a topic so argued in pelvic rehabilitation as the use of surface EMG biofeedback. There are practitioners who boldly state they are for or against it on their social media accounts and clinic pages. Therapists are not questioning the use of biofeedback with neurologic or orthopedic applications, so why is it such a polarizing topic in pelvic health? The Pelvic Rehab Report sits down with faculty members Tiffany Lee and Jane Kaufman to discuss the tool they love. This month they published a Special Issue article in the Biofeedback Journal for the Association for Applied Psychophysiology and Biofeedback. These two instructors have over 50 years of combined experience using biofeedback.(*)
Biofeedback provides visual and auditory feedback of muscle activity and is a non-invasive technique that allows patients to adjust muscle function, strength, and behaviors to improve pelvic floor function. The small electrical signal (EMG) provides information about an unconscious process and is presented visually on a computer screen, giving the patient immediate knowledge of muscle function, enabling the patient to learn how to alter the physiological process through verbal and visual cues. Jane Kaufman explains that "many patients gain knowledge and awareness of the pelvic floor muscle through tactile feedback, but the visual representation is what helps patients to hone in on body awareness and connect all the dots." Muscle evaluation through digital exam offers strength but does not appropriately address electrical activity such as resting tone, ability to recruit or release tone in the muscle. The use of biofeedback addresses the specificity of muscle contraction and release offering an additional view of muscle function.
In a 2020 research study by Pilkar et al, clinicians reported sEMG barriers of use which included limited time and resources, clinically inapplicable sEMG system features, and the majority of clinicians' lack of training and/or confidence in utilization of sEMG technology. This research also noted technical challenges including the limited transfer of ever-evolving sEMG research into the off-the-shelf EMG systems, nonuser-friendly intuitive interfaces, and the need for a multidisciplinary approach for accurate handling and interpretation of data. (1)
To break this down into layman terms, one contraindication may be the price of a biofeedback unit. Tiffany Lee recommends using a 2-channel sEMG biofeedback hand-held unit with the software on a laptop or computer. In fact, to become board certified in pelvic floor biofeedback, the Biofeedback Certification International Alliance (BCIA) requires that you have a 2 channel EMG system with software. If you are using a hand-held one channel unit, the patient will have a difficult time seeing the muscle activity and the coordination between the abdominals and pelvic floor. This prevents meaningful treatment with this treatment tool as the patient cannot understand or interpret the LED bars on the machine (and often the therapist cannot understand either). In truth, the benefits outweigh the cost of the equipment and within a few treatments, you can cover the cost of the unit with the appropriate software to offer the proper visualization of muscle function.
Training is another issue, to start utilizing biofeedback in your clinical setting you need to have proper training in the modality. Most therapists have never been properly trained and if they take a course where the instructor doesn’t believe in the benefits of biofeedback, they feel negatively toward a tool they have never personally explored. Biofeedback relies on a skilled clinician to interact with the patient, give verbal cues, ensure that the proper muscles are contracting and relaxing, and must be used in conjunction with their other skills and knowledge.
Think of sEMG biofeedback as a tool in your toolbox. Tiffany shares, "in a study by Aysun Ozlu MD, et al., the authors conclude that biofeedback-assisted pelvic floor muscle training, in addition to a home exercise program, improves stress urinary incontinence rates more than home exercise program alone." She continues, "Biofeedback is a powerful tool that can benefit your patient population and add to your skill-set."(2)
Essentially, the acceptance of sEMG biofeedback in rehabilitation requires a unit (with software and sensors), training, and a multidisciplinary approach. Used correctly, it can positively impact patient performance and care in the clinic. Keep in mind sEMG is a non-invasive technique. It has already shown great promise in the field of neuro-rehabilitation and has been a widely-utilized tool to assess neuromuscular outcomes in research. Jane Kaufman concludes that "In short, biofeedback treatment/training using the proper instrumentation provides the precise information necessary to change behaviors." This gives the patient the opportunity to recognize that ‘yes, they are in charge of this muscle and that they can achieve success in overpowering the symptoms.’ Biofeedback routinely allows the patient to understand that they are empowered to heal themselves with the tools you offer. They are in charge of their bodies and the outcome of treatment.
There is a long history of scientific evidence to support the use of sEMG biofeedback in the management of incontinence symptoms or pain symptoms. As a non-invasive, cost-effective, and powerful treatment modality, healthcare providers should consider this treatment tool when managing patients with pelvic floor dysfunction. Providers should be educated in the proper use of this valuable modality to gain the most out of the skills and knowledge that can be achieved through this intervention. For more information regarding courses and certification please visit www.BCIA.org.
Tiffany asked several PTs and OTs that have been to the board certification courses what they love about biofeedback. Here are a few answers:
- “Biofeedback empowers my patients and gives them the confidence that they are actually doing their exercises and/or relaxing correctly! I’ve had nothing but positive feedback from patients and it’s such a great tool to have as a pelvic floor therapist.”
- “My patients really love it, and they ask for it. I especially see the value for dyssynergia work on bearing down and learning eccentric abdominals and relaxed pelvic floor muscles. For men, I work on relaxing in standing and postures if they can’t empty their bladder. Ultimately the treatment needs to be meaningful to the patient. Biofeedback can complement other treatments. Their needs come before ours.”
- “After ONE session with a 5-year-old with constipation, mom called me in sheer excitement, screaming over the phone that he pooped on the potty!!! Something he has NEVER done before. Biofeedback helped him find and coordinate the potty muscles and tummy muscles and this made a huge difference for him!”
- “Becoming certified in biofeedback has only been positive for me. My patients feel that the initial sEMG evaluation sets the stage for my plan of care, and my reassessment at discharge is a tangible reflection of their progress. Not to mention its strength as a marketing tool.”
The Satellite Lab Course, Biofeedback for Pelvic Floor Muscle Dysfunction, scheduled for December 4-5, 2021 provides a safe space for clinicians to learn and practice this valuable tool. Registrants will gain knowledge about the benefits of using this modality in their clinical practice. Participants will learn how to administer biofeedback assessments, analyze and interpret sEMG signals, conduct treatment sessions, and role-playing patient instruction/education for each diagnosis presented during the many hands-on lab experiences.
Special Issue article in the Biofeedback Journal for the Association for Applied Psychophysiology and Biofeedback
- * Pelvic Floor Biofeedback for the Treatment of Urinary Incontinence and Fecal Incontinence. Jane Kaufman, PT, MEd BDB-PMD; Kathryn Stanton, PT, DPT; Tiffany Ellsworth Lee, MA, OTR BCB-PMD, PRPC. Biofeedback (2021) 49 (3): 71–76. https://doi.org/10.5298/1081-5937-49.3.01.
References:
- Use of Surface EMG in Clinical Rehabilitation of Individuals With SCI: Barriers and Future Considerations. Rakesh Pilkar, Kamyar Momeni, Arvind Ramanujam, Manikandan Ravi, Erica Garbarini, Gail F. Forrest. Front Neurol. 2020; 11: 578559. Published online 2020 Dec 18. doi: 10.3389/fneur.2020.578559 PMCID: PMC7780850
- Comparison of the efficacy of perineal and intravaginal biofeedback assisted pelvic floor muscle exercises in women with urodynamic stress urinary incontinence. Aysun Ozlu MD, Neemettin Yildiz MD, Ozer Oztekin MD. Neurourol Urodyn. 2017 Nov;36(8):2132-2141. Epub 2017 Mar 27. doi: 10.1002/nau.23257 PMID: 28345778.
- The basics of surface electromyography. R. Cram, G. S. Kasman. In E. Criswell (Ed.). Cram’s introduction to surface electromyography (2nd ed., pp. 3–7.) Jones and Bartlett. 2011
Using sEMG biofeedback to get real-time results
Tiffany Lee, MA, OTR, BCB-PMD and Jane Kaufman, PT, BCB-PMD are internationally board-certified clinicians in the treatment of pelvic floor muscle dysfunction through the Biofeedback Certification International Alliance. Combined, they have over fifty years of treatment experience using sEMG biofeedback. Their new course, “Biofeedback for Pelvic Floor Muscle Dysfunction”, will provide the nuts and bolts of this powerful tool so that clinicians can return to the clinic after this course with another component to their toolbox of treatment strategies.
 As a clinician treating patients with pelvic floor muscle dysfunction, have you gone away from a treatment session and asked yourself ‘what else can I do for this patient?’. Have you considered adding surface EMG, often referred to as biofeedback, to your treatment plan, but aren’t sure how to go about it correctly or effectively? Perhaps you think you can’t use the sensor because the patient has pain. Maybe you think biofeedback only helps with up-training or strengthening.
As a clinician treating patients with pelvic floor muscle dysfunction, have you gone away from a treatment session and asked yourself ‘what else can I do for this patient?’. Have you considered adding surface EMG, often referred to as biofeedback, to your treatment plan, but aren’t sure how to go about it correctly or effectively? Perhaps you think you can’t use the sensor because the patient has pain. Maybe you think biofeedback only helps with up-training or strengthening.
So exactly what is biofeedback? Why should I consider this modality? Biofeedback provides a non-invasive opportunity for patients to see muscle function visualized on a computer screen in a way that allows for immediate feedback, simple representation of muscle function, and allows the patient and the clinician the opportunity to alter the physiological process of the muscle through basic learning strategies and skilled cues. Many patients gain knowledge and awareness of the pelvic floor muscle through tactile feedback, but the visual representation is what helps patients really hone in on body awareness and connect all the dots. Here are a few comments that our patients have made; “I can now pay attention to my muscle while at work thanks to the visual of my muscle when sitting and standing”; “I needed to see my muscle to fully understand how to release the tension in it “; “I totally get what I need to do now that I have a clear picture of what you want”; “Seeing is believing”.
A 2017 study by Moretti, E., et al. is a great article that helps support the concept that measuring the pelvic floor electrical activity through a standard vaginal sensor is not always an option. For many patients, use of surface electrodes with peri-anal electrodes will provide the same reading and offer a more comfortable alternative for those patients who cannot use an internal sensor. This allows the clinician more opportunities to use this treatment modality with ease and assurance that the patient can learn from the visual representation of the muscle without fear of penetration from a sensor, and get great results!
In another study by Aysun Ozlu MD, et al. the authors conclude that biofeedback assisted pelvic floor muscle training, in addition to a home exercise program, improves stress urinary incontinence rates more than home exercise program alone.
Herman & Wallace is offering a course for clinicians in Alexandria, Virginia this June that will answer all of your questions and concerns about this fabulous treatment tool: biofeedback! This course enables the clinician to learn and practice this valuable tool and gain knowledge about the benefits of this modality, so that treatment can begin immediately with ample opportunity for patient’s positive feedback and awareness of muscle function. Participants will experience being a biofeedback practitioner and patient (using a self-inserted vaginal or rectal sensor). Participants will be administering biofeedback assessments, analyzing and interpreting sEMG signals, conducting treatment sessions, and role-playing patient instruction/education for each diagnosis presented during the many hands-on lab experiences. Biofeedback is a powerful tool that can benefit your patient population, and add to your skill-set.
Moretti, E., Galvao de moura Filho, A., Correia de Almedia, J., Araaujo, C., Lemos, C. “Electromyographic assessment of women’s pelvic floor: What is the best place for a superficial sensor?” Neurology and Urodynamics; 2017; 9999:1-7.;
Aysun Ozlu MD, Neemettin Yildiz MD, Ozer Oztekin MD, “Comparison of the efficacy of perineal and intravaginal biofeedback assisted pelvic floor muscle exercises in women with urodynamic stress urinary incontinence”
Influencing pelvic floor EMG activity through hip joint mobilization and positioning
EMG is a helpful tool to observe pelvic floor muscle activity and how it is influenced by everything from regional musculoskeletal factors and mucosal health, to client motor control, awareness, and comfort.
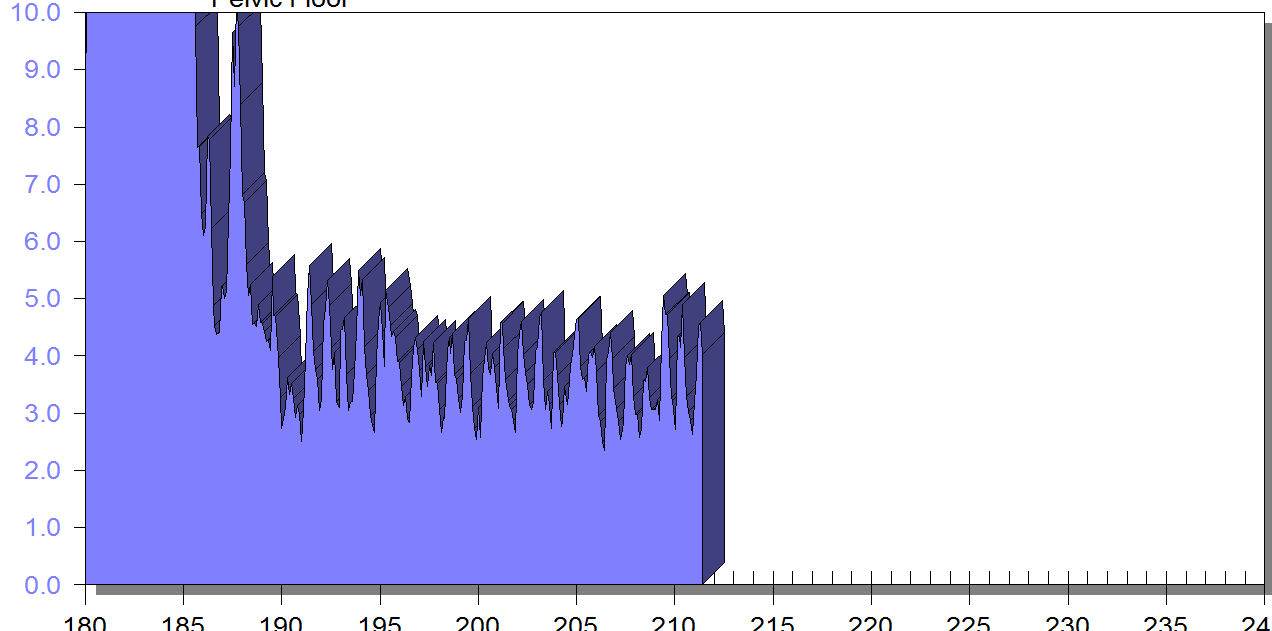
In this post I will discuss the case of one client who was referred for dyspareunia treatment, and whose SEMG findings are outlined in Figures 1-3. She had validated test item clusters for right hip labral tear as well as femoral acetabular impingement, in addition to right sided pelvic floor muscle overactivity and sensitivity with less than 3 ounces of palpation pressure.
The figures below demonstrate peri-anal SEMG response of pelvic floor muscles within a single treatment session, which included sacral unloading in supine as well as hip joint mobilization to demonstrate the relationship between her pelvic floor and her hips. Our focus for this SEMG downtraining treatment was to enable her to understand the connection between her pelvic floor muscle holding patterns and her body’s preferences to remain out of ranges of motion that impinged and irritated her hip.
By creating a clear understanding of how the client could 'listen" to her muscle activity via SEMG (as well as her kinesthetic awareness of her own comfort), she began to understand the difference between body and hip position, her pelvic floor muscle activity, and her pain during intercourse.
Pelvic floor motor control with normalized respiration, orthopedic considerations of sexual activity, and other physical therapy as well as multidisciplinary treatments were integrated into her ability to resume intercourse. The lens of SEMG, however, was a powerful tool to help her make the connection between her hip and its influence on her pelvic floor overactivity and symptoms.
Musculoskeletal co-morbidities in pelvic pain are common, requiring the clinician to have a set of test item clusters to scan and clear key structures, as well as the ability to convey this information without creating distress to the client when positive findings are discovered. For example, labral tears and subchondral cysts are common findings in asymptomatic clients and physical therapy plays a key role in reducing client fear, avoiding symptom provocation, reducing regional muscle overactivity, as well as facilitating movement and strengthening in painfree ROM.
Although this case example describes intraarticular hip dysfunction as a driver of this clients PFM overactivity, Finding the Driver in Pelvic Pain is a course that is designed to cover comprehensive key test item clusters for a fundamental pelvic pain scan exam of intrapelvic as well as extrapelvic drivers, to ensure the clinician understands the contributing factors that can influence or be influenced by the pelvic floor. This course is best suited for physical therapists and physical therapist assistants who are looking to create an organized approach to their scan exam for pelvic pain. For non-physical therapists, this can be a powerful introduction to the skill set and vocabulary needed to create a multidisciplinary team with a PT in the treatment of these clients.
FIGURE 1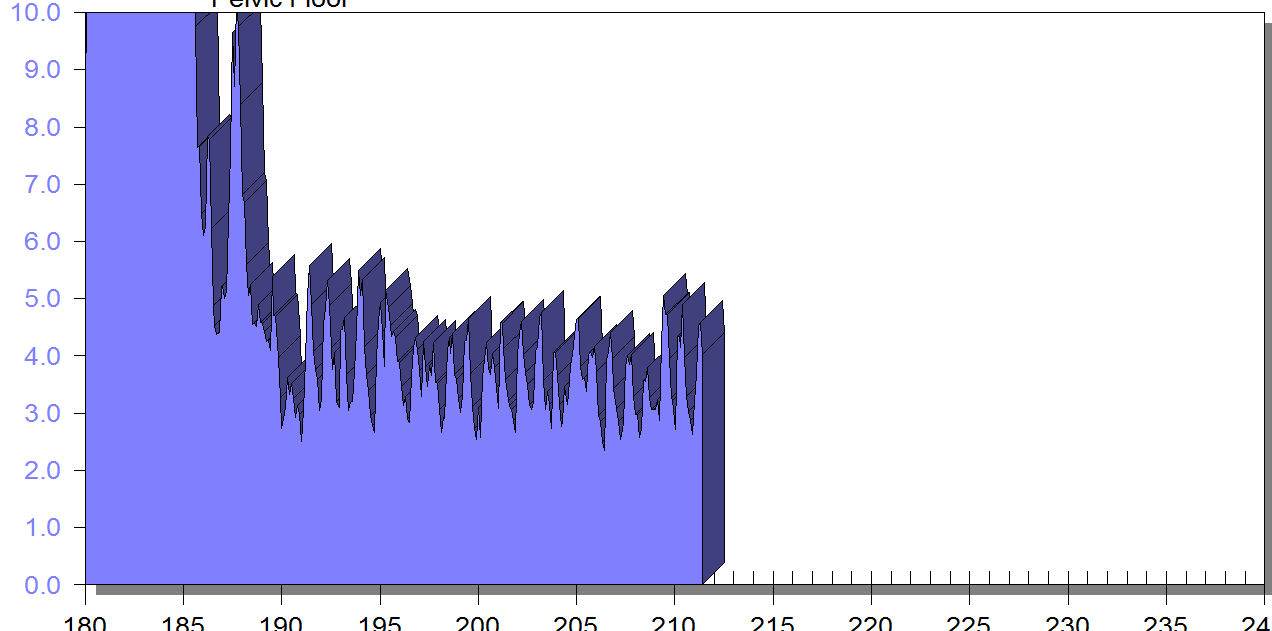
PFM EMG at rest in supine, knees bent, feet on table (peri-anal SEMG electrode placement)
FIGURE 2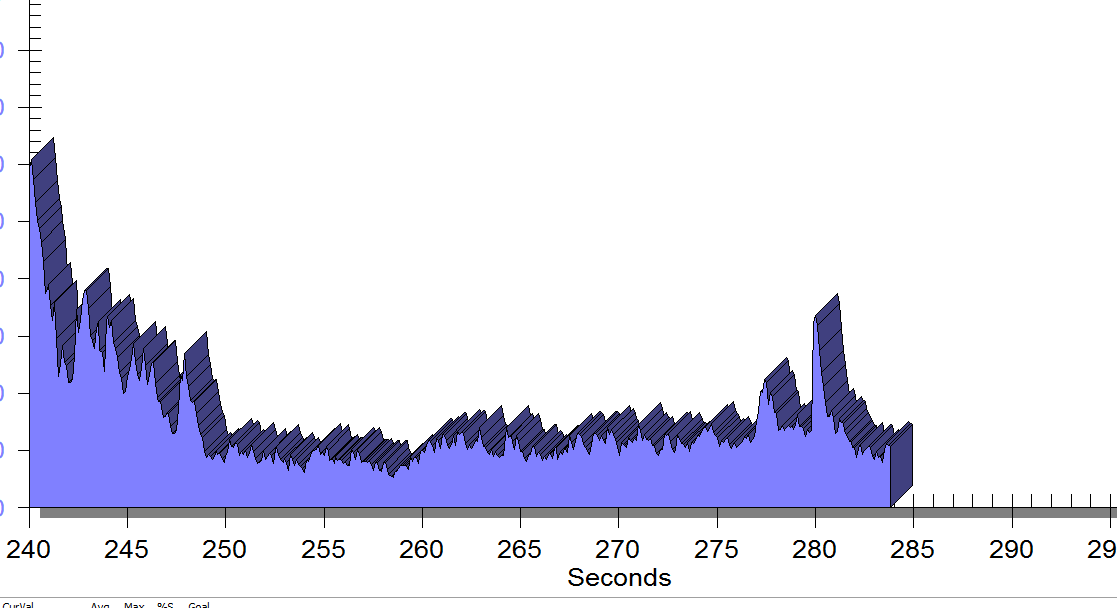
Same position, only with sacral unweighting by placing folded towels on either side of sacrum, unweighting all pressure from sacrum. Immediate report of increased comfort in buttocks, hips and pelvis.
Figure 3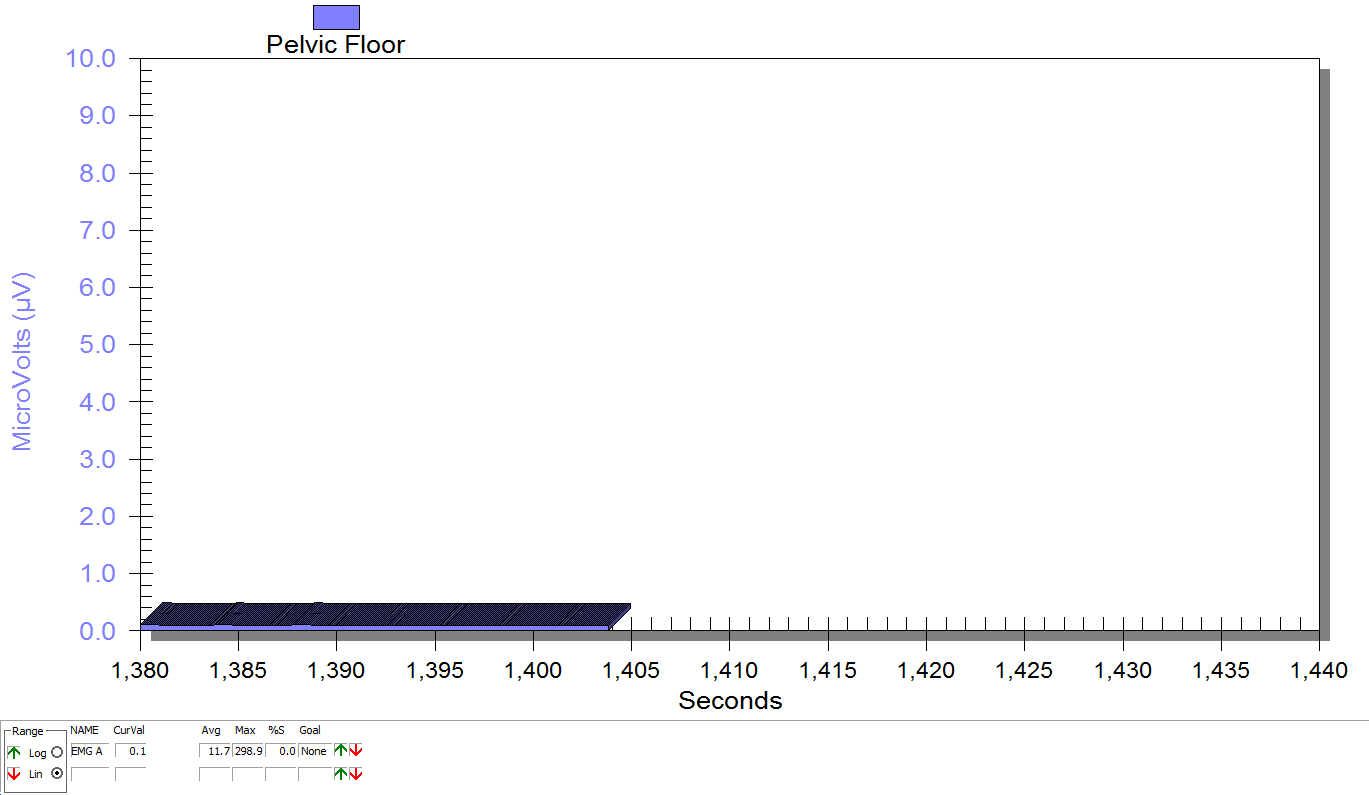
Supine, sacrum unweighted as in figure 2, after multidirecitonal hip joint mobilizaiton.
Groh, Herrera. A comprehensive review of hip labral tears. Curr Rev Musculoskelet Med. 2009 Jun; 2(2): 105–117. Published online 2009 Apr 7. doi: 10.1007/s12178-009-9052-9
Yosef, et al. Multifactorial contributors to the severity of chronic pelvic pain in women. Am J Obstet Gynecol. 2016 Dec;215(6):760.e1-760.e14. doi: 10.1016/j.ajog.2016.07.023. Epub 2016 Jul 18.
At the peak of my racing career I won awards in all my races from 5k to marathon. While warming up I would scope out my competition, intimidated by muscular females wearing outfits to accentuate their physiques. Many times, appearance out-weighed running capacity. In a similar manner, one strong pelvic floor contraction produced by a female athlete does not always mean she has the endurance to stay dry in the long run.
 Brennand et al. (2017) researched urinary leakage during exercise in Canadian women. A summary of their findings concluded that skipping, trampoline, jumping jacks, and running/jogging were most likely to cause leakage. To combat the problem, 93.2% emptied their bladder just before exercise, 62.7% required voiding breaks during exercise, and 37.3% actually restricted their fluid intake to minimize leakage. While 90.3% of women who reported leakage impacted their activity just decreased their intensity, 80.7% avoided the activity entirely. Many women used pads (49.2%). Interest in pelvic floor physiotherapy to improve their UI was high (84.6%), but 63.5% of women still sought pessary or surgical management. Unfortunately, 35.6% of the women had no idea treatment was even an option.
Brennand et al. (2017) researched urinary leakage during exercise in Canadian women. A summary of their findings concluded that skipping, trampoline, jumping jacks, and running/jogging were most likely to cause leakage. To combat the problem, 93.2% emptied their bladder just before exercise, 62.7% required voiding breaks during exercise, and 37.3% actually restricted their fluid intake to minimize leakage. While 90.3% of women who reported leakage impacted their activity just decreased their intensity, 80.7% avoided the activity entirely. Many women used pads (49.2%). Interest in pelvic floor physiotherapy to improve their UI was high (84.6%), but 63.5% of women still sought pessary or surgical management. Unfortunately, 35.6% of the women had no idea treatment was even an option.
Nygaard & Shaw (2016) reviewed and summarized the cross-sectional studies regarding the association between physical activity and pelvic floor disorders. Trampolinists, especially those in the 3rd tertile of competition, even those who were nulliparous, experienced greater leakage. Competitive athletes in the highest quartile of time exercising were found to have 2.5 times the amount of urinary incontinence (UI) as the lowest inactive quartile; however, 2nd and 3rd quartile recreational athletes had no difference in UI compared to inactive women. Type and dosage of exercise were both factors in UI risk. Various studies showed habitual walking decreased UI in older women, moderate exercise decreased the risk of UI, and no exercise increased the risk of UI. The incidence of UI being related to having performed strenuous exercise early in life has been limited and variable, with one study of Norwegian athletes and US Olympians not having any greater UI later in life, while another showed middle-aged women who used to exercise 7.5 hours per week had a higher incidence of UI. This review also reported athletes had a 20% greater cross sectional area of the levator ani muscle and a greater pubovisceral muscle mean diameter; however, the pelvic floor strength recorded was lower than non-athletes.
Interestingly, Leitner et al. (2017) explored pelvic floor muscle activation for continent and incontinent females during running. For 10 seconds, EMG tripolar vaginal probe recorded activity at 7, 11, and 15km/h. No statistically significant differences between continent or incontinent subjects were found for the EMG values. Pre-activity and reflex activity mean EMG increased significantly with speed; mean pelvic floor muscle EMG activity during running was significantly above onset activation value; and, maximum voluntary contraction was exceeded 100% for all time intervals at 15km/h in women with UI. These authors suggested the stimulus of running could actually be beneficial in pelvic floor muscle training considering the reflex activity of the muscles.
At races now, I still silently survey my competition, but now I am more curious as to how many women are actually able to complete the run without leakage. The prevalence of UI among athletes continues and is becoming more of an open topic of conversation. The research as to how much and which kind of exercise correlates with UI or what activity and level of participation may be preventative for UI is growing. The need for pelvic floor therapists to treat athletes who are fit to be dry is ever increasing.
Brennand, E., Ruiz-Mirazo, E., Tang, S., Kim-Fine, S., Calgary Women’s Pelvic Health Research Group. (2017). Urinary leakage during exercise: problematic activities, adaptive behaviors, and interest in treatment for physically active Canadian women. International Urogynecology Journal. http://www.doi:10.1007/s00192-017-3409-1
Nygaard, I. E., & Shaw, J. M. (2016). Physical Activity and the Pelvic Floor. American Journal of Obstetrics and Gynecology, 214(2), 164–171. http://doi.org/10.1016/j.ajog.2015.08.067
Leitner M, Moser H, Eichelberger P, Kuhn A, Radlinger L. (2017). Evaluation of pelvic floor muscle activity during running in continent and incontinent women: An exploratory study. Neurourology and Urodynamics. 36:1570–1576. https://doi.org/10.1002/nau.23151
Everyone experiences constipation, sometime! Maybe it was on vacation and you felt bloated and miserable; or when you were busy at work and had to rush to complete a task. In any event, you felt ‘awful’. Maybe you couldn’t zip your favorite jeans due to abdominal bloating, maybe you experienced lower abdominal discomfort or experienced a painful ‘movement’ once you went. There are many people who experience these symptoms and more on a daily basis. When someone finally gets the courage to see a specialist about this problem, they might be diagnosed with ‘pelvic floor dyssynergia’ or ‘muscle incoordination’.

Pelvic muscle dyssysnergia (incoordination) refers to the action that occurs in the pelvic floor musculature at the time of defecation. It can become a withholding pattern and in the case of vacation or a change in your work schedule, it can simply be tensing the muscle to avoid the bowel movement (due to inconvenience) rather than heeding the ‘call’. Over time, if this behavior is repeated, it becomes muscle memory; instead of relaxing the pelvic muscle to defecate, the patient tenses the muscle; thus the term dyssynergia or incoordination. The function of the pelvic floor for bowel function is to provide closure of the anal canal to maintain continence. The muscle should signal the rectum and the colon when to defecate and should provide opening of the anal canal by total relaxation to allow for complete and effortless elimination. A dyssynergic pattern shuts the opening of the canal by tensing the muscle to prevent elimination. Thus an incoordination.
The research by Heymen, Scarlett, Ringman, Drossman et al entitled “Randomized, Controlled Trial Shows Biofeedback to Be Superior to Alternative Treatments for Patients with Pelvic Floor Dyssynergia-Type Constipation” supports the value of biofeedback in the treatment of this withholding pattern associated with stool elimination. This study supports the benefit of biofeedback treatments using internal sensors to provide the feedback displayed on a computer screen for visualization. This study goes on to say, “We also have shown that the machines are necessary—instrumented biofeedback is an essential element of successful training; however, there is a shortage of practitioners who are trained to provide this form of biofeedback, and there are few clinics where biofeedback instruments are available and where this form of biofeedback can be obtained”.
Biofeedback provides visual and auditory feedback of muscle tension. It is a non-invasive technique that allows patients to adjust muscle function, strength, and behaviors to improve pelvic floor function. The small electrical signal (EMG) provides information about an unconscious process and is presented visually on a computer screen, giving the patient immediate knowledge of muscle function, enabling the patient to learn how to alter the physiological process through verbal and visual cues. This mechanism allows the patient to assess muscle resting tone, creating an environment that teaches how to downtrain a tense pelvic floor while providing the means to teach co-ordination of muscle function.
In short, biofeedback treatment/training using the proper instrumentation provides the precise information necessary to change behaviors associated with tensing the pelvic floor for defecation instead of the proper relaxation of the pelvic floor for release of stool from the anal canal.
The Herman Wallace Course on Biofeedback Training for Pelvic Muscle Dysfunction provides the clinician with the proper treatment technique to use in the clinic to rehabilitate patients with pelvic floor muscle dyssynergia. Learning the proper use of biofeedback equipment and understanding the components to treating these challenging patients successfully is an essential component to this course. The clinician will learn numerous ways to teach this challenging patient population how to make this muscle function as intended, providing the patient with successful strategies for improved patient outcomes.
Today's blog is a contribution from Kristen Digwood, DPT, CLT, of the Elite Pelvic Rehab clinic in Wilkes-Barre, PA.
Urgency urinary incontinence (UUI), which is the involuntary loss of urine associated with urgency, is a common health problem in the female population. The effects of UUI result in limitations to daily activity and quality of life.
Current guidelines recommend conservative management as a first-line therapy in urinary incontinence, defined as "interventions that do not involve treatment with drugs or surgery targeted to the type of incontinence".
 Electrical stimulation is commonly used as part of a treatment program for women with UUI. There are several methods and parameters that can be used to improve urge incontinence, however the magnitude of the alleged benefits and best parameters is not completely established. Studies have suggested that the use of electrical stimulation to inhibit an overactive bladder functions to modulate unwanted detrusor contractions by way of sensory afferent stimulation of S2 and S3. This causes parasympathetic inhibition. In addition to this effect, contraction of the pelvic floor muscles results in inhibition and relaxation of the detrusor muscle which reduces urinary urgency.
Electrical stimulation is commonly used as part of a treatment program for women with UUI. There are several methods and parameters that can be used to improve urge incontinence, however the magnitude of the alleged benefits and best parameters is not completely established. Studies have suggested that the use of electrical stimulation to inhibit an overactive bladder functions to modulate unwanted detrusor contractions by way of sensory afferent stimulation of S2 and S3. This causes parasympathetic inhibition. In addition to this effect, contraction of the pelvic floor muscles results in inhibition and relaxation of the detrusor muscle which reduces urinary urgency.
Common methods of electrical stimulation include suprapubical, transvaginal, sacral and tibial nerves stimulation.
As with any medical treatment, practitioners seek the most effective methods and parameters to achieve the patient’s goals. A recent systematic review of electrical stimulation in the treatment of UUI included nine trials to treat UUI were included with total of 534 female patients. Most patients in the trials were close to 55 years of age. Five articles (total of nine) described a frequency of twice-weekly therapy and sessions of 20 minutes. Twelve weeks was the most common duration of therapy. All the studies applied an intensity of stimulation below 100 mA, with four of them (4/9) using 10 hz as the frequency. Intervaginal electrical stimulation showed the greatest subjective improvement and was the most effective.
The most frequent outcome measure was bladder diary, used in all papers; subjective satisfaction was used in 8; and quality-of-life questionnaires in 6, from a total of 9 papers.
The study noted that reports about electrical stimulation generally lack information on its cost-effectiveness. This is an important point, especially because in therapies with similar benefits cost may be one of the factors to indicate the most appropriate treatment. If we consider the relatively few adverse effects, low cost, and similar effectiveness when compared to medication, intravaginal electrical stimulation, according to available data, appears to be a good alternative treatment for UUI.
1. Thüroff JW, Abrams P, Andersson KE, Artibani W, Chapple CR, Drake MJ, et al.: EAU guidelines on urinary incontinence. Eur Urol. 2011; 59: 387-400.
2. Kralj B. The treatment of female urinary incontinence by functional electrical stimulation. In:Ostergard DR, Dent AD (eds). Urogenecology and Urodynamics. 3rd ed. Baltimore, MD: Williams and Wilkins; 1991.
3. Eriksen, BC. Electrical Stimulation. In: Benson JT editor. Female pelvic floor disorders: investigation and management. New York:Norton, 1992; 219-231.
4. Lucas Schreiner , Thais Guimarães dos Santos , Alessandra Borba Anton de Souza, et al. Int. braz j urol. vol.39 no.4 Rio de Janeiro July/Aug. 2013.
Allison Ariail, PT, DPT, CLT-LANA, BCB-PMD, PRPC is a published researcher and practitioner who has worked in the realms of brain injury, lymphedema, and oncology. Now she's leading the charge to encourage rehabilitation practitioners to utilize ultrasound diagnostic imaging with their patients, and you can learn these techniques in her Rehabilitative Ultrasound Imaging - Women's Health and Orthopedic Topics course taking place May 1 - 3 in Dayton, OH. We've partnered with SonoSite to make the best ultrasound equipment available for participants in this course.
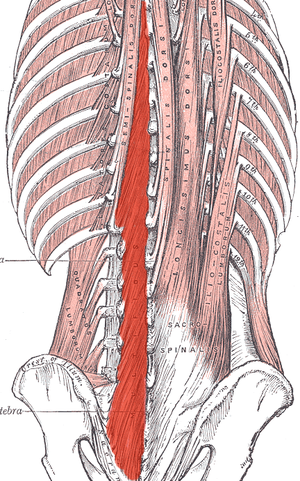
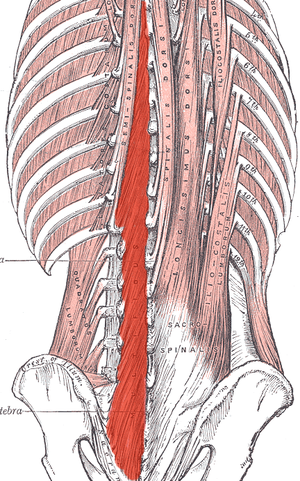 Most of us are treating patients who have back pain of some nature, and we know the importance of the local stabilizing muscles including the transverse abdominis, the lumbar multifidus, and the pelvic floor muscles. These muscles work together to provide tension and create a corset of stability throughout the trunk. A common goal is to rehabilitate these muscles in order to restore motor control and strength, but the muscle depth can make them difficult to assess and palpate.
Most of us are treating patients who have back pain of some nature, and we know the importance of the local stabilizing muscles including the transverse abdominis, the lumbar multifidus, and the pelvic floor muscles. These muscles work together to provide tension and create a corset of stability throughout the trunk. A common goal is to rehabilitate these muscles in order to restore motor control and strength, but the muscle depth can make them difficult to assess and palpate.
I recently read a study that is looking at the development of a test to identify lumbar multifidus function. Herbert et al. found promising results when looking at this “multifidus lift test” for inter-rater reliability and concurrent validity to identify dysfunction in the multifidus. They compared the results of this test with real-time ultrasound imaging of the lumbar multifidus. Inter-rater reliability was excellent and free from errors of bias and prevalence. Concurrent validity was demonstrated through its relationship with the reference standard results at L4-L5, but not so much for L5-S1. This preliminary research supports the reliability and validity of the multifidus lift test to assess lumbar multifidus function at some spinal levels. If this test could be further validated for other spinal levels it would be very beneficial for therapists who are using a specific stabilization program to treat patients.
Until this test is further developed and validated how can therapists know for sure that their patient is truly activating their multifidus? Ultrasound imaging is the answer! Ultrasound imaging gives therapists real-time feedback for whether a patient is able to correctly activate a muscle or not. It is also a wonderful biofeedback tool for patients who are trying to rehabilitate these muscles. Getting your hands on an ultrasound machine can be tough, but therapists who work in a hospital system may have an easier time than you'd think. I have worked with many therapists to help them get access to ultrasound units through “hand me down” units from imaging or labor and delivery departments. I also have helped private practice therapists set up a working relationship with a physician who has an ultrasound in their office. Thinking outside of the box can allow clinicians to gain access to ultrasound units without having to spend a lot of money. Join me in Dayton Ohio this May to hear more about how ultrasound imaging can improve your practice and allow you to incorporate a specific stabilization program into your toolbox.
Herbert JJ, Koppenhaver SL, Teyhen DS, Walker BF, Fritz JM. The evaluation of lumbar multifidus muscle function via palpation: reliability and validity of a new clinical test. Spine J. 2015; 15(6): 1196-202.
Faculty member Lila Bartkowski- Abbate PT, DPT, MS, OCS, WCS, PRPC teaches the Bowel Pathology, Function, Dysfunction and the Pelvic Floor course for Herman & Wallace. Join her in Tampa on April 2-3, or one of the other two events currently open for registration.
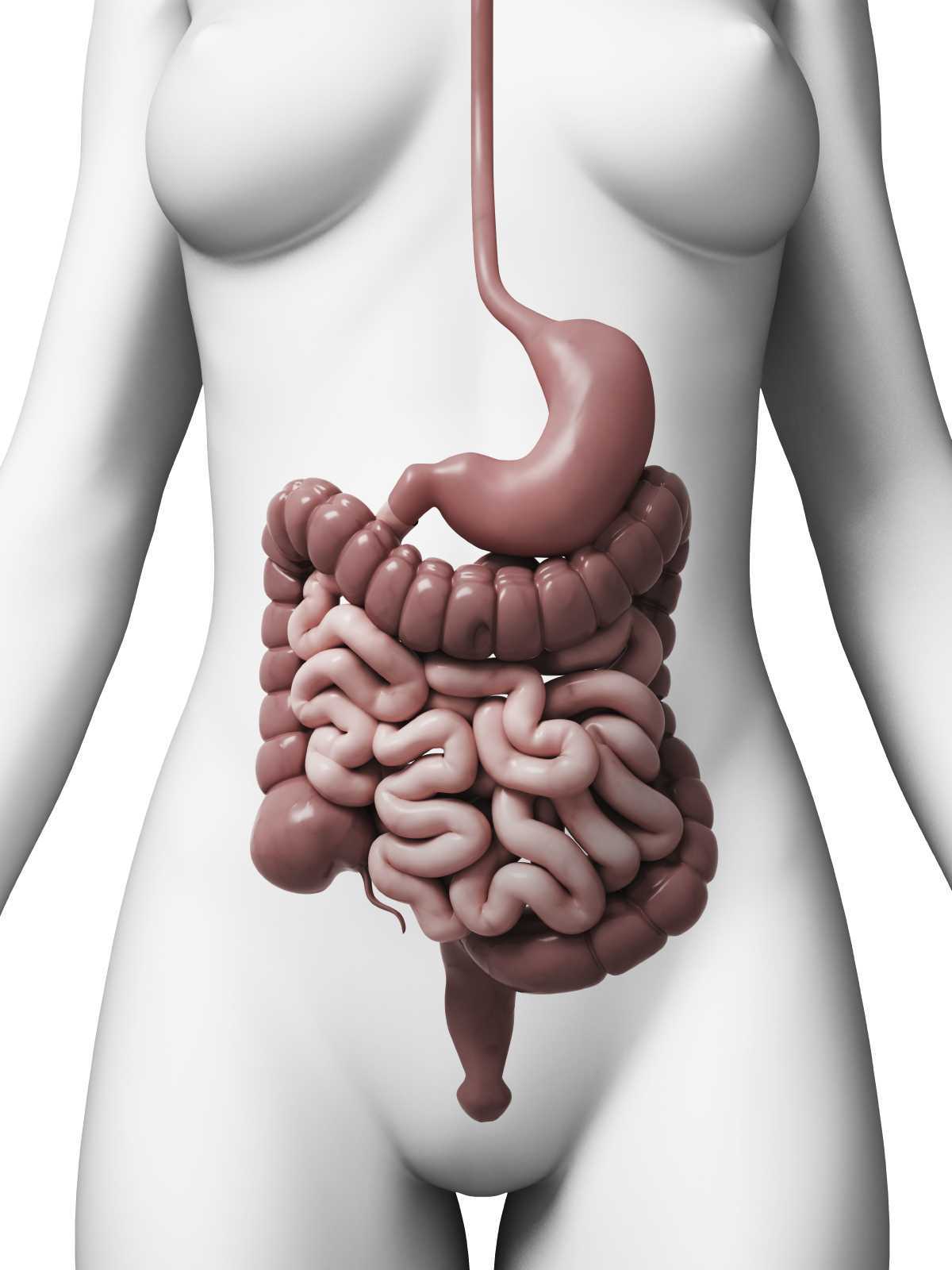 Constipation, an often under reported health issue, afflicts about 30% of Americans. ¹ The diagnosis of chronic constipation may seem like a simple concept, however the etiology of chronic constipation presents itself in many different forms. Dyssynergic defecation is one of many factors that can lead to a presentation of chronic constipation in a patient. Dyssynergic defecation or “paradoxical contraction” occurs when the muscles of the abdominals, puborectalis sling, and external anal sphincter function inappropriately while attempting a bowel movement. ² The lack of coordination of these muscles results in a contraction versus a lengthening of the pelvic floor muscles with baring down. Dyssynergic defecation is different than a structural issue such as a rectocele or hemorrhoids causing the inability to pass stool effectively or constipation due to slow colon transit time or pathological disease. Making the diagnosis of dyssynergic defecation by symptoms alone is often not reliable secondary to overlap of similar symptoms with chronic constipation due to factors such as a structural issue, irritable bowel syndrome (IBS), or irritable bowel disease (IBD). The diagnosis of dyssynergic defecation can be difficult and is often made through physiologic testing such as balloon expulsion testing or MRI with defecography. ² However, physical therapists can often manually feel that a paradoxical contraction is happening when asking a patient to bare down on evaluation.
Constipation, an often under reported health issue, afflicts about 30% of Americans. ¹ The diagnosis of chronic constipation may seem like a simple concept, however the etiology of chronic constipation presents itself in many different forms. Dyssynergic defecation is one of many factors that can lead to a presentation of chronic constipation in a patient. Dyssynergic defecation or “paradoxical contraction” occurs when the muscles of the abdominals, puborectalis sling, and external anal sphincter function inappropriately while attempting a bowel movement. ² The lack of coordination of these muscles results in a contraction versus a lengthening of the pelvic floor muscles with baring down. Dyssynergic defecation is different than a structural issue such as a rectocele or hemorrhoids causing the inability to pass stool effectively or constipation due to slow colon transit time or pathological disease. Making the diagnosis of dyssynergic defecation by symptoms alone is often not reliable secondary to overlap of similar symptoms with chronic constipation due to factors such as a structural issue, irritable bowel syndrome (IBS), or irritable bowel disease (IBD). The diagnosis of dyssynergic defecation can be difficult and is often made through physiologic testing such as balloon expulsion testing or MRI with defecography. ² However, physical therapists can often manually feel that a paradoxical contraction is happening when asking a patient to bare down on evaluation.
Patients with dyssynergic defecation may present to pelvic floor physical therapy with complaints of: ¹ ²
- Abdominal symptoms such as bloating, pain, and cramping
- Poor response to laxatives and fiber supplementation that does not fully resolve their issue
- Have had testing for anatomical or neurological abnormalities with no significant findings
- Complaints of concomitant pelvic pain due to over activity of the pelvic floor muscles
Physical Therapists specializing in pelvic floor rehab can be a valuable part of the medical team with treating these patients. Biofeedback training by physical therapists has been shown to decrease anorectal related constipation symptoms and abdominal symptoms in patients with dyssynergic defecation. In a sample of 77 patients with dyssynergic defecation, physical therapists provided biofeedback training for 6-8 weeks that included manual and verbal feedback, surface EMG, exercises using a rectal catheter, rectal ballooning to improve rectal sensory abnormalities, ultrasound, pelvic floor and abdominal massage, electrical stimulation if needed, and core strengthening and stretching to improve the patients’ maladaptive habits while attempting to pass a bowel movement. Significant decreases were seen on all three domains (abdominal, rectal, and stool) on the PAC-SYM (Patient Assessment of Constipation) questionnaire post biofeedback training. ² It is noteworthy that 74% of these patients presented to the clinic with complaints of abdominal symptoms such as bloating, pain, discomfort, and cramping.
Knowing how to effectively treat these patients and ask the right questions is valuable in the scheme of pelvic floor rehab secondary to overlapping symptoms of different causes of chronic constipation. Physical therapists are able to provide these patients with conservative treatment that can effectively improve or eliminate their problem, recognize dyssynergic defecation as a possible differential diagnosis, and refer to the appropriate medical professional for further testing. Recognizing and treating dyssynergic defecation is something physical therapists will learn how to become effective at in the upcoming Herman and Wallace Course: Bowel Pathology, Function, Dysfunction & the Pelvic Floor April 2-3 in Tampa, FL and October 8-9 in Fairfield, CA.
1. Sahin M, Dogan I, Cengiz M et al. (2015). The impact of anorectal biofeedback therapy on quality of life of patients with dyssynergic defecation. Turk J Gastroenterol. 26(2):140-144
2. Baker J, Eswaran S, Saad R, et al. (2015). Abdominal symptoms are common and benefit from biofeedback therapy in patients with dyssynergic defecation. Clin Transl Gastroenterol. 30(6)e105. doi: 10.1038/ctg.2015.3
As pelvic rehabilitation providers, it may be safe to assume a lot of us are treating adults with bladder and bowel dysfunction. Often we get questions from these patients about treatment for children with voiding dysfunction. How comfortable are we treating children for these problems and what would we do? Pediatric voiding dysfunction and bowel problems are common and can have significant consequences to quality of life for the child and the family, as well as negative health consequences to the lower urinary tract if left untreated. No clear gold standard of treatment for pediatric voiding dysfunction has been established and treatments range from behavioral therapy to medication and surgery.
 A randomized controlled trial in 2013 that was published in European Journal of Pediatrics, explores treatment options for pediatric voiding dysfunction. Pediatric voiding dysfunction is defined as involuntary and intermittent contraction or failure to relax the urethral striated sphincter during voluntary voiding. The dysfunctional voiding can present with variable symptoms including urinary urgency, urinary frequency, incontinence, urinary tract infections, and abnormal flow of urine from bladder back up the ureters (vesicoureteral reflux).
A randomized controlled trial in 2013 that was published in European Journal of Pediatrics, explores treatment options for pediatric voiding dysfunction. Pediatric voiding dysfunction is defined as involuntary and intermittent contraction or failure to relax the urethral striated sphincter during voluntary voiding. The dysfunctional voiding can present with variable symptoms including urinary urgency, urinary frequency, incontinence, urinary tract infections, and abnormal flow of urine from bladder back up the ureters (vesicoureteral reflux).
The 2013 study compared 60 children over one year who were diagnosed with dysfunctional voiding into two treatment groups. One group received behavioral urotherapy combined with PFM (pelvic floor muscle) exercises while the other group received just behavioral urotherapy. The behavioral urotherapy consisted of hydration, scheduled voiding, toilet training, and high fiber diet. Voiding pattern, EMG (electromyography) activity during voids, urinary urgency, daytime wetting, and PVR (post-void residue) were assessed at the beginning and end of the one year study with parents completing a voiding and bowel habit chart as well as uroflowmetry with pelvic floor muscle sEMG (surface electromyography) was administered to the child for voiding metrics.
All parents and children in both groups received education about urinary and gastrointestinal tract function as well as healthy bladder habits, effects of high fiber diet, scheduled voiding, and normal mechanics of toilet training. For the group that completed PFM exercises and education, they participated in 12 sessions (2x/week for 30 minutes) to learn the PFM exercises under the guidance of a single physical therapist. There was bimonthly follow up for both groups throughout the 12 months to ensure retention and application of the behavioral urotherapy.
The goal of the PFM exercises for the children was too restore the normal function of the PFM’s and their coordination with abdominal muscles. The exercises that the children completed, included exercises with and without a swiss ball. The exercises without a swiss ball included breathing with the diaphragm, Transversus Abdominus muscle isolation, hip adductor squeeze (isolation), bridging with PFM relaxation, and cat/camel to improve lumbopelvic coordination. Swiss ball exercises included seated PFM contraction and relaxation exercise with a seated lift and relax, supine bridge with roll out on the ball with PFM contraction, and supine swiss ball lift with the legs and pelvic contraction. (Pictures and more details about how the exercises were carried out in the article itself.)
The conclusion of the study was that the functional PFM exercises with swiss ball combined with behavioral urotherapy reduced the frequency of urinary incontinence, PVR (post void residue), and the severity of constipation in children with voiding dysfunction. The children in the combined group showed improvements with voiding pattern, reduced EMG activity during voids, reduced urgency, reduced daytime wetting, and improvements with more complete emptying with voids (reduced PVR).
The Functional PFM exercises are easy to teach and easy for children to complete. They are a safe, inexpensive, and effective treatment option for children with dysfunctional voiding. PFM exercises combined with behavioral urotherapy seems to be a logical treatment option for treating pediatric voiding dysfunction.
To learn more about pediatric bowel and bladder dysfunction and treatment for it consider attending Dawn Sandalcidi's Pediatric and Pelvic Floor Dysfunction course. The three opportunities in 2016 are Pediatric Incontinence - Augusta, GA April 16-18, Pediatric Incontinence - Torrance, CA June 11-12, and Pediatric Incontinence - Waterford, CT on September 17-18.
Seyedian, S. S. L., Sharifi-Rad, L., Ebadi, M., & Kajbafzadeh, A. M. (2014). Combined functional pelvic floor muscle exercises with Swiss ball and urotherapy for management of dysfunctional voiding in children: a randomized clinical trial. European Journal of Pediatrics, 173(10), 1347-1353.