Infertility is often times a very sensitive subject for couples who are struggling to conceive. In the US, there are approximately 6.7 million women who are facing challenges with getting pregnant. (CDC 2006). In 2015, a ten-year retrospective study examined the efficacy of manual physical therapy to treat female infertility and discovered significantly positive outcomes.
The study looked at data collected from 2002-2011, which included approximately 1,392 patients treated for infertility. It specifically included those with single or multiple causes for infertility that involved: 1) elevated FSH (follicle stimulating hormone) of 10 mIU/ml or higher 2) fallopian tube occlusion 3) Endometriosis- when the lining of the uterus grows outside of the uterus causing significant pain, abnormal bleeding, infertility 4) Polycystic Ovarian Syndrome (PCOS)- a condition that affects female hormone regulation at times producing multiple follicles that remain as cysts in and around the ovary 5) Premature Ovarian Failure (POF)-loss of ovarian function before a woman is 40 years old and 6) Unexplained Infertility (Rice, 2015)
Patients were treated using an individualized physical therapy treatment plan that was named the CPA (Clear Passage Approach) protocol. This protocol was tailored to meet the individual needs of the patients and to treat specific sites of restrictions and immobility within each patient’s body. Treatment included integrated manual therapy techniques focused on minimizing adhesions and decreasing mechanical blockages in order to improve mobility of soft tissue structures. Visceral manipulation was also used to help restore normal physiologic motion of organs with decreased motility.
The application of these specific manual therapy modalities are thought to activate the central nervous system by stimulating a local tissue response and thus increasing communication with higher control centers in the brain that have the ability to positively influence the activity of the ovary and uterus, as a result effecting hormone production and regulation.
The study compared manual physical therapy treatment to previously published success rates with standard, conventional treatments for female infertility. The results were astounding. Researchers discovered that with the application of the CPA manual therapy approach, fallopian tube patency of at least one fallopian tube was 60.8% successful. When compared with the reported success rates in the literature, “it was observed that the CPA performed as well as or at higher rates of success than surgery did.” The rate of pregnancy for those patients with at least 1 open fallopian tube was also very successful with an overall pregnancy rate of 56.64% post CPA treatment.
For those women with endometriosis (n=558), the success rates for pregnancy post CPA treatment was 42.8%. For those who underwent IVF (In Vitro Fertilization) after CPA treatment, the pregnancy rates were even higher at 55.4%. These findings were also comparable to or better than standard medical interventions published in current literature.
Manual therapy has even shown to decrease elevated FSH levels and improve pregnancy rates by almost 50%. Researchers acknowledge that, to date, there are no medical treatments that represent standard care for women with elevated FSH levels and require more investigation for comparative results.
Of the 59 women with PCOS, the overall pregnancy success rate was 53.57%. The only significant and direct comparison with standard of care literature was with the use of metformin. Comparably, CPA produced significantly higher rates of pregnancy than with metformin alone. No statistically significant outcomes were reported. Unexplained infertility and POF had the least success rates of pregnancy reported. This is most likely attributable to a lack in subject size and/or no published medical treatment in these specific patient cases, further warranting the need for future investigation.
In conclusion, manual physical therapy has been shown to reverse female infertility in cases such as occluded fallopian tubes, endometriosis, hormone dysregulation, and PCOS. With all of the conventional options available, it is wonderful to know that manual therapists specializing in pelvic health have a clinical significance in helping change the lives of women struggling with infertility.
Center for Disease Control and Prevention (2006-2010). Infertility. Retrieved from http://www.cdc.gov/nchs/fastats/infertility.htm
Rice AD, Patterson K, Wakefield LB, Reed ED, Breder KP, Wurn BF, King CR, Wurn LJ. Ten-year Retrospective Study on the Efficacy of a Manual Physical Therapy to Treat Female Infertility. Alternative Therapies. 2015.(21)3;32-40.
Does prior training in pelvic floor muscle exercises contribute to a woman’s ability to contract the pelvic floor shortly after childbirth? Researchers aimed to study this question and other variables in a prospective observational study involving 958 women. Within one week of childbirth, and in the hospital setting, participants were instructed by a physiotherapist (specializing in pelvic floor) to contract the pelvic floor in a supine position. Confirmation of a contraction was determined by visual observation of the perineum moving inward. The women were also asked by a physiotherapist if they had prior knowledge or experience with pelvic floor muscle training, and if not, the women were briefly instructed in the location and function of the pelvic floor muscles. The women who had some knowledge of the pelvic floor muscles including exercise experience “…were asked if they considered themselves able to perform correct…” pelvic muscle contractions.
All women was asked to complete three pelvic muscle contractions in a row and were assessed visually using a score of 0 (no movement of the perineum), 1 (weak movement), or 2 (strong inward displacement/lift of perineum). The physiotherapist gave feedback if the women completed a correct, insufficient, or incorrect contraction. Further verbal instruction was provided to those who could not adequately contract, and a re-assessment was completed with a quantification of any change in ability to contract. After providing feedback on pelvic muscle contractions, 73.6% of the women were able to perform a better contraction. In 500 of the 958 women, no inward displacement of the perineum was observed. Additionally, a significant number of the women (33%), believed that they were doing a contraction correctly but in fact were not. Another interesting point is that women with urinary incontinence before or during pregnancy had more knowledge about pelvic floor function and training.
Although in this study, 47.8% of the participants were able to perform a pelvic floor muscle contraction shortly after giving birth, “Knowing about the function and location of the pelvic floor was a positive predictor for being able to complete a pelvic floor muscle contraction.” Interestingly, having prior training in pelvic muscle exercises was not predictive of being able to complete a contraction. The value of assessing the ability to contract the pelvic floor is evident in this study, and with methods that are quick, easy, and non-invasive, women can be empowered with an improved ability to improve performance of a pelvic muscle contraction which is necessary for an effective pelvic muscle training program.
Dr. Susane (Susie) Mukdad is the founder of Healing Hands Physical Therapy, Inc., located in Willow Springs, IL.
Being a new mom is such a blessing, a new chapter in a woman’s life filled with joy, happiness, and many surprises! But giving birth can also bring about many changes in a woman’s physical, emotional, and social health. Increased level of sex hormones can result in physiological, cognitive, and musculoskeletal changes. These fluctuations continue to occur after birth, placing a new mom, who is now faced with many physical and emotional challenges at risk for burn out. In addition, new moms have to worry about their careers and relationships, suffer sleep deprivation, and the availability for support from their family and friends all of which can affect a new mom’s self-esteem, mood, and most importantly parenting ability.
According to a recent CDC survey, approximately 8-19% of women experience postpartum depression. In most cases, this occurs during the first 3 mo postpartum.
So, how can a new mom improve her well-being after having a baby?
"The number of women who were 'at risk' for postpartum depression prior to the treatment, dropped by nearly 50% at the end of treatment"
A recent study published in the Journal of the American Physical Therapy Association reports that participating in an individualized exercise and education program can significantly improve postpartum well-being. The researchers performed a Randomized Control Trail that looked at 161 new moms all of which were randomly selected into two groups: 1) Mom & Baby Program + Education 2) Education Only. The Mom & Baby Program consisted of an individualized postpartum exercise regimen for 60 min/1x per week conducted by a licensed physical therapist. In addition, participants received 30-minute educational sessions from various healthcare professionals that included, physical therapist, health psychologists, nutritionists, midwives, and speech pathologists. The Education Only group received informational material mailed to them over an 8-week period. Treatment lasted for a total of 8 weeks.
When the two groups were compared, the results were significant! Moms that were in the Mom & Baby Program + Education group reported significantly better well-being and depressive scores and the number of women who were “at risk” for postpartum depression prior to the treatment, dropped by nearly 50% at the end of treatment.
So what does this all mean?

It means that having a support group, someone coaching you through a safe exercise program and educating you on the ins and outs of being a new mom can be extremely beneficial to your health and overall well-being, reducing your risk of the postpartum blues. Having a team of well rounded healthcare practitioners such as physical therapists, doulas, midwives, and nutritionists can significantly improve your experience of being a new mom and provide you with the lasting support that you need to not only take care of yourself, but also your new baby.
For more on postpartum patient health, consider attending Herman & Wallace's Care of the Postpartum Patient course. The next event will be in Seattle, WA on March 12-13, 2016.
Norman, et al. An Exercise and Education Program Improves the Well-Being of New Mothers: A Randomize Control Trial. PHYS THER. 2010; 90:348-355
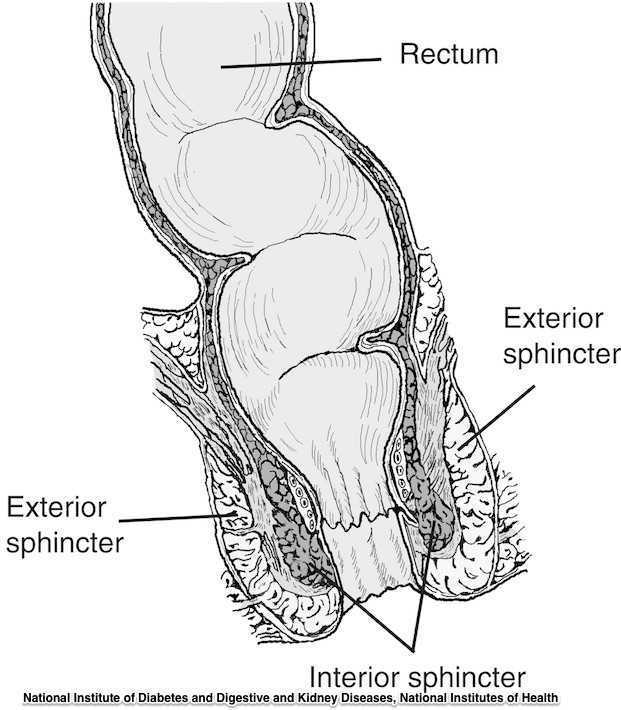
Guidelines for the management of 3rd and 4th degree tears were updated and published last month by The Royal College of Obstetricians & Gynaecologists. The purpose of the guidelines are to provide evidence-based guidelines on diagnosis, management and treatment of 3rd and 4th degree perineal tears. These types of tears are also referred to as obstetric anal sphincter injuries, or OASIS. The authors acknowledge an increased rate of reported anal sphincter injuries in England that may in part be due to increased awareness and detection of the issue. In terms of classification of anal sphincter injuries, the following is recommended (note the different levels at grade 3:
- 1st degree tear: injury to the perineal skin and/or the vaginal mucosa
- 2nd degree tear: injury to the perineum involving the perineal muscles but not involving the anal sphincter.
- 3rd degree tear: injury to the perineum involving the the anal sphincter complex
- Grade 3a tear: Less than 50% of the external anal sphincter (EAS) thickness is torn.
- Grade 3b tear: More than 50% of the EAS thickness is torn.
- Grade 3c tear: Both the EAS and the internal anal sphincter (OAS) are torn.
- 4th degree tear: Injury to the perineum involving the anal sphincter complex (EAS and IAS) and the anorectal mucosa.
Risk factors for anal injury are also outlined in the guidelines, although the authors point out that accurate prediction based on the risk factors is not reliable. The noted risk factors are as below:
- Asian ethnicity
- Nulliparity
- Birthweight greater than 4 kg (8.8 lb)
- Shoulder distocia
- Occipito-posterior position
- Prolonged 2nd stage labor
- Instrumented delivery
Recommendations worth noting include Level A evidence that warm compression during the 2nd stage of labor reduces the risk of OASIS. A noted best practice recommendation is that “Women should be advised that physiotherapy following repair of OASIS could be beneficial.” Guidelines such as these from The Royal College of Obstetricians & Gynaecologists can help in creating common language and in making recommendations that improve communication and expectations between patients and providers.
If you are interested in learning more about anal tears, Herman & Wallace offers several courses which cover the topic. For postpartum care specifically, check out Care of the Postpartum Patient.
Pelvic rehabilitation providers commonly treat a variety of conditions associated with peripartum pelvic girdle dysfunction. This list of conditions includes coccyx pain, and a recent study aimed to identify risk factors which may lead to coccyx pain in the postpartum period. Dr. Jean-Yves Maigne, who is well known for providing foundational research on the topic of coccyx pain, and colleagues completed a case series of 57 postpartum women presenting to a specialty coccydynia clinic. Dynamic x-rays were taken to assess mobility of the coccyx, and data about delivery methods were collected. (A control group of 192 women were comprised of women who also presented to the clinic but who had coccyx pain from other causes.)
The authors found that the women reported immediate postpartum pain in the coccyx with sitting. Instrumentation was a common finding in regards to the patients’ deliveries. 50.8% of the deliveries utilized forceps while 7% were vacuum-assisted. An additional 12.3% of the deliveries were spontaneous and were described as “difficult.” A subluxation of the coccyx was observed in 44% of the women who developed coccyx pain after childbirth as compared to 17% of the controls. A fractured coccyx occurred in 5.3 % of the women. Body mass index (BMI) of more than 27 and having 2 or more vaginal deliveries was also associated with a higher prevalence of a subluxation of the coccyx.
Being unable to sit comfortably following childbirth could make a new parent’s life very difficult with limitations in activities such as sitting to feed the baby. Socially, being unable to sit comfortably can also limit many activities. The women in this study reported immediate tailbone pain with sitting, which can alert providers to a condition requiring both immediate and follow-up attention. Risk factors such as having a difficult delivery or use of forceps may also signal a patient history that may lead to coccyx pain.
If you are interested in learning more about managing coccyx pain, join Lila Abbate at Coccyx Pain Evaluation and Treatment in Bay Shore, NY on October 25-26! You may also be interested to learn more about treating patients during the postpartum period, in which case Care of the Postpartum Patient is right up your alley!
Researchers in Brazil assessed the effects of low-frequency and high-frequency TENS, or transcutaneous electrical stimulation on post-episiotomy pain. This randomized, controlled, double-blind trial included the two electrotherapy interventions as well as a control group. TENS was applied for 30 minutes to the three groups: the high-frequency TENS (HFT) (100 Hz, 100 ms) the low-frequency TENS (5 Hz, 100 ms), and the placebo group. Electrode placement was near the episiotomy in a parallel pattern, and pain evaluations were completed before and after TENS application in resting, sitting, and ambulating. (Electrode placement specifics can be found in the article that is available within the above link.) The interventions and pain evaluations were carried out between six and 24 hours after vaginal delivery.
The intensity of the HFT and LFT was controlled by the participants, with instructions to allow the sensation to be both strong and tolerable. A total of 33 participants completed the study, with 11 in the HFT group, 13 in the LFT group, and 9 in the placebo therapy group. The researchers found that for HFT and LFT, pain improved following application of the electrotherapy, and the effects of the pain reduction lasted one hour after the intervention. Because TENS is a low-cost, low-risk modality, TENS use may be a welcome addition for postpartum care following an episiotomy. The women using high or low-frequency TENS in this study reported that TENS was comfortable and that they would opt to use it again.
If you are interested in learning more about postpartum care and issues such as episiotomies which can interfere with return to function, join faculty member Jenni Gabelsberg in Santa Barbara in January. In addition to discussing a wide variety of common musculoskeletal conditions, she will discuss pelvic floor issues following childbirth that can impact a woman's postpartum recovery. Click here to view the learning objectives for Care of the Postpartum Patient as well as additional dates and locations for this course.

A recent literature review addressing the effectiveness of yoga for depression reports that the positive findings are promising. The 2007 National Health Interview Survey (NHIS) found that yoga was one of the top 10 complementary health approaches used among adults in the United States. (The linked page for the NHIS also includes a video of the scientific results of yoga for health.)
Yoga is not only about bodies bending- ancient yoga traditions offer physical, mental, and spiritual techniques that are designed to be holistic in nature. Many instructors in the US focus on the many physical benefits of yoga, yet there are many types of yoga, many instructors with varied levels of training, and many health issues that require an individualized program of yoga therapy. In relation to the potential effects of yoga on depressive symptoms, theories in neurobiology point to the potential positive effects on the HPA (hypothalamic-pituitary-adrenal) axis, according to the linked article by Lila Louie.
While none of the articles described in the literature review are specific to the one patient group or population, the subjects studied include incarcerated women, older patients, university students, and patients from the general population who struggle with depression. One group of patients known to be at risk for severe depression is postpartum women. The definition of postpartum varies, and a generous definition may include any issue that, once imparted in a postpartum period and left unaddressed, could persist throughout a woman's lifetime. This is commonly seen in the clinic as uncorrected postural dysfunction, pelvic floor dysfunction, or gait changes, for example.
Because both yoga and exercise "appear to ameliorate depression," the author of the literature review states that motivation and compliance towards either modality should be considered during treatment planning for patients. Louie further states that yoga practice of asanas is safe, cost-effective, versatile, and can be used on its own or as an adjunct to medication. If you would like to learn more about the use of yoga for the postpartum population, sign up for Ginger Garner's continuing education course: Yoga as Medicine for Labor and Delivery and Postpartum offered in Seattle in August. To read about Ginger's Yoga as Medicine for Pregnancy course, click here.
In our blog, we have highlighted the importance of recognizing and screening for postpartum depression. What relationships exist between a person's posture and depression in the postpartum period? Prior research reporting on four studies of posture (Riskind & Gotay, 1982) noted that subjects placed in a slumped physical posture appeared to develop helplessness more easily than those placed in an upright posture. These authors also stated that physical posture was a valuable clue for an observer who attempted to identify states of depression. Results of the fourth study include that "…subjects who were placed in a hunched, threatened physical posture verbally reported self-perceptions of greater stress than subjects who were placed in a relaxed position."
A recent study addressed depression, back pain and postural alignment in eighty women between 2 and 30 weeks postpartum. Depressive symptoms were measured with the Edinburgh Postnatal Depression Scale (EPDS). Pain scales included a visual analog scale (VAS) and the Nordic Musculoskeletal Questionnaire (NMQ while posture was assessed with visual observation. Findings of the study include that VAS pain scores were elevated in the women who were depressed. Back pain intensity and postpartum depression were also strongly associated. The authors suggest that back pain may be a risk factor for postpartum depression as well as a comorbidity. The article further states that physical therapists "…should be prepared to identify depressive symptoms as a comorbidity associated with posture changes and recurrent symptoms, signs of remission and recurrence that generate difficulties for treatment progression."
Can we look at this issue as a chicken and egg discussion, as in, is poor posture causativeto depression, or vice versa? And,if smiling has been determined to have the ability to improve happiness, can improved posture positively affect symptoms of depression? We know that postural dysfunction and pain can be a vicious cycle in our patients. Is screening for depression an equally important aspect of postural correction? Could postural taping, support, or re-training positively affect postpartum depression, and if so, should we be assessing and re-assessing our patients for depression as a means to document therapy benefits? The fun thing about reading research results is that the studies often lead to more questions, further hypotheses, and curiosity in relationship to how we interact with our patients. Can patients understand the relationship between postural correction and emotional health? Sounds like an opportunity for more research, and for dialoging with our patients!
If you are interested in learning more about postpartum health, click here for more information about the second course in our Peripartum series, Care of the Postpartum Patient. The next opportunities to take this class are June in Houston, and Chicago in September!
Wendy Sword, Professor in the School of Nursing at McMaster University, and her colleagues have recently published a study in which they looked at the relationship between mode of delivery and risk for post-partum depression. An interesting correlation that the authors found shows that having urinary incontinence in the first 6 weeks after childbirth doubles the risk for having post-partum depression. In McMaster University's post about this research, it is pointed out that up to 20% of new mothers experience post-partum depression, and this can interfere with the mother's self-care, with bonding between the mother and child, and with the care needed by the infant. Early detection and treatment of post-partum depression is critical.
In this research, 1900 new mothers were studied, up to 1/3 of them had c-sections as the mode of delivery. At 6 weeks post-partum, nearly 8% of the mothers had post-partum depression. The depression was not identified as being related to one mode of child delivery over another. The 5 strongest predictors of post-partum depression were identified as: 1) mother's age less than 25, 2) mother requiring hospital readmission, 3) non-initiation of breast-feeding, 4) good, fair, or poor self-reported health by the mother, and 5) urinary incontinence.
Dr. Sword recommends that providers ask patients about continence status early in the post-partum period, as patients may be embarrassed to bring it up, and also because incontinence is often dismissed as a common issue post-partum that will likely improve. When patients are referred to rehabilitation for continence issues, we often find that the symptoms have persisted for years, sometimes decades, unfortunately. During our marketing visits and education of the community, we can also encourage patient providers to send the patients to rehabilitation as early as possible. It is often at the 6 week appointment that the patient can be screened for such concerns, and this is when many of our referrers are comfortable sending a patient in for a check of the pelvic muscles.










































