Rehabilitative ultrasound imaging has been used in clinical practice for well over a decade now. It has been used for core stabilization, as well as with female incontinence patients. In recent years, transperineal ultrasound imaging has emerged as a useful tool for assessing prolapses and identifying other women’s health issues in the anterior compartment.
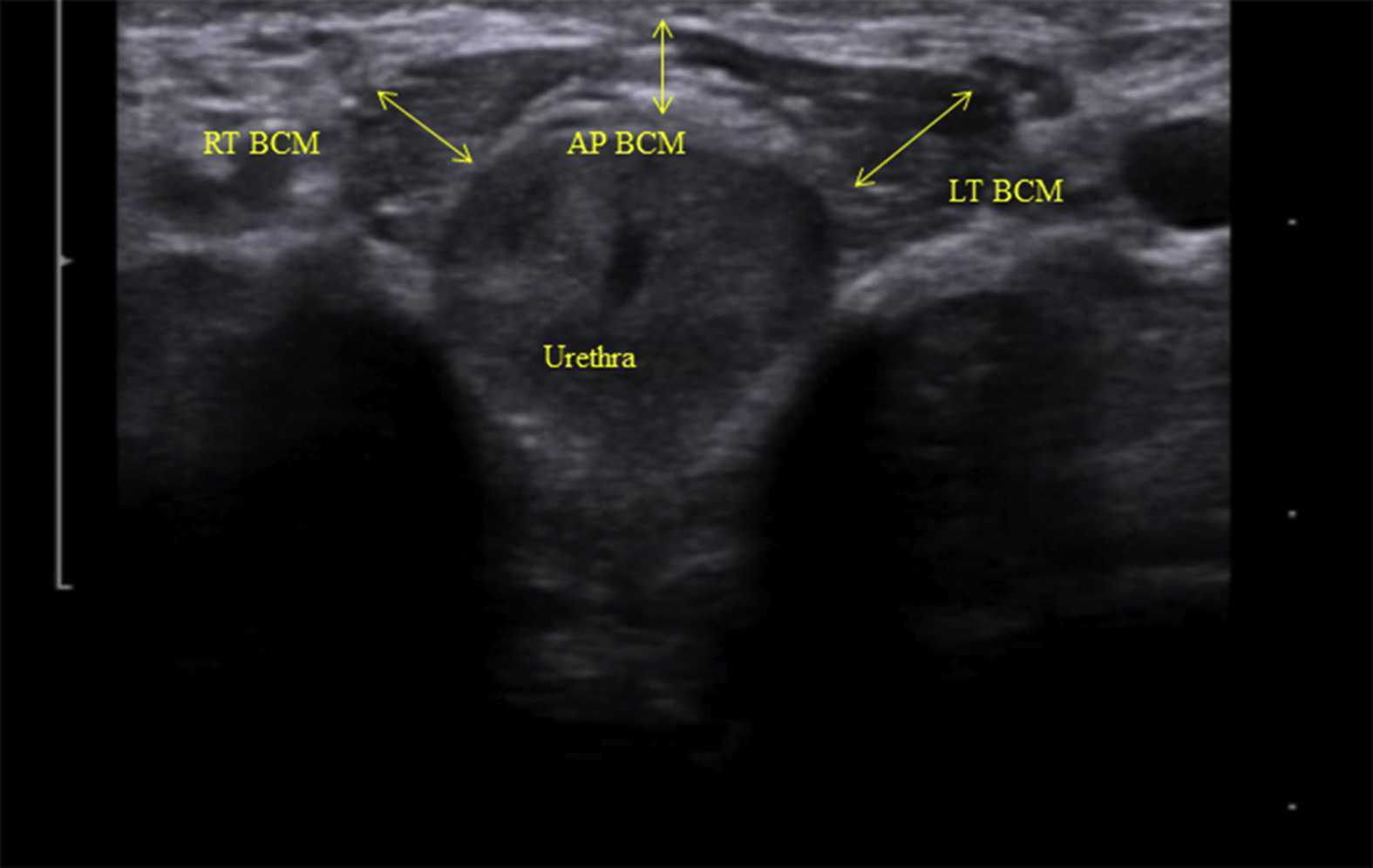
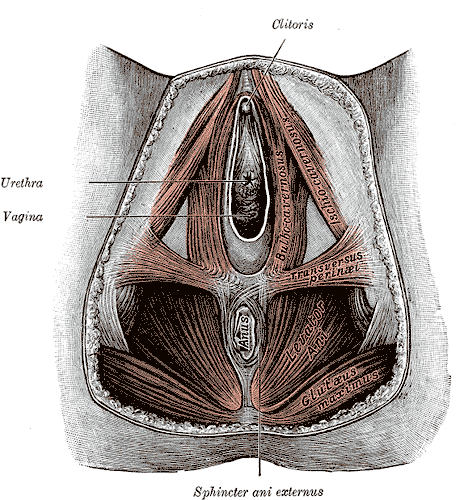
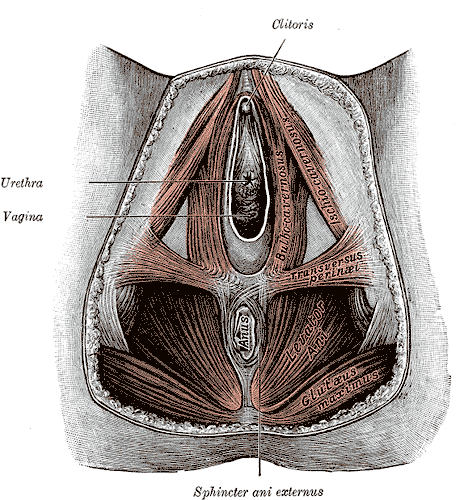
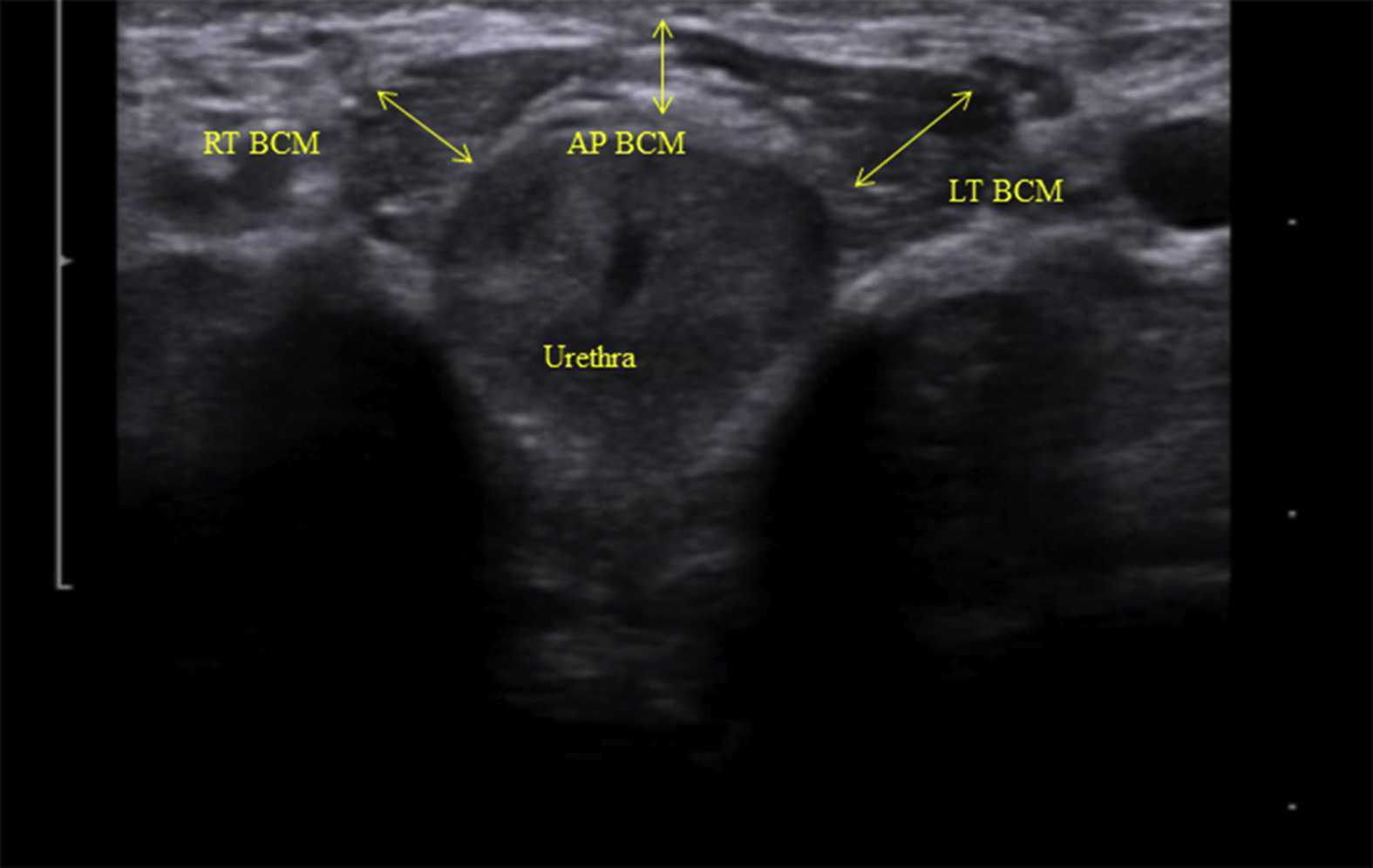 Like other things in men’s pelvic health, the use of ultrasound imaging for rehabilitation has lagged behind that in women’s pelvic health. Ryan Stafford is a researcher that is working to change that. In 2012, Stafford began looking at the normal responses to pelvic floor contractions and what is seen on ultrasound in men. He has since taken his research further to examine differences in men that present with post-prostatectomy incontinence. Stafford, van den Hoorn, Coughlin, and Hodges performed a study looking at the dynamic features of activation of specific pelvic floor muscles, and anatomical parameters of the urethra. The study included forty-two men who had undergone prostatectomy. Some of these men were incontinent and others remained continent. Transperineal ultrasound imaging was used to obtain images of the pelvic structures during a cough, and a sustained maximal contraction. The research team calculated displacements of pelvic floor landmarks with contraction, as well as anatomical features including urethral length, and resting position of the ano-rectal and urethra-vesical junctions.
Like other things in men’s pelvic health, the use of ultrasound imaging for rehabilitation has lagged behind that in women’s pelvic health. Ryan Stafford is a researcher that is working to change that. In 2012, Stafford began looking at the normal responses to pelvic floor contractions and what is seen on ultrasound in men. He has since taken his research further to examine differences in men that present with post-prostatectomy incontinence. Stafford, van den Hoorn, Coughlin, and Hodges performed a study looking at the dynamic features of activation of specific pelvic floor muscles, and anatomical parameters of the urethra. The study included forty-two men who had undergone prostatectomy. Some of these men were incontinent and others remained continent. Transperineal ultrasound imaging was used to obtain images of the pelvic structures during a cough, and a sustained maximal contraction. The research team calculated displacements of pelvic floor landmarks with contraction, as well as anatomical features including urethral length, and resting position of the ano-rectal and urethra-vesical junctions.
The data was analyzed and combinations of variables that best distinguished men with and without incontinence were reported. Several important components were identified in the study. Striated urethral sphincter activation, as well as bulbocavernosus and puborectalis muscle activation were significantly different between men with and without incontinence. When these two parameters were examined together, they were able to correctly identify 88.1% of incontinent men. They further reported that poor function of the puborectalis and bulbocavernosus could be compensated for if the man had good striated urethral sphincter function. However, the puborectalis and bulbocavernosus had less potential to compensate for poor striated urethral sphincter function. This is important for a therapist that works with post prostatectomy patients to know. This can explain part of why some men improve and do so well after a prostatectomy and others don’t, even with therapy to help. If the striated urethra sphincter is damaged and its normal responses are changed during surgery, then incontinence after prostatectomy may be more likely.
Using ultrasound imaging, the therapist can examine and see exactly where a man is deficient in response; whether it is the puborectalis, or the striated urethra sphincter. It is exciting to see this new research and see how rehabilitative ultrasound imaging can influence men’s pelvic health! Come and learn how to use ultrasound imaging for your men’s pelvic health patients as well as your women’s health and back pain patients! You will see how ultrasound imaging can change your practice and how much your patients will enjoy seeing real-time images of their contractions! Thanks to our partnership with The Prometheus Group, this course includes hands-on training on the latest in pelvic ultrasound imaging.
1. Stafford R, Ashton-Miller J, Constantinou C, et al. Novel insights into the dynamics of male pelvic floor contractions through transperineal ultrasound imaging. J. Urol. 2012; 188: 1224-30.
2. Stafford RE, van den Hoorn W, Couglin G, Hodges P. Postprostatectomy incontinence is related to pelvic floor displacements observed with trans-perineal ultrasound imaging. Neurol and Urodyn. 2018; 37:658-665.
Image credit Gupta et al. 2016 https://doi.org/10.1016/j.ajur.2016.11.002 https://www.sciencedirect.com/science/article/pii/S2214388216300881#fig2
Appropriate sun exposure and/or daily supplements provide our bodies with sufficient amounts of Vitamin D. I would venture to guess almost every one of the patients I treated in Seattle had a deficiency of Vitamin D if they were not taking a supplement. Running outside year round has always kept my skin slightly tan and my levels of Vitamin D healthy; however, when I was pregnant in the Pacific Northwest, I had to supplement my diet with Vitamin D, which was a first for this East Coast beach girl. The benefit of Vitamin D has spread beyond just bone health, with studies showing its impact on pelvic floor function.
Parker-Autry et al., (2012) published a study discerning the Vitamin D levels in women who already presented with pelvic floor dysfunction versus “normal” gynecological patients. The retrospective study involved a chart review of 394 women who completed the Colorectal Anal Distress Inventory (CRADI)-8 and the Incontinence Impact Questionnaire (IIQ-7). These women all had a total serum 25-hydroxy Vitamin D [25(OH)D] drawn within one year of their gynecological visit. The authors defined a serum 25(OH)D of <15ng/ml as Vitamin D deficient, between 15-29ng/ml as Vitamin D insufficient, and >30ng/ml as Vitamin D sufficient. In the pelvic floor disorder group comprised of 268 women, 51% were found Vitamin D insufficient, 13% of whom were deficient. The CRADI-8 and IIQ-7 scores were noted as higher among the Vitamin D insufficient women. Overall, the mean 25(OH)D levels in the women without pelvic floor issues were higher than those who presented with pelvic floor disorder symptoms.
Another case-control study in 2014 by Parker-Autry et al., focused on the association between Vitamin D deficiency and fecal incontinence. They considered 31 women with fecal incontinence versus a control group of 81 women without any pelvic floor symptoms, looking at serum Vitamin D levels. The women with fecal incontinence had a mean serum Vitamin D level of 29.2±12.3 ng/ml (insufficient/deficient), while the control group had a higher mean level of 35±14.1 ng/ml (sufficient). The women completed the Modified Manchester Health Questionnaire and the Fecal Incontinence Severity Index, and women with deficient Vitamin D scored higher on the questionnaire, indicating fecal incontinence as a burden on quality of life. The severity scores were higher for Vitamin D deficient women, but there was not a statistically significant difference between the groups. Once again, the pelvic floor disorder and Vitamin D deficiency correlation prevailed in this study.
An even more recent study looked at postmenopausal women and Vitamin D deficiency (Navaneethan et al., 2015). This prospective case control study involved 120 postmenopausal women, 51 of whom had pelvic floor disorders. The serum 25-hydroxy Vitamin D levels were obtained, and the results revealed a deficiency in those women with pelvic floor dysfunction. Vitamin D levels were found to be significantly lower in women who were 5 years or more into menopause. Overall, Vitamin D was deemed a worthy factor to consider in the pelvic floor disorder population as well as in postmenopausal women.
Taking time to talk to patients about their lifestyle, daily supplements, and diet can often shed light on their ability to benefit from our treatments. If a Vitamin D deficiency sounds possible, discuss current research with them and suggest they get their serum Vitamin D levels checked. Don’t underestimate the power of a little sunshine – it just might have a positive impact on pelvic floor health.
Parker-Autry, C. Y., Markland, A. D., Ballard, A. C., Downs-Gunn, D., & Richter, H. E. (2012). Vitamin D Status in Women with Pelvic Floor Disorder Symptoms. International Urogynecology Journal, 23(12), 1699–1705. http://doi.org/10.1007/s00192-012-1700-8
Parker-Autry, C. Y., Gleason, J. L., Griffin, R. L., Markland, A., & Richter, H. E. (2014). VITAMIN D DEFICIENCY IS ASSOCIATED WITH INCREASED FECAL INCONTINENCE SYMPTOMS. International Urogynecology Journal, 25(11), 1483–1489. http://doi.org/10.1007/s00192-014-2389-7
Navaneethan, P. R., Kekre, A., Jacob, K. S., & Varghese, L. (2015). Vitamin D deficiency in postmenopausal women with pelvic floor disorders. Journal of Mid-Life Health, 6(2), 66–69. http://doi.org/10.4103/0976-7800.158948
The following post comes to us from long-time faculty member Dawn Sandalcidi PT, RCMT, BCB-PMD! Dawn is a figurehead in the world of pediatric pelvic floor, she teaches Pediatric Incontinence and Pelvic Floor Dysfunction (available three times in 2016) and she just completed the 2nd edition of the Pediatric Pelvic Floor Manual!! Today Dawn is sharing her insights an urotherapy for pediatric patients.
 If you read any papers on pediatric bowel and bladder dysfunction you will often come across the word "urotherapy". It is by definition a conservative based management based program used to treat lower urinary tract (LUT) dysfunction using a variety of health care professionals including the physician, Physical Therapists, Occupational Therapists and Registered Nurses.
If you read any papers on pediatric bowel and bladder dysfunction you will often come across the word "urotherapy". It is by definition a conservative based management based program used to treat lower urinary tract (LUT) dysfunction using a variety of health care professionals including the physician, Physical Therapists, Occupational Therapists and Registered Nurses.
Basic urotherapy includes education on the anatomy and function of the LUT, behavior modifications including fluid intake, timed or scheduled voids, toilet postures and avoidance of holding maneuvers, diet, bladder irritants and constipation. This needs to be tailored to the patients’ needs. For example a child with an underactive bladder needs to learn how to sense urge and listen to their body and a child who postpones a void needs to be on a voiding schedule. Urotherapy alone can be helpful however a recent study demonstrated a statistically significant improvement in uroflow, pelvic floor muscle electromyography activity during a void, urinary urgency, daytime wetting and reduced post void residual (PVR) in those patients who received pelvic floor muscle training as compared to Urotherapy alone. This is great news for all of us who are qualified to teach pelvic floor muscle exercise!
The International Children’s Continence Society (ICCS) has now expanded the definition of Urotherapy to include Specific Urotherapy. This includes biofeedback of the pelvic floor muscles by a trained therapist who is able to teach the child how to alter pelvic floor muscle activity specifically to void. It also includes neuromodulation for many types of lower urinary tract dysfunction but most commonly with overactive bladder and neurogenic bladder. Cognitive behavioral therapy and psychotherapy are always important to assess (see blog post on psychological effects of bowel and bladder dysfunction).
It truly does take a village to help this kiddos and I am honored to be a team player!
To learn more about pediatric incontinence and pelvic floor rehabilitation, join Dawn Sandalcidi at one of her courses this year! Details at the following links:
Pediatric Incontinence - Augusta, GA - Apr 16, 2016 - Apr 17, 2016
Pediatric Incontinence - Torrance, CA - Jun 11, 2016 - Jun 12, 2016
Pediatric Incontinence - Waterford, CT - Sep 17, 2016 - Sep 18, 2016
Chang SJ, Laecke EV, Bauer, SB, von Gontard A, Bagli,D, Bower WF,Renson C, Kawauchi A, Yang SS-D. Treatment of daytime urinary incontinence: a standardization document from the international children's continence society. Neurourol Urodyn 2015;Oct 16. doi:10.1002/nau.22911
Ladi Seyedian SS, Sharifi-Rad L, Ebadi M, Kajbafzadeh AM. Combined functional pelvic floor muscle exercise with swiss ball and Urotherapy for management of dysfunctional voiding in children: a randomized controlled trial. Eur J Pediatr.2014 Oct;173(10):1347-53. I.J.N. Koppen, A. von Gontard, J. Chase, C.S. Cooper, C.S. Rittig, S.B. Bauer, Y. Homsy, S.S. Yang, M.A. Benninga. Management of functional nonretentive fecal incontinence in children: recommendations from the International Children’s Continence Society. J of Ped Urol (2015)
Koppen IJ, Di Lorenzo C, Saps M, Dinning PG, Yacob D, Levitt MA, Benninga MA. .Childhood constipation: finally something is moving! Expert Rev Gastroenterol Hepatol. 2015 Oct 14:1-15.
Episiotomy is defined as an incision in the perineum and vagina to allow for sufficient clearance during birth. The concept of episiotomy with vaginal birth has been used since the mid to late 1700’s and started to become more popular in the United States in the early 1900’s. Episiotomy was routinely used and very common in approximately 25% of all vaginal births in the United States in 2004. However, in 2006, the American Congress of Obstetricians and Gynecologists recommended against use of routine episiotomies due to the increased risk of perineal laceration injuries, incontinence, and pelvic pain. With this being said, there is much debate about their use and if there is any need at all to complete episiotomy with vaginal birth.
 What are the negative outcomes of episiotomy?
What are the negative outcomes of episiotomy?
The primary risks are severe perineal laceration injuries, bowel or bladder incontinence, pelvic floor muscle dysfunction, pelvic pain, dyspareunia, and pelvic floor laxity. Use of a midline episiotomy and use of forceps are associated with severe perineal laceration injury. However, mediolateral episiotomies have been indicated as an independent risk factor for 3rd and 4th degree perineal tears. If episiotomy is used, research indicates that a correctly angled (60 degrees from midline) mediolateral incision is preferred to protect from tearing into the external anal sphincter, and potentially increasing likelihood for anal incontinence.
What are the indications for episiotomy, if any?
This remains controversial. Some argue that episiotomies may be necessary to facilitate difficult child birth situations or to avoid severe maternal lacerations. Examples of when episiotomy may be used could include shoulder dystocia (a dangerous childbirth emergency where the head is delivered but the anterior shoulder is unable to pass by the pubic symphysis and can result in fetal demise.), rigid perineum, prolonged second stage of delivery with non reassuring fetal heart rate, and instrumented delivery.
On the other side of the fence, many advocate never using an episiotomy due to the previously stated outcomes leading to perineal and pelvic floor morbidity. In a recent cohort study in 2015 by Amorim et al., the question of “is it possible to never perform episiotomy with vaginal birth?” was explored. 400 women who had vaginal deliveries were assessed following birth for perineum condition and care satisfaction. During the birth there was a strict no episiotomy policy and Valsalva, direct pushing, and fundal pressure were avoided, and perineal massage and warm compresses were used. In this study there were no women who sustained 3rd or 4th degree perineal tears and 56% of the women had completely intact perineum. 96% of the women in the study responded that they were satisfied or very satisfied with their care. The authors concluded that it is possible to reach a rate of no episiotomies needed, which could result in reduced need for suturing, decreased severe perineal lacerations, and a high frequency of intact perineum’s following vaginal delivery.
Are episiotomies actually being performed less routinely since the 2006 American Congress of Obstetricians and Gynecologists recommendation?
Yes, a recent study in the Journal of the American Medical Association by Friedman, it showed that the routine use of episiotomy with vaginal birth has declined over time likely reflecting an adoption of the American Congress of Obstetricians and Gynecologists recommendations. This is ideal, as it remains well established that episiotomy should not be used routinely. However, indications for episiotomy use remain to be established. Currently, physicians use clinical judgement to decide if episiotomy is indicated in specific fetal-maternal situations. If one does receive an episiotomy then a mediolateral incision is preferred. The World Health Organization’s stance is that an acceptable global rate for the use of episiotomy is 10% or less of vaginal births. So the question still remains, (and of course more research is needed) to episiotomy or not to episiotomy?
Amorim, M. M., Franca-Neto, A. H., Leal, N. V., Melo, F. O., Maia, S. B., & Alves, J. N. (2014). Is It Possible to Never Perform Episiotomy During Vaginal Delivery?. Obstetrics & Gynecology, 123, 38S.
Friedman, A. M., Ananth, C. V., Prendergast, E., D’Alton, M. E., & Wright, J. D. (2015). Variation in and Factors Associated With Use of Episiotomy. JAMA, 313(2), 197-199.
Levine, E. M., Bannon, K., Fernandez, C. M., & Locher, S. (2015). Impact of Episiotomy at Vaginal Delivery. J Preg Child Health, 2(181), 2.
Melo, I., Katz, L., Coutinho, I., & Amorim, M. M. (2014). Selective episiotomy vs. implementation of a non episiotomy protocol: a randomized clinical trial. Reproductive health, 11(1), 66.
Therapists are increasingly learning about and treating pediatric patients who have pelvic floor dysfunction, yet there are still not enough of them to meet the demand. Many therapists I have spoken to are understandably concerned about how to transfer what they have done for adult patients to a younger population. Here are some of the more common concerns therapists express or questions they ask in relation to the pediatric population:

- Can we use biofeedback with children?
- Do we complete internal assessments on kids?
- How do we change the way we talk to the children?
- How much do we have to teach the parents to get the information across?
- Why do we teach strengthening even if some of the kids mostly need relaxation or coordination?
Although each question deserves a longer answer, we can start with biofeedback, and the answer is a resounding “yes”. There is abundant research affirming the potential benefit of biofeedback training for children with pelvic floor dysfunction. And no, we do not typically complete an internal pelvic muscle assessment on children, as that would not be appropriate. Considering that pediatrics can refer to young adults up to age 18-21, there may be a reasonable clinical goal in mind for utilizing internal assessment or treatment. The words we use when we speak to children become very important. Herman & Wallace faculty member Dawn Sandalcidi (known as “Miss Dawn” to her younger patients) gives ample strategies for adapting our language in her continuing education course Pediatric Incontinence and Pelvic Floor Dysfunction. For example, Dawn emphasizes the importance of describing an episode of incontinence as a “bladder leak” and of pointing out to a child that his or her bladder leaked, rather than the child leaking. She also likes to encourage parents and school personnel to drop the term “accident” from vocabulary. In her 2-day course, Dawn also teaches therapists how to train children to become a “Bladder Boss”, and how to teach young patients about relevant anatomy.
The way we teach anatomy to kids is really important in making sure they “get” it. One study published in 2012Equit 2013 describes the results when children are asked to draw a urinary tract in a body diagram. Only half of the children drew a bladder and other organs, and nearly 43% of the children drew “anatomically incorrect pictures.” The authors point out that older children and the ones who had gone through group training for bowel and bladder were more likely to draw correct images. For the last question about teaching contract/relax exercises to children, I had an opportunity to ask Dawn this question recently when she was filming a pediatrics course for MedBridge Education. Her answer emphasized the importance of getting children to develop awareness of the pelvic muscles, and to improve their coordination as well as strength- concepts that participating in an exercise program can work toward.
If you would like to learn more about working with children, the next opportunity to take Dawn’s course is in Boston later this month.
Equit, Monika et al. "Children's concepts of the urinary tract". Journal of Pediatric Urology , Volume 9 , Issue 5 , 648 - 652