Faculty member Jennafer Vande Vegte, MSPT, BCB-PMD, PRPC has written in to encourage us all to practice kindness and patience. A positive attitude can affect more than just your friends and family; your patients will benefit in so many ways as well!
 First a little personal story. Several years ago my daughter was going through a tough time and we worked with a child psychologist. He was a wonderful man who taught my husband and I so much about how to raise a challenging kiddo. The foundation of what we needed to learn was the power of positive. People need nine (or so) positive interactions to override a negative one. Poor kid was definitely at a deficit! So if she did something that needed correcting, we were to give her a chance at a "do over" where sometimes we had to coach her to choose a better action. After she got it right, we lavished praise on our little pumpkin. And would you believe, not only did all that positiveness make a difference for her, it made a difference for her parents too!
First a little personal story. Several years ago my daughter was going through a tough time and we worked with a child psychologist. He was a wonderful man who taught my husband and I so much about how to raise a challenging kiddo. The foundation of what we needed to learn was the power of positive. People need nine (or so) positive interactions to override a negative one. Poor kid was definitely at a deficit! So if she did something that needed correcting, we were to give her a chance at a "do over" where sometimes we had to coach her to choose a better action. After she got it right, we lavished praise on our little pumpkin. And would you believe, not only did all that positiveness make a difference for her, it made a difference for her parents too!
Now back to the clinical. Just about two years ago I had the privilege of teaching with Nari Clemons. We taught PF2B together. Nari said something during one of her lectures that revolutionized my PT practice. She challenged us in lab to find three positive things about our lab partner and share those things before recognizing any deficits. How many times do we get finished with an evaluation and sit down with a patient and list all the things we found that need correction or help, perhaps drawing on our Netter images to fully illustrate the parts of their body that are broken or need fixing.
So I changed things up a bit and started remarking about the positive things I found on exam. "Wow, your hips are really strong and stable." "You've got a really coordinated breathing pattern, that is going to work in your favor." "You're pelvic muscles are really strong." and then later drawing on those positives outline how we could use the patient's strengths to help them overcome their challenges. "Because you have a great breathing strategy we are going to use that to help your whole nervous system to relax which with help your pelvic floor relax," for example.
The results were shocking. Person after person told me how much it meant to them to leave feeling positive and hopeful. One delightful woman who I saw for a diastasis had amazing leg muscles and I told her so. When she returned she said, "I've felt so self conscious about my flabby belly, but this week all I could think about were my strong leg muscles. Thanks for telling me that."
We do know is that our attitudes and beliefs as providers influence not only our clinical management but patient outcomes as well. Darlow et. al. performed a comprehensive literature review looking at how attitudes and beliefs among health care providers affected outcomes in patients with low back pain and discovered, "There is strong evidence that health care provider beliefs about back pain are associated with the beliefs of their patients."
Why not use that truth to our advantage and be positive? Would love to hear about your experiences!
Join Jennafer at one of her upcoming courses, Pelvic Floor Level 2B - Trenton, NJ - February 24-26, 2017, Pelvic Floor Series Capstone - Arlington, VA - May 5-7, 2017, Pelvic Floor Series Capstone - Columbus, OH - August 18-20, 2017, and Pelvic Floor Series Capstone - Tampa, FL - December 2-4, 2016.
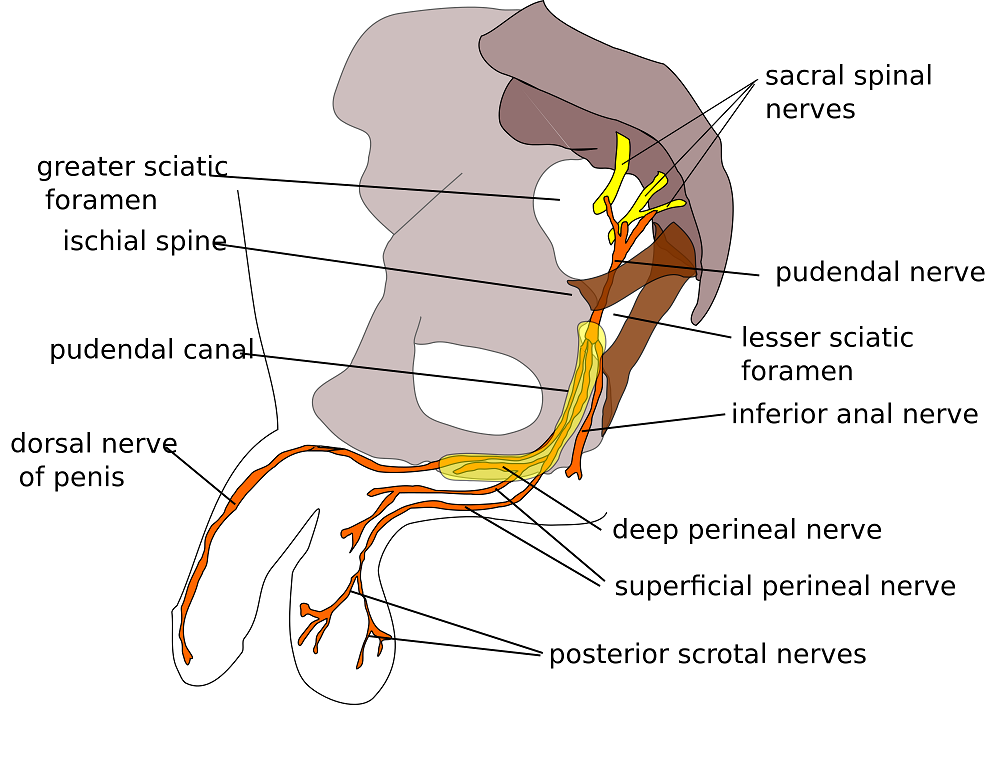
Herman & Wallace are pleased to announce a new course! Pudendal Neuralgia and Nerve Entrapment will be presented by Michelle Lyons in Freehold, NJ on June 17/18, 2017. We chatted with Michelle about this new course to hear her thoughts and get an overview of the contents
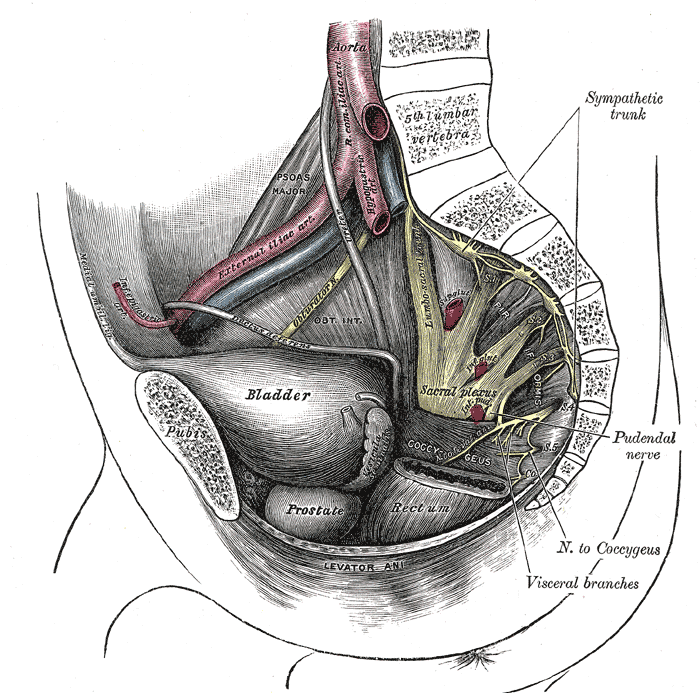 There are a number of courses which I teach for Herman & Wallace including Pelvic Floor Level 2A, my Male Oncology and Female Oncology and the The Athlete and the Pelvic Floor courses. They all have sections on pudendal dysfunction and it’s an area that participants always want more information on. There’s no other nerve that elicits the same interest, discussion and confusion! Nobody really talks about iliohypogastric or ulnar neuralgia with the same intensity as pudendal neuralgia, and no other nerve dysfunction provokes the same amount of controversy and mystery.
There are a number of courses which I teach for Herman & Wallace including Pelvic Floor Level 2A, my Male Oncology and Female Oncology and the The Athlete and the Pelvic Floor courses. They all have sections on pudendal dysfunction and it’s an area that participants always want more information on. There’s no other nerve that elicits the same interest, discussion and confusion! Nobody really talks about iliohypogastric or ulnar neuralgia with the same intensity as pudendal neuralgia, and no other nerve dysfunction provokes the same amount of controversy and mystery.
When I was approached about developing this course for the Institute, I jumped at the opportunity. For those who don’t know me, I really like to bring an integrative approach to my work, both clinically and educationally. I have experience and training in nutrition, coaching, yoga, Pilates and mindfulness as a therapeutic intervention and I think these fit really well alongside traditional pelvic rehab approaches. Manual therapy and bespoke exercise prescription will always be the bedrock of my approach, but sometimes our patients, especially those with chronic pain, need some extra support. I’m also a bit of an anatomy nerd, so the chance to delve deep into pelvic neuroanatomy and neurodynamics was too much to resist!
I think this is a Golden Age in pelvic health – there are so many great learning opportunities and resources available to us to help serve our patients better. Another area that I find fascinating to explore is the huge leap we have made in understanding neuroscience and the role of pain education when it comes to chronic pelvic pain. I’m a big fan of the work done by Moseley and Butler in Australia, and I love how authors like Hilton, Vandyken and Louw have transferred that to the world of pelvic pain in their book "Why Pelvic Pain Hurts". The language that we use is very important when discussing how the brain responds to chronic pain and the changes that occur with central sensitization. We never want our patients to feel as if we think their pain is ‘all in their heads’ but at the same time, we need to be able to incorporate strategies such as motor imagery and graded exposure and to demonstrate to our patients that"…it is important to acknowledge that chronic pain need not involve any structural pathology" (Aronoff 2016).
Those are some of the discussions we’ll be having in Freehold, NJ next June – I hope you’ll come and join the conversation!
"What Do We Know About the Pathophysiology of Chronic Pain? Implications for Treatment Considerations" Aronoff, GM Med Clin North Am. 2016 Jan;100(1):31-42
"Why Pelvic Pain Hurts: Neuroscience Education for Patients with Pelvic Pain" Hilton, Vandyken, Louw, International Spine and Pain Institute (May 28, 2014)
With menopause and the hormonal shifts that take place, some women suffer more than others with symptoms such as hot flashes. If you have ever been near someone during a hot flash, you know that this curious condition is more than feeling a little hot under the collar. During a hot flash, women will suddenly disrobe, wake from a deep sleep covered in sweat (so much so that they have to change the sheets!), or otherwise appear distressed and oftentimes suffer interference in whatever activity in which they were engaging. As we reported in an earlier post, women on average may have hot flashes for 5 years after the date of her last period. Some women (up to 1/3 in the referenced study) will report hot flashes for 10 or more years after menopause.
 Hot flashes and night sweats also significantly disrupt sleep, according to research by Baker and colleagues. Menopausal women with insomnia may also have higher levels of psychologic, somatic, vasomotor symptoms, and score lower on the Beck Depression Inventory, and sleep efficiency and duration scores. Poor sleep can be associated with morbidity such as hypertension, stroke, diabetes and depression, so interrupted sleep is more than an inconvenience, but potentially a serious health issue.
Hot flashes and night sweats also significantly disrupt sleep, according to research by Baker and colleagues. Menopausal women with insomnia may also have higher levels of psychologic, somatic, vasomotor symptoms, and score lower on the Beck Depression Inventory, and sleep efficiency and duration scores. Poor sleep can be associated with morbidity such as hypertension, stroke, diabetes and depression, so interrupted sleep is more than an inconvenience, but potentially a serious health issue.
A more recent study linked anxiety as a potential risk factor for menopausal hot flashes. In 233 women who are premenopausal at baseline and who were followed for at least a year after their final menstrual cycle, anxiety symptoms, hormone levels, hot flashes and other psychosocial variables were assessed. During the 14 year follow-up 72% of the women reported having moderate to severe hot flashes, and the researchers correlated somatic anxiety as a potential predictive association with anxiety. Somatic anxiety refers to the physical symptoms of anxiety, such as stomach ache, increased heart rate, sweating, muscle aches.
In order to help a woman support her wellness during menopausal transitions, being able to address somatic anxiety and conditions like hot flashes is imperative. Teaching skills such as breathing, relaxation training, meditation, or mindfulness may positively impact the anxiety, and therefore have the potential to reduce hot flashes and other adverse symptoms. Herman & Wallace's Menopause Rehabilitation and Symptom Management course is an excellent opportunity to learn some of these valuable skills.
Baker, F. C., Willoughby, A. R., Sassoon, S. A., Colrain, I. M., & de Zambotti, M. (2015). Insomnia in women approaching menopause: beyond perception. Psychoneuroendocrinology, 60, 96-104.
Freeman, E. W., & Sammel, M. D. (2016). Anxiety as a risk factor for menopausal hot flashes: evidence from the Penn Ovarian Aging cohort. Menopause, 23(9), 942-949.
Freeman, E. W., Sammel, M. D., & Sanders, R. J. (2014). Risk of long term hot flashes after natural menopause: Evidence from the Penn Ovarian Aging Cohort. Menopause (New York, NY), 21(9), 924.
The following comes from a male patient who wanted to share his story about finding care for his pelvic floor dysfunction. His story highlights the important role pelvic rehab practitioners can play, and why we need to continue training more therapists in this field.
I’m 65 year old male and I developed pudendal neuralgia and pelvic floor issues as a result of an accident about four years ago. Shortly after my accident I started to experience pain in my testicles and perineum. At the time, I did not think that one had anything to do with the other. I made an appointment with my urologist who did an ultrasound and assured me that there was nothing physically wrong. I don’t think my testicles quite believe that but mentally I felt relieved. But the pain persisted and started to spread. Now it was also in my groin and penis. I was also having problems with chronic constipation, urinary retention and erectile dysfunction. Since I did have back surgery years ago I started to suspect my low back was causing the problem. I made an appointment with a well-respected orthopedic surgeon in New York. While he gave me his analysis with regards to my back problems he clearly avoided addressing the pelvic issues. I left there feeling lost. Suffice it to say that over the course of the next couple of years I saw several other specialists who either skirted around the issue or told me that nothing was wrong. A couple of years passed but the pelvic issues just continued to get worse and worse. I started seeing a new primary care physician who indicated that perhaps the source of the pelvic pain was coming from the pudendal nerve and felt that physical therapy might help. She gave me a prescription for physical therapy to evaluate for pudendal nerve.
 Well, I have a diagnosis now so I start researching pudendal neuralgia and land on the Pudendal Hope website. Wow! What an eye opener that was. I’m reading the information on the website and it was like I had an epiphany. I realized that I was not going crazy and that Pudendal Neuralgia and pelvic pain are very real issues.
Well, I have a diagnosis now so I start researching pudendal neuralgia and land on the Pudendal Hope website. Wow! What an eye opener that was. I’m reading the information on the website and it was like I had an epiphany. I realized that I was not going crazy and that Pudendal Neuralgia and pelvic pain are very real issues.
OK, so where do I go from here? With prescription in hand I’ll make an appointment with a physical therapist that deals with pudendal neuralgia. Ha, I thought getting a diagnosis was tough but finding a physical therapist that treats pudendal neuralgia and pelvic issues was no easy task. To make things even more challenging, finding a physical therapist who treats men was even harder. I made a few calls and kept looking online without much success. Desperate to find a physical therapist that treats men, I sent an email off to a therapist in California asking if by some chance she could recommend a physical therapist here in New Jersey. As luck would have it, I got both a response and a referral. With that, I called Michelle Dela Rosa at Connect Physical Therapy. I had to wait about six weeks for an appointment but finally the day arrived. OK, so now, I had set my expectations. I’ll go for a few weeks of physical therapy, the pain will go away and it will be back to a normal life. Well, not so much… the journey and education were just getting started.
There are days when I am in so much pain that I ask myself if the pelvic therapy is really doing me any good. But then I reflect back to how things were before I started the therapy. Funny thing about pain… often times it makes us forget how things were in the past and shift our focus to the here and now. That being said, I quickly realize how much I have truly progressed since starting therapy.
So what have I learned? Well, the first thing is to understand the anatomy and how all the pelvic muscle groups and nerves are integrated. After all you can’t fix what you don’t know is broken. Therapy has certainly helped educate me in that respect; I’ve learned the importance of proper breathing and strengthen the core muscles. I know that when I was in pain I would tighten up the pelvic muscles and hold my breath which would only make things worse, as the muscles would get into a knot, and make it even more difficult to get relief. I’ve learned a whole new set of exercises that I now have in my arsenal to help fight this battle. To help me deal with the chronic constipation I’ve learned how to massage my abdomen to help move things along. For those folks dealing with chronic constipation, well, we all know what happens when we push just a little too hard… flare time! I could go on and on. I learned to use tools, such as the TheraWand, to help break the tension for those internal pelvic muscles. Pelvic therapy has taught me the importance and benefits of the proper use of cold packs, glides, exercise, breathing, relaxing the pelvic floor and on and on and on.
I was a bit embarrassed getting started but the prospect of relieving some of the pelvic pain and the professionalism of my therapist quickly turned my embarrassment into a non-issue.
I want to express my thanks and gratitude to all those physical therapists who have the courage and vision to take on this problem. You are truly making a difference in the lives of the people you are helping.
The following testimonial comes to us from Karen Dys, PTA. Karen recently attended the Care of the Pregnant Patient course, and she was inspired to send in the following review. Thanks for your contribution, Karen!
 I have been working as a physical therapist assistant for 11 years and worked in a variety of settings. In the past two year I have become more focused on pelvic floor rehabilitation. During that time frame I have had a handful of pregnancy patient including being a pregnant woman myself. Since taking this course, my mind has been opened up of how I can treat my patients and educate them for their best future outcomes. I also can see now how I would have benefited myself if I knew some of these techniques that I’ve now learned. With knowing with my personal story and that my PT could have helped me more with avoiding bed rest and staying active longer with pregnancy, it has become my goal now to treat my pregnant patients differently. I am thankful for Herman and Wallace courses to gain these wonderful techniques to reach out and help so many people.
I have been working as a physical therapist assistant for 11 years and worked in a variety of settings. In the past two year I have become more focused on pelvic floor rehabilitation. During that time frame I have had a handful of pregnancy patient including being a pregnant woman myself. Since taking this course, my mind has been opened up of how I can treat my patients and educate them for their best future outcomes. I also can see now how I would have benefited myself if I knew some of these techniques that I’ve now learned. With knowing with my personal story and that my PT could have helped me more with avoiding bed rest and staying active longer with pregnancy, it has become my goal now to treat my pregnant patients differently. I am thankful for Herman and Wallace courses to gain these wonderful techniques to reach out and help so many people.
Within the first few moments of meeting the teacher at a continue education class I can tell if is going to be a good class or not. This course started out great with a very friendly and kind person. Sarah’s compassion and knowledge brightly shined throughout the weekend of teaching. It was very refreshing having a teacher who also has experienced some of the same problems are patients go through. It gave it a good personal perspective of how we can affect our patient outcomes.
One thing that I really appreciated at this course was the comfort level felt during the entire weekend. Right from the beginning Sarah made it clear that no question was stupid to ask. She explained that we are all at different learning stages in our career and that we are working together to gain this knowledge to be better therapists. I really appreciated hearing that and I know it made some of the new pelvic floor therapists feel more comfortable as well. I enjoyed having different labs throughout the weekend to practice these new techniques with new therapists of different educational levels. Sometimes I attend courses being more confused on techniques because the teacher, assistant or other course mates don’t have the time or knowledge to explain in further detail. At any of my Herman and Wallace courses I have attended, especially this one, I have not felt that way.
So I attended this wonderful class and now what? Well during the class I was thinking of my pregnant friends who are expecting multiples and how I can help them with their already felt extra swelling and low back pain. I also was thinking of some of my post-partum pelvic floor patients and how if I would have known some of this information sooner I could have impacted their pregnancy. Some things I would have changed were compression stock wear, abdominal binder/ brace wear, labor positioning techniques and strengthening more with education for post-partum phase. So now I have brought back to my company more knowledge of how to evaluate, assess more correctly and treat pregnancy patients. I have led a in-service for my coworkers who are primarily orthopedic based . They had a good take away of how to help patients with orthopedic complaints of pain who also happen to be pregnant.
I am thankful for this course I attended and look forward to making it a regular event I attend. Herman and Wallace courses never disappoint. Thank you.
Karen R Dys, PTA
My little boy has a t-shirt with a potato telling french fries, “I am your father,” to which the french fries cry, “NO!!!!” The Star Wars spoof makes me laugh, but sometimes the struggle is real. Testicular cancer and the toxic remedies for it can potentially prevent young men from having a successful reproductive life. Survivors of the cancer may one day have to tell their children they are adopted or came from a sperm donor. With the advances in technology and research, however, testicular cancer survivors have a greater chance for their own sperm to be spared or even produced naturally years later to create their offspring.
 Vakalopoulos et al. (2015) discussed the impact cancer and the related treatments have on fertility of males. Better survival rates for oncology patients have made preservation of reproductive means more imperative for men. Testicular cancer represents 5% of male urologic cancers, disturbing spermatogenesis and impairing fertility. Chemotherapy, radiotherapy, and surgery can all have gonadotoxic effects in men. Thankfully, only 1 in 5000 men die from testicular cancer now with advanced treatments, but fertility does become a long term factor for survivors. This paper showed chemotherapy combined with radiotherapy was most detrimental to sperm than either treatment alone. Gonadal shielding and moving the testes out of the way to target the malignant cells can help decrease the deleterious effects of cancer treatments. Radiotherapy, however, has been shown to damage sperm up to 2 years after recovery of spermatogenesis. Regarding surgery, radical unilateral orchiectomy is the standard for testicular tumors, and within the first few months, a 50% decrease in sperm concentration occurs, and 10% of patients become azoospermic. On a more encouraging note, after receiving Hematopoietic Stem Cell Transplantation, recovery of sperm in the ejaculate was noted in 33% of patients after 1 year and 80% of patients after 7 years.
Vakalopoulos et al. (2015) discussed the impact cancer and the related treatments have on fertility of males. Better survival rates for oncology patients have made preservation of reproductive means more imperative for men. Testicular cancer represents 5% of male urologic cancers, disturbing spermatogenesis and impairing fertility. Chemotherapy, radiotherapy, and surgery can all have gonadotoxic effects in men. Thankfully, only 1 in 5000 men die from testicular cancer now with advanced treatments, but fertility does become a long term factor for survivors. This paper showed chemotherapy combined with radiotherapy was most detrimental to sperm than either treatment alone. Gonadal shielding and moving the testes out of the way to target the malignant cells can help decrease the deleterious effects of cancer treatments. Radiotherapy, however, has been shown to damage sperm up to 2 years after recovery of spermatogenesis. Regarding surgery, radical unilateral orchiectomy is the standard for testicular tumors, and within the first few months, a 50% decrease in sperm concentration occurs, and 10% of patients become azoospermic. On a more encouraging note, after receiving Hematopoietic Stem Cell Transplantation, recovery of sperm in the ejaculate was noted in 33% of patients after 1 year and 80% of patients after 7 years.
Regardless of advancements in decreasing toxicity of cancer treatments and being minimally invasive with surgery, the best guarantee for preservation of sperm is cryopreservation.
A study collecting baseline data for semen quality of cancer patients prior to any gonadotoxic treatment was performed by Auger et al. (2016). Less than 60% of the testicular cancer patients had normal sperm production prior to treatment. The study also looked at patients with Hodgkin’s disease, non-Hodgkin’s Lymphoma, Leukemia, sarcoma, Behcet’s disease, brain tumor, and Multiple Sclerosis. The motility of sperm after freezing (cryopreservation) of the cancer patients was less than half of the healthy sperm donor control group. Intra Cytoplasmic Sperm Injection (ICSI) was shown to provide the best chance of paternity for men, and the authors conclude this as a necessary step in case men do not regain any spermatogenesis after cancer treatment.
There is no perfect circumstance when it comes to cancer. Survival is the primary goal, and then quality of life becomes the “problem,” particularly when it comes to fulfilling dreams of having a family. The toxic cancer treatments are improving but cannot guarantee return of spermatogenesis. Depending on the sperm integrity prior to getting treatment, cryopreservation success can vary but is the most highly recommended step to preserving fertility. In the end, a fresh or frozen spud can still make french fries.
Herman & Wallace has two great courses which can give you the tools needed to help assess and treat male patients who suffer from cancer-related dysfunctions. Consider Oncology and the Male Pelvic Floor: Male Reproductive, Bladder, and Colorectal Cancers or Post-Prostatectomy Patient Rehabilitation for your next continuing education courses.
Vakalopoulos, I., Dimou, P., Anagnostou, I., Zeginiadou T. (2015). Impact of cancer and cancer treatment on male fertility. Hormones. 14(4):579-89. DOI: 10.14310/horm.2002.1620
Auger, J., Sermondade, N., & Eustache, F. (2016). Semen quality of 4480 young cancer and systemic disease patients: baseline data and clinical considerations. Basic and Clinical Andrology, 26, 3. http://doi.org/10.1186/s12610-016-0031-x
My job as a pelvic floor therapist is rewarding and challenging in so many ways. I have to say that one of my favorite "job duties" is differential diagnosis. Some days I feel like a detective, hunting down and piecing together important clues that join like the pieces of a puzzle and reveal the mystery of the root of a particular patient's problem. When I can accurately pinpoint the cause of someone's pain, then I can both offer hope and plan a road to healing.
 Recently a lovely young woman came into my office with the diagnosis of dyspareunia. As you may know dyspareunia means painful penetration and is somewhat akin to getting a script that says "lower back pain." As a therapist you still have to use your skills to determine the cause of the pain and develop an appropriate treatment plan.
Recently a lovely young woman came into my office with the diagnosis of dyspareunia. As you may know dyspareunia means painful penetration and is somewhat akin to getting a script that says "lower back pain." As a therapist you still have to use your skills to determine the cause of the pain and develop an appropriate treatment plan.
My patient relayed that she was 6 months post partum with her first child. She was nursing. Her labor and delivery were unremarkable but she tore a bit during the delivery. She had tried to have intercourse with her husband a few times. It was painful and she thought she needed more time to heal but the pain was not changing. She was a 0 on the Marinoff scare. She was convinced that her scar was restricted. "Oh Goodie," I thought. "I love working with scars!" But I said to her, "Well, we will certainly check your scar mobility but we will also look at the nerves and muscles and skin in that area and test each as a potential pain source, while also completing a musculoskeletal assessment of the rest of you."
Her "external" exam was unremarkable except for adductor and abdominal muscle overactivity. Her internal exam actually revealed excellent scar healing and mobility. There was significant erythemia around the vestibule and a cotton swab test was positive for pain in several areas. There was also significant muscle overactivity in the bulbospongiosis, urethrovaginal sphincter and pubococcygeus muscles. Also her vaginal pH was a 7 (it should normally be a 4, this could indicate low vaginal estrogen). I gave her the diagnosis of provoked vestibulodynia with vaginismus. Her scar was not the problem after all.
Initially for homework she removed all vulvar irritants, talked to her doctor about trying a small amount of vaginal estrogen cream, and worked on awareness of her tendency to clench her abdominal, adductor, and pelvic floor muscles followed by focused relaxation and deep breathing. In the clinic I performed biofeedback for down training, manual therapy to the involved muscles, and instructed her in a dilator program for home. This particular patient did beautifully and her symptoms resolved quite quickly. She sent me a very satisfied email from a weekend holiday with her husband and daughter.
Although this case was fairly straightforward, it is a great example of how differential diagnosis is imperative to deciding and implementing an effective treatment plan for our patients. In Herman & Wallace courses you will gain confidence in your evaluation skills and learn evidence based treatment processes that will enable you to be more confident in your care of both straightforward and complex pelvic pain cases. Hope to see you in class!
We are all familiar with the old saying, “You are what you eat.” A functional medicine lecture I attended recently at the Cleveland Clinic explained how chronic pain can be a result of how the body fails to process the foods we eat. Patients who just don’t seem to get better despite our skilled intervention make us wonder if something systemic is fueling inflammation. Even symptoms of vulvodynia, an idiopathic dysfunction affecting 4-16% of women, have been shown to correlate to diet.
In a single case study of a 28 year old female athlete in Integrative Medicine (Drummond et al., 2016), vulvodynia and irritable bowel syndrome (IBS) were addressed with an elimination diet. After being treated by a pelvic floor specialist for 7 months for vulvodynia, the patient was referred out for a nutrition consultation. Physical therapy was continued during the vegetarian elimination diet. In the patient’s first follow up 2 weeks after starting eliminating meat, dairy, soy, grains, peanuts, corn, sugar/artificial sweeteners, she no longer had vulvodynia. The nutrition specialist had her add specific foods every 2 weeks and watched for symptoms. Soy, goat dairy, and gluten all caused flare ups of her vulvodynia throughout the process. Eliminating those items and supplementing with magnesium, vitamin D3, probiotics, vitamin B12, and omega-3 allowed the patient to be symptom free of both vulvodynia and IBS for 6 months post-treatment.
 On the more scientific end of research, Vicki Ratner published a commentary called “Mast cell activitation syndrome” in 2015. She described how mast cells appear close to blood vessels and nerves, and they release inflammatory mediators when degranulated; however, mast cell activation syndrome (MCAS) involves mast cells that do not get degranulated properly and affect specific organs like the bladder. She proposed measuring the number of mast cells and inflammatory mediators in urine for more expedient diagnosis of interstitial cystisis and bladder pain syndrome.
On the more scientific end of research, Vicki Ratner published a commentary called “Mast cell activitation syndrome” in 2015. She described how mast cells appear close to blood vessels and nerves, and they release inflammatory mediators when degranulated; however, mast cell activation syndrome (MCAS) involves mast cells that do not get degranulated properly and affect specific organs like the bladder. She proposed measuring the number of mast cells and inflammatory mediators in urine for more expedient diagnosis of interstitial cystisis and bladder pain syndrome.
Sigrid Regauer’s correspondence to Ratner’s article followed in 2016 relating MCAS to bladder pain syndrome (BPS), interstitial cystitis (IC), and vulvodynia. He described vulvodynia as a pain syndrome with excessive mast cells and sensory nerve hyperinnervation, often found with BPS and IC. The vulvodynia patients had mast cell hyperplasia, most of which were degranulated, and 70% of the patients had comorbidities due to mast cell activation such as food allergies, histamine intolerance, infections, and fibromyalgia.
Considering the association between mast cells and acute inflammatory responses and how mast cells release proinflammatory mediators, it makes sense that dysfunctions such as vulvodynia as well as IC and BPS can result from an excessive amount and dysfunctional granulation of mast cells. Enhanced activation of mast cells causes histamine release, stimulating peripheral pain neurotransmitters (Fariello & Moldwin 2015). If medication and therapy do not solve a patient’s pain, perhaps eliminating the consumption of inflammatory foods could positively affect the body on a cellular level and relieve irritating symptoms of vulvodynia. Pardon the parody, but patients on the brink of being “insane in the brain” from vulvodynia will likely try anything to resolve being “inflamed in the membrane.”
Drummond, J., Ford, D., Daniel, S., & Meyerink, T. (2016). Vulvodynia and Irritable Bowel Syndrome Treated With an Elimination Diet: A Case Report.Integrative Medicine: A Clinician’s Journal, 15(4), 42–47.
Ratner, V. (2015). Mast cell activation syndrome. Translational Andrology and Urology, 4(5), 587–588. http://doi.org/10.3978/j.issn.2223-4683.2015.09.03
Regauer, S. (2016). Mast cell activation syndrome in pain syndromes bladder pain syndrome/interstitial cystitis and vulvodynia. Translational Andrology and Urology, 5(3), 396–397. http://doi.org/10.21037/tau.2016.03.12
Fariello, J. Y., & Moldwin, R. M. (2015). Similarities between interstitial cystitis/bladder pain syndrome and vulvodynia: implications for patient management. Translational Andrology and Urology, 4(6), 643–652. http://doi.org/10.3978/j.issn.2223-4683.2015.10.09
Help others by helping ourselves
As pelvic rehabilitation practitioners, we have all been there, looking ahead to see what patients are on our schedules and recognizing that several will require immense energy from us… all afternoon! Then we prepare ourselves, hoping we have enough stamina to get through, and do a good job to help meet the needs of these patients. Then we still have to go home, spend time with our families, do chores, run errands, and have endless endurance. This can happen day after day. Naturally, as rehabilitation practitioners, we are helpers and problems solvers. However, this requires that we work in emotionally demanding situations. Often in healthcare, we experience burnout. We endure prolonged stress and/or frustration resulting in exhaustion of physical and/or emotional strength and lack of motivation. Do we have any vitality left for ourselves and our loved ones? How can we help ourselves do a good job with our patients, but to also honor our own needs for our energy?
 How do we as health care practitioners’ prevent burnout?
How do we as health care practitioners’ prevent burnout?
Ever hear of “mindfulness” ... I am being facetious. The last several years we have been hearing a lot about “mindfulness” (behavioral therapy or mindfulness-based stress reduction) and its positive effects in helping patients cope with chronic pain conditions. Mindfulness is defined as “the practice of maintaining a nonjudgmental state of heightened or complete awareness of one's thoughts, emotions, or experiences on a moment-to-moment basis,” according to Merriam-Webster’s Dictionary. One can practice mindfulness in many forms. Examples of mindfulness-based practice include, body scans, progressive relaxation, meditation, or mindful movement. Many of us pelvic rehabilitation providers teach our patients with pelvic pain some form of mindfulness in clinic, at home, or both, to help them holistically manage their pain. Whether it is as simple as diaphragmatic breathing, awareness of toileting schedules/behavior, or actual guided practices for their home exercise program, we are teaching mindfulness behavioral therapy daily.
Why don’t we practice what we preach?
As working professionals, we are stressed, tired, our schedules too full, and we feel pain too, right? Mindfulness behavioral therapy interventions are often used in health care to manage pain, reduce stress, and control anxiety. Isn’t the goal of using such interventions to improve health, wellness, and quality of life? Mindfulness training for healthcare providers can reduce burnout by decreasing emotional exhaustion, depersonalization, and increasing sense of personal accomplishment. Additionally, it can improve mood, empathy for patients, and communication.1 All of these improvements, leads to improved patient satisfaction.
Let’s take what we teach our patients every day and start applying it to ourselves. An informal way to integrate mindfulness is by building it into your day. Such as when washing hands in between patients, or before you walk into the room to greet the patient. However, sometimes we have a need for a tangible strategy to combat stress and the desire to be guided by an expert with this strategy.2 I think one of the easiest ways to begin practicing mindfulness is to try a meditation application (app) on a smart phone or home computer. Meditation is one of the most common or popular ways to practice mindfulness and is often a nice starting point to try meditation for yourself or to suggest to a motivated patient. Many popular guided meditation apps include Headspace, Insight Timer, and Calm, just to name a few. Generally, these guided meditation apps have free versions and paid upgrades. Challenge yourself to complete a 10-minute guided meditation app, daily, for three weeks, and see how you feel. It takes three weeks to make a new habit. Hopefully, guided meditation will be a new habit to help you be present with your patients and improve your awareness and energy. After all, how can we help others heal, if we can’t help ourselves?
To learn more about ways, you as a professional can help yourself or your patients with meditation, consider attending Meditation for Patients and Providers.
1)Krasner, M.S., Epstein, R.M., Beckman, H., Suchman, A.L., Chapman, B., Mooney C.J., et al. (2009). Association of an educational program in mindful communication with burnout, empathy, and attitudes among primary care physicians. JAMA 302(12):1284–93.
2)Willgens, A. M., Craig, S., DeLuca, M., DeSanto, C., Forenza, A., Kenton, T., ... & Yakimec, G. (2016). Physical Therapists' Perceptions of Mindfulness for Stress Reduction: An Exploratory Study. Journal of Physical Therapy Education, 30(2).
Jennafer Vande Vegte, PT, BCB-PMD, PRPC is a H&W faculty member and one of the developers of the advanced Pelvic Floor Capstone course. In this guest post, she reflects on her own clinical and personal experience that informed her work on this advanced course, and her approach with patients.
 Most days I feel like I am on a journey. Some days I make big strides forward, other days I might fall back. But I am always learning, and eventually I hope to grow. I think it is much the same for our patients. And also for ourselves.
Most days I feel like I am on a journey. Some days I make big strides forward, other days I might fall back. But I am always learning, and eventually I hope to grow. I think it is much the same for our patients. And also for ourselves.
My youngest daughter was diagnosed with eczema, allergies (food and others) and asthma at an early age. In my hubris I felt if I could learn all I could about what was going on in her body I could "fix" her. So began a journey that took me outside the realm of traditional medicine into holistic care. I learned so much! My daughter got a lot healthier. The rest of my family got a lot healthier. I got healthier too. And I began to recognize patients in my practice that needed more holistic care. Guess what, they got healthier too.
When she was in first grade she was diagnosed with ADHD. I retraced the steps of my previous journey that had helped her so much with her allergies, eczema and asthma. But ADHD proved to be resistant to diet , supplements, and homeopathy. We visited an OT and got some good suggestions. A family therapist helped us a ton as parents, but I'm not sure how much he helped my daughter. We tried Ritalin to no avail. Energy therapy and essential oils followed before I finally made an appointment with a ADHD child specialist MD. We will see where that step leads. Why
Why am I telling you all this you may ask? Because I realized that my journey with my daughter is very much like our journey walking next to our patients with chronic pain. They/we may try so many things trying to find the "fix" to make their pain go away. As we grow on our own life journeys and experiences and we add quality clinical tools to our toolboxes we very well may be able to help more people experience freedom from pain, improvements in function, and meeting their goals. But there will be always still be those that we feel like we didn't help. Don't despair dear friends. Every person we have come in contact with in the quest to better equip and understand my daughter's mental and physical health has been a wealth of information, inspiration, and resources. Some things I learned some years ago (essential oils for example) and only now am putting into practice. I wasn't ready before but I am now! I realized that there is a similar dynamic for our patients. We may help them take just one step forward. We may walk a whole journey to healing beside them, or we may never know what the impact of our treatment had on them. But in the end we both end up exactly where we needed to be.
Insignia Health developed the PAM (Patient Activation Measure) Survey (http://www.insigniahealth.com/products/pam-survey) to help heath care providers determine where along the pathway of activation of self care a patient falls. What is interesting about the tool is that a single point increase correlates to a 2% decrease in hospitalization and a 2% increase in medication adherence. The science behind the PAM shows that helping our patients to move forward just one step can have a profound influence on their health. The trick is meeting them where they are at.
Pelvic Floor Capstone was a joy to develop with Nari Clemons and Allison Arial. Our goal was to equip you to take one more step in your learning journey in pelvic health. We delve into intense topics like endocrine disorders, pelvic surgery, gynecological cancer, nutrition and pharmacology. Labs are focused on evaluating and treating myofascial restrictions utilizing a gentle, indirect three dimensional system that invites the brain to reconnect with connective tissue in a safe way for powerful change. We would love to see you at Capstone and hear your stories later on how our time together empowered you to help your patients take one more step.
By accepting you will be accessing a service provided by a third-party external to https://hermanwallace.com/










































