After menopause, more than half of women may have vulvovaginal symptoms that can impact their lifestyle, emotional well-being and sexual health. What's more, the symptoms tend to co-exist with issues such as prolapse, urinary and/or bowel problems. But unfortunately many women aren't getting the help they need, despite a growing body of evidence that skilled pelvic rehab interventions are effective in the management of bladder/bowel dysfunctions, POP, sexual health issues and pelvic pain.
 Vaginal dryness, hot flashes, night sweats, disrupted sleep, and weight gain have been listed as the top five symptoms experienced by postmenopausal women in North America and Europe, according to a study by Minkin et al 2015, and they also concluded ‘The impact of postmenopausal symptoms on relationships is greater in women from countries where symptoms are more prevalent.’
Vaginal dryness, hot flashes, night sweats, disrupted sleep, and weight gain have been listed as the top five symptoms experienced by postmenopausal women in North America and Europe, according to a study by Minkin et al 2015, and they also concluded ‘The impact of postmenopausal symptoms on relationships is greater in women from countries where symptoms are more prevalent.’
Between 17% and 45% of postmenopausal women say they find sex painful, a condition referred to medically as dyspareunia. Vaginal thinning and dryness are the most common cause of dyspareunia in women over age 50. However pain during sex can also result from vulvodynia (chronic pain in the vulva, or external genitals) and a number of other causes not specifically associated with menopause or aging, particularly orthopaedic dysfunction, which the pelvic physical therapist is in an ideal position to screen for.
According to the North America Menopause Society, ‘…beyond the immediate effects of the pain itself, pain during sex (or simply fear or anticipation of pain during sex) can trigger performance anxiety or future arousal problems in some women. Worry over whether pain will come back can diminish lubrication or cause involuntary—and painful—tightening of the vaginal muscles, called vaginismus. The result can be a vicious circle, again highlighting how intertwined sexual problems can become.’
The research has demonstrated that the optimal strategy for post-menopausal stress incontinence is a combination of local hormonal treatment and pelvic floor muscle training – the strategy of combining the two approaches has been shown to be superior to either approach used individually (Castellani et al 2015, Capobianco et al 2012) and similar conclusions can be drawn for promoting sexual health peri- and post-menopausally.
The pelvic rehab specialist may be called upon to screen for orthopaedic dysfunction in the spine, hips or pelvis, to discuss sexual ergonomics such as positioning or the use of lubricant as well as providing information and education about sexual health before, during and after menopause.
To learn more about sexual health and pelvic floor function/dysfunction at menopause, join me in Atlanta in March for Menopause: A Rehab Approach!
Prevalence of postmenopausal symptoms in North America and Europe, Minkin, Mary Jane MD, NCMP1; Reiter, Suzanne RNC, NP, MM, MSN2; Maamari, Ricardo MD, NCMP3, Menopause:November 2015 - Volume 22 - Issue 11 - p 1231–1238
Low-Dose Intravaginal Estriol and Pelvic Floor Rehabilitation in Post-Menopausal Stress Urinary Incontinence, Castellani D. · Saldutto P. · Galica V. · Pace G. · Biferi D. · Paradiso Galatioto G. · Vicentini C., Urol Int 2015;95:417-421
Unfortunately one of the most common things we hear in pelvic rehab is “I hope you can help me, you’re my last hope.” In severe cases, this translates to the patient having little hope of surviving their life with pelvic pain. In severe but not necessarily life-threatening cases, being a patient’s last hope can also mean “please help me have sex in my relationship or my partner is going to leave me.” This situation places a lot of pressure on the patient and also on the therapist. How long did it take this patient to find her way to pelvic rehab? Research tells us that most women have been through multiple physicians, under- or misdiagnosed, and that many have failed attempts at intervention with medications or procedures.
 It’s clear to women that they are being judged when they go to medical appointments complaining of pelvic pain or pain with intercourse. Although it seems really old school to hear that a provider said “It’s all in your head.” or “How much do you like your partner?” or “Well, you’re getting older, sex isn’t that important.” these dismissive phrases are still used. A study by Nguyen et al., 2013 reported that women who reported chronic pain were more likely to perceive being stereotyped by doctors and others. Interestingly, among the group of women who had chronic vulvar pain, the women who sought care for their condition reported feeling more stigmatized. Because the support a woman perceives may influence her willingness to seek out help for chronic vulvar pain, we need to keep educating our peers, the public, and the providers about the real challenges women face, and the power of rehabilitation in overcoming those challenges.
It’s clear to women that they are being judged when they go to medical appointments complaining of pelvic pain or pain with intercourse. Although it seems really old school to hear that a provider said “It’s all in your head.” or “How much do you like your partner?” or “Well, you’re getting older, sex isn’t that important.” these dismissive phrases are still used. A study by Nguyen et al., 2013 reported that women who reported chronic pain were more likely to perceive being stereotyped by doctors and others. Interestingly, among the group of women who had chronic vulvar pain, the women who sought care for their condition reported feeling more stigmatized. Because the support a woman perceives may influence her willingness to seek out help for chronic vulvar pain, we need to keep educating our peers, the public, and the providers about the real challenges women face, and the power of rehabilitation in overcoming those challenges.
Vulvodynia is a common pelvic pain condition, and one that typically is associated with painful intercourse, or dyspareunia. (Arnold et al., 2006) It's estimated that by the age of 40, as many as 8% of women will have or have had a diagnosis of vulvodynia (Harlow et al., 2014), and this is clearly a significant quality of life issue.
Physical therapy has been shown to be successful in treating vulvar pain and pain with intercourse, including as part of a multidisciplinary approach. (Brotto et al., 2015) That's why Herman & Wallace is so eager to help empower more therapists to help patients live a life free of vulvar pain and dyspareunia. You can learn more about our courses and other resources at https://www.hermanwallace.com/continuing-education-courses.
Arnold, L. D., Bachmann, G. A., Kelly, S., Rosen, R., & Rhoads, G. G. (2006). Vulvodynia: characteristics and associations with co-morbidities and quality of life. Obstetrics and gynecology, 107(3), 617.
Brotto, L. A., Yong, P., Smith, K. B., & Sadownik, L. A. (2015). Impact of a multidisciplinary vulvodynia program on sexual functioning and dyspareunia. The journal of sexual medicine, 12(1), 238-247.
Harlow, B. L., Kunitz, C. G., Nguyen, R. H., Rydell, S. A., Turner, R. M., & MacLehose, R. F. (2014). Prevalence of symptoms consistent with a diagnosis of vulvodynia: population-based estimates from 2 geographic regions. American journal of obstetrics and gynecology, 210(1), 40-e1.
Nguyen, R. H., Turner, R. M., Rydell, S. A., MacLehose, R. F., & Harlow, B. L. (2013). Perceived stereotyping and seeking care for chronic vulvar pain. Pain Medicine, 14(10), 1461-1467.
The following post comes to us from long-time faculty member Dawn Sandalcidi PT, RCMT, BCB-PMD! Dawn is a figurehead in the world of pediatric pelvic floor, she teaches Pediatric Incontinence and Pelvic Floor Dysfunction (available three times in 2016) and she just completed the 2nd edition of the Pediatric Pelvic Floor Manual!! Today Dawn is sharing her insights an urotherapy for pediatric patients.
 If you read any papers on pediatric bowel and bladder dysfunction you will often come across the word "urotherapy". It is by definition a conservative based management based program used to treat lower urinary tract (LUT) dysfunction using a variety of health care professionals including the physician, Physical Therapists, Occupational Therapists and Registered Nurses.
If you read any papers on pediatric bowel and bladder dysfunction you will often come across the word "urotherapy". It is by definition a conservative based management based program used to treat lower urinary tract (LUT) dysfunction using a variety of health care professionals including the physician, Physical Therapists, Occupational Therapists and Registered Nurses.
Basic urotherapy includes education on the anatomy and function of the LUT, behavior modifications including fluid intake, timed or scheduled voids, toilet postures and avoidance of holding maneuvers, diet, bladder irritants and constipation. This needs to be tailored to the patients’ needs. For example a child with an underactive bladder needs to learn how to sense urge and listen to their body and a child who postpones a void needs to be on a voiding schedule. Urotherapy alone can be helpful however a recent study demonstrated a statistically significant improvement in uroflow, pelvic floor muscle electromyography activity during a void, urinary urgency, daytime wetting and reduced post void residual (PVR) in those patients who received pelvic floor muscle training as compared to Urotherapy alone. This is great news for all of us who are qualified to teach pelvic floor muscle exercise!
The International Children’s Continence Society (ICCS) has now expanded the definition of Urotherapy to include Specific Urotherapy. This includes biofeedback of the pelvic floor muscles by a trained therapist who is able to teach the child how to alter pelvic floor muscle activity specifically to void. It also includes neuromodulation for many types of lower urinary tract dysfunction but most commonly with overactive bladder and neurogenic bladder. Cognitive behavioral therapy and psychotherapy are always important to assess (see blog post on psychological effects of bowel and bladder dysfunction).
It truly does take a village to help this kiddos and I am honored to be a team player!
To learn more about pediatric incontinence and pelvic floor rehabilitation, join Dawn Sandalcidi at one of her courses this year! Details at the following links:
Pediatric Incontinence - Augusta, GA - Apr 16, 2016 - Apr 17, 2016
Pediatric Incontinence - Torrance, CA - Jun 11, 2016 - Jun 12, 2016
Pediatric Incontinence - Waterford, CT - Sep 17, 2016 - Sep 18, 2016
Chang SJ, Laecke EV, Bauer, SB, von Gontard A, Bagli,D, Bower WF,Renson C, Kawauchi A, Yang SS-D. Treatment of daytime urinary incontinence: a standardization document from the international children's continence society. Neurourol Urodyn 2015;Oct 16. doi:10.1002/nau.22911
Ladi Seyedian SS, Sharifi-Rad L, Ebadi M, Kajbafzadeh AM. Combined functional pelvic floor muscle exercise with swiss ball and Urotherapy for management of dysfunctional voiding in children: a randomized controlled trial. Eur J Pediatr.2014 Oct;173(10):1347-53. I.J.N. Koppen, A. von Gontard, J. Chase, C.S. Cooper, C.S. Rittig, S.B. Bauer, Y. Homsy, S.S. Yang, M.A. Benninga. Management of functional nonretentive fecal incontinence in children: recommendations from the International Children’s Continence Society. J of Ped Urol (2015)
Koppen IJ, Di Lorenzo C, Saps M, Dinning PG, Yacob D, Levitt MA, Benninga MA. .Childhood constipation: finally something is moving! Expert Rev Gastroenterol Hepatol. 2015 Oct 14:1-15.
Herman & Wallace Pelvic Rehabilitation Institute faculty member, Ginger Garner PT, L/ATC, PYT, will be giving 2 lectures at this year’s annual Montreal International Symposium for Therapeutic Yoga, or MISTY for short, in Montreal, Quebec. The first is a 2-hour lecture titled, Vocal Liberation, and the second is a 4-hour lecture titled, Hip Preservation: Yoga Reconsidered, Visit http://www.homyogaevents.com to learn more. Read below as Ginger shares why the voice is a linking science.
The Voice as a Linking Science for Clinical and Business Efficacy
 Your voice can be the key to your success. Forbes magazine’s #3 habit in an article, Five Habits of Highly Effective Communicators, is “Find your own voice.” London’s think tank Tomorrow’s Company declares in a recent report on efficacy in business leadership, “Having a voice really matters for employees today.” The director of the Involvement and Participation Association (IPA) and vice-chair of the London-based MadLeod Review on employee engagement says, “Voice is extremely important because there are many changing business concepts and one of the essential ones is trust. Our voice is one of the things we really need to change old management paradigms and build trust in an organization.”
Your voice can be the key to your success. Forbes magazine’s #3 habit in an article, Five Habits of Highly Effective Communicators, is “Find your own voice.” London’s think tank Tomorrow’s Company declares in a recent report on efficacy in business leadership, “Having a voice really matters for employees today.” The director of the Involvement and Participation Association (IPA) and vice-chair of the London-based MadLeod Review on employee engagement says, “Voice is extremely important because there are many changing business concepts and one of the essential ones is trust. Our voice is one of the things we really need to change old management paradigms and build trust in an organization.”
If you are an instructor, teacher, educator, therapist, or all four, having a voice is synonymous with having a job. You can’t do your job without a voice. And yet, we don’t spend much time thinking about vocal physiology, much less how to maintain and even improve it.
The most powerful change agent or therapeutic modality you have - is your voice. Yet, the voice is often overlooked as a therapeutic tool. Think of how important it is for someone giving a TED talk to have good vocal quality, for example. Now consider how important it is for others, like you, who may have to speak for hours on end each day. The vocal folds must be cared for just like we attend to the mind and body during postural yoga practice or movement therapy.
What were the other findings of the report?
- Voice is the foundation of sustainable business success. It increases employee engagement, enables effective decision-making and drives innovation.
- Finding your voice involves both cultural and structural pursuit. First, we need to be culturally competent and sensitive. Only then can we provide the right process through which our voice can be heard.
The power of the voice cannot be ignored, particularly for those who have allergies, respiratory issues, or struggle to make a powerful impact or to establish themselves as an effective team member or thought leader. Oftentimes, the voice is the single variable that holds us back from making the success we are seeking in our work. US News World and Report states,
“Whether you are an aspiring leader or in a support role, developing your communication skills can impact your success. First, let’s take a look at the complexities of communication. It's more than the words you use. It's how and when you choose to share information. It's your body language and the tone and quality of your voice.”
Psychology Today and National Public Radio have recently reported on the relationship between vocal quality and job success and effectiveness. Both agree that speech rate, tone of voice, facial expression, and diction have a great deal of power to make or break effective communication. If tone doesn’t match facial expression, for example, neural dissonance occurs, which erodes trust, increase skepticism, and cooperation.1 In fact, warm vocal tone is a sign of transformational leadership, which generates “more satisfaction, commitment, and cooperation between team members”.2 Changing pitch increases therapeutic potential and improves the chances of your being understood by colleagues, especially when diction is congruent with emotion.1 Additionally, training mindfulness during public speaking can improve prefrontal cortex activity, which allows for improved social awareness, mood-regulation, decision-making, and empathy.4 Vocal awareness and training can slow your pace of speaking, which is shown to deepen others’ respect for you and simultaneously calm anxiety, traits which are bridge-building and healing for all relationships, business and personal.
About MISTY
MISTY is a not-for-profit organization and event dedicated to teaching others about therapeutic yoga.
Ginger’s workshop, “Vocal Liberation,” will introduce techniques for developing and preserving the voice, including projection, quality, longevity, and therapeutic impact through fusion of nada yoga and ENT physiology, which Ginger has developed over her career in public speaking and vocal performance. Want to learn about therapeutic yoga at MISTY? There’s still time to join Ginger and a host of other talented speakers and therapists. Learn more and register at http://www.homyogaevents.com.
Use of affective prosody by young and older adults. Dupuis K, Pichora-Fuller MK. Psychol Aging. 2010 Mar;25(1):16-29.
Leadership = Communication? The Relations of Leaders' Communication Styles with Leadership Styles, Knowledge Sharing and Leadership Outcomes. de Vries RE, Bakker-Pieper A, Oostenveld W. J Bus Psychol. 2010 Sep;25(3):367-380.
Short-term meditation training improves attention and self-regulation. Tang YY, Ma Y, Wang J, Fan Y, Feng S, Lu Q, Yu Q, Sui D, Rothbart MK, Fan M, Posner MI. Proc Natl Acad Sci U S A. 2007 Oct 23;104(43):17152-6.
Since the passing of Title IX in 1972, which protects people from sex discrimination in education or activity programs receiving federal funding, the number of females participating in sports has greatly increased. The National Federation of State High School Associations states that in 2011 nearly 3.2 million girls are participating in high school sports.
Unfortunately, a consequence of this increased participation in sports is a higher prevalence in urinary incontinence (UI) and stress urinary incontinence (SUI) in female athletes. Borin et al looked at the ability of nulliparous female athletes to generate intracavity perineal pressure in comparison to nonathletic women. The study demonstrated that higher mean pressures were generated by nonathletic women in comparison to the athletic women group and that lower perineal pressures in the athletic women were also related to number of games per year and time spent on sport specific workouts and strength training workouts.
UI and SUI are underreported in the general population and also in the athletic population. As health care professionals it is important to screen for UI and SUI in our clients. Physical therapy interventions using pelvic floor muscle rehabilitation have shown to decrease the severity of UI and SUI (Rivalta et al, Hulme). Rivalta used internal methods to improve the function of the pelvic floor muscle. Hulme’s success was achieved through activation of the pelvic floor muscles’ extrinsic synergists.
 |
 |
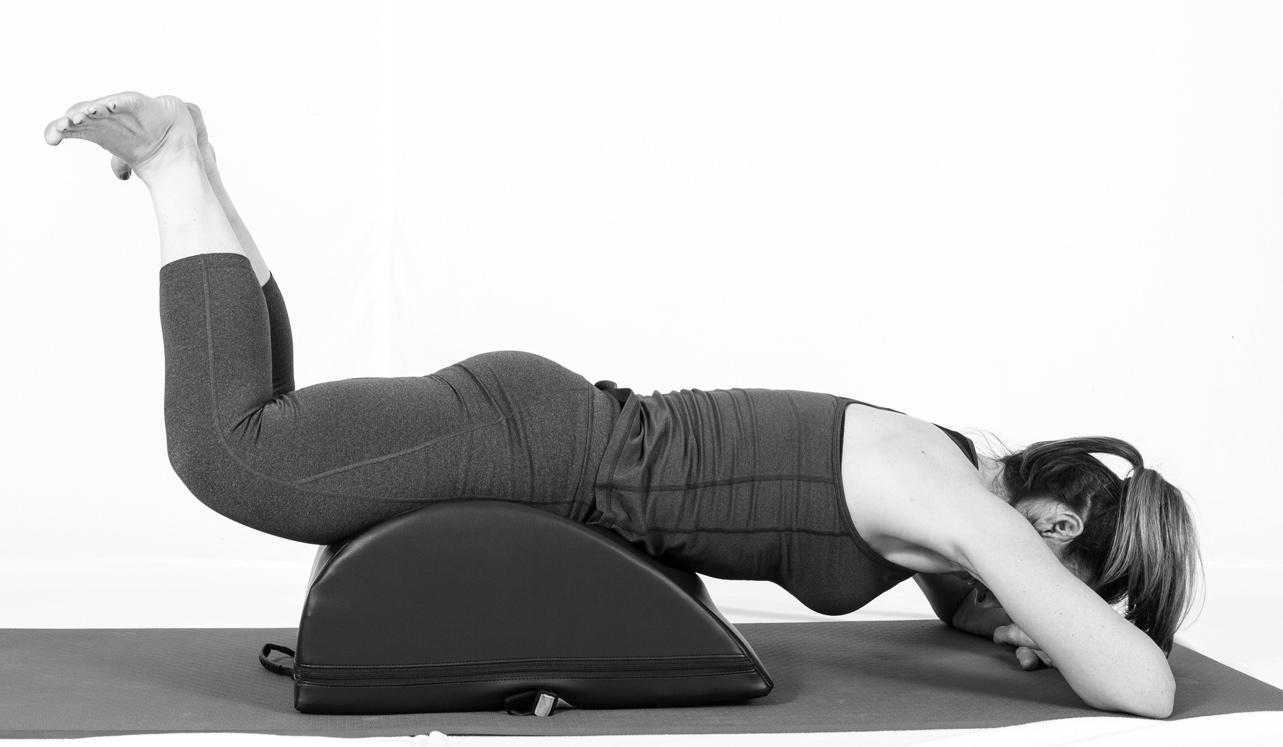
Pilates is often used in physical therapy as a therapeutic tool to improve lumbar stability with studies showing increases in abdominal strength (Sekendiz), trunk extensor endurance (Sekendiz) and to improve posture (Kloubec). Pilates is often also used in pelvic floor muscle rehabilitation and can easily be modified for low level clients. For example the use of resistance can assist supporting the weight of the leg. Practical proof, while lying supine in neutral lumbar spine position, stretch an arm and a leg away from center, notice the difficulty to maintain neutral spine. Now hold a resistance strap, which is also attached to the foot, and notice how maintaining neutral lumbar spine is easier to maintain (pictured above).
Pilates can also be modified for the higher level client or more athletic client. The use of arc barrels, BOSUs or the Hooked on Pilates MINIMAX (pictured belowy) allow the athletic client to achieve an inverted position, unloading the pelvic floor muscles. In the inverted position, pelvic floor muscles may be activated as intrinsic and/or extrinsic synergists of the pelvic floor muscles are also activated. These types of exercises may be more appealing to the athletic client ensuring continuation of the exercise post discharge from physical therapy.
 |
 |
Borin LC, Nunes FR, Guirro EC. Assessment of pelvic floor muscle pressure in female athletes. PMR. 2013; 5(3):189-193.
Hulme, Janet. Beyond Kegels 3rd edition, 2012 Phoenix Publishing Co. Missoula, Montana
Kloubec JA. Pilates for improvement of muscle endurance, flexibility, balance and posture. J Strength Cond Res. 2010;24:661-667.
Rivalta M, Sughunolfi MC, Micali S, De Stafani S, Torcasio F, Bianchi G, Urinary incontinence and sport. First and preliminary experience with a combined pelvic floor rehabilitation program in three female athletes. Health Care Women Int. 2010;31(5);330-334.
Sekendiz B, Altun O, Korkusuv F, Akin S, Effects of pilates exercise on trunk strength, endurance and flexibility in sedentary adult females. J Bodyw Mov Ther. 2005;9:52-57.
One of the dilemmas for many clinicians new to pelvic rehab is trying to figure out which equipment to purchase, and how to convince their employer (or themselves) to purchase the equipment. A common question in relation to equipment for pelvic rehabilitation is “what do I really need?” In a perfect world, and based on both existing and emerging research as well as clinical practice recommendations, we would all have access to pressure biofeedback and real-time ultrasound to help us document and train our patients in best strategies. The truth, however, lies in the fact that when those devices are not available, clinical practice can gain meaningful information from our best tools: our eyes and our hands. Certainly when completing research about pelvic floor generated pressures we might choose pressure biofeedback, and when looking for muscle activation patterns, needle EMG is the right choice, but no one should deny patients the opportunity to learn how to increase or decrease muscle activity, focus on movement retraining, and learn strategies to decrease improve quality of life and function because the latest technology is unavailable.
 Recent research published in the Brazilian Journal of Physical Therapy helps affirm the value of vaginal palpation in an article that assessed the relationship between vaginal palpation, vaginal squeeze pressure, electromyography and ultrasound. Eighty women between the ages of 18 and 35 years old, who had never given birth, and who had no known pelvic floor dysfunction were given a thorough evaluation using a multitude of evaluative methods. These methods included vaginal digital palpation (using Modified Oxford scale), vaginal squeeze pressure, electromyographic activity, diameter of the bulbocavernosus muscles as well as bladder neck movement using transperineal ultrasound. The muscles were assessed in a supine, hooklying position. A strong and positive correlation was found between pelvic floor muscle function and pelvic floor muscle contraction pressure. A less strong correlation was found between pelvic muscle function and pressure and electromyography and ultrasound.
Recent research published in the Brazilian Journal of Physical Therapy helps affirm the value of vaginal palpation in an article that assessed the relationship between vaginal palpation, vaginal squeeze pressure, electromyography and ultrasound. Eighty women between the ages of 18 and 35 years old, who had never given birth, and who had no known pelvic floor dysfunction were given a thorough evaluation using a multitude of evaluative methods. These methods included vaginal digital palpation (using Modified Oxford scale), vaginal squeeze pressure, electromyographic activity, diameter of the bulbocavernosus muscles as well as bladder neck movement using transperineal ultrasound. The muscles were assessed in a supine, hooklying position. A strong and positive correlation was found between pelvic floor muscle function and pelvic floor muscle contraction pressure. A less strong correlation was found between pelvic muscle function and pressure and electromyography and ultrasound.
Vaginal pelvic muscle assessment via palpation has been shown to be more accurate when assessed by more experienced therapists, and use of multiple methods may be most valuable in gaining the most accurate data. In addition to validating the usefulness of pelvic muscle palpation as an evaluative tool, the authors point out that transperineal ultrasound may also be the most appropriate tool for pediatric patients or patients who are otherwise not appropriate for internal pelvic muscle assessment.
Pereira, V. S., Hirakawa, H. S., Oliveira, A. B., & Driusso, P. (2014). Relationship among vaginal palpation, vaginal squeeze pressure, electromyographic and ultrasonographic variables of female pelvic floor muscles. Brazilian journal of physical therapy, 18(5), 428-434.
Rarely does a patient with sacroiliac joint dysfunction come to see us with a goal of having surgery. Sometimes surgery winds up being the last resort for relief if our efforts and the patient’s commitment to physical therapy and prescribed exercises fail. Some of the most recent research shows positive results from minimally invasive surgery; however, the bottom line is to make sure the most educated, clinically accurate diagnosis has been made in implicating the SI joint as the source of pain.
Capobianco et al (2015) performed a prospective multi-center trial regarding SI joint fusion using a minimally invasive technique in women with post-partum pain in the pelvic girdle. Eligibility for the study required subjects to have 3 out of 5 positive SI joint stress tests and at least 50% relief with image-guided intra-articular SI joint block with a local anesthetic. Of the 172 subjects in the study, 20 of the 100 females had post-partum pelvic girdle pain, and 52 subjects were male. Significant improvements in pain, quality of life, and function were found for not only the post-partum group but all groups 12 months after surgery. Worth noting is one to three weeks after surgery, the subjects engaged in physical therapy, two times per week for six weeks.
Whang et al (2015) assessed the 6-month outcomes of SI joint fusion using triangular titanium implants versus non-surgical management in a prospective randomized controlled trial. Of the 148 subjects chosen based on similar diagnostic criteria as the study mentioned above, 102 underwent surgery, and 46 had non-surgical management. Non-surgical management involved appropriate pain medication administration, physical therapy, intra-articular SI joint steroid injections, and radiofrequency ablation of sacral nerve roots, all based on individual needs. The surgical group subjects in this study were also asked to have physical therapy two times per week for six weeks anywhere from one to three weeks post-op. The results in a six month follow up showed “clinical success” of >80% in the surgical group and <25% in the non-surgical management group.
The Journal of Neurosurgery: Spine presented an article in July 2015 by Zaidi et al with results of a systematic review of literature regarding the surgical and clinical effectiveness of SI joint fusion. The studies included open as well as minimally invasive surgery, and the causes of surgery included SI joint degeneration and arthritis, SIJ dysfunction, postpartum instability, posttraumatic, idiopathic, pathological fractures, and HLA-B27+/rheumatoid arthritis. A mean rate of satisfaction with open surgery was 54%; whereas, the mean was 84% with minimally invasive surgery. Ultimately, the authors concluded, “serious consideration of the cause of pain” is necessary before embarking on SI joint fusion as the evidence for the surgery’s efficacy is lacking.
So, who is responsible for making the definite diagnosis for SI joint dysfunction? As many patients get minimal time in doctor offices, we have a professional responsibility to competently perform a thorough evaluation for our patients. When the diagnosis is “SI joint dysfunction,” rule out the lumbar spine and hip; and, of course, when “low back pain” or “hip pain” fills the diagnosis line, rule out/in the SI joint. If you are confused about how, it is time to consider taking the Sacroiliac Joint Evaluation and Treatment course!
References:
Capobianco, R., Cher, D., & for the SIFI Study Group. (2015). Safety and effectiveness of minimally invasive sacroiliac joint fusion in women with persistent post-partum posterior pelvic girdle pain: 12-month outcomes from a prospective, multi-center trial. SpringerPlus, 4, 570. http://doi.org/10.1186/s40064-015-1359-y
Zaidi, Hasan A., Montoure, Andrew J., and Dickman, Curits A. (2015). Surgical and clinical efficacy of sacroiliac joint fusion: a systematic review of the literature. Journal of Neurosurgery: Spine. (23)1:59-66. DOI: 10.3171/2014.10.SPINE14516
Whang, P., Cher, D., Polly, D., Frank, C., Lockstadt, H., Glaser, J., … Sembrano, J. (2015). Sacroiliac Joint Fusion Using Triangular Titanium Implants vs. Non-Surgical Management: Six-Month Outcomes from a Prospective Randomized Controlled Trial. International Journal of Spine Surgery, 9, 6. http://doi.org/10.14444/2006
The following post comes to us in part from Ginger Garner, PT, ATC, PYT, who teaches three yoga courses for Herman & Wallace; Yoga for Pelvic Pain, Yoga as Medicine for Pregnancy, and Yoga as Medicine for Labor and Postpartum. Check out her poster at the Combined Sections Meeting this weekend in Anaheim!

Maternal health care in the United States is abysmal. Especially wretched is care and support of women post-partum. Our insurance system is partially to blame by dictating that women receive only one visit with the provider who participated in the delivery of their baby 6 weeks after the baby is born, no matter the method of delivery. This is often after most of the scary, unexpected side effects of delivery, like heavy bleeding, nipple pain, urinary incontinence, difficulty with bowel movements, scar pain and tremendous mood swings have begun to ease. Only the women who are the most persistent, or those who have chosen unique care models (like out of hospital births with midwives), seem to get real support post-partum, leaving marginalized and less self-driven women to fend for themselves.
What if research could show that immediately treating some of the side effects of birth, like diastasis recti abdominus, which occurs in 50-60% of post-partum women, could result in improved outcomes in the long run? What if someone could prove that retraining and strengthening the abdominal wall as part of a biopsychosocial model empowering women could change the costly effects of prolapse and urinary incontinence treatment later on in life? What if that research aimed to show that treating women in partnership will all care providers was the most effective? These are big questions, but through research beginning with Diastasis Recti Abdominis (DRA), some Women’s Health Physical Therapists trained in Medical Therapeutic Yoga are hoping to highlight some answers.
At CSM in San Diego next month, these researchers (listed below) are presenting a poster via the Section on Women’s Health showcasing their paper, Diastasis Recti Abdominis: A Narrative Review. They found that good, solid research focusing on the co-morbidities and treatment of DRA is really lacking. Most well-done studies focus on the reliability and validity of measurement techniques, showing that calipers and ultrasound are the most valid and reliable ways to measure the gap. There is not even agreement on what precise measurement technically constitutes a DRA, though most agree that normal inter-recti distance is 15-25mm supraumbilically among parous females with digital calipers. (Chiarello 2013).
Besides the obvious cosmetic and general strengthening concerns, why do we care about physical therapy care for a post-partum DRA? Spitznagle’s retrospective chart review of women presenting for gynecological care with a mean age of 52 found that 52% had DRA and 66% of them had a least one support-related pelvic floor muscle dysfunction. Those with DRA were more likely to have pelvic organ prolapse, urinary incontinence and fecal incontinence. Another study by Parker found a DRA prevalence of 74.4% among women with back or pelvic area pain who had delivered at least one child and sought PT. They found a significant difference in VAS pain levels in those with DRA and abdominal or pelvic pain compared to those without DRA. More well-done, prospective studies are really needed to correlate these sequalea in later life to DRA post-partum.
The topic of how to retrain the abdominal wall to restore optimal function and cosmetic appearance is hot in the blogosphere right now. Does it matter if the width of the diastasis recti is reduced? Or is it a matter of having tension in the linea alba as the clinician sinks his/her fingers toward the spine? Biomechanically we know that in order to improve stiffness in the trunk, we need synergistic and symmetrical firing of the diaphragm, transversus abdominis, multifidus and the pelvic floor with proper timing and contraction of the hip and external abdominal muscles. Benjamin completed a review of the research on the effects of exercise in the antenatal and postnatal periods and concluded that antenatal exercise may be protective against the formation of a DRA, but that the available studies are of such poor quality and varied in the way that abdominal/core strengthening was applied in the post-partum population, that it is impossible to tell how or why exercise may or may not help with DRA!
There is clearly a huge hole in the literature and as usual, new mothers are suffering. Women are spending money on programs they find on the internet that are not backed by solid research, because there is not any! Regarding DRA, post-partum women in our country desperately need well-done, high quality studies promoting a specific and well-described exercise for healing. In addition, in our patriarchal health care model, we need to show without a shadow of a doubt that treating post-partum muscle weakness, body mechanics issues and DRA is essential for saving money in the long run on prolapse and urinary incontinence surgery, as well as decreasing expenditure on back pain treatments.
If our discipline could provide this research, ALL women could have access to personal, post-partum recovery. As an established part of the health care system and with longer treatment times and the chance to get to know our patients better, physical therapists are the IDEAL healthcare practitioners to ensure that post-partum women are getting adequate physical retraining, but also psycho-social support that is so lacking in the United States.
The Women’s Health Poster Presentations at CSM in Anaheim will be on Saturday, Feb 20 from 1-3PM. I look forward to meeting with some of you and visiting about what you are working on to further the cause of improving maternal health care and DRA treatment.
Ginger Garner PT, ATC, PYT, Professional Yoga Therapy Institute, Emerald Isle, NC
Elizabeth Trausch, DPT, PYT Des Moines University, Des Moines IA
Stefanie Foster, PT, PYT Asana with Intelligence, Houston, TX
Paige Raffo, PT, PYT, CPI, Balance+Flow Physio, Bellevue, WA
Janet Drake, PT, LCCE, FACCE, PYT, Central Bucks Physical Therapy, Doylestown, PA
Stacie Razzino, PT, PYT, Free Motion Physical Therapy, Melbourne, FL
Blog post by Libby Trausch, DPT
Spitznagle T, Leong F, Van Dillen L, Prevalence of diastasis recti abdominis in a urogynecological patient population, International Urogynecology Journal. 2007; 18: 321-328.
Chiarello CM, Mcauley JA. Concurrent validity of calipers and ultrasound imaging to measure interrecti distance. Orthop Sports Phys Ther. 2013; 43(7): 495-503
Benjamin DR, et al., Effects of exercise on diastasis of the rectus abdominis muscle in the antenatal and postnatal periods: a systematic review. Physiotherapy. 2014 Mar;100(1):1-8.
The following is a guest post from Nancy Fish, LCSW, MPH who will be presenting at the Alliance for Pelvic Pain Retreat on May 20-22 in Ellenville, NY. Check out this flier to learn more about the retreat.
Gaining a Sense of Hope and Empowerment
Nancy Fish, LCSW, MPH (co-author, with Deborah Coady,M.D. of Healing Painful Sex)
About the Alliance For Pelvic Pain Retreat, May 20-22, 2016, Ellenville, NY
When thinking about registering for the Alliance for Pelvic Pain Patient Retreat, I imagine you are asking yourself “Why would a person suffering from pelvic pain, with more medical appointments than is humanly possible to handle, add another item on an already overwhelming “to do” list?” It would be completely understandable if that is your initial reaction. So why is this retreat a must in your path to physical and emotional healing? There are so many reasons why this retreat can be a life-altering event but I’ll just name a few compelling ones. As a psychotherapist who specializes in pelvic pain (I am also a pelvic pain patient) the primary challenges I hear from most of my clients are:
- “I feel so alone.”
- “This is too embarrassing to talk about with ANYONE.”
- ”I feel so hopeless and that there is nothing that can help me.”
- “I feel like I will never have sex again.”
- “Who will want me?”
- “No doctor understands this and no doctor can help me.”
If you are reading this blog, I’m sure you can identify with a few if not all of these statements. If only ONE of these statements is something you relate to, then the AFPP retreat is an event you cannot afford to miss. It will provide you with invaluable tools to address all of your concerns. You will have access to some of the world’s most renowned medical, physical therapy, and mental health professionals specializing in the integrative treatment of pelvic pain who will be able to answer any of your questions or concerns. There will be opportunities to register for significantly discounted one on one sessions with expert physical therapists, an Acupuncturist, a yoga instructor, and services from the EarthMind Wellness Center at Honors Haven. You will also be with other individuals who share the same concerns and challenges and you will not have to explain issues like “why you can’t sit” or “why this pain makes you feel you are going crazy.” For the first time in a long time you will not have to justify behaviors or decisions that you are confronted with on a daily basis – you can just be you.
One of the greatest tools you will gain from this retreat is empowerment. Pelvic pain can be so disempowering and our goal is give you the ability to empower yourself so you begin or continue on the path of self-healing through a combination of medical and integrative health techniques. I never ask any of my clients to use a technique that I don’t use myself. And I have found that medical interventions are often essential but not enough. Overcoming pelvic pain takes an “East meets the West” approach using a daily practice of mindfulness, meditation, and other integrative techniques. Participants leave the retreat with a new support system, a sense of self-empowerment, and a host of self-healing practices (such as a physical therapy home program) that will be invaluable on your journey to recovery – and most important, A RENEWED SENSE OF HOPE.
(Spaces are limited so please book your reservation as soon as possible. Also, for funding opportunities, all participants should go to Gofundme.com.)
The following post comes to us from Herman & Wallace faculty member Allison Ariail, PT, DPT, CLT-LANA, BCB-PMD, PRPC. Allison authored "Use of transabdominal ultrasound imaging in retraining the pelvic-floor muscles of a woman postpartum" and is a leading expert in the use of ultrasound imaging for pelvic rehab. She is the author and instructor of the Rehabilitative Ultrasound Imaging: Women’s Health and Orthopedic Topics offered with Herman & Wallace.
In the pelvic floor series we learn how to perform examinations for cystoceles and rectoceles. It can be more difficult for therapists to examine and quantify the degree of uterine descent. In the last few years translabial ultrasound imaging has also been used to identify what is happening in the anterior compartment upon Valsalva and pelvic floor contraction, including the uterus. This is helpful when trying to determine the degree of uterine prolapse. Degree of pelvic organ descent visible on by ultrasound has been shown to have a near-linear relationship with measures on the POPQ.
 Clinically we see that some patients with severe prolapses have few symptoms, while other patients with smaller prolapses will have more severe complaints of symptoms. This can be puzzling to the clinician who is trying to treat prolapse patients. Shek and Dietz performed a study to set cutoff measures of uterine descent that will predict symptoms of prolapse. Translabial ultrasound imaging was performed on 538 women with 263 women reporting prolapse symptoms. Seventy-five percent of the women presented with grade two or greater prolapse on the POPQ, with most of being cystoceles or rectoceles. The women with more complaints of symptoms of prolapse were more likely to have uterine prolapse. There was a strong association between degree of uterine descent and symptoms of prolapse. They determined that an optimal cutoff to predict symptoms of prolapse due to uterine descent is a cervix descending to 15 mm above the pubic symphysis.
Clinically we see that some patients with severe prolapses have few symptoms, while other patients with smaller prolapses will have more severe complaints of symptoms. This can be puzzling to the clinician who is trying to treat prolapse patients. Shek and Dietz performed a study to set cutoff measures of uterine descent that will predict symptoms of prolapse. Translabial ultrasound imaging was performed on 538 women with 263 women reporting prolapse symptoms. Seventy-five percent of the women presented with grade two or greater prolapse on the POPQ, with most of being cystoceles or rectoceles. The women with more complaints of symptoms of prolapse were more likely to have uterine prolapse. There was a strong association between degree of uterine descent and symptoms of prolapse. They determined that an optimal cutoff to predict symptoms of prolapse due to uterine descent is a cervix descending to 15 mm above the pubic symphysis.
This study intrigues me and makes me wonder how much we are focusing on cystoceles and rectoceles and not looking at uterine prolapses. Using translabial ultrasound imaging is a nice tool to allow the clinician to see what is going on with all of the pelvic organs. With one Valsalva maneuver you are able to assess a lot of information including support of the pelvic organs. It also gives the clinician another way to quantify the degree of prolapse. Ultrasound imaging is a wonderful tool that clinicians can use for assessment as well as a biofeedback tool. If you are interested in learning how to perform this type of assessment, I will be teaching Rehabilitative Ultrasound Imaging: Women’s Health and Orthopedic Topics May 1-3 in Dayton, OH.
Shek KL, Dietz HP. What is abnormal uterine descent on translabial ultrasound? Int. Urogynecol J. 2015; 26(12)1783-7.
By accepting you will be accessing a service provided by a third-party external to https://hermanwallace.com/











































