In this post, we want to give a high-level overview of interstitial cystitis and an introduction to other resources if you’d like to dive deeper into treatment the condition. There’s a printable, patient-friendly version of this overview if you’d like to use it in describing the condition with patients. In addition, you may want to review the 8 Myths of Interstitial Cystitis series and the AUA Guidelines for Interstitial Cystitis.
Definition
Interstitial cystitis is defined as pain or pressure perceived to be related to the urinary bladder, associated with lower urinary tract symptoms of more than six weeks duration, in the absence of infection or other identifiable causes.
Unfortunately, for physicians, pelvic floor dysfunction falls under category of ‘unidentifiable cause.’ Interstitial cystitis is really more of a description of symptoms, rather than a discrete diagnosis, and the condition presents in many different ways.

Symptoms
The hallmarks of interstitial cystitis are pelvic pain, often in the suprapubic area or inner thighs, and urinary urgency and frequency. Other common symptoms include pain with intercourse, nocturia, low back pain, constipation, and urinary retention.
Many patients are surprised to realize that symptoms like painful intercourse, low back pain, and constipation are related to their IC diagnosis. This challenges the misconception that issues are arising solely from the bladder, and is a good way to help patients (and their physicians) understand that IC is about more than just the bladder.
Diagnosis
Interstitial cystitis is fundamentally a diagnosis of exclusion. Most patients suspect a urinary tract infection (UTI) when their symptoms first present. It’s actually common for symptoms to start as the result of a UTI, and simply not resolve once the infection has cleared. Patients are often treated with multiple rounds of antibiotics for these ‘phantom’ UTIs, where cultures have come back negative, before an IC diagnosis is considered.
It’s important for us as physical therapists to be able to share with patients that no testing is required to confirm an IC diagnosis, it can be diagnosed clinically. In practice, a urologist will likely want to conduct a cystoscopy, which can rule out more serious issues like bladder cancer as well as check for Hunner’s lesions (wounds in the bladder that are present in about 10% of IC patients). However, after that, no additional testing is needed. The potassium sensitivity test (PST) was formerly used by some urologists, but it has been shown to be useless diagnostically and extremely painful for patients and is not recommended by the American Urological Association. Urodynamic testing is also often conducted, but again is not necessary to establish an IC diagnosis.
Physical Therapy for IC
According to the American Urological Association, physical therapy is the most proven treatment for interstitial cystitis. It’s given an evidence grade of ‘A’ (the only treatment with that grade) and recommended in the first line of medical treatment.
In controlled clinical trials, manual physical therapy has been shown to benefit up to 85% of both men and women. These trials reported benefits after ten visits of one-hour treatment sessions.
In a study conducted at our clinic , PelvicSanity, we found that physical therapy was able to reduce pain for IC patients from an average of 7.6 (out of 10) before treatment to 2.6 following physical therapy. Similarly, how much their symptoms bothered patients fell from 8.3 to 2.8. More than half of patients reported improvements within the first three visits.
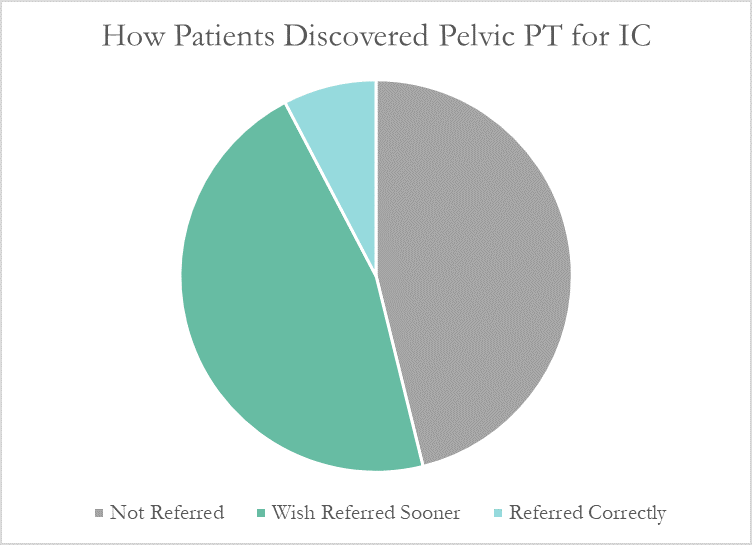
Unfortunately, many patients still aren’t referred to pelvic physical therapy by their physician. More than half of the patients in the study had seen more than 5 physicians before finding pelvic PT, and only 7% of patients felt they had been referred to physical therapy at the appropriate time by their doctor.
Multi-Disciplinary Approach
Patients with interstitial cystitis or pelvic pain always benefit from a multidisciplinary approach to treatment.This can include:
- Stress relief to downregulate the nervous system can decrease symptoms and reduce flares. Gentle exercise, meditation, yoga, deep breathing, or working with a psychologist can all provide benefits for patients.
- Diet and nutrition are important when working with IC patients. There is no formal ‘IC Diet’, but most patients are sensitive to at least a few trigger foods. The gold standard of treatment is an elimination diet, where the common culprits are completely removed from the diet and then added back in one at a time. This identifies which foods are triggers for patients. With nutrition for IC, patients should avoid their personal trigger foods and eat healthy – it doesn’t have to be any more restrictive or complicated.
- Alternative treatments like acupuncture have been shown to reduce pelvic pain in patients, and several supplements have shown benefits in trials or anecdotally among patients.
- Bladder treatments include instillations and nerve stimulation. Some patients may benefit from bladder instillations, but many others find that the process of the instillation actually causes additional symptoms. If instillations are beneficial, patients should be encouraged to address the underlying issues during the reprieve that instillations bring. Percutaneous tibial nerve stimulation or an implanted nerve stimulation device can both be possible treatment options.
- Oral medications can also reduce symptoms, but do not address the underlying cause of symptoms in patients. Medication that dampens the nervous system, often an anti-depressant or similar medication, can reduce pain and hypersensitivity. Anti-inflammatories may be beneficial in lowering inflammation and helping break the cycle of dysfunction-inflammation-pain. Most patients are started on Elmiron®, the only FDA-approved medication for IC; unfortunately, in the most recent clinical trial research Elmiron has been shown to be no more effective than a placebo. If it is effective, it only is beneficial for about one-third of patients, and many won’t be compliant with the drug due to cost and side effects.
 Nicole Cozean, PT, DPT, WCS (www.pelvicsanity.com/about-nicole) is the founder of PelvicSanity physical therapy in Southern California. Name the 2017 PT of the Year by the ICN, she’s the first physical therapist to serve on the Interstitial Cystitis Association’s Board of Directors and the author of the award-winning book The IC Solution (www.pelvicsanity.com/the-ic-solution). She teaches at her alma mater, Chapman University, as well as continuing education through Herman & Wallace. Nicole also founded the Pelvic PT Huddle (www.facebook.com/groups/pelvicpthuddle), an online Facebook group for pelvic PTs to collaborate.
Nicole Cozean, PT, DPT, WCS (www.pelvicsanity.com/about-nicole) is the founder of PelvicSanity physical therapy in Southern California. Name the 2017 PT of the Year by the ICN, she’s the first physical therapist to serve on the Interstitial Cystitis Association’s Board of Directors and the author of the award-winning book The IC Solution (www.pelvicsanity.com/the-ic-solution). She teaches at her alma mater, Chapman University, as well as continuing education through Herman & Wallace. Nicole also founded the Pelvic PT Huddle (www.facebook.com/groups/pelvicpthuddle), an online Facebook group for pelvic PTs to collaborate.
Interstitial Cystitis Course
In our upcoming course for physical therapists in treating interstitial cystitis (April 6-7, 2019 in Princeton, New Jersey), we’ll focus on the most important physical therapy techniques for IC, home stretching and self-care programs, and information to guide patients in creating a holistic treatment plan. The course will delve into how to handle complex IC presentations. It’s a deep dive into the condition, focusing not just on manual treatment techniques but also how to successfully manage an IC patient from beginning to resolution of symptoms.
Additional Resources
- Interstitial Cystitis Overview (printable)
- The Interstitial Cystitis Solution
- Patient groups include the Interstitial Cystitis Association (ICA) (www.ic-help.org) and the IC Network (www.ic-network.com), which both have fantastic resources for patients.
- The AUA Guidelines for IC
- IC Flare-Busting Plan
Dr. Nicole Cozean was just awarded the IC/BPS Physical Therapist of the Year by the IC Network, one of the largest patient advocacy groups for interstitial cystitis! Today she shares her treatment approach for this complex dysfunction. Join Dr. Cozean in San Diego on April 28-29, 2018 to learn everything there is to know about interstitial cystitis.
Interstitial cystitis (IC) is a chronic pelvic pain condition characterized by pelvic pain and urinary urgency/frequency. IC is frequently accompanied by other symptoms1, including painful intercourse, low back or hip pain, nocturia, and suprapubic tenderness.
While pelvic floor physical therapy is the most proven treatment for interstitial cystitis, most patients require a multi-disciplinary approach for optimal results. The majority are forced to develop this holistic approach on their own, but one of the most valuable things a physical therapist can provide is assistance in creating their own unique treatment plan. The American Urological Association has released treatment guidelines for interstitial cystitis, and potential treatments fall into several different categories. It is important to note that most treatments aren’t effective for the majority of patients, so a trial-and-error approach is needed to find the right balance for each patient. Tracking symptoms with a weekly symptom log can be a powerful tool to optimize the individual treatment plan.

Summary of the AUA Guidelines for IC – Download Here
Oral Medications
Oral medications are primarily used to reduce pain.Anti-depressants can dampen the nervous system, decreasing the severity of pain reported. Anti-histamines have also been shown to be effective in reducing the pain and symptoms of interstitial cystitis, perhaps because of their ability to reduce inflammation and break the cycle of dysfunction-inflammation-pain (the DIP cycle). Some patients require opioid painkillers for adequate pain control.
Urinary tract analgesics can provide temporary pain relief for some patients, but cannot be taken consistently because they thicken the urine and strain the kidneys. Some patients find success using these medications (Azo, Pyridium, Uribel) during severe pain flares.
The only FDA-approved oral treatment for interstitial cystitis is Pentosan Polysulfate (PPS, Elmiron®). This is commonly prescribed to patients after an IC diagnosis, but has been shown to be effective in only 28-32% of patients. It also requires a long time (often 6-9 months) to build up in the system and take effect, and many patients stop taking the drug before they could see effect because of side effects (including hair loss) or cost. Unfortunately, many patients lose more than a year after their initial diagnosis waiting to see if Elmiron will work for them, when it is unlikely to provide complete relief.
Antibiotics should never be prescribed for IC in the absence of a confirmed infection.
Bladder and Medical Procedures
Bladder instillations deliver numbing medication directly to the bladder through a catheter and can provide temporary pain relief for some patients. If these are effective, they typically are repeated at least weekly as symptoms return. Some patients don’t tolerate the catheterization well, finding the procedure causes more pain than it prevents. Typical bladder instillations consist of Lidocaine, Heparin, or a combination of the two.
Another route of treatment works by artificially stimulating the nerves the innervate the bladder and pelvic floor.Percutaneous tibial nerve stimulation (PTNS) directs electrical impulses from the ankle up through the pelvic floor. This is an outpatient procedure typically performed weekly for a course of 12 weeks. A more permanent option is implanting a device under the skin of the buttock to target the sacral or pudendal nerve root directly.With this procedure, the patient is given a ‘trial run’ with an external device to see how it performs. If significant improvements are noted, the device can be permanently implanted.
Many patients see marked improvement in their symptoms with a home care program. Deep breathing or meditation can calm the nervous system and reduce the amplifying effect of an upregulated nervous system. A stretching regimen targeting the inner thighs, glutes, abdomen, and pelvic floor can relax muscles and reduce nerve irritation in the region. Self-massage can find and eliminate the trigger points that are causing symptoms. Home tools like a foam roller can address external trigger points, while patients can be taught internal self-release with the help of a tool like the PelviWand or another tool.
Elimination Diet
One of the most common misunderstandings about IC centers on the ‘IC Diet.’ In fact, there’s no such thing. While nearly 90% of IC patients report that diet influences their symptoms in some way, the scope and severity of dietary triggers varies greatly between patients. There are a few common culprits - coffee, tea, citrus fruits, artificial sweeteners, tomatoes, cranberry juice - but no guarantee that a patient will be sensitive to all (or any) of these. Many patients read about an ‘IC Diet’ online after receiving their diagnosis, and are convinced that they need to cut out a huge portion of their diet.
Instead, they should be doing an elimination diet focused on identifying their trigger foods.With this approach, they eliminate most of those common culprits and see how it affects their symptoms.If they notice an improvement, they can gradually add foods back into their diet, one at a time, until they see symptoms increase again. This allows patients to identify their specific trigger foods.
Our advice for IC patients is simple - avoid your trigger foods and eat healthy. It doesn’t have to be any more restrictive than that.
There are also several supplements that have shown benefit for patients, either in clinical trials or anecdotally. Prelief (calcium glycerophospate) is an antacid that may reduce the consequences of eating a trigger food. L-Arginine is a semi-essential amino acid that facilitates blood flow and vasodilation; in clinical trials it was shown to be effective for nearly 50% of patients in reducing pain and urinary symptoms. Aloe Vera pills are used by many patients, and thought to help replenish the bladder’s protective layer. Finally, a combination of supplements known as Cystoprotek is also a common supplement taken by IC patients, combining anti-inflammatory flavonoids with molecules that may reinforce the bladder lining.
Complementary and Alternative Medicine
Acupuncture has been shown to provide relief for pelvic pain patients2, with 73% of men with chronic prostatitis (either identical or closely related to IC) reporting improvement. These men received two treatments weekly for six weeks, focusing around the sacral nerve. Women with pelvic pain and painful intercourse have also reported improvements in pain with 10 sessions of acupuncture3.
Cognitive-Behavioral Therapy (CBT) has been shown to help reduce pain in conditions as diverse as cancer, low back pain, and pelvic pain. In pelvic pain, ten one-hour sessions of CBT was shown to provide significant benefit for nearly half of patients4. Supportive psychotherapy was also shown to have benefits for pelvic pain patients.
A multi-disciplinary approach provides the best results for patients. Physical therapists, who see our patients regularly, can be a great resource in suggesting additional treatment options. The American Urological Association IC Guidelines can be an important resource in guiding patients to other options and developing their unique treatment plan.
Information and Resources
For additional patient resources available for download, feel free to visit The IC Solution page.. In our upcoming course for clinicians treating interstitial cystitis (April 28-29, 2018 in San Diego), we’ll focus on the most important physical therapy techniques for IC, home stretching and self-care programs, and information to guide patients in creating a holistic treatment plan.
1. Cozean, N. "Pelvic Floor Physical Therapy in the Treatment of a Patient with Interstitial Cystitis, Dyspareunia, and Low Back Pain: A Case Report". Journal of Women's Health Physical Therapy. 2017
2. Chen R, Nickel JC. "Acupuncture ameliorates symptoms in men with chronic prostatitis/chronic pelvic pain syndrome"Urology. 2003 Jun;61(6):1156-9; discussion 1159.
3. Schlaeger, J, et al. "Acupuncture for the Treatment of Vulvodynia: A Randomized Wait‐List Controlled Pilot Study". Journal of Sexual Medicine. 30 January 2015. https://doi.org/10.1111/jsm.12830
4. Masheb, et al. "A randomized clinical trial for women with vulvodynia: Cognitive-behavioral therapy vs. supportive psychotherapy". PAIN® Volume 141, Issues 1–2, January 2009, Pages 31-40
You have been treating a highly motivated 24-year-old woman with a diagnosis of Interstitial Cystitis/Painful Bladder Syndrome (IC/BPS). The plan of care includes all styles of manual therapy, including joint mobilization, soft tissue mobilization, visceral mobilization, and strain counterstrain. You utilize neuromuscular reeducation techniques like postural training, breath work, PNF patterns, and body mechanics. Your therapeutic exercise prescription includes mobilizing what needs to move and strengthening what needs to stabilize. Your patient is feeling somewhat better, but you know she has the ability to feel even more at ease in their day to day. Is there anything else left in the rehab tool box to use?
 Kanter et al. set out to discover if mindfulness-based stress reduction (MBSR) was a helpful treatment modality for (IC/BPS). The authors were interested in both the efficacy of a treatment centered on stress reduction and the feasibility of women adopting this holistic option.
Kanter et al. set out to discover if mindfulness-based stress reduction (MBSR) was a helpful treatment modality for (IC/BPS). The authors were interested in both the efficacy of a treatment centered on stress reduction and the feasibility of women adopting this holistic option.
The American Urological Association defined first-line treatments for IC/PBS to include relaxation/stress management, pain management and self-care/behavioral modification. Second-line treatment is pelvic health rehab and medications. The recruited patients had to be concurrently receiving first- and second-line treatments, and not further down the treatment cascade like cystoscopies and Botox.
The control group (N=11) received the usual care (as described above in first- and second-line treatments). The intervention group (N=9) received the usual care plus enrollment in an 8-week MBSR course based on the work of Jon Kabat- Zinn. The weekly course was two hours in the classroom supplemented with a 4-CD guide and book for home meditation practice carryover. The course content included meditation, yoga postures, and additional relaxation techniques.
The patients who participated in the MBSR program reported improved symptoms post-treatment, and perhaps more notably, their pain self-efficacy score (PSEQ) significantly improved. All but one of the participants reported feeling “more empowered” to control their bladder symptoms.
As clinicians working so intimately with our patients, we are often given the privilege of bearing witness to the emotional pain of healing chronic, persistent pelvic pain. We understand how terribly frightening it is for our patients to feel like they will never get better and we see this come out sometimes as fear-avoidance, which has the potential to cascade further into other areas of the social sphere.
If we are able to encourage holistic methods of building strategies to handle the challenges of IC/BPS, our patients will be set up for success in ways beyond the treatment room. While we hope for immediate results in the form of pain relief (which five patients in the study did), we also can appreciate the strategy building for resiliency in the face of persistent pain. As a very strong woman said, “hope serves us best when we do not attach specific outcomes to it”.
Dustienne Miller is the author and instructor of Yoga for Pelvic Pain. Join her in Manchester, NH on September 7-8, 2019 or in Buffalo, NY on October 5-6, 2019 to learn about treating interstitial cystitis/painful bladder syndrome, vulvar pain, coccydynia, hip pain, and pudendal neuralgia with a yoga approach.
Kanter G, Kommest YM, Qaeda F, Jeppson PC, Dunivan GC, Cichowski, SB, and Rogers RG. Mindfulness-Based Stress Reduction as a Novel Treatment for Interstitial Cystitis/Bladder Pain Syndrome: A Randomized Controlled Trial. Int Urogynecol J. 2016 Nov; 27(11): 1705–1711.
Interstitial cystitis is a chronic pain condition characterized by both pelvic pain and urinary symptoms. It’s diagnosed by unexplained pain or pressure that is perceived to be related to the bladder, and affects more than 12 million Americans. It’s often described as the sensation of a urinary tract infection, but without any bacterial infection. Many patients report severe pain, often more intense than that associated with bladder cancer, and up to 85% of patients have accompanying pelvic floor dysfunction.
Pelvic floor physical therapy is the most proven treatment for interstitial cystitis. It’s recommended by the American Urological Association (AUA) as a first-line medical treatment in their IC Guidelines, and is the only treatment given an evidence grade of ‘A’. Furthermore, it’s the sole intervention that provides sustained relief; bladder treatments and oral medications must be continued indefinitely to provide benefit, if they work at all.
Research has demonstrated that at least 85% of patients with interstitial cystitis also have pelvic floor dysfunction. In fact, many of the symptoms of IC can only be explained by the pelvic floor. The majority of patients report painful intercourse, low back pain, hip pain, or constipation accompanying the condition; symptoms that have nothing to do with the bladder.
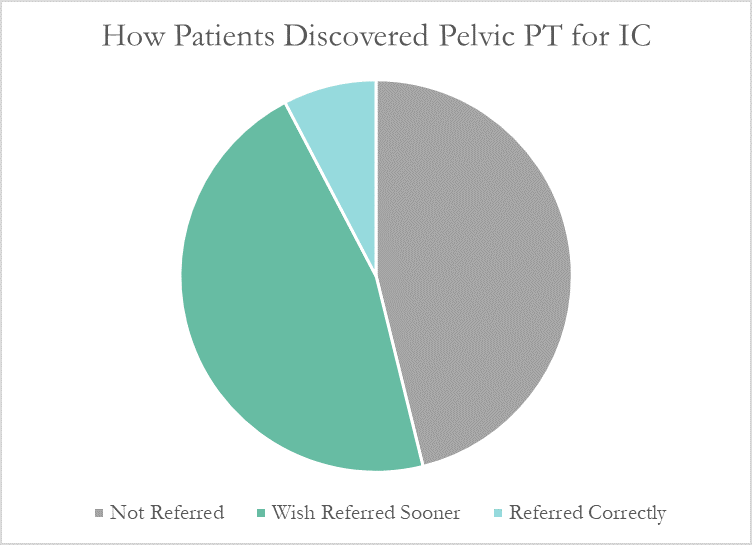
Despite this, many patients don’t learn about pelvic floor physical therapy for years after their diagnosis. Many have to discover pelvic PT for themselves, or their doctor only mentions physical therapy as a last resort. At PelvicSanity, we just published a study of our interstitial cystitis patients in the International Pelvic Pain Society (IPPS) meeting, reporting on both patient outcomes and their experience with the medical system following their IC diagnosis.
In following the results for thirteen consecutive patients with an interstitial cystitis diagnosis, patients reported more than a 60% improvement in pain, symptom bother, and how much symptoms limited their daily activities. On average, their pain level was at a 7.6 out of 10 upon initial evaluation, which fell to 2.6 after treatment.
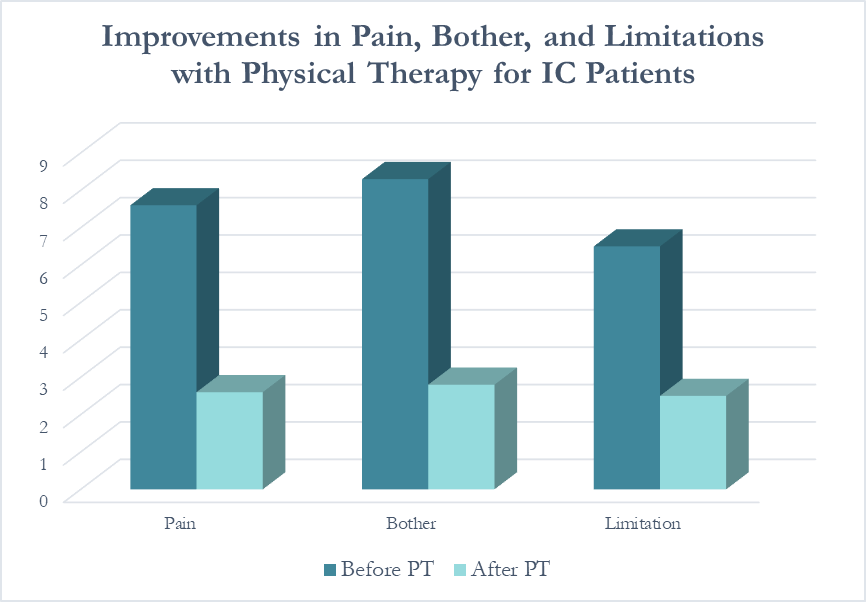 Patients saw a relatively rapid improvement in their symptoms with treatment. Over half (54%) reported an improvement in symptoms within their first three visits; 31% saw their first improvement in visits 4-6 and 15% required ten or more visits for subjective improvement. Importantly, all patients in the study reported a better understanding of their condition and feeling more hopeful for recovery after their initial evaluation.
Patients saw a relatively rapid improvement in their symptoms with treatment. Over half (54%) reported an improvement in symptoms within their first three visits; 31% saw their first improvement in visits 4-6 and 15% required ten or more visits for subjective improvement. Importantly, all patients in the study reported a better understanding of their condition and feeling more hopeful for recovery after their initial evaluation.
More than half of these patients reported seeing five or more medical doctors for their condition prior to beginning pelvic floor physical therapy, and had been prescribed multiple medications and undergone bladder treatments without success. However, only a single respondent (7.7%) believed they had been referred to pelvic PT by their doctor at the appropriate time. Nearly half (46%) had to find out about pelvic floor physical therapy for interstitial cystitis themselves, while the remainder felt they had been referred by their doctor far too late, as a last resort.
With more than 12 million women and men suffering with this condition in the United States alone, increasing education – for both doctors and patients – is vital. In our upcoming course for physical therapists in treating interstitial cystitis (April 28-29, 2018 in San Diego), we’ll focus on the most important physical therapy techniques for IC, home stretching and self-care programs, and information to guide patients in creating a holistic treatment plan
If you area clinic owner, are in a management or leadership position, one of your jobs is making sure your therapists are using best practices. This can be a challenge when best practices are continually being researched and discussed, and when systematic reviews continue to tell us that pelvic rehabilitation research lacks homogeneity and enough high-level evidence to make convincing arguments about interventions. In the absence of this, we can still integrate recommendations from clinical practice guidelines and from best practice statements. The American Physical Therapy Association's (APTA) Section on Women's Health (SOWH) is participating in the APTA's initiative to develop clinical practice guidelines. For current guidelines, check out their page here. To see which guidelines are in development at the APTA, click here.

The American Urological Association (AUA) has also developed practice guidelines, including the Guideline on the Diagnosis and Treatment of Interstitial Cystitis/Bladder Pain Syndrome (IC/PBS). Within this guideline, the first line treatments are listed as general relaxation/stress management, pain management, patient education, and self-care/behavioral modification. Second-line treatments include "appropriate manual physical therapy techniques", oral medications, bladder medications (administered inside the bladder), and pain management. What is very interesting about this guideline is that the authors define what types of manual therapy approaches are appropriate, and these include techniques that resolve muscle tenderness, lengthen shortened muscles, release painful scars or other connective tissue restrictions. The guidelines also define who should be working with patients who have IC/PBS and pelvic muscle tenderness: "appropriately trained clinicians". Very importantly, the authors state that pelvic floor strengthening exercises should be avoided.
How can these guidelines be used to assess best practices? Find out if your therapists who work with patients who have IC/PBS are indeed instructing in relaxation strategies, using pain education and pain management techniques (for pain-brain education specific to pelvic pain, check out the book "Why Pelvic Pain Hurts". Find out if your therapist is instructing in pelvic muscle strengthening as a first-line of treatment, since this would not be in line with the AUA guidelines. (Having said this, teaching pelvic muscle strengthening can be very appropriate when done with consideration of pelvic muscle pain.) Lastly, ask your therapist if she feels that her skill set and training is sufficient to treat the condition. Even in our comprehensive pelvic floor series, there is so much to learn at the initial course that IC/PBS is not discussed in great detail until PF2B. Maybe a little more knowledge and training would help your therapist feel that she is providing the "appropriate manual physical therapy techniques" recommended in the guidelines.
To find out when the next intermediate or advanced course in the series is happening, or to find other specialty courses, check our course listings to see if there is a course happening near you!