Cancer and oncology treatments have several common side effects like fatigue, changes in appetite, and pain. However, patients who have bladder or gynecological cancers can also experience side effects that affect the bladder, bowel, and sexual functioning. The pelvic floor muscles of these patients can be negatively impacted by many things including surgery, radiation, and in some cases, the tumor itself. Pelvic rehab programs can play a crucial role in improving pelvic floor function and overall quality of life for patients who have been diagnosed or treated for these cancers. Don't underestimate the impact of pelvic rehab on regaining both the quality and satisfaction of life after treatment.
Radiation for gynecological cancers, for instance, has been reported to cause vaginal stenosis resulting in generalized pelvic pain and dyspareunia.1 Surgical options including tumor debulking, hysterectomy, and salpingo-oophorectomy can result in scar tissue that can cause tissues or muscles to shift. As pelvic rehab professionals, it is our privilege to offer an evidence-based and solution-focused approach for the often overlooked pelvic health issues faced by people undergoing treatment for pelvic cancers. Our role is crucial in providing much-needed support and care for these patients.
Pelvic rehab therapy can improve and sometimes even prevent the detrimental impacts on the pelvic and abdominal area that negatively impact the patient’s quality of life. Some of the most common therapy options to help improve your patient's pelvic functioning are:
- Soft tissue mobilization and stretching of tight muscles.
- Exercises to strengthen the core and pelvic floor muscles.
- Recommending dietary changes such as avoiding alcohol or caffeinated beverages and other dietary irritants.
- Relaxation and deep breathing to relax the muscles.
- Postural corrections.
- Biofeedback techniques.
- Vaginal dilators or anal dilators for pain during intercourse.
As Michelle Lyons shared in a past blog with the Pelvic Rehab Report, “Whether it is advice on managing anal fissures (skin protection, down-training overactive pelvic floor muscles, achieving good stool consistency, teaching defecatory techniques) or dealing with dyspareunia (dilator or vibrator selection, choosing and using an appropriate lubricant, dealing with the ergonomic or orthopedic challenges that can be a barrier to returning to sexual function and enjoyment), pelvic rehab practitioners are probably the best clinicians for optimizing a return to both pelvic and global health during and after treatment for pelvic cancers.”2
If you work with patients facing pelvic or abdominal issues from a cancer diagnosis or treatment regime, join Herman & Wallace in Oncology of the Pelvic Floor Level 2B scheduled for May 4-5, 2024. This course covers topics on bladder and gynecological cancers including diagnoses, medical treatments, and ways a pelvic rehab professional can help these patients recover. Learn how to help your patients, not just survive, but thrive after treatment. Pelvic therapy interventions from urinary continence to sexual function can offer valuable tools for your patient's long-term well-being.
Resources:
- Damast S, Jeffery DD, Son CH, Hasan Y, Carter J, Lindau ST, Jhingran A. Literature Review of Vaginal Stenosis and Dilator Use in Radiation Oncology. Pract Radiat Oncol. 2019 Nov;9(6):479-491. doi: 10.1016/j.prro.2019.07.001. Epub 2019 Jul 11. PMID: 31302301; PMCID: PMC7944435. https://pubmed.ncbi.nlm.nih.gov/31302301/
- Lyons, Michelle. “Rehabilitating Pelvic Floor Muscles after Cancer Treatment.” The Pelvic Rehab Report, Herman & Wallace. February 13, 2017. https://hermanwallace.com/blog/rehabilitating-pelvic-floor-muscles-after-cancer-treatment.
This article has been reviewed for accuracy by Allison Ariail.
So often as “pelvic floor therapists”, our name and scope of manual treatment can seem to center around stretching or strengthening pelvic floor muscles. But, if you have been practicing for a while, maybe you want to go deeper.
We talk in the Pelvic Function Series about “zooming out” (considering postural, musculoskeletal, breathing, autonomics, and pressure systems). We also have noticed in our field an increased emphasis on the nervous system for regulating the system.
We also talk about “zooming in”, bringing our focus inside the pelvis. That could be pelvic floor muscles, but if we want to zoom in even deeper, we may start to look at peripheral nerves, supportive ligaments, and the interplay between bones, ligaments, fascia, and muscles that could be keeping pain, dysfunction, over-activity, or tension syndromes alive.
The sacrospinous and sacrotuberous ligaments are incredible structures we often don’t give enough attention to. Both the SS and ST ligaments have coccyx attachments and can affect coccyx pain, position, and create tension in the coccygeal nerves.
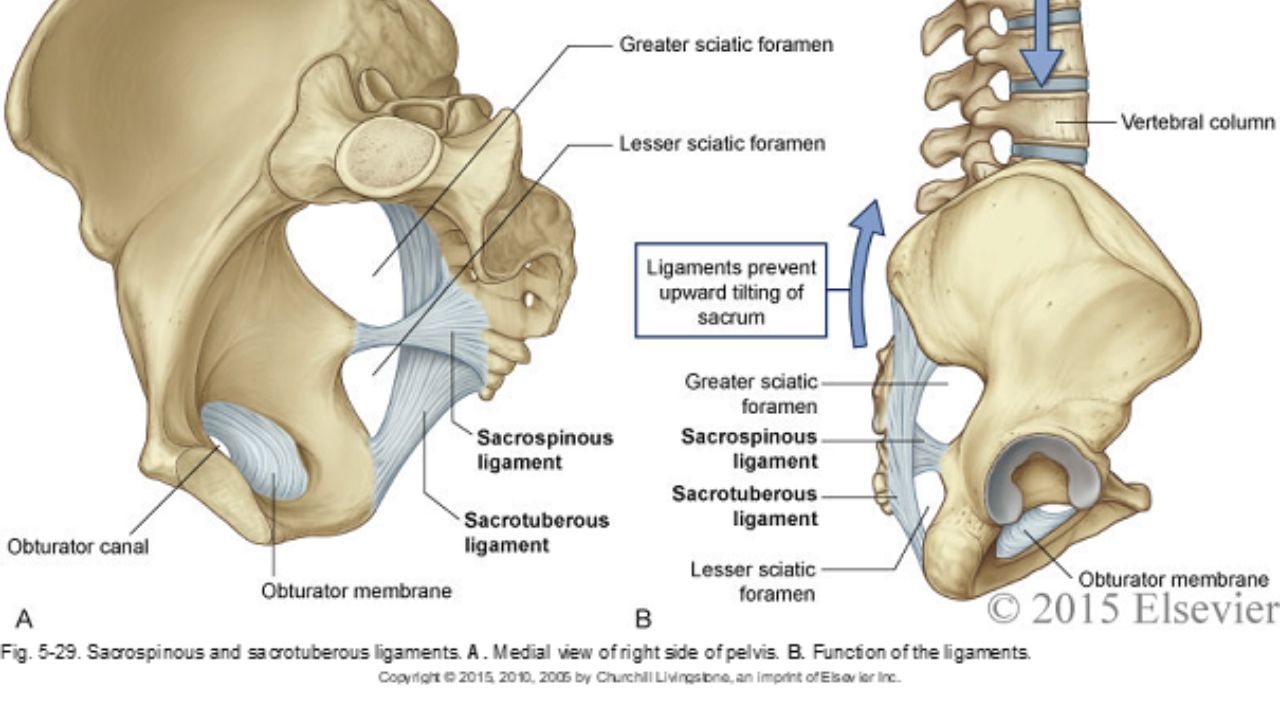
The entire support and structure of the posterior-lateral pelvic bowl is constructed from these two ligaments (with the posterior longitudinal SI ligament). They can become tight and rigid from bearing the burden of stabilizing. The SS ligament may even hold the support for the vaginal canal after hysterectomy. These two ligaments create the greater and lesser sciatic foramen and the nerves of the sacral plexus (pudendal, sciatic, gluteal nerves, and posterior femoral cutaneous nerves) all have intimate relationships and are affected by the tension in these ligaments.
In the Sacral Nerve Manual Assessment and Treatment Class, we learn techniques to deeply release these ligaments (without stressing our hands), external fascial techniques for the coccyx fascia and ligaments, releases for the deep hip muscles that these nerves run through, and how to individually do neuro-lymphatic work to decrease perineural thickening and swelling within the nerve that prevents pain-free gliding. We use differential diagnosis, manual technique, home program, and intricate anatomy study to learn how to get closer to the root of dysfunction in the pelvic floor and posterior gluteals, saddle region, and leg. Come join us on May 11&12 to add depth to your toolbox and understanding of the anatomy of the pelvic nerves.
*Images used with permission from Elsevier 2015.
AUTHOR BIO:
Nari Clemons, PT, PRPC

Nari Clemons was born and raised in the Midwest before moving to Portland, Oregon. At Herman & Wallace, Nari teaches the Pelvic Function Series (PF1, 2A, 2B, and PF Capstone). She was one of three co-authors. Her passion is taking difficult concepts and techniques and simplifying them so that participants can leave courses with confidence, enthusiasm, and feeling empowered in their clinical practice.
Nari graduated from the Medical College of Ohio in consortium with the University of Toledo, with a degree in physical therapy. She owns a private practice, Portland Pelvic Therapy, where she focuses on pelvic, abdominal, and neural issues. Nari has studied visceral and neural manipulation extensively, traveling as far as France to take courses from Jean Pierre Barral. She is also a registered yoga teacher, having trained at the Yoga Center of Seattle and It’s Yoga. Additionally, she has accumulated months of time at intensive meditation retreats. Nari’s approach to the body is holistic and eclectic while being well-rooted in research.

Over the last five years, there has been a groundswell in the recognition that healthcare for those in the LGBTQ+ community has been, at best, incredibly lacking & the world of physical therapy is no exception. Fortunately, this growing awareness is being followed by tangible efforts to improve the quality of care provided to this population as evidenced by the formation of PT Proud, a Catalyst Group in the APTA, & a growing body of research to address the unique needs of LGBTQ+ patients. Hermann & Wallace is even offering its first-ever 2-day course solely focused on treating patients who are gender diverse!
However, it is not uncommon for people to feel overwhelmed by all of the changing terminology & fear of accidentally offending someone. Thus, despite good intentions, many providers find themselves avoiding education & discussion of this topic altogether. The problem with this is that every clinician will inevitably encounter someone who is LGBTQ+ & merely “treating everyone the same '' may inadvertently end up causing harm. This is especially pertinent to pelvic health practitioners as we work on highly personal & vulnerable areas of the body. There are countless reasons why it is a worthwhile endeavor to share your knowledge on this topic which is discussed more thoroughly in a blog post I wrote a few years ago (here), but this post will focus more on practical takeaways that you can implement in your practice.
As mentioned earlier, the terminology can be intimidating; let's break them below into two categories: gender and sexual minorities:
- Sex - biological characteristics of chromosomes & anatomy (ie. male, female, intersex)
- Gender - societal & cultural catego
- rization based on one’s sex (ie. man, woman, non-binary)
- Cisgender - one who identifies with the gender assigned to them at birth
- Intersex- someone born with aspects of both male & female anatomy (i.e. external vulva & internal testes)
- Transgender - one whose gender does not match the sex they were born with (maybe abbreviated trans; this includes people who are non-binary)
- AFAB- assigned female at birth
- AMAB- assigned male at birth
- Transwoman/MTF - assigned male at birth & identifies female
- Transman/FTM - assigned female at birth & identifies male
- Non-binary- one who identifies as neither male nor female; may use gender-neutral pronouns (they/them)
- Top surgery - breast removal (typically FTM) or augmentation (typically MTF)*
- Bottom surgery - reassigning one’s genitalia to the anatomy they identify with
- Gender identity - the gender that someone associates with internally
- Gender expression - the external gender that someone conveys through appearance & behavior
- *Non-binary folks may also undergo various gender affirmation surgeries & /or take hormones.
- Sexual orientation - the gender(s) that one is attracted to. (Transgender is not a sexual orientation.)
- Lesbian- a woman attracted to other women
- Gay- a man attracted to other men
- Bisexual- a person attracted to both men and women
- Pansexual- someone attracted to people regardless of their gender identity
- Asexual- a person who is not sexually attracted to others; may still experience romantic attraction
- Queer- an umbrella term that applies to all LGBTQ+ people; used as a sexual orientation when other labels are not accurate; may be perceived as a derogatory slur, especially among older individuals
There can be many combinations of the terms above. Someone could identify internally as male but live outwardly as a woman for a variety of reasons including safety, cost of transition, etc. Also, gender & sexual orientation do not always pair up in a heteronormative fashion. A person could be cisgender & bisexual (a woman AFAB attracted to both men & women) or transgender & lesbian (a transwoman AMAB attracted to women). Furthermore, not all people who are transgender have surgery or undergo hormone therapy, but this does not change their gender identity. Some helpful visuals to understand these ideas are the Gender Unicorn (here) & the Genderbread Person (here).
Now that you have some context to work with, what else can you do to put patients at ease?
- Consider having a rainbow flag in the waiting room to let patients know they are in a safe space
- Wear a small pin indicating that you are an ally.
- Have inclusive intake forms with a blank space to enter gender rather than a checkbox for male or female.
- If applicable, know where gender-neutral bathrooms are located & inform patients.
Ultimately, the best method to provide compassionate and competent care is to minimize your assumptions. There are many things you can do in your day-to-day interactions with patients to convey that you are trying to open up your worldview. For example, if you find yourself assuming someone’s gender identity based on their name or appearance, I’d challenge you to practice using the gender-neutral they/them pronoun until you learn how they identify. If you are unsure, it is okay to privately ask them! This is far less triggering than misgendering someone. Another common microaggression is assuming a patient’s partner’s gender based on heteronormative values. Try using the terms “spouse” or “partner” when talking to a patient about their loved one(s). It may seem banal to you, but your LGBTQ+ patients will notice.
Disclaimer: I can only represent the part of the community that I identify with. The views expressed are my informed opinions & may not be generalizable to all LGBTQ+ persons. I am thankful to be given a platform to address a topic that is so rarely discussed, but if I have made any errors or misrepresentations, please correct me!
My course will provide a safe space to ask all the questions about caring for LGBTQ+ patients and practicing the skills needed to help advance your practice. Join me for Inclusive Care for Gender and Sexual Minorities next scheduled for June 8th.
AUTHOR BIO:
Brianna Durand, PT, DPT
 Brianna Durand, PT, DPT earned her Doctor of Physical Therapy at Texas Woman’s University in Houston, TX. During graduate school, she led and co-founded PT Proud, a Catalyst Group within the Health Policy and Administration Section of the APTA, to improve the education, equity, and inclusion of LGBTQ+ patients, students, and clinicians.
Brianna Durand, PT, DPT earned her Doctor of Physical Therapy at Texas Woman’s University in Houston, TX. During graduate school, she led and co-founded PT Proud, a Catalyst Group within the Health Policy and Administration Section of the APTA, to improve the education, equity, and inclusion of LGBTQ+ patients, students, and clinicians.
Brianna owns and operates Empower Physiotherapy, a private practice in Seattle. As a competitive powerlifter, Brianna enjoys working with strength athletes who experience pelvic floor dysfunction, especially stress incontinence. She is passionate about providing care to individuals in the LGBTQ+ community, including those undergoing hormonal/surgical transition. Additional clinical interests of hers include prenatal/postpartum care for trans and gender-nonconforming folx and pelvic floor care for patients that are intersex. In her spare time, Brianna enjoys playing board games, lifting heavy, and watching stand-up comedy.
Working with survivors of sexual violence has been the most challenging and rewarding aspect of my pelvic rehabilitative work. I am fortunate to have been trained as a legal and medical advocate for sexual assault survivors and worked in mental health before becoming a physical therapist. I hope to give everything I know about being a patient-centered trauma-aware practitioner.
Can we talk about how common sexual violence is within our society and our work? I can spout the statistics: 1 in 4 women and about 1 in 26 men have experienced completed or attempted rape. About 1 in 9 men were made to penetrate someone during his lifetime. Additionally, 1 in 3 women and about 1 in 9 men experienced sexual harassment in a public place.1 But in our rooms, sexual violence is pandemic.
Please feel empowered to provide appropriate, trauma-informed support to these patients. It starts with our wellness and self-care. We cannot empower others if we have not empowered ourselves. We don’t have to be perfect. Practice self-forgiveness. Know your triggers. Commit to impeccable self-care. Be well. Keep ourselves safe by practicing empowered choice. If you have empowered choice, you can provide and teach empowered choice to your patients. What is empowered choice? Empowered choice is saying: we don’t do anything you don’t want to do, or I don’t do anything I don’t want to do. Ever. Give your patient the power to direct their healing while providing extensive physiology and anatomy education with trauma-focused, patient-centered care. With information, patients choose what they want to be treated and when. And with empowered choice, they tend to choose higher-level treatment quicker.
Additionally, they may show up to more appointments and, from my experience, they get better faster. I know we all do this with informed consent, but I have found success with being immensely purposeful in repeatedly telling the patient that they are in control of the treatment. Patients are completely in control of the treatment, not to be confused with being in control of me.
After empowered choice, normalizing their experience is valuable for our treatment relationship. This is possibly the saddest part of this work- how normal it is for my patients to have sexually violent experiences. I say over and over how typical it is for patients to have experienced sexual violence and how it negatively affects pelvic function. I also say they don’t need to tell me anything about their trauma and that I don’t require them to go to counseling to participate in pelvic rehab. I do, however, let them know if they want to disclose their traumas or be connected to resources, I will gladly assist in their support. I do let them know that there are times I have to report (I live in a mandated reporting state) and tell them exactly what my rules are. Being clear and informative while being supportive and trauma-informed helps reduce the SHAME patients who experienced sexual violence carry. These patients typically feel embarrassed and ashamed by the abuse perpetrated against them in addition to the physical somatization from the trauma. And that their response during treatment is a normal response to an abnormal situation.
Take care of you. Empowered choice for all involved. Normalize the survivors’ response. Disempower Shame. Join me for Trauma Awareness for the Pelvic Therapist if you want more science and skills for patient care the next course is scheduled for May 11-12th.
Reference:
Fast Facts: Preventing Sexual Violence | Violence Prevention | Injury Center | CDC. (n.d.). https://www.cdc.gov/violenceprevention/sexualviolence/fastfact.html#:~:text=One%20in%204%20women%20and,Sexual%20violence%20starts%20early.
AUTHOR BIO:
Lauren Mansell DPT, CLT, PRPC
 Lauren received her Doctor of Physical Therapy degree from Governors State University and a Bachelor's Degree in Psychology and Sociology from Northwestern University. Before becoming a physical therapist, Lauren counseled suicidal and homicidal SES at-risk youth who had survived sexual violence. Lauren was certified as a medical and legal advocate for sexual assault survivors in 1999 and has advocated for over 130 sexual assault survivors of all ages in the ED. Lauren's physical therapy specialty certifications include Certified Lymphedema Therapist (CLT), Pelvic Rehabilitation Professional Certificate (PRPC), and Certified Yoga Therapist (CYT). She is a board member of the Chicagoland Pelvic Floor Research Consortium, American Physical Therapy Association Section of Women's Health and Section of Oncology, and is a 2017 Fellow of the Chicago Trauma Collective. Her goal as a trauma-sensitive practitioner is to empower patients to create meaningful, healthful lifestyle changes to improve their physiology and wellness.
Lauren received her Doctor of Physical Therapy degree from Governors State University and a Bachelor's Degree in Psychology and Sociology from Northwestern University. Before becoming a physical therapist, Lauren counseled suicidal and homicidal SES at-risk youth who had survived sexual violence. Lauren was certified as a medical and legal advocate for sexual assault survivors in 1999 and has advocated for over 130 sexual assault survivors of all ages in the ED. Lauren's physical therapy specialty certifications include Certified Lymphedema Therapist (CLT), Pelvic Rehabilitation Professional Certificate (PRPC), and Certified Yoga Therapist (CYT). She is a board member of the Chicagoland Pelvic Floor Research Consortium, American Physical Therapy Association Section of Women's Health and Section of Oncology, and is a 2017 Fellow of the Chicago Trauma Collective. Her goal as a trauma-sensitive practitioner is to empower patients to create meaningful, healthful lifestyle changes to improve their physiology and wellness.
In the realm of rehabilitation, where innovative methods continuously emerge, one particular approach stands out for its unique blend of traditional wisdom and modern science: hippotherapy improves function for people who have experienced trauma. This unconventional form of therapy harnesses the healing power of horses to aid individuals in overcoming physical and emotional trauma while working on their rehabilitation goals. From veterans grappling with post-traumatic stress disorder (PTSD) to survivors of abuse or accidents, hippotherapy has shown remarkable efficacy in promoting function, healing, and resilience.
Understanding Equine-Assisted Therapy Versus Hippotherapy:
Equine-assisted therapy involves interaction with horses in a structured environment under the guidance of trained mental health therapists. Unlike traditional therapy settings, the presence of horses creates a dynamic and immersive experience that facilitates emotional expression within the mental health realm. Hippotherapy is a treatment tool used by physical therapists, occupational therapists, and speech-language therapists to address impairments, functional limitations, and disabilities in clients with neuromusculoskeletal dysfunction (AHA). Unlike equine-assisted therapy focused on mental health, hippotherapy is a tool that uses evidence-based practice and clinical reasoning in the purposeful manipulation of equine movement as a therapy tool to engage sensory, neuromotor, and cognitive systems to promote functional outcomes.
The Bond Between Humans and Horses:
Horses, known for their sensitivity and intuition, possess a remarkable ability to mirror human emotions and respond to nonverbal cues. This unique quality forms the foundation of equine-assisted therapy and hippotherapy, where the therapeutic relationship between humans and horses serves as a catalyst for healing.
Physical Benefits of Hippotherapy:
For individuals recovering from physical trauma or injury, interacting with horses can offer a range of physical benefits. The rhythmic motion of a pelvis on the horse’s back mimics the tri-planar movement of walking, helping to improve balance, coordination, and muscle strength. Additionally, the movement of the horse provides a passive range of motion to the pelvic muscular joint. Additionally, grooming and caring for horses provide opportunities for gentle exercise and fine motor skill development.
Addressing Emotional Trauma:
Beyond its physical benefits, hippotherapy is particularly effective in addressing emotional trauma while working towards rehabilitation goals. Horses, as prey animals, are highly attuned to their surroundings (neuroception) and can sense fear, anxiety, or distress in humans (interoception). Through interactions with horses, individuals are encouraged to experience their emotions in a safe and supportive environment.
Building Trust and Confidence:
For trauma survivors, rebuilding trust and self-confidence can be a challenging journey. Horses, with their nonjudgmental nature and unconditional acceptance, offer a unique platform for survivors to develop trust and assertiveness. As survivors learn to communicate effectively with horses, they often experience a newfound sense of empowerment and self-worth.
Case Studies:
Numerous case studies and anecdotal evidence attest to the transformative impact of horse-assisted therapy on trauma recovery. Veterans struggling with PTSD have reported reduced symptoms and improved coping mechanisms after participating in equine-assisted programs. Similarly, survivors of abuse or accidents have found solace and healing through their interactions with horses.
The Science Behind Working with Horses:
While the healing power of horses has been recognized for centuries, modern research is beginning to unravel the science behind equine-assisted therapies including hippotherapy. Studies have shown that interactions with horses can lead to decreased levels of stress hormones, such as cortisol, and increased production of endorphins and oxytocin, often referred to as the "love hormone." These physiological changes contribute to a sense of relaxation and emotional well-being
Conclusion:
In a world where trauma and adversity are all too common, innovative approaches to rehabilitation are essential for promoting healing and resilience. Hippotherapy offers a holistic and experiential approach to trauma recovery, addressing both the physical and emotional aspects of healing. As the evidence supporting its efficacy continues to grow, hippotherapy stands as a beacon of hope for individuals on the path to healing.
In the serene presence of these majestic creatures, individuals find solace, strength, and a renewed sense of purpose. In the dance between human and horse, healing takes flight, one hoofbeat at a time.
 Lauren Mansell, PT, DPT, CLT, PRPC utilizes her horse Maggie as the tool of Hippotherapy for her pelvic, oncology, and lymphatically dysfunctioned patients through her private practice in Frankfort, IL. Lauren took Hippotherapy I and II in Lexington, KY in 2010 and 2011 respectively. Working with patients with high trauma rates, utilizing hippotherapy has been a tool to help patients create safety within their bodies. Lauren has spent over 25 years working with people who have experienced severe trauma and has developed Trauma Awareness for the Pelvic Therapist to increase trauma awareness and the ability to provide appropriate physical therapy for trauma survivors.
Lauren Mansell, PT, DPT, CLT, PRPC utilizes her horse Maggie as the tool of Hippotherapy for her pelvic, oncology, and lymphatically dysfunctioned patients through her private practice in Frankfort, IL. Lauren took Hippotherapy I and II in Lexington, KY in 2010 and 2011 respectively. Working with patients with high trauma rates, utilizing hippotherapy has been a tool to help patients create safety within their bodies. Lauren has spent over 25 years working with people who have experienced severe trauma and has developed Trauma Awareness for the Pelvic Therapist to increase trauma awareness and the ability to provide appropriate physical therapy for trauma survivors.
Join Lauren In the remote course scheduled for May 11th to take a deep dive into the science of trauma.

The 2024 Summer Olympics this summer (July 26 - August 11) will showcase the most elite athletes from all over the world. We will watch these athletes perform at World and Olympic Record times in various running events from sprints to long distances. These athletes demonstrate above-average form and strength, allowing their bodies to perform at peak ability. While these individuals are far above average, there is still the risk of dysfunction, including pelvic floor dysfunction, that can occur as a result of poor running form and from lower extremity injuries. Poor form can affect even the highest-level runners.
Recently, I co-treated a 32-year-old patient who was 4 months postpartum, with a pelvic therapist. Before childbirth, the patient was an avid runner participating in multiple running events who ran distances from 5k to a marathon. Since giving birth, the patient had complaints of increased urinary urgency and increased urinary frequency, having to urinate 11-14x/day and a minimum of 2x during the night. The patient still had not returned to running due to poor bladder control. This patient’s running evaluation demonstrated the following:
- ·Running video analysis: overstriding, bilateral hip drop, increased vertical displacement, and a heel whip on the left side.
- ·Movement assessment of squat: increased lumbar lordosis and increased sacral counternutation uncontrolled.
- ·Movement assessment of pistol squat: bilateral hip drop and bilateral genu valgum
- ·Musculoskeletal assessment: decreased gluteus medius and maximus strength, decreased motor control of left greater than right hip rotators.
This patient was seen for a total of 7 visits over 4 months, receiving a combination of therapy focusing on the above deficits and pelvic therapy. By the end of physical therapy, the patient had no complaints of urinary frequency/urgency, demonstrated improved squat, pistol squat, and running form as well as significant gains in lower extremity strength.
In the remote course, The Runner and Pelvic Health, Aparna Rajagopal and I will discuss the various assessments and treatments that we provide for runners and for this patient too. We will perform video analysis of runners, discuss postpartum runners, and learn strength and conditioning exercises specific to runners. Join us on April 27, 2024 to expand your knowledge on the treatment of runners from a pelvic health perspective.
AUTHOR BIO:
Leeann Taptich DPT, SCS, MTC, CSCS

Leeann Taptich has been a physical therapist since 2006. She graduated with a BS in Kinesiology from Michigan State University and a Doctorate of Physical Therapy from the University of St Augustine. In 2009, she earned her Manual Therapy from the University is St Augustine and her board certification as a Sports Certified Specialist in 2018.
Leeann leads the Sports Physical Therapy team at Henry Ford Macomb Hospital in Michigan where she mentors a team of therapists. She also works very closely with the pelvic team at the hospital which gives her a very unique perspective of the athlete. With her combination of credentials and her exposure to pelvic health, she is able to use a very eclectic but complete approach in her treatment of orthopedic and sports patients. With the hospital system, she is involved with the community promoting health and wellness at local running competitions and events.
Leeann is passionate about educating and teaching and has assisted in teaching multiple courses at the local State University PT department. She is co-chair of the continuing education committee at her hospital where she writes and develops courses. She is co-author with Aparna Rajagopal of the Breathing and Diaphragm and The Runner and Pelvic Health remote courses at Herman & Wallace.
Leeann lives in the metro Detroit area with her husband and 2 children. She enjoys hiking, traveling, and watching football.

HWConnect 2025 is scheduled for March 28-30, 2025 in Seattle Washington. Register before April 1 to save money with early bird pricing!
Are you ready to level up your professional game and connect with industry leaders from around the world? Look no further than HWConnect 2025 - the must-attend event of the year for anyone serious about staying ahead of the curve. In this article, we'll walk you through everything you need to know about registering for HWConnect 2025 and securing your spot for an unforgettable experience. From speakers and breakout sessions to networking opportunities and registration details, we've got you covered. Get ready to immerse yourself in three days of innovation, education, and networking that will leave you inspired and empowered. Don't miss out - let's dive in!
Why Attend HWConnect 2025
At HWConnect 2025, you'll have the opportunity to engage with top-notch keynote speakers and insightful sessions that will expand your knowledge and skills in the industry. Let's take a closer look at what you can expect from this year's lineup.
Speakers and Sessions
HWConnect 2025 will feature a lineup of speakers who are experts in their respective fields, offering valuable insights and cutting-edge strategies to help you elevate your career. The sessions planned for the 2025 event will cover a wide range of topics, from emerging trends to practical tips for success.
Sunday’s Keynote Speaker, Leticia Nieto Psy.D., LMFT is booked! Dr. Nieto is a leadership coach, psychotherapist, and educator specializing in liberation and equity, cultural responsiveness, motivational patterning, and evolutionary creativity. Her book, Beyond Inclusion, Beyond Empowerment is an accessible analysis of oppression that offers readers ways to develop skills for social justice. She is recognized for her expertise in addressing social justice from a developmental ecological perspective including orienting to systemic transformation, survivance, song and poetry, relational repair, joy, radical rest, intersectional coalition, and reparative and restorative justice
We are continuing to confirm our speaker line-up and have lots of exciting topics in the works.
Here’s what participants last year said about the speakers:
- "I enjoyed the opportunity to collaborate and meet/network with local therapists in my area. The content is very applicable to my practice and a great way to get a "taste" of other courses offered through H&W I may want to take in the future." -Stephanie Nguyen
- "I found this conference so educational, inspiring, motivating, and gave me a great opportunity to make professional connections to help me to better address my more complex patients' concerns." -Cydney Dashkoff
In addition to speakers, HWConnect will feature break-out sessions and opportunities for hands-on learning. Look for station-style break-outs including rehabilitative US, squat analysis for various pelvic floor dysfunctions, and a workshop on inclusivity in intake forms and clinical interviewing, all led by HW faculty.
We will also be offering morning yoga and meditation sessions so that attendees can ground themselves before a big day of learning.
Registration Details and Early Bird Pricing
For those eager to secure their spot at HWConnect 2025, here are the registration details and early bird pricing you need to know. Early bird pricing is available for a limited time and will end at midnight on March 31st, so act fast to take advantage of the discounted rate of $595. Be sure to reserve your spot early to lock in your attendance and save on registration fees. After securing your spot, you'll be ready to make the most of the networking opportunities available at HWConnect 2025.
Networking Opportunities
After securing your spot, you'll be ready to make the most of the networking opportunities available. HWConnect 2025 offers a unique chance to connect with industry leaders, experts, and fellow attendees, creating valuable relationships that can last long after the event is over.
- "It was a great time! Interesting topics and research, well thought out, and planned schedule. Loved the intro music selections!!!!! Great energy from the speakers." -Stephanie Rutherford
Preparing for HWConnect 2025
As you prepare for HWConnect 2025, it's essential to maximize your experience by setting goals and planning ahead. Consider what you hope to achieve at the event, whether it's learning from industry leaders, making valuable connections, or gaining insights to advance your career. Take some time to research the speakers, panel topics, and activities scheduled for the event so you can make informed decisions about how to best allocate your time.
Additionally, make sure you have all the necessary materials ready for the conference. This could include business cards, a notebook, pens, and any relevant documents or presentations you may need. Being organized and prepared will allow you to focus on making the most of your time at HWConnect 2025 without any last-minute scrambling.
Lastly, take the opportunity to set some personal and professional goals for the event. What do you hope to learn or accomplish during your time at HWConnect 2025? By setting clear objectives, you'll be able to stay focused and make the most of the networking opportunities and valuable insights available to you. Get ready to make the most of your time at HWConnect 2025 and further your success in the industry.
Don't miss out on the opportunity to be a part of HWConnect 2025 - register now to secure your spot and take advantage of early bird pricing before April 1st. Get ready for three days filled with innovation, education, and networking that will leave you inspired and empowered. Join us at HWConnect 2025 and be a part of something truly unforgettable. Register now and get ready to connect, learn, and grow. See you there!

Who are you? Describe your clinical practice.
Hi! I’m Molly O’Brien-Horn. I’m a Pelvic Health Physical Therapist practicing in an outpatient hospital-based clinic in California. I work with patients of a variety of ages, gender identities, and body variations.
What has your educational journey as a pelvic rehab therapist looked like and how did you get involved in the pelvic rehabilitation field?
I started my career in pediatrics and outpatient orthopedics. I began to notice that those patient populations also had pelvic floor dysfunction, in addition to the diagnoses I was seeing them for. I was fortunate enough to shadow a colleague at the time who did pelvic health. That colleague recommended I take Pelvic Function Level 1 with Herman & Wallace, which I did, and I loved it. During the course, I decided that Pelvic Health was what I wanted to do with my life and the rest is history.
What patient population do you find most rewarding to treat and why?
I know it may sound cliché, but variety is the spice of life, right? I like having the ability to treat a variety of diagnoses within the pelvic health field and be able to help as many different people from as many different walks of life as possible. Being able to treat people of all gender identities, sexual orientations, ability levels, body variations, ages, etc. within the pelvic health field is what’s the most rewarding to me.
What lesson have you learned in a course, from an instructor, or from a colleague or mentor that has stayed with you?
Learning how to practice from a trauma-informed lens has really stayed with me. I’ve been fortunate enough to take multiple courses over the years that centered around trauma-informed care. Trying to practice from a trauma-informed lens, especially when working with patient populations who may have experienced trauma or abuse in their lifetime has been so helpful for my practice and growth as a healthcare provider and as a person.
Now that we know a little bit about you, can you tell us about your new course Intersex Patients: Rehab and Inclusive Care?
What made you want to create this course?
I’ve been to plenty of courses about LGBTQIA+ healthcare and Gender-Affirming Care for LGBTQIA+ folx, but I started to notice that Intersex folx were only briefly mentioned if they were mentioned at all. Healthcare providers need to be better educated on how to provide Intersex-Affirming Healthcare and to learn how to be better allies in healthcare to Intersex folx. They also need to be educated on the healthcare needs that are unique and specific to Intersex patient populations, as those needs may be different than non-Intersex LGBTQIA+ folx, and I wanted to make a course to address that.
What need does your course fill in the field of pelvic rehabilitation?
My course fills a gap in healthcare education about how to provide Intersex-Affirming Healthcare and hopefully helps healthcare workers learn how to be better allies to Intersex folx. Many courses don’t address Intersex-specific needs and wishes in healthcare, and I my course can address that. In the course, I’ve included resources, interviews, and quotes from multiple Intersex folx, activists, and advocacy organizations, as well as research from international human rights groups. I wanted this course to include a variety of Intersex voices from different people across different walks of life so that Intersex folx could discuss their specific wishes, asks, and needs from healthcare providers who are working with Intersex folx.
Who, what demographic, would benefit from your course?
Any healthcare provider can benefit from my course, especially pelvic health providers. I wanted as much of my course to be applicable to as many healthcare providers in different fields and different countries as possible. However, some of the treatments may be geared more towards pelvic health providers since I’m a pelvic health PT in the U.S. and that’s the lens I work through.
What message do you want to send to practitioners who take your course?
I want practitioners to know that I hope they enjoy the course, learn something new, and that they walk away from the course as a better ally in healthcare and as a better Intersex-affirming healthcare provider.
Anything else you want to tell us?
I’m just very grateful for this opportunity to teach with Herman & Wallace and debut this course. I really hope that everyone learns and enjoys the course. And I can’t wait to see everyone for the course's inaugural date on May 4th!

As Rehab professionals we help our patients by listening to them, allowing them space to hear their body's wisdom, and educating them on how their bodies work. When it comes to educating people about their bodies, we often use pictures, models, and verbal explanations of movement and function. In addition, one of the best ways we can teach them about how they move is by actually touching them. By allowing them to learn where they are holding greater tone or how to move in a different way, we give them insight into their body and give them a way to move forward in their recovery.
Manual therapy is a modality that we can utilize to help a patient become aware of a part of their body that they did not realize they had the ability to control or change. Take the example of living next to an airport – after a while we may not hear the planes anymore – now take this example to our bodies. Many of us, including our patients, are not aware of the way we hold our bodies. We are unaware that we are holding increased tension in our body and that we have the ability to control the muscle activity of our body. By using manual therapy, we help the patient gain access to the part of their body and help them learn how to manage or change that part of their body.
Fascia is defined as “a three-dimensional continuum of connective tissues present everywhere throughout the body, from the head to the toes and from the skin to the bone.” 1, 2 When reading about the attachments of the abdominal fascia we learn that there are connections from the abdomen to the breathing diaphragm, the pelvic floor region, and the lateral hip.3, 4 By addressing the abdominal wall superficial fascia, deep fascia, and abdominal muscles we can also assist these other areas of the body. Improving breathing, trunk mobility, the pelvic girdle, and the function of the genitourinary and gastrointestinal systems to name a few.
With our trained Rehab eye, we often see that folks have developed patterns of movement that are not beneficial for the way they need to function in their lives. We as humans really cannot see ourselves and may not be aware of how we are moving, how we might be bracing, protecting, or limiting movement. In pelvic rehab, if a patient has IC/PBS, endometriosis, dysmenorrhea, or has had an abdominal surgery they may unknowingly hold their abdominal myofascial tissues in a way that limits their movement for bending, reaching, and lifting. If those tissues have greater tone or restriction, they may limit the power the muscles can generate, or the coordination needed to assist with bowel movements or relaxation needed for insertion into a canal for intimacy or exam.
As Rehab professionals we have learned some basic interventions to address the myofascial tissues of the body, but when it comes to applying those techniques to the abdominal wall we sometimes are at a loss about how and when it is safe to touch the abdominal wall. In this one-day course, Manual Therapy for the Abdominal Wall, we take the skills we learned to address the myofascia in the leg, neck, and back and apply them to the abdominal wall. We discuss precautions, things to consider/monitor and discuss how to touch. By connecting in this way, the patient is then able to become aware and you as the therapist can help them improve their movement and improve their function.
- This class has no prerequisites and while it is a beginner class, it has been appreciated by the experienced pelvic health provider wanting to review basic myofascial techniques application to the abdominal wall.
- This class was developed as a way for folks to hone their manual skills by applying them to the abdominal wall and then you can take those techniques and connect them to the perineum and the thorax. We utilize lectures, videos, and practice in this course.
Join me on the April 27th or October 20th to take your skills to the next level!
Resources:
- Kirchgesner, T., Demondion, X., Stoenoiu, M. et al. Fasciae of the musculoskeletal system: normal anatomy and MR patterns of involvement in autoimmune diseases. Insights Imaging 9, 761–771 (2018). https://doi.org/10.1007/s13244-018-0650-1
- Adstrum, S., Hedley, G., Schleip, R., Stecco, C., & Yucesoy, C. A. (2017). Defining the fascial system. Journal of bodywork and movement therapies, 21(1), 173-177.
- Stecco, C. (2020). Fascial Anatomy. In Fascia, Function, and Medical Applications (pp. 19-30). CRC Press.
- American Osteopathic Association. (2010). Foundations of osteopathic medicine. A. G. Chila (Ed.). Lippincott Williams & Wilkins
COURSE TESTIMONIALS:
- “This class was fantastic. It covered many immediately applicable tools that can be used on a wide range of patients in the clinic. I really liked the videos of assessment and intervention that Tina provided, as well.”
- “The course was wonderful Tina was extremely kind and generous with her knowledge and feedback, taking time for questions even if it meant not taking a break herself. The videos were super helpful, as is the manual. Thank you so much!”
- “It was a great course and instructor is very knowledgeable.”
- “Great mix of anatomy review and then applying the concepts to patient care.”
AUTHOR BIO:
Tina Allen, PT, BCB-PMD, PRPC Tina Allen, PT, BCB-PMD, PRPC has been a physical therapist since 1993. She received her PT degree from the University of Illinois at Chicago. Her initial five years in practice focused on acute care, trauma, and outpatient orthopedic physical therapy at Loyola Medical Center in Illinois. Tina moved to Seattle in 1997 and focused her practice in Pelvic Health. Since then she has focused her treatment on the care of all genders throughout their life spans with bladder/bowel dysfunction, pelvic pain syndromes, pregnancy/ postpartum, lymphedema, and cancer recovery.
Tina Allen, PT, BCB-PMD, PRPC has been a physical therapist since 1993. She received her PT degree from the University of Illinois at Chicago. Her initial five years in practice focused on acute care, trauma, and outpatient orthopedic physical therapy at Loyola Medical Center in Illinois. Tina moved to Seattle in 1997 and focused her practice in Pelvic Health. Since then she has focused her treatment on the care of all genders throughout their life spans with bladder/bowel dysfunction, pelvic pain syndromes, pregnancy/ postpartum, lymphedema, and cancer recovery.
Tina’s practice is at the University of Washington Medical Center in the Urology/Urogynecology Clinic where she treats alongside physicians and educates medical residents on how pelvic rehab interventions will assist clients. She presents at medical and patient conferences on topics such as pelvic pain, continence, and lymphedema. Tina has been faculty at Herman & Wallace Pelvic Rehabilitation Institute since 2006. She was the physical therapist provider for the University of Washington on a LURN Multi-Center study for Interstitial Cystitis/Painful Bladder Syndrome treatment with physical therapy techniques. Tina was also a co-investigator for a content package on pain education for the NIDA/NIH on the treatment of pelvic pain.
For the past 20 of my 49 years as a physical therapist, I have been focusing on osteoporosis management thanks to the intervention of Sara Meeks who began studying osteoporosis in the 1980s before it was even a “thing.” The WHO did not identify osteoporosis as a systemic disease until 1993! About 15 years ago, after attending all of Sara’s Osteoporosis seminars, she selected my current business partner, Frank Ciuba, and I to “carry the torch.” Since then, we have been teaching her course with updated evidence, additions, and new research as it becomes available.
According to the Bone Health and Osteoporosis Foundation, 50% of individuals over age 50 are diagnosed with low bone density (osteopenia or osteoporosis) and many assume the only therapy option is medication.
Not so fast!
While some individuals may need bisphosphonates or anabolic drugs to get control of their rapidly decreasing bone strength, everyone can benefit from exercise. And research is showing that exercise can slow bone density loss and even help increase it. But it must be the right exercise, performed correctly and consistently.
Even though strength training consisting of high-intensity resistance and impact training (HiRIT) has been shown to build bone, it is not traditionally recommended for individuals with osteoporosis because of the perceived high risk of fracture.
Today I want to talk about the LIFTMOR Trial. LIFTMOR stands for Lifting Intervention For Training Muscle and Osteoporosis Rehab. This program, from Australia, utilizes brief, bone-targeted HiRIT with impact loading for post-menopausal women with low bone mass. It found that there was an increase in bone density compared to the more traditional low-intensity exercise program, and no adverse effects other than one report of minor lower back spasm. Additionally, functional measures such as TUG, 5 Times Sit-to-Stand, and Functional Reach improved.
As rehab practitioners, and especially PTs and OTs treating people with fragile bones, when it comes to exercise prescription, the question is often, “How much is too much?” As the ancient Greek physician, Hippocrates said, “Primum non nocere.” First, do no harm! So often we default to being gentle with our elderly, frail population in order to not harm them. Don’t get me wrong. I’m not saying we should have them all doing Burpees! One of the standout aspects of the LIFTMOR trial was lifting weights at 85% of 1 Rep Max compared to the Control group who worked at 65% of their 1 Rep Max. The report, according to the American Society for Bone and Mineral Research in 2017 reads: Contrary to current opinion, HiRIT was efficacious and induced no adverse events under highly supervised conditions for our sample of otherwise healthy postmenopausal women with low to very low bone mass.
“Highly supervised conditions.” I think that’s the key. We must make sure that our patients are educated and can demonstrate proper alignment and body mechanics. And of course, we must provide the correct exercises. And then increase the weights methodically with continued supervision to load the bones once our patients have the proper technique. Many patients (and therapists) want to know, does exercise really build bone density? Not to be coy, but my answer is often, “It depends.”
It depends on whether it’s the right exercises, performed with proper technique, and good compliance by the patient. Then yes, exercise does build bone density. One of our challenges though, is in trying to follow the evidence, is that “Exercise” means many different things to different people. Even the professionals! Teaching the wrong exercises can be unsuccessful at best and possibly catastrophic (causing a fracture) at worst!
That’s why Frank and I, with Sara’s blessing, created this program that is exercise-specific, based on solid evidence, and one that can be shifted into gear first thing on Monday morning.
Osteoporosis Management is scheduled for this spring and fall. Consider joining us in the remote course on April 27th or September 14th. We hope to see you soon!
AUTHOR BIO:
Deb Gulbrandson, PT, DPT has been a physical therapist for over 49 years with experience in acute care, home health, pediatrics, geriatrics, sports medicine, and consulting to business and industry. She owned a private practice for 27 years in the Chicago area specializing in orthopedics and Pilates. 5 years ago, Deb and her husband “semi-retired” to Evergreen, Colorado where she works part-time for a hospice and home-care agency, sees private patients as well as Pilates clients in her home studio and teaches Osteoporosis courses for Herman & Wallace. In her spare time, she skis and is busy checking off her Bucket List of visiting every national park in the country- currently 46 out of 63 and counting.
Deb is a graduate of Indiana University and a former NCAA athlete where she competed on the IU Gymnastics team. She has always been interested in movement and function and is grateful to combine her skills as a PT and Pilates instructor. She has been certified through Polestar Pilates since 2005, a Certified Osteoporosis Exercise Specialist through the Meeks Method since 2008, and a Certified Exercise Expert for the Aging Adult through the Geriatric Section of the APTA.
She can be reached at This email address is being protected from spambots. You need JavaScript enabled to view it.
By accepting you will be accessing a service provided by a third-party external to https://hermanwallace.com/