
Rachel Kilgore, DPT, OCS, COMT, PRPC, PPCES graduated from Central Washington University with a Bachelor of Science (BS) in exercise science and a minor in nutrition in 2004 and completed her Doctor of Physical Therapy (DPT) at the University of Washington in 2007. Rachel practices in Seattle at Flow Rehab in the Freemont Neighborhood with Holly Tanner and focuses her patient care on orthopedics, female athletes, and women’s health conditions for bladder & bowel dysfunctions, pelvic, pain, pregnancy, and post-partum issues.
I have always been very particular about the precision of words. I have been known to ruminate about the origin, evolution, and application of words. As my husband always kindly says, I am an overthinker. This leads me to our nomenclature analysis for today, Diastasis.
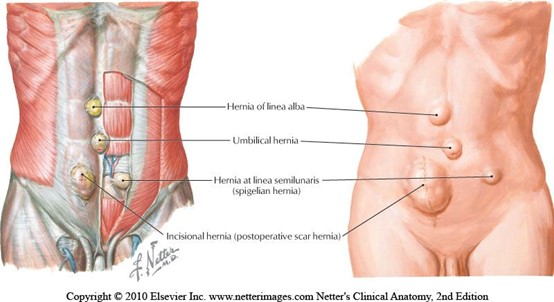
When teaching pregnancy and post-partum courses we always have healthy discussions about Diastasis Rectus Abdominus (DRA) as this is an important topic in the peripartum world. One question that always comes up is what is the difference between a hernia and DRA? If DRA is not a condition you deal with often in the clinic, it can be a bit confusing. According to the Merriam-Webster Dictionary diastasis means “an abnormal separation of parts normally joined together,” so DRA is often defined as a separation of the Rectus Abdominus muscles. I think the word separation is what causes the confusion. This word may lead some people to think there is an actual disruption of the abdominal tissue which is not the case. The rectus abdominus halves remain joined together by the linea alba. The linea alba is the tendinous raphe formed by interdigitating fascia of external/internal obliques and Transversus Abdominis. A DRA is an increase in the distance between the right and left Rectus Abdominus halves. If you stretch connective tissues (increase the distance between two ends), they may become thinner, lengthened, or weakened. A DRA is an increased distance between the right and left Rectus Abdominus halves that may result in lengthened, thinner, weaker tissue. In contrast, a hernia is an actual defect in the connective tissue. DRA and hernias are not the same thing; however, they can exist together.


I have always enjoyed working with the peripartum population. However, the longer I worked in pelvic rehabilitation the more I heard the same story over and over when interviewing patients. For example, when working with a patient with urinary incontinence or prolapse, I would say: “when did this start” and some of my elderly patients would laugh and say “when Johnny was born” and I would say “how old is Johnny” they would reply “40!” Many of the pelvic patients I was treating had symptoms originating around the time of childbirth and they had been suffering for decades. So, I figured, let’s get to the root of the problem and focus on earlier intervention.
What is the root of the problem? In my opinion, it is the lack of postpartum care. Pregnant patients are often inundated with birth education programs and information about pregnancy and childbirth. Additionally, there is a battery of prenatal visits, prenatal testing, and preparations for birth. All of which are wonderful to help prepare for birth. Conversely, the resources and guidance to help with physiological and musculoskeletal healing postpartum are lacking. Patients are counseled about serious signs and symptoms, but clear guidance to help to return to daily functional activities including recreation and exercise is often not provided. As musculoskeletal and exercises experts we are in a wonderful position to help patients reduce pain and improve function following the birth of a child.
Prior to 2018, the first post-partum checkup was six weeks following birth. Barring any severe problems, this was often the last contact with a medical provider for the parent. Patients were not provided specific guidance on how to return to daily activities, let alone higher-level activities such as running, exercising, and/or lifting weights.
So many physiological changes occur to a woman’s body during pregnancy, it is no wonder that pregnant women have back and lower extremity aches and pains. These women experience hormonal changes, weight gain, reduced abdominal strength, and their center of mass shifts anteriorly. These physiological changes result in altered spinal and pelvic alignment, and increased joint laxity. Also, many women report increases in size of their feet and a tendency to have flatter arches during and after pregnancy. Alignment changes may influence pain. Altered alignment could change the physical stresses placed upon different tissues of the body, which that specific tissue was not adapted to, therefore, causing pain or injury to that tissue.
A recent study published in 2016, in the Journal of Women’s Health Physical Therapy1, investigated if there may be a relationship between anthropometric changes of the foot that occur with pregnancy, and pregnancy related musculoskeletal pain of the lower extremity. The study included 15 primigravid women and 14 weight matched controls. This study was a repeated-measurements design study, where the investigators measured foot length, foot width, arch height index, arch rigidity index (ARI), arch drop (AD), rear foot angle, and pelvic obliquity during the second and third trimesters and post-partum. The subjects were surveyed on pain in the low back, hips/buttocks, and foot/ankle.
The author’s findings were that measures of arch flexibility (ARI and AD) correlated with pain at the low back and the foot and ankle. They concluded that medial longitudinal arch flexibility may be related to pain in the low back and foot. The more flexible arches were associated with more pain in the study participants. They reported the participants in their study did not have very high pain levels in general, and recommend further studies to compare pregnant women who experience severe pain with women who do not while comparing their alignment factors. This article is a good reminder for physical therapists to consider the changes that occur to the foot including changes in arch height, arch flexibility, and foot size and how that influences the pelvis and lower extremity for prevention and treatment of musculoskeletal pain during pregnancy.
Have you ever tried to teach a patient how to isolate their transversus abdominis (TA) contraction or a pelvic floor muscle (PFM) contraction and the patient had difficulty or you weren’t sure how well they were isolating it? Did you ever wish you had the ability to use real-time ultrasound (US) to confirm which abdominal layers they were isolating or use it for visual feedback to assist in your patient’s learning? Could it be helpful to be able to use real-time US to identify if they were isolating the pelvic floor muscles and give your patient visual feedback? Of course!
Real- time US has been used as an assessment and teaching tool to directly visualize abdominal and PFMs. PFM function can be assessed by observing movement at the bladder base and bladder neck. Various studies have used US on women with and without urinary incontinence (UI). These studies usually use transabdominal (TAUS) and transperineal (TPUS) ultrasound to measure if PFM isometrics or exercises are performed correctly or incorrectly, or how the muscles are functioning.
A 2015 study in the International Urogynecology Journal utilized TAUS to identify the ability to perform a correct elevating PFM contraction and assess bladder base movement during an abdominal curl up exercise. Abdominal curl ups are cited to increase intra-abdominal pressure. Activities that increase intra-abdominal pressure have been cited to provoke stress urinary incontinence (SUI). Abdominal curl ups are often completed in group exercise classes and have been found to provoke SUI in up to 16% of women.
The Center for Disease Control reports that prostate cancer is the most common form of male cancer in the United States (just ahead of lung cancer and colorectal cancer), and the American Cancer Society estimates that 1 in 7 men will be diagnosed with prostate cancer at some point in their lifetime. With prostate cancer being so common, it is likely that a male with symptoms of urinary incontinence following a prostatectomy may show up at your clinic’s door for treatment. What do you do? Whether you have extensive training for male pelvic floor disorders or are just starting your initial training for pelvic floor dysfunctions, you likely have some intervention skills to help this population.
A recent case report in the Journal of Women’s Health Physical Therapy, outlines management of a 76-year-old male patient with mixed urinary incontinence postprostatectomy 10 years. This case report does a nice job describing not just physical therapy (PT) interventions, but also multifaceted management of a typical patient post radical prostatectomy. The case report describes a thorough history, systems review, pelvic floor muscle (PFM) examination, tests &measures, and outcome assessment. Our discussion will focus on interventions as you may already possess the skills for several of the treatments included in this patient’s plan of care.
The patient’s complaints were mixed urinary incontinence (UI) symptoms including 3-4 pads per day and 1 pad at night. He reported nocturia 3-4 times per night. 2-3 times per week he had large UI episodes that soaked his outwear. Also, he complained of inability to delay voiding, and UI with walking to the bathroom, sit to stand, lifting, coughing, and sneezing.
Myofascial release (MFR) can be one of your greatest treatment tools as a pelvic rehabilitation practitioner. Just in case you don’t think about fascia often here are a couple helpful things to remember. Fascia is the irregular connective tissue that covers the entire body, and it is the largest sensory system in the body, making it highly innervated. The mobilizing effect of MFR techniques occurs by stimulating various mechanoreceptors within the fascia (not by the actual force applied). MFR techniques can help to reduce tissue tension, relax hypertonic muscles, decrease pain, reduce localized edema, and improve circulation just to name a few physiological effects.
An interesting case report published in 2015 by the Journal of Women’s Health Physical Therapy1 offers a wonderful example of how a physical therapist used specific MFR techniques for a patient with clitoral phimosis and dyspareunia. The specific MFR techniques used helped to provide relief and restore mobility to the pelvic tissues for this patient.
Clitoral phimosis is adherence between the clitoral prepuce (also known as the clitoral hood) and the glans. This condition can be the result of blunt trauma, chronic infection, inflammatory dermatoses, and poor hygiene. In this case report, the 41-year-old female patient had sustained a blunt trauma injury to the vulva (when her toddler son charged, contacting his head forcibly into her pubic region). She presented to physical therapy with complaints of dyspareunia, low back pain, a bruised sensation of her pubic region, vulvar pain provoked by sexual arousal, decreased clitoral sensitivity, and anorgasmia. The physical therapist completed an orthopedic assessment for the lower quarter (including spine and extremities), as well as a thorough pelvic floor muscle assessment.
Help others by helping ourselves
As pelvic rehabilitation practitioners, we have all been there, looking ahead to see what patients are on our schedules and recognizing that several will require immense energy from us… all afternoon! Then we prepare ourselves, hoping we have enough stamina to get through, and do a good job to help meet the needs of these patients. Then we still have to go home, spend time with our families, do chores, run errands, and have endless endurance. This can happen day after day. Naturally, as rehabilitation practitioners, we are helpers and problems solvers. However, this requires that we work in emotionally demanding situations. Often in healthcare, we experience burnout. We endure prolonged stress and/or frustration resulting in exhaustion of physical and/or emotional strength and lack of motivation. Do we have any vitality left for ourselves and our loved ones? How can we help ourselves do a good job with our patients, but to also honor our own needs for our energy?
How do we as health care practitioners’ prevent burnout?
Ever hear of “mindfulness” ... I am being facetious. The last several years we have been hearing a lot about “mindfulness” (behavioral therapy or mindfulness-based stress reduction) and its positive effects in helping patients cope with chronic pain conditions. Mindfulness is defined as “the practice of maintaining a nonjudgmental state of heightened or complete awareness of one's thoughts, emotions, or experiences on a moment-to-moment basis,” according to Merriam-Webster’s Dictionary. One can practice mindfulness in many forms. Examples of mindfulness-based practice include, body scans, progressive relaxation, meditation, or mindful movement. Many of us pelvic rehabilitation providers teach our patients with pelvic pain some form of mindfulness in clinic, at home, or both, to help them holistically manage their pain. Whether it is as simple as diaphragmatic breathing, awareness of toileting schedules/behavior, or actual guided practices for their home exercise program, we are teaching mindfulness behavioral therapy daily.
Urinary incontinence (UI) can be problematic for both men and women, however, is more prevalent in women. Incontinence can contribute to poor quality of life for multiple reasons including psychological distress from stigma, isolation, and failure to seek treatment. Patients enduring incontinence often have chronic fear of leakage in public and anxiety about their condition. There are two main types of urinary leakage, stress urinary incontinence (SUI) and urge urinary incontinence (UUI).
SUI is involuntary loss of urine with physical exertion such as coughing, sneezing, and laughing. UUI is a form of incontinence in which there is a sudden and strong need to urinate, and leakage occurs, commonly referred to as “overactive bladder”. Currently, SUI is treated effectively with physical therapy and/or surgery. Due to underlying etiology, UUI however, can be more difficult to treat than SUI. Often, physical therapy consisting of pelvic floor muscle training can help, however, women with UUI may require behavioral retraining and techniques to relax and suppress bladder urgency symptoms. Commonly, UUI is treated with medication. Unfortunately, medications can have multiple adverse effects and tend to have decreasing efficacy over time. Therefore, there is a need for additional modes of treatment for patients suffering from UUI other than mainstream medications.
An interesting article published in The Journal of Alternative and Complimentary Medicine reviews the potential benefits of yoga to improve the quality of life in women with UUI. The article details proposed concepts to support yoga as a biobehavioral approach for self-management and stress reduction for patients suffering with UUI. The article proposes that inflammation contributes to UUI symptoms and that yoga can help to reduce inflammation.
A diagnosis of breast cancer means many different things to many different people. Regardless, receiving this diagnosis means some sort of treatment will likely follow. The types of treatment and outcomes are largely dependent on individual patient scenarios, however, one thing is for certain: A patient’s life will be forever changed after having received this diagnosis.
Historically, comprehensive care for a patient with breast cancer has focused on treatment and prevention. However, more and more women are surviving breast cancer every year. Therefore, more attention needs to be paid to survivorship. Once someone has survived cancer, comprehensive, quality care should obviously focus on preventing recurrence, however, it may also include guidance and counseling on maintaining a healthy lifestyle and addressing physical and psychosocial changes.
A very recent 2016 article published in the Annals of Surgical Oncology discusses the subject of survivorship in breast cancer patients. This article suggests that the key to achieving successful outcomes for management of a breast cancer survivor is a multidisciplinary approach to help these survivors deal with the physical and psychosocial sequela resulting from their diagnosis.
As a pelvic rehabilitation provider, this is a very thought-provoking article as it outlines several areas in which I feel breast cancer survivors could benefit from physical therapy. A pelvic rehabilitation provider can be a valuable part of the multidisciplinary team that helps manage a breast cancer survivor towards positive and meaningful outcomes, ultimately enhancing their quality of life. The following are some areas addressed in the article in which a breast cancer survivor may need assistance to improve and support a meaningful quality of life.
III. Postpartum
Nourishing my baby and myself, a complicated dichotomy
The care I received from the doctors, nurses, and hospital staff during labor, delivery, and postpartum period was excellent. I felt all the staff members explained all procedures for myself and the baby. The labor and delivery nurses were helpful and compassionate. They showed me how to breastfeed the baby, assisted me with skin to skin contact, and taught my husband and I how to care for the baby when we took her home. The birth center site at the hospital was amazing. I had an individual birthing suite with a bathroom, a television, a bathtub and a place for my husband to sleep. Health care for the baby and I following delivery continued to be excellent. I had a surgical follow up one week later with my doctor and another postpartum visit at 6 weeks. At each visit I was given The Edinburgh Postnatal Depression Scale (a scale to help identify postpartum depression) as well as educational pamphlets on self-care following a cesarean delivery. The only complaints I had that required assistance from a health care provider was with getting baby to latch with breast feeding and neck and shoulder pain from breast feeding the baby. I took it upon myself to work on core and hip exercises I would give a postpartum patient who had undergone a cesarean delivery and was working on my scar tissue to prevent problems with bladder, bowel, abdomen, and uterus. I sought some massage for my neck and shoulders and did my physical therapy exercises for my neck and shoulders. I sought a lactation consultant for the latching issues with breast feeding. Seeking care helped resolve these issues which reduced my neck and shoulder pain and helping me enjoy breastfeeding my baby.
Before having my daughter, I had preconceived notions about postpartum care. For the last ten years since I started working with women’s health patients I have heard repeatedly from my patients that they felt they did not receive comprehensive postpartum care. Many of these women hopped from health care provider to health care provider, sometimes taking years to resolve orthopedic or pelvic floor problems from their pregnancy or labor and delivery experience. Quality postpartum care was my soap box issue and still is. That being said, I was very satisfied with my postpartum health care experience. My experience revealed that support and education about postpartum problems as well as proactive healthcare for theses challenges is becoming mainstream. I have always felt that women in our country need better post-partum care and I am happy to see improvements being made. We may forget between the constant baby changing, soothing, and feedings that mom needs some care too. I am not sure that we always remember that there have been 9 months of physiologic changes occurring to a woman’s body. Additionally, physical trauma that occurs with caesarean or vaginal delivery. A mother may need physical therapy for exercises to strength abdominals or back, help for bowel or bladder problems, manual therapy for painful intercourse, or scar tissue work for abdominals or pelvic floor.
I think as a society we are getting more aware of the influence of hormones, crying babies, sleep deprivation, and a heavy work load can overwhelm a postpartum mother. Based on my experience only, I think we are doing a better job of monitoring postpartum depression, pain management, and pelvic floor problems. I was so pleased at the availability of information and counseling opportunities presented to me during my birthing and postpartum experience. I received so much encouragement and permission to seek help from others during my postpartum healing.