Dustienne Miller, CYT, PT, MS, WCS instructed the H&W remote course Yoga for Pelvic Pain. Dustienne passionately believes in the integration of physical therapy and yoga in a holistic model of care, helping individuals navigate through pelvic pain and incontinence to live a healthy and pain-free life. You can find Dustienne Miller on Instagram at @yourpaceyoga
Research demonstrates multiple benefits of a yoga practice that extend beyond the musculoskeletal system. These benefits include improved mood and depression, changes in pain perception, improved mindfulness and associated improved pain tolerance, and the ability to observe situations with emotional detachment.
Do the brains of yoga practitioners vs non-practitioners look different?
A study by Villemure et al looked at the role the insular cortex plays in mediating pain in the brains of yoga practitioners. They included various styles of yoga to capture the essence of yoga across multiple styles - Vinyasa, Ashtanga, Kripalu, Sivananda, and Iyengar.
Rewind back to neuroanatomy class - remember the insular cortex? The insular cortex is responsible for sensory processing, decision-making, and motor control by communicating between the cortical and subcortical aspects of the brain. The outside inputs include auditory, somatosensory, olfactory, gustatory, and visual. The internal inputs are interoceptive (Gogolla).
Villemure et al found several interesting objective differences. The practitioners had increased grey matter volume in several areas of the brain. This increase in grey matter specifically in the insula correlated with increased pain tolerance. The length of time practiced correlated with increased grey matter volume of the left insular cortex. Additionally, white matter in the left intrainsular region demonstrated more connectivity in the yoga group.
Other differences were seen in strategies utilized to manage pain. Most folks in the yoga group expected their practice would decrease reactivity to pain, which it did. The yoga group used parasympathetic nervous system accessing strategies and interoceptive awareness. These strategies were breathwork, noticing and being with the sensation, encouraging the mind and body to relax, and acceptance of the pain. The control group strategies were distraction techniques and ignoring the pain.
The authors determine that the insula-related interoceptive awareness strategies of the yoga practitioners being used during the experiment correlated with the greater intra-insular connectivity. Therefore, the authors conclude that the insular cortex can act as a pain mediator for yoga practitioners.
The more strategies our patients have for pain management, the better! Yoga is one of several non-invasive modalities our patients can add to their healing toolbox.
Yoga for Pelvic Pain was developed by Dustienne Miller to offer participants an evidence-based perspective on the value of yoga for patients with chronic pelvic pain. This course focuses on two of the eight limbs of Patanjali’s eightfold path: pranayama (breathing) and asana (postures) and how they can be applied for patients who have hip, back, and pelvic pain.
A variety of pelvic conditions are discussed including interstitial cystitis/painful bladder syndrome, vulvar pain, coccydynia, hip pain, and pudendal neuralgia. Other lectures discuss the role of yoga within the medical model, contraindicated postures, and how to incorporate yoga home programs as therapeutic exercise and neuromuscular re-education both between visits and after discharge.
References:
Gogolla N. The insular cortex. Current Biology. 2017; 27(12): R580-R586.
Villemure C, Ceko M, Cotton VA, Bushnell MC. Insular cortex mediates increased pain tolerance in yoga practitioners. Cereb Cortex. 2014 Oct;24(10):2732-40. doi: 10.1093/cercor/bht124. Epub 2013 May 21. PMID: 23696275; PMCID: PMC4153807.

Mia Fine, MS, LMFT, CST, CIIP is the author and instructor of the Sexual Interviewing for Pelvic Health Therapists remote course scheduled for August 14-15, 2021. Mia’s specialties are sexual health concerns, eroticism, intimacy, alternative sex and relationships (kink/BDSM and non-monogamy), LGBTQIA+ genders/orientations/sexualities, and desire discrepancy. Her course Sexual Interviewing for Pelvic Health Therapists is intended for pelvic rehab therapists who want to learn tools and strategies from a sex therapist’s toolkit. Mia shares the following blog detailing some of the books that have influenced her.
As a science, psychology, somatics, and sexuality education nerd, books are my go-to psychoeducation sources. The books listed below are resources that I offer to my clients, send to family and friends for birthdays and holidays, and inform the work I do as a clinical supervisor, professor, and therapist. I’m excited to share some of my favorites that might help you and the patients with whom you work.
A prerequisite for anyone with a vulva (or who is partnered with someone with a vulva) is the book Come As You Are written by Emily Nagoski. Before a therapeutic intake session, I invite my clients who have vulvas to read this book. It is important to me that my clients and I share the same language that is offered in this fabulous resource. Nagoski illustrates the Dual Control Model for sexual arousal, interest, and desire in ways that are accessible and digestible for all. When clients understand the difference between Spontaneous Arousal and Responsive Arousal, and why these happen, and when, it is a game-changer for them and their partner. This book is a must for anyone who works with pelvic floor pain. And excitingly, these topics will be covered in my upcoming Herman & Wallace course!
The Politics of Trauma written by Staci Haines (also the author of Healing Sex) is a deep dive into, well, the politics of trauma. In this book, she explores the somatic experiences we humans have when we are activated. Her detailed description of fight, flight, freeze, fawn, and dissociate is nothing short of brilliant. This book is a must for those who are interested in exploring the impact that social justice, racial justice, transformative justice, and restorative justice have on our lived experiences of trauma.
The Body is Not An Apology is another brilliant book by Sonya Renee Taylor. It highlights the many effects of the “isms and obias” (such as Sexism, Racism, Fat-phobia, Transphobia) embedded in our everyday life and how identifying these frees us of the barriers they place on our quality of life. The isms and obias she explores impact the way we view ourselves, talk to ourselves, and relate to others. This book is incredibly inspiring, as is the author, Sonya Renee Taylor.
Additional books I love, many of which are written by close friends and colleagues include:
- Trans Sex by Lucie Fielding
- Wild Side Sex: the Book of Kink by Midori
- Gender Trauma by Alex Iantaffi
- Polyvagal Exercises for Safety and Connection by Deb Dana
- Becoming Cliterate by Laurie Mintz
- Better Sex Through Mindfulness by Lori A. Brotto
- The Art of Giving and Receiving: The Wheel of Consentby Betty Martin, Robyn Dalzen
These books have improved, and informed, my therapeutic work with clients and are recommendations I offer on a weekly, if not daily, basis. For additional resources, check out my website:https://miafinetherapy.com/. I look forward to exploring more comprehensive and accessible resources with you at my upcoming course Sexual Interviewing for Pelvic Health Therapists remote course scheduled for August 14-15, 2021!
Pelvic pain is a common diagnosis that we see as pelvic floor therapists. Pelvic pain is pain located in the lower abdomen, but above pubic symphysis, and is associated with various causes; myofascial pain, neuropathies, endometriosis, painful bladder, and irritable bowel syndromes. A common symptom of pelvic pain is deep dyspareunia or pain with deep vaginal penetration. Vulvar pain is different, as it is below pubic symphysis, and has several sub-classifications. These sub-classifications can often be confusing. The National Vulvodynia Association has a free online education that explains the different sub-types very succinctly. This article focuses on provoked vestibulodynia, which is the most commonly studied.
 PVD or Provoked Vestibulodynia often has superficial dyspareunia which can negatively affect sexual functioning, which can lead to changes in psychological function and quality of life. Women with PVD often complain of greater pain during and after intercourse, pain catastrophization, and allodynia when compared to women with superficial dyspareunia but without PVD. These symptoms indicate central nervous system upregulation or sensitivity. This study sought to investigate the impact of these symptoms.
PVD or Provoked Vestibulodynia often has superficial dyspareunia which can negatively affect sexual functioning, which can lead to changes in psychological function and quality of life. Women with PVD often complain of greater pain during and after intercourse, pain catastrophization, and allodynia when compared to women with superficial dyspareunia but without PVD. These symptoms indicate central nervous system upregulation or sensitivity. This study sought to investigate the impact of these symptoms.
Pelvic pain encompassed a variety of complaints: “dysmenorrhea, deep dyspareunia, dyschezia, chronic pelvic pain, back pain, or diagnosed or suspected endometriosis”. Participants were excluded if postmenopausal or if self reported never sexually active.
One hundred twenty nine participants were divided into those with pelvic pain and PVD (43), and those with pelvic pain alone (87). For this study PVD was diagnosed as superficial dyspareunia (>4/10) and positive Q-tip test with a fixed pressure of 30g. Those with did not meet this criteria were considered to have pelvic pain alone.
The two groups were compared for superficial and deep sexual discomfort severity, sexual quality of life; fear avoidance, feelings of guilt, frustration, etc, physical examination of trigger points along abdominal wall (positive Carnett test), and numeric pain scale of various painful lumbo-pelvic regions.
Of the 129 participants notable findings in both the two groups include 31% had confirmed endometriosis, 40% suspected of endometriosis, and in the remaining 18% had no confirmed or suspected endometriosis. The authors found that the pelvic pain + PVD group had significantly more superficial dyspareunia (p=<.001) and deep dyspareunia (p=.001) which was rated >7/10 for both. This group was also had greater (3x more likely to have) depression symptoms, greater anxiety, and catastrophizing, and was more likely to have painful bladder syndrome than the pelvic pain alone group. There were no differences between the two groups for irritable bowel syndrome or abdominal wall tenderness.
This research is consistent with other research findings. The authors explore various causes of the findings including; cross- sensitization - where there may be cross talk of nerve signals from viscera to viscera and viscera to muscular structures that converge in the spinal cord. The authors note that the poor relationship between PVD and irritable bowel and PVD and abdominal wall tenderness limit that theory. They explore the psychological symptoms may be a consequence of pelvic pain or it may be that having anxiety/depression may make women more sensitive to developing pelvic pain and PVD. This sounds like a little chicken or egg theory. The authors suggest that those with PVD and pelvic pain may benefit from a more intensive multi-disciplinary approach including; “medical, surgical, psychological, or physical therapy approaches”.
Bao, C., Noga, H, Allaire, C. et al. “Provoked Vestibulodynia in Women with Pelvic Pain” Sex Med 2019; 1-8
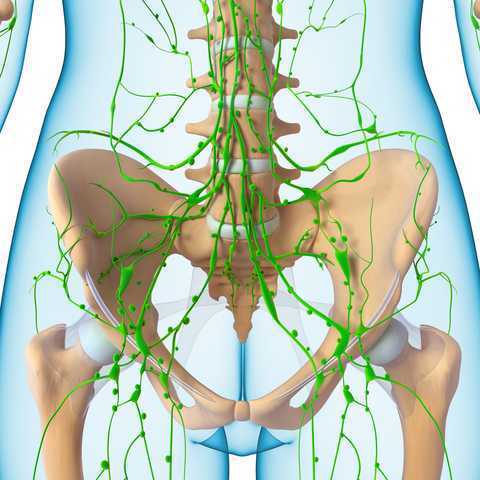
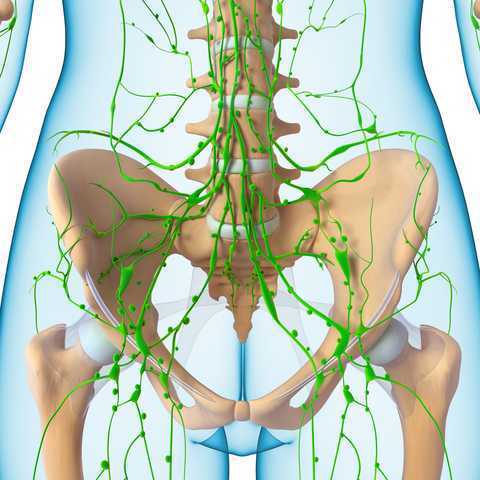
Pelvic pain can often involve adverse neural tension. The hip and pelvic nerves wrap around like spaghetti, making diagnosis and treatment difficult. Is the pain driver boney, capsular, muscle or neurovascular? Luckily, impingement and labral tears are fairly easy to diagnosis. Nerve entrapment can be a little bit tricky to diagnosis and treat. Part of being a good pelvic floor physical therapist is appropriately diagnosing and then partnering with patients to treat symptoms, pain, and movement dysfunction.
 The authors of this study focused on hip, so this blog focuses on sciatic and pudendal nerve entrapment in the athletic population. Nerve entrapment occurs when the normal slide and glide is limited. That can be from any structure in the pelvis and hip region that cause strain or compression on the nerves in the area. Often patient’s descriptions of pain can be the first sign with complaints of ‘burning’, ‘sharp’, or changes in sensation. Evaluation for changes in reflexes and motor function are helpful. Other signs of nerve entrapment are tenderness to palpation and reproduction of pain with movements that elongate the nerve. Medical management to confirm diagnosis include nerve blocks, and diagnostic imaging, and nerve conduction velocity tests.
The authors of this study focused on hip, so this blog focuses on sciatic and pudendal nerve entrapment in the athletic population. Nerve entrapment occurs when the normal slide and glide is limited. That can be from any structure in the pelvis and hip region that cause strain or compression on the nerves in the area. Often patient’s descriptions of pain can be the first sign with complaints of ‘burning’, ‘sharp’, or changes in sensation. Evaluation for changes in reflexes and motor function are helpful. Other signs of nerve entrapment are tenderness to palpation and reproduction of pain with movements that elongate the nerve. Medical management to confirm diagnosis include nerve blocks, and diagnostic imaging, and nerve conduction velocity tests.
Specific locations of pain can help determine where the nerve is being squished. The sciatic nerve (L4-S3) can be entrapped as it passes between the piriformis and deep hip rotators. This often presents with a history of trauma to the gluteal area and limited sitting tolerance (>30 minutes). As the sciatic nerve moves down it can have ischiofemoral impingement, when the nerve gets compressed between lateral ischial tuberosity and greater trochanter at level of quadratus femoris muscle. This will often present as pain during mid- to terminal-stance during walking. Then, once the sciatic nerve clears the pelvis it can become entrapped by the proximal hamstring. There can be hamstring trauma in the history, and possible partial avulsion or thickening of the hamstring may entrap the sciatic nerve.
The pudendal nerve (S2-S4) can become entrapped in several areas and symptoms often include pain medial to the ischium and can include genital regions for all genders, perineum, and peri-rectal regions. The most common areas consist of the space between the posterior pelvic ligaments (sacrospinous and sacrotuberous) and the obturator internus muscle. History often includes bike riding, and a common complaint is pain with sitting, except a toilet seat.
Differential diagnosis for posterior nerves physical examination can include the following tests:
Sciatic Nerve
- Seated palpation: where the clinician palpates the subgluteal space (between sacrum and deep hip rotators), ischial tuberosity and hamstring attachment, and in the area medial to ischial.
- Seated piriformis stretch - involved lower extremity is adducted and internally rotated while palpating posterior hip region.
- Active piriformis - resisted lateral abduction and external rotation while palpating posterior hip region.
- Ischiofemoral impingement: the involved is placed in extension with adduction and external rotation
- Active knee flexion: this test is done seated with knee at 30° and 90° flexion. Clinician palpates ischial canal while providing knee flexion resistance for 5 seconds in both positions.
Pudendal Nerve 
- Palpation around sciatic notch, region medial ischium
- Internal palpation for obturator internus tenderness
- Internal palpation of alcocks canal
Consertative treatment including physical therapy can be helpful. Manual therapy including nerve glides and soft tissue mobilization. Nerve mobilizations require anatomical nerve pathway knowledge. Mobilizing the nerves is thought to improve blood flow within and around the nerve, decrease adhesions, and also may affect central sensitivity. Soft tissue mobilization is geared towards positively affecting scar tissue and encouraging movement that may be restricting neural movement.
Therapeutic exercises for strengthening and stretching are also helpful, however use caution to avoid aggressive stretching as it may aggravate nerves. Exercises to promote load transfer through the pelvis and lower extremities can be helpful. The authors also suggest lower extremity passive PNF (proprioceptive neurofacilitation) diagonal movements. The authors also suggest aerobic conditioning, cognitive behavioral therapy, and for the chronic pelvic pain population, pelvic floor muscle training that does not provoke symptoms.
When conservative treatment including injections produces limited results, surgical treatments are often the next step. Often surgeries where the nerves are decompressed, neurolysis, or removed, neurectomy can be helpful.
To learn more nerve assessment and treatment techniques, join Nari Clemons, PT, PRPC in her course Sacral Nerve Manual Assessment and Treatment in Tampa, FL this December 6-8, 2019!
Martin R, Martin HD1, Kivlan BR 2.Nerve Entrapment In The Hip Region: Current Concepts Review.Int J Sports Phys Ther. 2017 Dec;12(7):1163-1173.
“What's wrong with children?”
As pelvic health physical therapists we take care of people suffering from bladder and bowel incontinence and/or dysfunction as well as pre-natal/ post-partum back pain, weak core muscles and pelvic pain. I was approached over 30 years ago by a urologist to take care of his pediatric patients. My reply: “What’s wrong with children?” It’s been a whirlwind of learning since that day!
Pediatric pelvic floor dysfunction is common and can have significant consequences on quality of life for the child and the family, as well as negative health consequences to the lower urinary tract if left untreated.
 According to the National Institute of Diabetes and Digestive and Kidney Diseases, by 5 years of age, over 90% of children have daytime bladder control (NIDDK, 2013) What is life like for the other 10% who experience urinary leakage during the day?
According to the National Institute of Diabetes and Digestive and Kidney Diseases, by 5 years of age, over 90% of children have daytime bladder control (NIDDK, 2013) What is life like for the other 10% who experience urinary leakage during the day?
Bed-wetting is also a pediatric issue with significant negative quality of life impact for both children and their caregivers, with as much as 30% of 4-year-olds experiencing urinary leakage at night (Neveus, 2010). Children who experience anxiety-causing events may have a higher risk of developing urinary incontinence, and in turn, having incontinence causes considerable stress and anxiety for children (Austin, 2014; Neveus, 2010).
Additionally, bowel dysfunction, such as constipation, is a contributor to urinary leakage or urgency. With nearly 5% of pediatric office visits occurring for constipation (Thibodeau 2013, NIDDK, 2013), the need to address these issues is great! And, since pediatric bladder and bowel dysfunction can persist into adulthood, we must direct attention to the pediatric population to improve the health of all our patients.
Children suffer from many diagnoses that affect the pelvic floor including (Austin et al, 2014);
- Voiding dysfunction
- Enuresis (Bedwetting)
- Daytime urinary incontinence
- Urinary urgency and frequency
- Vesicoureteral reflux (Backflow of urine into the kidney)
- Pelvic pain (yes pelvic pain!)
The most common diagnoses I treat are voiding dysfunction and constipation. Pediatric voiding dysfunction is defined as involuntary and intermittent contraction or failure to relax the urethral muscles while emptying the bladder. (Austin et al, 2014); The dysfunctional voiding can present with variable symptoms including urinary urgency, urinary frequency, incontinence, urinary tract infections, and vesicoureteral reflux. Frequently, constipation is a culprit or cause. (Austin et al, 2014; Hodges S. 2012); Managing constipation can have a very positive effect on voiding dysfunction.
“What do we do to teach the pelvic floor (Kegel) muscles to work?”
Common questions I am asked include:
- Can I use biofeedback with children?
- Do we complete internal assessments on pediatric patients?
- How do we teach kids so they can understand?
- Do kids have the ability to learn strengthening versus relaxation?
- How do you teach a child to become aware of their pelvic floor and coordinate it?
If you have pondered these questions, let’s delve in! I see children as young as 4 who have been able to master biofeedback and recite back to me how their pelvic floor works with bowel and bladder function! Children are so eager to please and they love working with animated biofeedback sessions. The research supports the potential benefit of biofeedback training for children with pelvic floor dysfunction (DePaepe et al. 2002, Kaye 2008, Kajbafzadeh 2011, Fazeli 2014). The children are engaged and learn how to isolate their pelvic floor muscles (PFM) through positioning and breathing. The exercises are fun and easy to do. We also incorporate the core! What a wonderful opportunity we have to educate the younger population on these vital muscles as well as proper diet and bowel/bladder habits!
It is not typical to complete an internal pelvic muscle assessment on children, as this would not be appropriate.
“How do I treat it?”
In the literature on pediatric bowel and bladder dysfunction you will often come across the word "Urotherapy". It is, by definition, a conservative management-based program used to treat lower urinary tract (LUT) dysfunction. (Austin 2014)
Basic Urotherapy includes education on the anatomy, behavior modifications including fluid intake, timed or scheduled voids, toileting postures and avoidance of holding maneuvers, diet, avoiding bladder irritants and constipation. Parents are often not aware of their children’s voiding habits once they are cleared from diaper duty after successful potty training occurs.
Urotherapy alone can be helpful however a recent study (Chase, 2010) demonstrated a much greater improvement in those patients who received pelvic floor muscle training as compared to Urotherapy alone.
The International Children’s Continence Society (ICCS) has now expanded the definition of Urotherapy to include Specific Urotherapy (Austin et al, 2014). This includes biofeedback of the pelvic floor muscles by a trained professional who can teach the child how to alter pelvic floor muscle activity specifically for voiding. Cognitive behavioral therapy and psychotherapy are also important and can be a needed in combination with biofeedback in specific cases.
As you can see, PFM exercise combined with Urotherapy is a safe, inexpensive, and effective treatment option for children with pediatric voiding dysfunction.
Do bladder and bowel problems cause psychological problems or is the reverse true?
When we think of pediatric bowel and bladder issues, we primarily focus on what is happening to cause the bowel or bladder leakage and treat it accordingly. It is imperative to teach a child that she/he did not have an “accident”, but their bladder or bowel had a leak. It makes the incident a physiological problem and not something they did. See my blog post on “Accident” for more information.
It is not always apparent how much the child is suffering from issues with self-esteem, embarrassment, internalizing behaviors, externalizing behaviors or oppositional defiant disorders. Dr. Hinman recognized theses issues years ago (1986) and commented that voiding dysfunctions might cause psychological disturbances rather than the reverse being true. Dr. Rushton in 1995 wrote that although a high number of children with enuresis are maladjusted and exhibit measurable behavioral symptoms, only a small percentage have significant underlying psychopathology. In other more recent studies (Joinson et al. 2006a, 2006b, 2008, Kodman-Jones et al, 2001) it was noted that elevated psychological test scores returned to normal after the urologic problem was cured.
I frequently get testimonials from my patients. I would say the common denominator is the child and/or caregivers report that the child is “much better adjusted,” “happier”, “come out of his shell”, “more outgoing”, “making friends.” As a side note -- they’re happy they don’t leak anymore.
You can learn more about treating pediatric patients in my courses,
Pediatric Incontinence and Pelvic Floor Dysfunction and Pediatric Functional Gastrointestinal Disorders.
Austin, P., Bauer, S.B., Bower, W., et al. The standardization of terminology of lower urinary tract function in children and adolescence: update report from the standardization committee of the international children’s continence society. J Urol (2014) 191.
Chase J, Austin P, Hoebeke P, McKenna P. The management of dysfunctional voiding in children: a report from the standarisation committee of the international children’s continence society. 2010; J Urol183:1296-1302.
Constipation in Children. (2013)retrieved June 9, 2014 from http://kidney.niddk.nih.gov/kudiseases/pubs/uichildren/index.aspx
DePaepe H., Renson C., Hoebeke P., et al: The role of pelvic- floor therapy in the treatment of lower urinary tract dysfunctions in children. Scan J of Urol and Neph 2002; 36: 260-7.
Farahmand, F., Abedi, A., Esmaeili-dooki, M. R., Jalilian, R., & Tabari, S. M. (2015). Pelvic Floor Muscle Exercise for Paediatric Functional Constipation.Journal of Clinical and Diagnostic Research : JCDR, 9(6), SC16–SC17. http://doi.org/10.7860/JCDR/2015/12726.6036
Fazeli MS, Lin Y, Nikoo N, Jaggumantri S1, Collet JP, Afshar K. Biofeedback for Non-neuropathic daytime voiding disorders in children: A systematic review and meta-analysis of randomized controlled trials. J Urol. 2014 Jul 26. pii: S0022-5347(14)04048-8.
Hinman, F. Nonneurogenic neurogenic bladder (the Hinman Syndrome)-15 years later. J Urol 1986;136, 769-777.
Hodges SJ, Anthony E. Occult megarectum:a commonly unrecognized cause of enuresis. Urology. 2012 Feb;79(2):421-4. doi: 10.1016/j.urology.2011.10.015. Epub 2011 Dec 14.
Hoebeke, P., Walle, J. V., Theunis, M., De Paepe, H., Oosterlinck, W., & Renson, C. Outpatient pelvic-floor therapy in girls with daytime incontinence and dysfunctional voiding. Urology 1996; 48, 923-927.
Joinson, C., Heron, J., von Gontard, A. and the ALSPAC study team: Psychological problems in children with daytime wetting. Pediatrics 2006a; 118, 1985-1993.
Joinson, C., Heron, J., Butler, U., von Gontard, A. and the ALSPAC study team: Psychological differences between children with and without soiling problems. Pediatrics 2006b; 117, 1575-1584.
Joinson, C., Heron, J., von Gontard, A., Butler, R., Golding, J., Emond, A.: Early childhood risk factors associated with daytime wetting and soiling in school-age children. Journal of Pediatric Psychology2008; e-published.
Kajbafzadeh AM, harifi-Rad L, Ghahestani SM, Ahmadi H, Kajbafzadeh M, Mahboubi AH. (2011) Animated biofeedback: an ideal treatment for children with dysfunctional elimination syndrome. J Urol;186, 2379-2385.
Kaye JD, Palmer LS (2008) Animated biofeedback yields more rapid results than nonanimated biofeedback in the treatment of dysfunctional voiding in girls. J Urol 180, 300-305
Kodman-Jones, C., Hawkins, L., Schulman, SL. Behavioral characteristics of children with daytime wetting. J Urol 2001;Dec(6):2392-5.
Neveus, T, Eggert P, Evans J, et al. Evaluation of the treatment for monosymptomatic enuresis: a standarisation document from the international children’s continence society. J Urol 2010; 183: 441-447
Rushton, H. G. Wetting and functional voiding disorders. Urologic Clinics of North America, 1995; 22(1), 75-93.
Seyedian, S. S. L., Sharifi-Rad, L., Ebadi, M., & Kajbafzadeh, A. M. (2014). Combined functional pelvic floor muscle exercises with Swiss ball and urotherapy for management of dysfunctional voiding in children: a randomized clinical trial. European Journal of Pediatrics, 173(10), 1347-1353.
Thibodeau, B. A., Metcalfe, P., Koop, P., & Moore, K. (2013). Urinary incontinence and quality of life in children. Journal of pediatric urology, 9(1), 78-83.
Urinary Incontinence in Children. (2012). Retrieved June 9, 2014 from http://kidney.niddk.nih.gov/kudiseases/pubs/uichildren/index.aspx
Zivkovic V, Lazovic M, Vlajkovic M, Slavkovic A, Dimitrijevic L, Stankovic I, Vacic N. (2012). Diaphragmatic breathing exercises and pelvic floor retraining in children with dysfunctional voiding. European Journal of Physical Rehabilitation Medicine. 48(3):413-21. Epub 2012 Jun 5.
In this post, we want to give a high-level overview of interstitial cystitis and an introduction to other resources if you’d like to dive deeper into treatment the condition. There’s a printable, patient-friendly version of this overview if you’d like to use it in describing the condition with patients. In addition, you may want to review the 8 Myths of Interstitial Cystitis series and the AUA Guidelines for Interstitial Cystitis.
Definition
Interstitial cystitis is defined as pain or pressure perceived to be related to the urinary bladder, associated with lower urinary tract symptoms of more than six weeks duration, in the absence of infection or other identifiable causes.
Unfortunately, for physicians, pelvic floor dysfunction falls under category of ‘unidentifiable cause.’ Interstitial cystitis is really more of a description of symptoms, rather than a discrete diagnosis, and the condition presents in many different ways.

Symptoms
The hallmarks of interstitial cystitis are pelvic pain, often in the suprapubic area or inner thighs, and urinary urgency and frequency. Other common symptoms include pain with intercourse, nocturia, low back pain, constipation, and urinary retention.
Many patients are surprised to realize that symptoms like painful intercourse, low back pain, and constipation are related to their IC diagnosis. This challenges the misconception that issues are arising solely from the bladder, and is a good way to help patients (and their physicians) understand that IC is about more than just the bladder.
Diagnosis
Interstitial cystitis is fundamentally a diagnosis of exclusion. Most patients suspect a urinary tract infection (UTI) when their symptoms first present. It’s actually common for symptoms to start as the result of a UTI, and simply not resolve once the infection has cleared. Patients are often treated with multiple rounds of antibiotics for these ‘phantom’ UTIs, where cultures have come back negative, before an IC diagnosis is considered.
It’s important for us as physical therapists to be able to share with patients that no testing is required to confirm an IC diagnosis, it can be diagnosed clinically. In practice, a urologist will likely want to conduct a cystoscopy, which can rule out more serious issues like bladder cancer as well as check for Hunner’s lesions (wounds in the bladder that are present in about 10% of IC patients). However, after that, no additional testing is needed. The potassium sensitivity test (PST) was formerly used by some urologists, but it has been shown to be useless diagnostically and extremely painful for patients and is not recommended by the American Urological Association. Urodynamic testing is also often conducted, but again is not necessary to establish an IC diagnosis.
Physical Therapy for IC
According to the American Urological Association, physical therapy is the most proven treatment for interstitial cystitis. It’s given an evidence grade of ‘A’ (the only treatment with that grade) and recommended in the first line of medical treatment.
In controlled clinical trials, manual physical therapy has been shown to benefit up to 85% of both men and women. These trials reported benefits after ten visits of one-hour treatment sessions.
In a study conducted at our clinic , PelvicSanity, we found that physical therapy was able to reduce pain for IC patients from an average of 7.6 (out of 10) before treatment to 2.6 following physical therapy. Similarly, how much their symptoms bothered patients fell from 8.3 to 2.8. More than half of patients reported improvements within the first three visits.
Unfortunately, many patients still aren’t referred to pelvic physical therapy by their physician. More than half of the patients in the study had seen more than 5 physicians before finding pelvic PT, and only 7% of patients felt they had been referred to physical therapy at the appropriate time by their doctor.
Multi-Disciplinary Approach
Patients with interstitial cystitis or pelvic pain always benefit from a multidisciplinary approach to treatment.This can include:
- Stress relief to downregulate the nervous system can decrease symptoms and reduce flares. Gentle exercise, meditation, yoga, deep breathing, or working with a psychologist can all provide benefits for patients.
- Diet and nutrition are important when working with IC patients. There is no formal ‘IC Diet’, but most patients are sensitive to at least a few trigger foods. The gold standard of treatment is an elimination diet, where the common culprits are completely removed from the diet and then added back in one at a time. This identifies which foods are triggers for patients. With nutrition for IC, patients should avoid their personal trigger foods and eat healthy – it doesn’t have to be any more restrictive or complicated.
- Alternative treatments like acupuncture have been shown to reduce pelvic pain in patients, and several supplements have shown benefits in trials or anecdotally among patients.
- Bladder treatments include instillations and nerve stimulation. Some patients may benefit from bladder instillations, but many others find that the process of the instillation actually causes additional symptoms. If instillations are beneficial, patients should be encouraged to address the underlying issues during the reprieve that instillations bring. Percutaneous tibial nerve stimulation or an implanted nerve stimulation device can both be possible treatment options.
- Oral medications can also reduce symptoms, but do not address the underlying cause of symptoms in patients. Medication that dampens the nervous system, often an anti-depressant or similar medication, can reduce pain and hypersensitivity. Anti-inflammatories may be beneficial in lowering inflammation and helping break the cycle of dysfunction-inflammation-pain. Most patients are started on Elmiron®, the only FDA-approved medication for IC; unfortunately, in the most recent clinical trial research Elmiron has been shown to be no more effective than a placebo. If it is effective, it only is beneficial for about one-third of patients, and many won’t be compliant with the drug due to cost and side effects.
 Nicole Cozean, PT, DPT, WCS (www.pelvicsanity.com/about-nicole) is the founder of PelvicSanity physical therapy in Southern California. Name the 2017 PT of the Year by the ICN, she’s the first physical therapist to serve on the Interstitial Cystitis Association’s Board of Directors and the author of the award-winning book The IC Solution (www.pelvicsanity.com/the-ic-solution). She teaches at her alma mater, Chapman University, as well as continuing education through Herman & Wallace. Nicole also founded the Pelvic PT Huddle (www.facebook.com/groups/pelvicpthuddle), an online Facebook group for pelvic PTs to collaborate.
Nicole Cozean, PT, DPT, WCS (www.pelvicsanity.com/about-nicole) is the founder of PelvicSanity physical therapy in Southern California. Name the 2017 PT of the Year by the ICN, she’s the first physical therapist to serve on the Interstitial Cystitis Association’s Board of Directors and the author of the award-winning book The IC Solution (www.pelvicsanity.com/the-ic-solution). She teaches at her alma mater, Chapman University, as well as continuing education through Herman & Wallace. Nicole also founded the Pelvic PT Huddle (www.facebook.com/groups/pelvicpthuddle), an online Facebook group for pelvic PTs to collaborate.
Interstitial Cystitis Course
In our upcoming course for physical therapists in treating interstitial cystitis (April 6-7, 2019 in Princeton, New Jersey), we’ll focus on the most important physical therapy techniques for IC, home stretching and self-care programs, and information to guide patients in creating a holistic treatment plan. The course will delve into how to handle complex IC presentations. It’s a deep dive into the condition, focusing not just on manual treatment techniques but also how to successfully manage an IC patient from beginning to resolution of symptoms.
Additional Resources
- Interstitial Cystitis Overview (printable)
- The Interstitial Cystitis Solution
- Patient groups include the Interstitial Cystitis Association (ICA) (www.ic-help.org) and the IC Network (www.ic-network.com), which both have fantastic resources for patients.
- The AUA Guidelines for IC
- IC Flare-Busting Plan
In the dim and distant past, before I specialised in pelvic rehab, I worked in sports medicine and orthopaedics. Like all good therapists, I was taught to screen for cauda equina issues – I would ask a blanket question ‘Any problems with your bladder or bowel?’ whilst silently praying ‘Please say no so we don’t have to talk about it…’ Fast forward twenty years and now, of course, it is pretty much all I talk about!
But what about the crossover between sports medicine and pelvic health? The issues around continence and prolapse in athletes is finally starting to get the attention it deserves – we know female athletes, even elite nulliparous athletes, have pelvic floor dysfunction, particularly stress incontinence. We are also starting to recognise the issues postnatal athletes face in returning to their previous level of sporting participation. We have seen the changing terminology around the Female Athlete Triad, as it morphed to the Female Athlete Tetrad and eventually to RED S (Relative Energy Deficiency Syndrome) and an overdue acknowledgement by the IOC that these issues affected male athletes too. All of these issues are extensively covered in my Athlete & The Pelvic Floor’ course, which is taking place twice in 2018.
But what about pelvic pain in athletes?
 How can we ensure that pelvic floor muscle dysfunction is on the radar for a differential diagnosis, or perhaps a concomitant factor, when it comes to athletes presenting with hip, pelvis or groin pain? Gluteal injuries, proximal hamstring injuries, and pelvic floor disorders have been reported in the literature among runners: with some suggestions that hip, pelvis, and/or groin injuries occur in 3.3% to 11.5% of long distance runners.
How can we ensure that pelvic floor muscle dysfunction is on the radar for a differential diagnosis, or perhaps a concomitant factor, when it comes to athletes presenting with hip, pelvis or groin pain? Gluteal injuries, proximal hamstring injuries, and pelvic floor disorders have been reported in the literature among runners: with some suggestions that hip, pelvis, and/or groin injuries occur in 3.3% to 11.5% of long distance runners.
In Podschun’s 2013 paper ‘Differential diagnosis of deep gluteal pain in a female runner with pelvic involvement: a case report’, the author explored the case of a 45-year-old female distance runner who was referred to physical therapy for proximal hamstring pain that had been present for several months. This pain limited her ability to tolerate sitting and caused her to cease running. Examination of the patient's lumbar spine, pelvis, and lower extremity led to the initial differential diagnosis of hamstring syndrome and ischiogluteal bursitis. The patient's primary symptoms improved during the initial four visits, which focused on education, pain management, trunk stabilization and gluteus maximus strengthening, however pelvic pain persisted. Further examination led to a secondary diagnosis of pelvic floor hypertonic disorder. Interventions to address the pelvic floor led to resolution of symptoms and return to running.
‘This case suggests the interdependence of lumbopelvic and lower extremity kinematics in complaints of hamstring, posterior thigh and pelvic floor disorders. This case highlights the importance of a thorough examination as well as the need to consider a regional interdependence of the pelvic floor and lower quarter when treating individuals with proximal hamstring pain.’ (Podschun 2013)
Many athletes who present with proximal hamstring tendinopathy or recurrent hamstring strains, display poor ability to control their pelvic position throughout the performance of functional movements for their sport: along with a graded eccentric programme, Sherry & Best concluded ‘…A rehabilitation program consisting of progressive agility and trunk stabilization exercises is more effective than a program emphasizing isolated hamstring stretching and strengthening in promoting return to sports and preventing injury recurrence in athletes suffering an acute hamstring strain’
If you are interested in learning more about how pelvic floor dysfunction affects both male and female athletes, including broadening your differential diagnosis skills and expanding your external treatment strategy toolbox, then consider coming along to my course ‘The Athlete and the Pelvic Floor’ in Chicago this June or Columbus, OH in October.
The IOC consensus statement: beyond the Female Athlete Triad—Relative Energy Deficiency in Sport (RED-S), Mountjoy et al 2014: http://bjsm.bmj.com/content/48/7/491
‘DIFFERENTIAL DIAGNOSIS OF DEEP GLUTEAL PAIN IN A FEMALE RUNNER WITH PELVIC INVOLVEMENT: A CASE REPORT’ Podschun A et al Int J Sports Phys Ther. 2013 Aug; 8(4): 462–471. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3812833/
‘A comparison of 2 rehabilitation programs in the treatment of acute hamstring strains’ Sherry MA, Best TM J Orthop Sports Phys Ther. 2004 Mar;34(3):116-25. https://www.ncbi.nlm.nih.gov/pubmed/15089024
Most of us spend our day sitting and do not think about the position of our ilia, sacrum or coccyx during the change from standing to sitting. Weightbearing through a tripod of bilateral ischial tuberosities and a sacrum that should have normalized form closure should be easy and pain free. The coccyx typically has minimal weight bearing in sitting, about 10%, just like the fibula, however, it can be a major pain generator, if the biomechanics of the ilia, sacrum and femoral head positions are not quite right.
 Coccydynia and Painful Sitting is a course that can be related to all populations that physical therapists treat. A lot of patients will state “my pain is worse with sitting” which can mean thoracic pain, low back/sacral pain and even lower extremity radicular pain. Women’s health providers treat anything regarding the pelvis, so we are seeing a lot of complicated histories and symptoms.
Coccydynia and Painful Sitting is a course that can be related to all populations that physical therapists treat. A lot of patients will state “my pain is worse with sitting” which can mean thoracic pain, low back/sacral pain and even lower extremity radicular pain. Women’s health providers treat anything regarding the pelvis, so we are seeing a lot of complicated histories and symptoms.
Scanning the literature for coccyx treatment does not always yield the best results for physical therapists. Most literature states what the medical interventions can be, and physical therapy is never at the forefront. However, as we are musculoskeletal and neuromuscular specialists, this is no different on our thinking patterns relating to coccyx pain or painful sitting.
During sitting, the coccyx has a normal flexion and extension moments that will change or become dysfunctional once mechanics above and below that joint change. A simple ankle sprain from 2 years ago can result in chronic knee pain, sacroiliac pain, and can lead to coccyx pain over time. Even the patient who has long standing TMJ (temporomandibular joint) and cervical dysfunction, now has a thoracic rotation and your correction of their coccyx deviation cannot maintain correction.
This course sparks your orthopedic mindset, encouraging the clinician to evaluate the coccyx more holistically. What are the joints doing? How does it change from sitting to standing? Standing to sitting? What is the difference from sitting upright to slump activities? Working through the basics and the obvious with failed results, takes you to the next step of critical thinking within this course. How does the patient present, what seems to be lacking and how to correct them biomechanically to achieve pain free sitting?
Related coccyx musculature and nerve dysfunction can seem like the easiest to treat, but what happens when those techniques fail? This course looks at the entire body, from cranium to feet, to determine the driver of coccyx pain and dysfunction. A better understanding of ilial motion, with accompanied spring tests (Hesch Method), normalizing spinal mechanics and lower extremity function is highlighted in this course. Internal vaginal and rectal release of pelvic floor muscles can lead to normalized coccyx muscle tension that are supported via coccyx taping.
Join me for "Coccydynia and Painful Sitting: Orthopedic and Pelvic Floor Muscle Implications", taking place May 6-7 in Dayton, OH and October 13-14 in Houston, TX.
In 2007, after only speaking on the phone and never meeting in person, my new friend and colleague Stacey Futterman and I presented at the APTA National Conference on the topic of male pelvic pain. It was a 3 hour lecture that Stacey had been asked to give, and she invited me to assist her upon recommendation of one of her dear friends who had heard me lecture. I still recall the frequent glances I made to match the person behind the voice I had heard for so many long phone calls.
 Upon recommendation of Holly Herman, we took this presentation and developed it into a 2 day continuing education course, creating lectures in male anatomy (we definitely did not learn about the epididymis in my graduate training), post-prostatectomy urinary incontinence, pelvic pain, and a bit about sexual health and dysfunction. Although it truly seems like the worst imaginable question, we asked each other “should we allow men to attend?” As strange as this question now seems, it speaks volumes about the world of pelvic health at that time; mostly female instructors taught mostly female participants about mostly female conditions.
Upon recommendation of Holly Herman, we took this presentation and developed it into a 2 day continuing education course, creating lectures in male anatomy (we definitely did not learn about the epididymis in my graduate training), post-prostatectomy urinary incontinence, pelvic pain, and a bit about sexual health and dysfunction. Although it truly seems like the worst imaginable question, we asked each other “should we allow men to attend?” As strange as this question now seems, it speaks volumes about the world of pelvic health at that time; mostly female instructors taught mostly female participants about mostly female conditions.
Make no mistake- women’s health topics were and are deserving of much attention in our typically male-centered world of medicine and research. Maternal health in the US is dreadful, and gone are the days when providers should allow urinary incontinence or painful sexual health to be “normal”, yet it is often described as such to women who are brave enough to ask for help. Times have changed for the better for us all.
The Male Pelvic Floor Course was first taught in 2008, and so far, 22 events have taken place in 18 different cities. 73 men have attended the course to date, with increasing numbers represented at each course. Rather than 20-25 attendees, the Institute is seeing more of the men’s health course filling up with 35-40 participants. In my observations, the men who attend the course are often very experienced, have excellent orthopedic and manual therapy skills, and have personalities that fit very well into the sensitive work that is pelvic rehabilitation.
The course was expanded to include 3 days of lectures and labs, and this expansion allowed more time for hands-on skills in examination and treatment. The schedule still covers bladder, prostate, sexual health and pelvic pain, and further discusses special topics like post-vasectomy syndrome, circumcision, and Peyronie’s disease. In my own clinical practice, learning to address penile injuries has allowed me to provide healing for conditions that are yet to appear in our journals and textbooks. As I often say in the course, we are creating male pelvic rehabilitation in real time.
Because the course often has providers in attendance who have not completed prior pelvic health training, instruction in basic techniques are included. For the experienced therapists, there are multiple lab “tracks” that offer intermediate to advanced skills that can be practiced in addition to the basic skills. Adaptations and models are used when needed to allow for draping, palpation, and education when working with partners in lab, and space is created for those therapists who want to learn genital palpation more thoroughly versus those who are deciding where their comfort zone is at the time. One of the more valuable conversations that we have in the course is how to create comfort and ease in when for most us, we were raised in a culture (and medical training) where palpation of the pelvis was not made comfortable. Hearing from the male participants about their bodies, how they are affected by cultural expectations, adds significant value as well.
We need to continue to create more coursework, more clinical training opportunities so that the representation of those treating male patients improves. If you feel ready to take your training to the next level in caring for male pelvic dysfunction, this year there are three opportunities to study. I hope you will join me in Male Pelvic Floor Function, Dysfunction and Treatment.
 In 1998, faculty member Debora Chassé was asked to evaluate a patient with bilateral lower extremity lymphedema following repeated surgeries for cervical cancer. Her formal education did not cover this in school, so Dr. Chassé began to study peer-review research and consult with other clinicians about the diagnosis. Her journey down the rabbit hole began.
In 1998, faculty member Debora Chassé was asked to evaluate a patient with bilateral lower extremity lymphedema following repeated surgeries for cervical cancer. Her formal education did not cover this in school, so Dr. Chassé began to study peer-review research and consult with other clinicians about the diagnosis. Her journey down the rabbit hole began.
Dr. Chassé became a certified lymphedema therapist in 2000 and a certified Lymphology Association of North America therapist in 2001. She continued training by moving into osteopathy taking her into the direction of lymphatic vessel manipulation. In 2006 she began taking courses in pelvic pain and obstetrics with a focus on pelvic floor dysfunction. It was at this point that Dr. Chasse realized nobody was applying lymphatic treatment to women’s health and pelvic floor dysfunction. In 2009 she became a Board Certified Women’s Health Clinical Specialist in Physical Therapy and began traveling around the United States offering workshops in the area of lymphatic treatment.
Dr. Chassé’s approach is to incorporate all her varied skills in the clinic to produce the best patient outcomes. Debora explains that she is “…showing the similarities between pelvic pain and the lymphatic system. The treatment principles are the same, when you are treating both lymphedema or pelvic pain, you are working to reduce inflammation, pain and scarring.”
Another advantage of the lymphatic treatment approach is that it is more comfortable for the patient. “Most intravaginal techniques causes increased pain and inflammation. However, using lymphatic drainage intravaginally is well tolerated and decreases the intravaginal pain. The results are phenomenal!”
Dr. Chassé recollects her experience with a 21 year old female who suffered from chronic pelvic pain. By applying intravaginal lymphatic drainage techniques for 5 consecutive days, the patient experience a 4.83 reduction in pelvic girdle circumference and her intravaginal pain went from 8/10 to 2/10. The patient was amazed at how much better she felt. “My pants fit better, my energy level increased 25% and pain decreased more than 50%. I went from having 2-3 bad days per week to having 2-3 bad days per month, even when my work level increased. My feet no longer swell and I haven’t missed any classes since receiving this treatment.
In her course, “Lymphatics and Pelvic Pain: New Strategies”, Dr. Chassé seeks to train practitioners to utilize lymphatic drainage techniques when treating specifically pelvic pain. Participants will learn lymphatic drainage principles and techniques. They will learn how to clear pathways to transport lymph fluid and internal techniques which will have incredible impacts for patients.