An interview with Frank Ciuba.
Frank Ciuba, co-instructor of Osteoporosis Management< alongside Deb Gulbrandson, explains that practitioners need the information provided in their course. "This course is the latest up-to-date research compiled by my partner Deb Gulbrandson and myself in the management of osteoporosis for clinicians." He shares that similar to learning about the pelvic floor, "when physical therapists go to school they get only a small amount of what osteoporosis is and very little on how to treat a patient."
Frank explains that he became interested in teaching osteoporosis management when he learned "that one in four men statistically will get osteoporosis or an osteoporosis-related fracture in their lifetime and they're really not being identified." Osteoporosis Management provides an exercise-oriented approach to treating these patients and it covers specific tests for evaluation, appropriate safe exercises and dosing, basic nutrition, and ideas for marketing your osteoporosis program.
In pelvic health rehabilitation, it's seen that osteoporosis-related kyphosis (curvature of the spine) can affect pelvic organ prolapse, breathing, and digestion. Patients who go through the osteoporosis management program with Frank and Deb, are shown that they reduce the likelihood of compression fracture by 80%.
This course, Osteoporosis Management, is not just for practitioners working with osteoporosis or osteopenia patients. Frank lists the types of patients he's been able to help. "I've used this on high school backpack syndrome, whiplash injuries, adhesive capsulitis, spinal stenosis, low back pain, lumbar strain, even some hip pathologies." He concludes with "We just need to get the word out to more individuals that this a program that can help them. Not only in the short term, but in the long term. This is a program for life."
Holly Tanner Short Interview Series - Episode 2 featuring Deb Gulbrandson
Holly Tanner and Deb Gulbrandson sat down to discuss the Osteoporosis Management Remote Course and why it is important for practitioners to recognize and know how to safely treat and manage osteoporosis patients in their practices.
Deb Gulbrandson shares the goal of the Osteoporosis Management remote course: "This course is based on the Meeks Method created by Sara Meeks, PT, MS, GCS...we have branched out to add information on sleep hygiene, exercise dosing, and basic nutrition for a person with low bone mass. Knowing how to recognize signs, screen for osteoporosis, and design an effective and safe program can be life-changing for these patients."
Join H&W at the Osteoporosis Management remote course, scheduled for September 18-19, 2021, to learn more about treating patients with osteoporosis.

Osteoporosis is known to be a painless, progressive condition that leads to a weakening of the bones and can lead to a higher risk for broken bones. The upcoming remote course, Osteoporosis Management, scheduled for September 18-19, 2021, will discuss the scope of problems, specific tests for evaluating patients, appropriate safe exercises and dosing, and basic nutrition.
H&W faculty member Deb Gulbrandson recommends using the National Osteoporosis Foundation database for a resource and emphasizes the prevalence of osteoporosis is in a past interview for the Pelvic Rehab Report. "Approximately 1 in 2 women over the age of 50 will suffer a fragility fracture in their lifetime...According to the US Census Bureau, there are 72 million baby boomers (age 51-72) in 2019. Currently, over 10 million Americans have osteoporosis and 44 million have low bone mass."
A well-known consequence of osteoporosis is the increased risk of fragility fractures. A fragility fracture is often the first sign of osteoporosis and can be the cause of pain, disability, and quality of life for the patient. Research by Marsha van Oostwaard provided data that suggests about 13 percent of men and 40 percent of women with osteoporosis will experience a fragility fracture in their lifetime. Men also have a higher rate of mortality from fragility fractures relative to women (1).
The International Osteoporosis Foundation reports that patients who have suffered from a fragility fracture are at a high risk of experiencing secondary fractures, especially within two years of the initial fracture. Fragility fractures can result in osteoporotic patients from events that would not elicit an injury in a healthy adult. These events can include falling from a standing position and other low-energy traumas.
Fragility fractures are characterized by low bone mineral density and have an increased incidence with age (2). The risk of a fragility fracture is also influenced by bone geometry and microstructure. The most serious fracture sites are at the hip and vertebrae, but fractures can occur also on the ribs and other locations. Healthcare practitioners can assist patients in adapting lifestyle factors including exercise, sleep positions, and nutrition with the aim of helping prevent falls from occurring.
Deb Gulbrandson shares the goal of the Osteoporosis Management remote course: "This course is based on the Meeks Method created by Sara Meeks, PT, MS, GCS...we have branched out to add information on sleep hygiene, exercise dosing, and basic nutrition for a person with low bone mass. Knowing how to recognize signs, screen for osteoporosis, and design an effective and safe program can be life-changing for these patients."
Join H&W at the Osteoporosis Management remote course, scheduled for September 18-19, 2021, to learn more about treating patients with osteoporosis.
- Fragility Fracture Nursing: Holistic Care and Management of the Orthogeriatric Patient [Internet]. Marsha van Oostwaard. Hertz K, Santy-Tomlinson J. Springer; 2018.
- The burden of osteoporotic fractures: a method for setting intervention thresholds. Kanis, J.A., et al. Osteoporos Int, 2001. 12(5): p. 417-27.
Deb Gulbrandson, PT, DPT, along with Frank J Ciuba DPT, MS, is the author and instructor for a new course on osteoporisis that is launching remotely this month. Join Deb in Osteoporosis Management: A Comprehensive Approach for Healthcare Professionals!
Osteoporosis is a disease of increasingly porous bones that are at greater risk for fracture. The normal “bone remodeling” of breaking down and building up bone as we age is out of balance. Similar to a bank account with withdrawals outpacing deposits, as time goes on there is more breaking down than building back up. This leaves the bone more vulnerable for fracture.
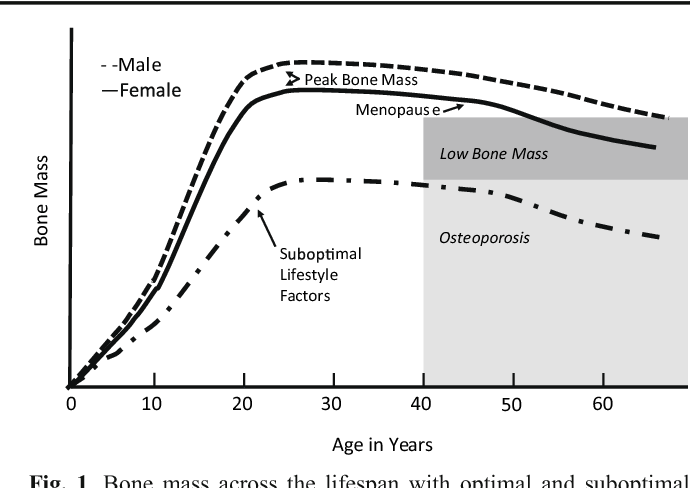
We tend to think of Osteoporosis as an old person’s disease and in fact age is certainly a risk factor. We see a sharp decline in bone density the first few years following menopause; a withdrawal from the “bone bank account.” But let me share a startling statistic. At the age of 20 we have 98% of the bone density we will ever achieve. We achieve Peak Bone Mass by age thirty when our bones have reached their maximum strength and density.
Factors affecting Peak Bone Mass include both Non-modifiable and Modifiable. Among the non-modifiable factors are gender (peak bone mass is higher in men), race (peak bone mass is higher in African Americans), and hormonal factors (early onset of menstruation and use of oral contraceptives tend to have higher peak bone mass). A family history of osteoporosis is another important factor.
Modifiable factors include nutrition (adequate calcium in the diets of young people), physical activity during the early years (specifically weight bearing and resistance exercises). Poor lifestyle behaviors (smoking, high alcohol intake, and sedentary lifestyle) have all been linked to low bone density in adolescents.
The American Physical Therapy Association website includes a section on “Container Baby Syndrome” (CBS). CBS is the name used to describe a range of physical, cognitive, and developmental conditions caused by a baby or infant spending too much time in containers such as baby carriers, strollers, and Bumpo seats. Bone mass can certainly be affected by reduced movement and weight bearing activities. Due to the SIDS scare, many young parents are fearful of allowing their children to spend time on their abdomens. Educate and share the “Supine to Sleep, Prone to Play” mantra.
The graph below shows a comparison of the Peak Bone Mass of males to females and to individuals with suboptimal lifestyle factors. You can see that the suboptimal group never catches up and enters the osteoporosis stage at around age 40.
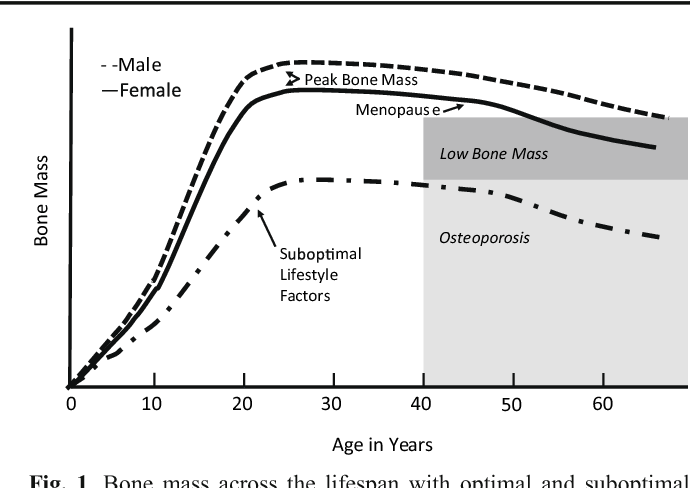
According to the Department of Human Services “Osteoporosis is a pediatric disease with geriatric consequences. Peak bone mass is built during our first three decades. Failure to build strong bones during childhood and adolescent years manifests in fractures later in life.”
What can we do?
• Start early: Encourage young children (and their parents) to move more and sit less.
• Spread the word: Speak to Young Mothers’ Clubs, Girl Scout Troops; anywhere to influence adolescent and teens about the importance of proper exercise and good nutrition.
• Write a blog: Share this information in newspapers, social media, and on your website. Get the word out! Because the bones of our future generation depend on it.
NIH Osteoporosis and Related Bone Diseases National Resource Center
Department of Human Services
American Physical Therapy Association
Deb Gulbrandson, PT, DPT is teaming up with Frank J Ciuba DPT, MS to create a new course called Osteoporosis Management: A Comprehensive Approach for Healthcare Professionals! This new course is launching remotely this July 25-26, 2020, and it emphasizes visual imagery cues which leads to enhanced performance for patients. Both course authors are trained by Sara Meeks, and have adapted her method to create this updated, evidence-based course on osteoporosis management.
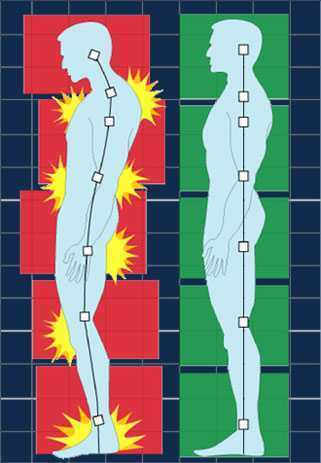
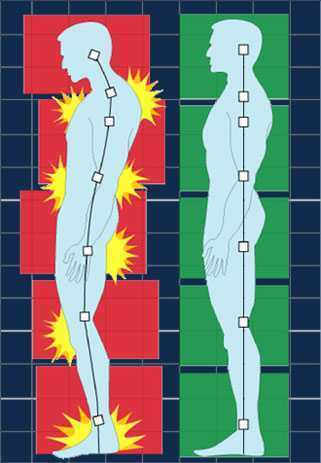
How many times have you told your patients to stand up straight and stop looking down while walking? How’d that work out? Probably not so good. At best you may have noticed a temporary correction only for the patient to return to the formerly mentioned poor posture. We know that balance is affected by alignment of our trunk and spine. 1 Everyone needs to avoid falls but it’s particularly important with osteoporosis patients due to bone fragility.
 We want our patients not only to move, but to move with optimal alignment. According to Fritz, et al 2 in the vhitepaper: “Walking Speed: The Sixth Vital Sign”, walking is a complex functional activity. Our ability to influence motor control, muscle performance, sensory and perceptual function, endurance and habitual activity level can result in a more efficient and safer gait.
We want our patients not only to move, but to move with optimal alignment. According to Fritz, et al 2 in the vhitepaper: “Walking Speed: The Sixth Vital Sign”, walking is a complex functional activity. Our ability to influence motor control, muscle performance, sensory and perceptual function, endurance and habitual activity level can result in a more efficient and safer gait.
Visual imagery cuing had been popular in the sports world for decades. By changing one or two words, physical performance has been shown to improve. 3 In a study involving standing long jump, Wu et al instructed undergraduate students to either “Jump as far as you can and think about extending your legs” (internal focus) or “Jump as far as you can and think about jumping as close to the green target as possible” (external focus). The external focus group jumped 10% farther. Lohse et al 4 and Zachry et al 5 surmised that an external focus reduces the "noise" in the motor system which affects muscular tension and optimal function.
It Starts with Posture
Before you can expect your patients to walk well, they have to stand well- stability before mobility. Assess their posture from all angles and determine where to start. One visual image may change a host of problems. A common postural fault, “slumping” is seen as forward head, increased thoracic kyphosis accompanied with either lumbar hyper or hypo lordosis. Your goal is to get the optimal alignment image that you have in your mind……. into their body.
Most people think in pictures rather than words. 6 Yet the medical industry uses words to communicate. Often we say, “Don’t slouch. Don’t look down.” Telling your patient what not to do is not helpful. Our brain hears the words, “Slouch or look down.” We don’t discern the negative. If I say to you, “Don’t think of a pink elephant,” what does your mind see? How can you not see a pink elephant?
Below are five common visual cues to improve a patient’s posture in standing and walking. These tend to follow the Pareto Principle. 20% of your cues work 80% of the time.
- “In standing, imagine a bungee cord running from the top of your head to the ceiling. Visualize a mother cat lifting her kitten up by the scruff of the neck.”
- “When breathing, imagine an umbrella inside your ribcage, opening up upon inhale, and closing on exhale. Breathe in all directions including into the back of your lungs as if you were filling up the sails of a sailboat.”
- “When walking, widen your collarbones as if they were arrows, shooting off the tips of your shoulders. Imagine your head is a floating balloon, gliding along above your shoulders.”
- “Pretend you are the King (or Queen) of England as you walk among your subjects. “
- “Slide your shoulder blades down toward your opposite hip pockets.”
Choose a cue and instruct your patient. Observe changes in posture, alignment, efficiency of movement, or length of step during gait. Ask your patient for feedback. “What did you notice?” Certain cues resonate more than others. Give them variety and options. The best cues are the ones they create themselves. When a patient says, “You mean like………..?” you know it’s a great cue for them. They have an intuitive understanding and relate to it which translates into their body. A patient’s response to the bungee cord cue was, “You mean like a Christmas ornament hanging from the tree?” My response? Absolutely!
While some visual cues may seem too flowery or not “medical” enough, the research is solid the impact powerful. Plus your patients love it! Visual cues are sticky. They help remind us when we’re out in the real world. Isn’t that the ultimate goal – helping patients become independent in their pursuit of health and safety?
1. Shiro Imagam, et all. Influence of spinal sagittal alignment, body balance, muscle strength, and physical ability on falling of middle-aged and elderly males. Eur Spine J. 2013 Jun;
2. Fritz S. et al White Paper: “Walking Speed: The Sixth Vital Sign” J Geriatr Phys Ther. 2009
3. Wu, et al Effect of Attentional Focus Strategies on Peak Force and Performance in the Standing Long Jump. Joun of Strength and Conditioning Research 2012
4. Lohse and Sherwood Defining the Focus of Attention: Effects of Attention on Perceived Exertion and Fatigue
5. Zachry, T et al. Increased Movement Accuracy and Reduced EMG Activity as a Result of Adopting an External Focus of Attention. Brain Research Bulletin Oct 2005
6. Dynamic Alignment Through Imagery. Franklin, Eric. Second Edition, 2012
Osteoporosis or low bone mass is much more common than most people realize. Approximately 1 in 2 women over the age of 50 will suffer a fragility fracture in their lifetime. A fragility fracture is identified as a fracture due to a fall from a standing height. According to the US Census Bureau there are 72 million baby boomers (age 51-72) in 2019. Currently over 10 million Americans have osteoporosis and 44 million have low bone mass.
Many myths abound regarding osteoporosis. Answer these 5 questions below to test your Osteoporosis IQ. 1
1. “Men don’t get osteoporosis.”
 Fact: In addition to the statistic above regarding the incidence of fractures in women, up to 1 in 4 men over the age of 50 will suffer a fragility fracture.
Fact: In addition to the statistic above regarding the incidence of fractures in women, up to 1 in 4 men over the age of 50 will suffer a fragility fracture.
2. “Osteoporosis is a natural part of aging.”
Fact: Although we do lose bone density as we age, osteopenia or osteoporosis is a much more significant loss than seen in normal aging. DXA (dual energy x-ray absorptiometry) is the gold standard for measuring bone density and the test shows whether an individual’s numbers fall into the normal, osteopenia, or osteoporosis range based on his or her age.
3. “I don’t need to worry about osteoporosis until I’m older.”
Fact: Osteoporosis has been called a “pediatric condition which manifests itself in old age.” Up until the age of 30 we build bone faster than it breaks down. This includes the growth phase of infants and adolescents and is also the time to build as much bone density as possible. By the age of 30, called our Peak Bone Mass, we have accumulated as much bone density as we will ever have. Proper nutrition, osteoporosis specific exercises, and good body mechanics in our formative years can all play a role in reducing the effects of low bone mass later on.
4. “I exercise regularly (including sit ups and crunches for my core). I would know if I had a fracture.”
Fact: Two myths here. Flexion based exercises such as sit-ups, crunches, and toe touches are contraindicated for osteoporosis. A landmark study done by Dr. Sinaki from Mayo clinic showed women with osteoporosis had an 89% re-fracture rate after performing flexion based exercises. 2
Fact: Secondly, only 30% of vertebral compression fractures (VCF) are symptomatic meaning many individuals fracture without knowing it. This can lead to a fracture cascade as individuals continue performing movements and exercises that are contraindicated.
5. “Tests for osteoporosis are painful and expose you to a lot of radiation.”
Fact: The DXA is a simple and painless test which lasts 5-10 minutes. You lay on your back and the machine scans over you with an open arm- no enclosed spaces. There is very little radiation. Your exposure is 10-15 times more when flying from New York to San Francisco.
How did you do? Feel free to share these myths with your patients, many of whom may have osteoporosis in addition to the primary diagnosis for which they are being treated. To learn more about treating patients with low bone density/osteoporosis, consider attending a Meeks Method for Osteoporosis course!
1. www.nof.org
2. https://www.ncbi.nlm.nih.gov/pubmed/6487063
3. https://www.aafp.org/afp/2016/0701/p44.html
Do you work with osteoporosis patients? This may be a trick question because you probably do whether you know it or not- even if you are a pediatric therapist! Osteoporosis is defined by the World Health Organization1 as a systematic skeletal disease characterized by:
- Low bone mass
- Micro-architectural deterioration of bone tissue
- Consequent increase in bone fragility and susceptibility to a fracture
 Osteoporosis occurs in men, women and even children. It is sometimes called the “silent disease” because often people don’t know they have it until they break a bone. And even then, compression fractures are painful only 20-30% of the time. Old fractures are often found on x-rays when a person is imaged for illnesses such as pneumonia. According to the National Osteoporosis Foundation2, about one in two women and one in four men over the age of 50 will suffer a fracture due to bone fragility. At this point in time, it is estimated 80% of patients entering Emergency Departments with a fragility fracture (a fall from a standing height) are never followed up for care.
Osteoporosis occurs in men, women and even children. It is sometimes called the “silent disease” because often people don’t know they have it until they break a bone. And even then, compression fractures are painful only 20-30% of the time. Old fractures are often found on x-rays when a person is imaged for illnesses such as pneumonia. According to the National Osteoporosis Foundation2, about one in two women and one in four men over the age of 50 will suffer a fracture due to bone fragility. At this point in time, it is estimated 80% of patients entering Emergency Departments with a fragility fracture (a fall from a standing height) are never followed up for care.
As therapists, we see patients for a variety of diagnoses with co-morbidities but osteoporosis may not be listed. This could be because they have never been identified. We are in a prime position to screen for signs associated with the disorder. Below are the top 3 signs to look for:
- History of fracture from minimal trauma (fall from a standing height, sneeze, lifting groceries, etc.) The typical fracture areas are wrist, hip, and spine although fragility fractures can happen anywhere in the body.
- Hyper-kyphosis. Note, I said hyper-kyphosis, not kyphosis. We are meant to have a thoracic kyphosis but an excessive curve, particularly when it hinges around T8 area may indicate a collapse of the anterior portion of the vertebral bodies. This is the pie shaped wedging seen on x-rays and further increases the stress on the anterior aspect of the spine. Observe your patients’ sagittal posture for proper alignment.
- Loss of height. Ask your patient their tallest height remembered; then measure them. A loss of 4 cm (1.5 inches) or more may indicate fractures in the spine.
Remember pain may or may not accompany a compression fracture. Patients may complain of a “catch” or muscle spasm or nothing at all. These quick and simple screens can alert the healthcare provider and may help prevent further disintegration of the bones. Research is showing that not only weight bearing exercises but a site specific back and hip strengthening program decreases the risk of fracture.3
1. World Health Organization. www.who.int
2. National Osteoporosis Foundation. www.nof.org
3. Current Osteoporosis Reports. Sept, 2010. The Role of Exercise in the Treatment of Osteoporosis. Sinaki M, Pfeifer M, Preisinger E, Itoi E, Rissoli R, Boonen S, Geusens P, Minne HW.
When It Comes to Bone Building Activities for Osteoporosis, there’s Weight Bearing and then there’s Weight Bearing!
Ask just about anyone on the street what one should do for osteoporosis and the typical answer is- weight bearing exercises. And they would be partially right. Weight bearing, or loading activities have been shown to increase bone density.1 But that’s not the whole story.
 Regarding weight bearing exercises, the million-dollar question is, “How much weight bearing is enough to stimulate bone growth and how much is too much to compromise bone at risk for a fracture? We know that there are incidents of individuals fracturing from just their own body weight upon standing. Recently patients have been asking about heel drops and stomping, and whether they should do them. One size does not fit all.
Regarding weight bearing exercises, the million-dollar question is, “How much weight bearing is enough to stimulate bone growth and how much is too much to compromise bone at risk for a fracture? We know that there are incidents of individuals fracturing from just their own body weight upon standing. Recently patients have been asking about heel drops and stomping, and whether they should do them. One size does not fit all.
An alternative is to focus on “odd impact” loading. A study by Nikander et al 2 targeted female athletes in a variety of sports classified by the type of loading they apparently produce at the hip region; that is, high-impact loading (volleyball, hurdling), odd-impact loading (squash-playing, soccer, speed-skating, step aerobics), high magnitude loading (weightlifting), low-impact loading (orienteering, cross-country skiing), and non-impact loading (swimming, cycling). The results showed high-impact and odd-impact loading sports were associated with the highest bone mineral density.
Morques et al, in Exercise Effects on Bone Mineral Density in Older Adults: A meta-analysis of randomized controlled trials, found that odd impact has potential for preserving bone mass density as does high impact in older women. Activities such as side stepping, figure eights, backward walking, and walking in square patterns help “surprise the bones” due to different angles of muscular pull on the hip. The benefit, according to Nikander, is that we can get the same osteogenic benefits with less force; moderate versus high impact. This type of bone training would offer a feasible basis for targeted exercise-based prevention of hip fragility. I tell my osteoporosis patients that if they walk or run the same route, the same distance, and the same speed that they are not maximizing the osteogenic benefits of weight bearing. Providing variety to the bones creates increased bone mass in the femoral neck and lumbar spine.4
Dancing is another great activity which combines forward, side, backward, and diagonal motions to movement. In addition, it adds music to make the “weight bearing exercises” more fun. Due to balance and fall risk many senior exercise classes offer Chair exercise to music. Unfortunately sitting is the most compressive position for the spine and is particularly problematic with osteoporosis patients. Also the hips do not get any weight bearing benefit. Whenever safely possible, have patients stand; you can position two kitchen chairs on either side, much like parallel bars, to hold on to while they “dance.”
Providing creativity in weight bearing activities using odd impact allows not only for fun and stimulation; it also offers more “bang for the buck!”
- Mosekilde L. Age-related changes in bone mass, structure, and strength--effects of loading. Z Rheumatol (2000); 59 Suppl 1:1-9.
- Nikander et al. Targeted exercises against hip fragility. Osteoporosis International (2009)
- Marques et al. Exercise effects on bone mineral density in older adults: a meta-analysis of randomized controlled trials. Epub 2011 Sep 16
- Weidauer L. et al. Odd-impact loading results in increased cortical area and moments of inertia in collegiate athletes. Eur J Appl Physiol (2014)
In 1984, Mersheed Sinaki MD and Beth Mikkelsen, MD published a landmark article based on their research with osteoporotic women. (Yes, it was 1984 but this is one study no one would want to reproduce).1
 The study follows 59 women with a diagnosis of postmenopausal spinal osteoporosis and back pain who were divided into 4 groups that included spinal Extension (E), Flexion (F), Combined (E+F), or No Therapeutic Exercises (N). Ages ranged from 49 to 60 years (mean, 56 years). Follow-up ranged from one to six years (mean for the groups, 1.4 to 2 years). All patients had follow-up spine x-rays before treatment and at follow-up, at which time any further wedging and compression fractures were recorded. Additional fractures occurred as follows:
The study follows 59 women with a diagnosis of postmenopausal spinal osteoporosis and back pain who were divided into 4 groups that included spinal Extension (E), Flexion (F), Combined (E+F), or No Therapeutic Exercises (N). Ages ranged from 49 to 60 years (mean, 56 years). Follow-up ranged from one to six years (mean for the groups, 1.4 to 2 years). All patients had follow-up spine x-rays before treatment and at follow-up, at which time any further wedging and compression fractures were recorded. Additional fractures occurred as follows:
Group E: 16%
Group F: 89%
Group E+F: 53%
Group N: 67%
This study suggests that a significantly higher number of vertebral compression fractures occur in patients with postmenopausal osteoporosis who followed a flexion based exercise program, than those using extension exercises. It also indicated that patients who did no exercises were less likely to sustain a vertebral compression fracture than those doing flexion exercises.
Due to the anatomical nature of the thoracic spine, the vertebral bodies are placed into a normal kyphosis. The anterior portion of the thoracic spine carries an excess load which can predispose an individual to fracture. Combine the propensity of flexion based daily activities such as brushing teeth, driving, texting or typing, with the fact that vertebral bodies are primarily made up of trabecular (spongy) bone and you have a recipe for disaster.
In the US, studies suggest that approximately one in two women and one in four men age 50 and older will break a bone due to osteoporosis.2 Now picture the many individuals who think that the only way to strengthen their core is by doing sit ups or crunches, further compressing the anterior portion of the spine. Often these exercises are being taught or led by fitness instructors who unknowingly put their clients at risk. Only 20-30% of compression fractures are symptomatic.3 This means that individuals may continue performing crunches, sit-ups, or toe touches even after they have fractured. No one realizes it until the person may notice a loss in height (they have trouble reaching a formerly accessible shelf or trouble hanging up clothes,) or the fracture is seen on an x-ray for pneumonia, etc. The Dowager’s Hump (hyper-kyphosis) may begin to appear. Or the person sustains another fragility fracture; possibly a hip.
Note that the E Group (Extension) still sustained fractures but significantly less than the other three groups. This suggests that there is a protective effect in strengthening the back extensors which has led to an emphasis on Site Specific back strengthening exercises as well as correct weight bearing activities.
Telling osteoporosis patients that they should exercise without giving them specific guidelines (such as in the Meeks Method) is doing them a disservice. General exercise provides minimal to no benefit in building stronger bones and the wrong exercises could put them at great risk for fractures. Educating our referral sources for the need to recommend therapists trained in correct osteoporosis management and the difference between “right” and “wrong” exercises may be the first step in reducing fragility fractures.
1. Sinaki M, Mikkelsen BA. Postmenopausal spinal osteoporosis: flexion versus extension exercises. Archives of Physical Medicine and Rehabilitation 1984 Oct; 65.
2. NOF.org. National Osteoporosis Foundation
3. McCarthy J, MD, Davis A, MD, Am Family Physician. Diagnosis and Management of Vertebral Compression Fractures
The following is part three in a series documenting Deb Gulbrandson, PT, DPT's journey treating a 72 year old patient who has been living with multiple sclerosis (MS) since age 18. Catch up with Part One and Part Two of the patient case study on the Pelvic Rehab Report. Dr. Gulbrandson is a certified Osteoporosis Exercise Specialist and instructor of the Meeks Method, and she helps teach The Meeks Method for Osteoporosis course.
 On Maryanne’s third visit, after reviewing her home exercises I told her that today our focus was on alignment. “In dealing with osteoporosis we want the forces that act upon our bodies to line up as optimally as possible. We have gravity providing a downward force from above and we have ground reaction forces coming up from below. Remember back to your first visit when we did the Foot Press in sitting and talked about Newton’s 3rd Law? For every action there’s an opposite and equal reaction and, how by pressing your feet down it helped you to sit straighter and gave more support to your back?” She nodded in agreement.
On Maryanne’s third visit, after reviewing her home exercises I told her that today our focus was on alignment. “In dealing with osteoporosis we want the forces that act upon our bodies to line up as optimally as possible. We have gravity providing a downward force from above and we have ground reaction forces coming up from below. Remember back to your first visit when we did the Foot Press in sitting and talked about Newton’s 3rd Law? For every action there’s an opposite and equal reaction and, how by pressing your feet down it helped you to sit straighter and gave more support to your back?” She nodded in agreement.
“Well, there’s another important component to that- one that we call optimal alignment. When we sit or stand in a flexed posture, those two opposing forces do not line up well and can put undue stress and pressure on our body, particularly the vertebral bodies.” I showed her the spine again with an increased flexion (hyper-kyphosis) in the thoracic area. “It’s normal to have a kyphosis in the thoracic spine. What we don’t want is a hyper-kyphosis. We often see the apex of the increased curve around T-7, 8, 9 levels near the bra line. We also call it the “slouch line” because from the front, that’s where we slouch in sitting. A thoracic hyper-kyphosis can lead to hyper-lordosis in the lumbar spine as the body tries to counteract the flexion forces above with extension or arching in the low back. We know that Wolff’s Law states that bone in a healthy person will adapt to the loads under which it is placed.1 But we want those loads to be optimally transmitted; otherwise the adaptation can be problematic.”
With Maryanne sitting in a Perch Posture position on the side of the low mat table, I placed a 4 foot dowel rod alongside her back, touching her sacrum and apex of her thoracic curve. I instructed her to bring her occiput back toward the dowel without extending her neck. I wanted her to do more of a cervical retraction move. She was a good 3+ inches away. Previously I had measured her using the WOD (Wall to Occiput Distance).2 This helps patients understand when they are forward flexed in the upper thoracic and cervical area and becomes an exercise as well. Since Maryanne was not safe in a standing position, we used an armless chair against the wall. I turned it sideways so the side of the chair was snugged up to the wall and transferred her to the chair, sitting so that her sacrum was flush against the wall. “Bring your upper back against the wall without allowing your low back to arch forward”, I told her as I placed a folded towel behind her head. “Now you’re going to press the back of your head into the towel, just as you do when lying down in the Re-alignment routine. Before you perform the Head Press, inhale to prepare, start your exhale, then do the head press. Hold for 3 -5 seconds as you continue to exhale, then relax as you inhale. Do 3-5 reps.”
The Head Press in standing, (or in Maryanne’s case, sitting) is a convenient way to not only strengthen the back muscles isometrically, but also increase awareness of body in space and relationship of head to trunk positioning. For any individual who has developed a forward head position over a period of years, there is a loss of the proprioceptive feedback necessary to know when we’re not in alignment, even if we have the ROM to achieve it. And often a lack of strength and especially muscle endurance to maintain that optimally aligned position is problematic. Using the wall several times a day can assist in building strength and awareness. In Maryanne’s case we needed a folded towel behind her occiput to give her something to press into and prevented her from going into increased cervical extension.
“I still want you to do the Head Press in supine as part of the Re-alignment routine everyday”, I told her. “But also practice it in sitting against a wall, making sure your sacrum is right up against it. Do this several times a day for several minutes, holding 3-5 seconds each. And be sure to use your breath to maintain neutral alignment of your lumbar spine.”
And with that, our work for the day was done.
1. Wolff's Law and bone's structural adaptations to mechanical usage: an ... https://www.ncbi.nlm.nih.gov/pubmed/8060014
2. Concurrent Validity of Occiput-Wall Distance to Measure Kyphosis in Communities. Journal of Clinical Trials. May 18, 2012 Sawitree Wongsa1,4, Pipatana Amatachaya2,4, Jeamjit Saengsuwan3,4 and Sugalya Amatachaya1,4*