A recent article in the Washington Post Health & Science section explored the wonders of dietary fibre in an article called ‘Fiber has surprising anti-aging benefits, but most people don’t eat enough of it’ The article discussed how ‘…Fiber gets well-deserved credit for keeping the digestive system in good working order — but it does plenty more. In fact, it’s a major player in so many of your body’s systems that getting enough can actually help keep you youthful. Older people who ate fiber-rich diets were 80 percent more likely to live longer and stay healthier than those who didn’t, according to a recent study in the Journals of Gerontology’
But what is fiber and why does it matter?
Before we jump in there, let me answer the perennial questions that arise when we, as pelvic rehab clinicians, talk about fiber…’Is it in our scope of practice to talk about food?!’ I think it is fundamental that if we are placing ourselves as experts in bladder and bowel dysfunction, that we also remember that we can’t focus on problems at one end of ‘the tube’ without thinking about what happens at the other end. Furthermore, let me quote the APTA RC 12-15: The Role of the Physical Therapist in Diet and Nutrition. (June 2015): “as diet and nutrition are key components of primary, secondary, and tertiary prevention of many conditions managed by physical therapists, it is the role of the physical therapist to evaluate for and provide information on diet and nutritional issues to patient, clients, and the community within the scope of physical therapist practice. This includes appropriate referrals to nutrition and dietary medical professionals when the required advice and education lie outside the education level of the physical therapist’’
Fiber plays a huge role in so many of the health issues that we as clinicians face daily – constipation is regarded as a scourge of a modern sedentary society, perhaps over-reliant on processed convenience food – this is borne out when we gaze upon the rows of constipation remedies and laxatives in our pharmacies and supermarkets.
Let's take a look at the effects of fiber on breast cancer recovery – what does the research say?
There is growing interest and evidence to suggest that making different food choices can help control symptoms of breast cancer treatment and improve recovery markers – avoiding food with added sugar, hydrating well and focusing primarily on plant based food. Fiber is of course beneficial for bowel health, but may also have added benefits for heart health, managing insulin resistance, preventing excess weight gain and actually helping the body to excrete excess estrogen, which is often a driver for hormonally sensitive cancers. Fiber may be Insoluble (whole grains, vegetables) or Soluble (oats, rice, beans, fruit) but both are essential and variety is best.
In their paper ‘Diets and Hormonal levels in Post menopausal women with or without Breast Cancer’ Aubertin – Leheudre et al (2011) stated that ‘…Women eating a vegetarian diet may have lower breast cancer because of improved elimination of excess estrogen’, but even prior to that, in ‘Estrogen excretion patterns and plasma levels in vegetarian and omnivorous women.’ Golden et al (1982) concluded that ‘…that vegetarian women have an increased fecal output, which leads to increased fecal excretion of estrogen and a decreased plasma concentration of estrogen.’
Fiber may also be beneficial in the management of colorectal cancer, which is on the rise in younger women and men. A recent report by the World Cancer Research Fund International/American Institute for Cancer Research found that eating 90 grams of fiber-rich whole grains daily could lower colorectal cancer risk by 17 percent…and the side effects? A happier healthy digestive system, improved cardiovascular health and a lower risk of Type 2 Diabetes.
Your mother was right – eat your vegetables!
For more information on colorectal function and dysfunction, take Pelvic Floor Level 2A or for a deeper dive on the role of nutrition and pelvic health, why not take Megan Pribyl’s excellent course, Nutrition Perspectives for the Pelvic Rehab Therapist? Physical Therapy Treatment for the Breast Oncology Patient is also an excellent opportunity to learn about chemotherapy, radiation and pharmaceutical side effects of breast cancer treatment, as well as expected outcomes in order for the therapist to determine appropriate therapeutic parameters.
https://www.washingtonpost.com/national/health-science/fiber-has-surprising-anti-aging-benefits-but-most-people-dont-eat-enough-of-it/2018/04/27/c5ffd8c0-4706-11e8-827e-190efaf1f1ee_story.html?fbclid=IwAR0b-9VFUOCyUOgwe2BqV7-ahqwGzWs9rNpd1mscT75KNOGqnHm4ooFAu74&utm_term=.4d2784974ddc
Estrogen excretion patterns and plasma levels in vegetarian and omnivorous women. Goldin BR, Adlercreutz H, Gorbach SL, Warram JH, Dwyer JT, Swenson L, Woods MN. N Engl J Med. 1982 Dec 16;307(25):1542-7.
Diets and hormonal levels in postmenopausal women with or without breast cancer. Aubertin-Leheudre M1, Hämäläinen E, Adlercreutz H. Nutr Cancer. 2011;63(4):514-24. doi: 10.1080/01635581.2011.538487.
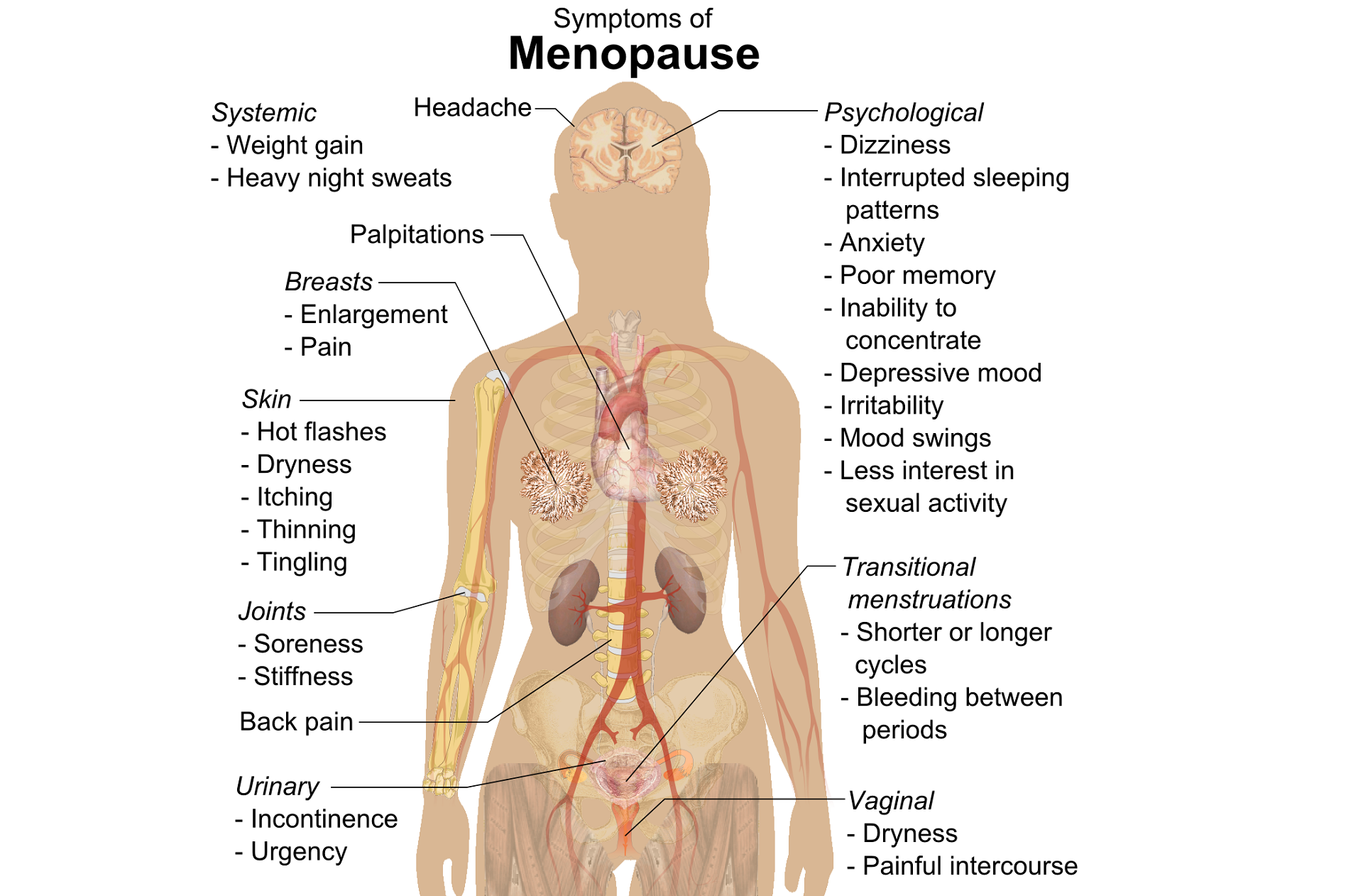
A question that often comes up in conversation around menopause is that of pelvic health – the effects on bladder, bowel or sexual health…what works, what’s safe, what’s not? Is hormone therapy better, worse or the same in terms of efficacy when compared to pelvic rehab? Do we have a role here?
An awareness of pelvic health issues that arise at menopause was explored in Oskay’s 2005 paper ‘A study on urogenital complaints of postmenopausal women aged 50 and over’ stating ‘…Urinary incontinence and sexual problems, particularly decline in sexual desire, are widespread among postmenopausal women. Frequent urinary tract infections, obesity, chronic constipation and other chronic illnesses seem to be the predictors of UI.’
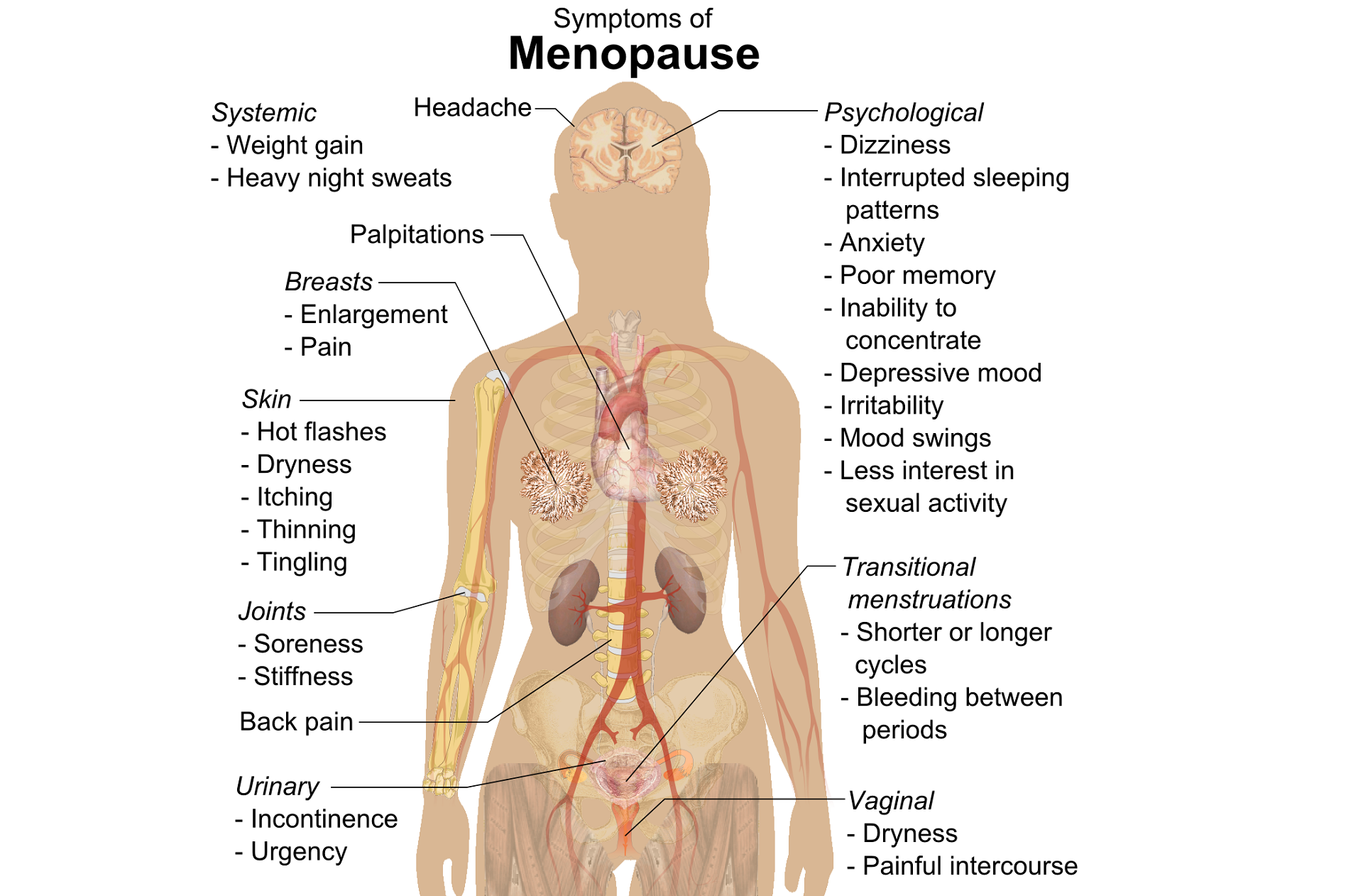 Moller’s 2006 paper explored the link between LUTS (Lower Urinary Tract Symptoms) and sexual activity at midlife: the paper discussed how lower urinary tract symptoms (LUTS) have a profound impact on women’s physical, social, and sexual well being, and confirmed that LUTS are likely to affect sexual activity. However, they also found that conversely, sexual activity may affect the occurrence of LUTS – in their study a questionnaire was sent to 4,000 unselected women aged 40–60 years, and they found that compared to women having sexual relationship, a statistically significant 3 to 6 fold higher prevalence of LUTS was observed in women with no sexual relationship. They also found that women who ceased sexual relationship an increase in the de novo occurrence of most LUTS was observed, concluding that ‘…sexual inactivity may lead to LUTS and vice versa’.
Moller’s 2006 paper explored the link between LUTS (Lower Urinary Tract Symptoms) and sexual activity at midlife: the paper discussed how lower urinary tract symptoms (LUTS) have a profound impact on women’s physical, social, and sexual well being, and confirmed that LUTS are likely to affect sexual activity. However, they also found that conversely, sexual activity may affect the occurrence of LUTS – in their study a questionnaire was sent to 4,000 unselected women aged 40–60 years, and they found that compared to women having sexual relationship, a statistically significant 3 to 6 fold higher prevalence of LUTS was observed in women with no sexual relationship. They also found that women who ceased sexual relationship an increase in the de novo occurrence of most LUTS was observed, concluding that ‘…sexual inactivity may lead to LUTS and vice versa’.
So, who advises women going through menopause about issues such as sexual ergonomics, the use of lubricants or moisturisers, or provide a discussion about the benefits of local topical estrogen? As well as providing a skillset that includes orthopaedic assessment to rule out any musculo-skeletal influences that could be a driver for sexual dysfunction? That would be the pelvic rehab specialist clinician! Tosun et al asked the question ‘Do stages of menopause affect the outcomes of pelvic floor muscle training?’ and the answer in this and other papers was yes; with the research comparing pelvic rehab vs hormone therapy vs a combination approach of pelvic rehab and topical estrogen providing the best outcomes. Nygaard’s paper looked at the ‘Impact of menopausal status on the outcome of pelvic floor physiotherapy in women with urinary incontinence’ and concluded that : ‘…(both pre and postmenopausal women) benefit from motor learning strategies and adopt functional training to improve their urinary symptoms in similar ways, irrespective of hormonal status or HRT and BMI category’.
We must also factor in some of the other health concerns that pelvic health can impact at midlife for women – Brown et al asked the question ‘Urinary incontinence: does it increase risk for falls and fractures?’ They answered their question by concluding that ‘‘… urge incontinence was associated independently with an increased risk of falls and non-spine, nontraumatic fractures in older women. Urinary frequency, nocturia, and rushing to the bathroom to avoid urge incontinent episodes most likely increase the risk of falling, which then results in fractures. Early diagnosis and appropriate treatment of urge incontinence may decrease the risk of fracture.’
If you are interested in learning more about pelvic health, sexual function and bone health at Menopause, consider attending Menopause Rehabilitation and Symptom Management.
Sexual activity and lower urinary tract symptoms’ Møller LA1, Lose G. Int Urogynecol J Pelvic Floor Dysfunct. 2006 Jan;17(1):18-21. Epub 2005 Jul 29.
A study on urogenital complaints of postmenopausal women aged 50 and over. Oskay UY1, Beji NK, Yalcin O. Acta Obstet Gynecol Scand. 2005 Jan;84(1):72-8.
Do stages of menopause affect the outcomes of pelvic floor muscle training? Tosun ÖÇ1, Mutlu EK, Tosun G, Ergenoğlu AM, Yeniel AÖ, Malkoç M, Aşkar N, İtil İM. Menopause. 2015 Feb;22(2):175-84. doi: 10.1097/GME.0000000000000278.
‘Impact of menopausal status on the outcome of pelvic floor physiotherapy in women with urinary incontinence.’ Nygaard CC1, Betschart C, Hafez AA, Lewis E, Chasiotis I, Doumouchtsis SK. Int Urogynecol J. 2013 Dec;24(12):2071-6. doi: 10.1007/s00192-013-2179-7. Epub 2013 Jul 17
September is Gynae Cancer Awareness Month – but how aware are we as clinicians of the signs and symptoms, the epidemiology and the sequalae of treatment afterwards? As pelvic rehab specialists, we have the privilege of helping women live well after cancer treatment ends, both on a ‘local’ pelvic area (bladder, bowel, sexual and pelvic pain management strategies) but also on a more ‘global’ level – dealing with issues such as cancer related fatigue, bone health and cardiovascular concerns.
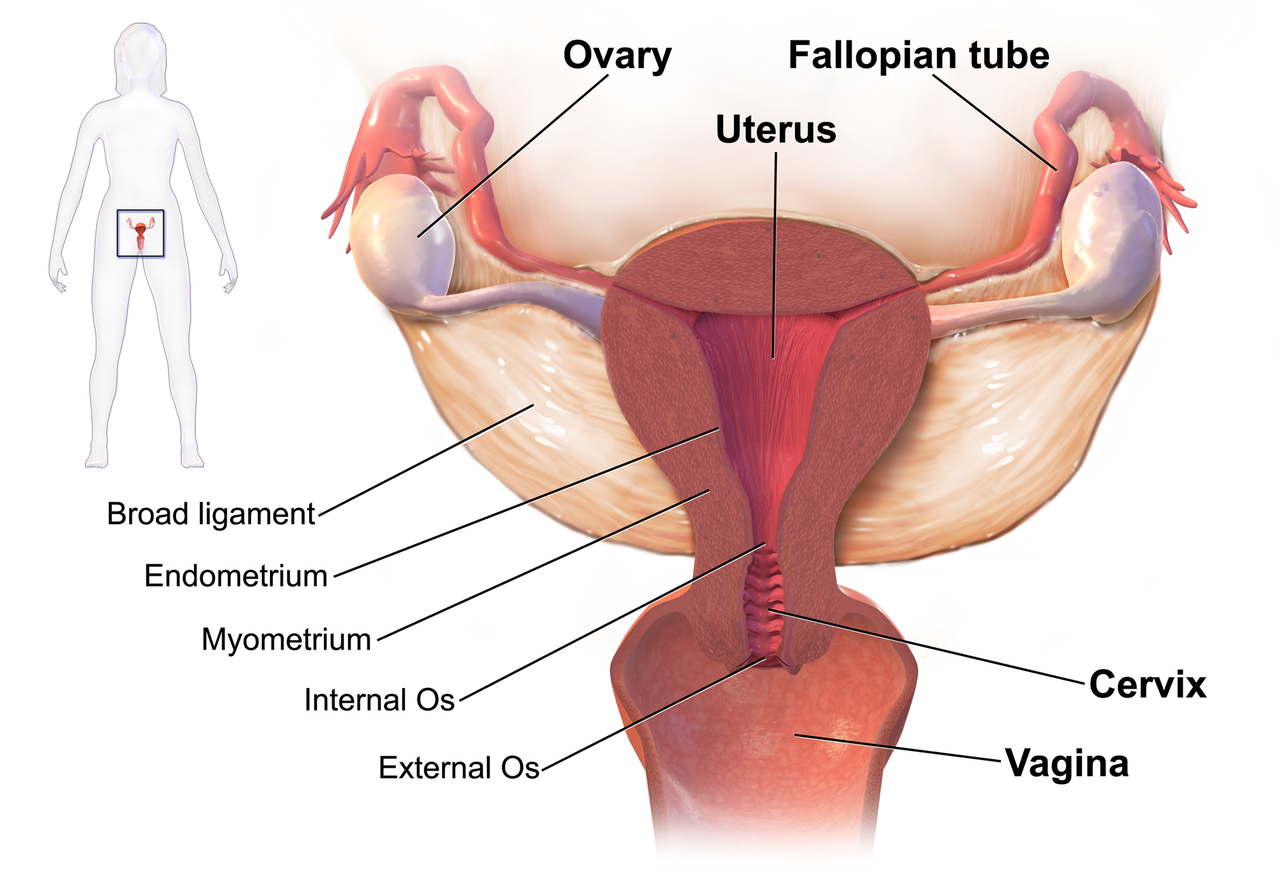 We know that women who are diagnosed with cancer of the vulva, vagina, cervix, endometrium or ovaries are treated with a combination of surgery, radiation or chemotherapy. However, with improving treatment and better survival rates, there is evidence that a variety of pelvic health concerns may arise for these women, both during and after treatment. (Hazewinkel et al 2010). For example, urinary incontinence is reported in 80% of women treated for endometrial cancer, with more severe symptoms and impact on quality of life in those who had adjuvant radiation (Erekson et al 2009) In Malone’s 2017 paper, ‘The patient’s voice: What are the views of women on living with pelvic floor problems following successful treatment for pelvic cancers?’, the author notes that ‘…there is currently a lack of knowledge regarding the effects of PFD on QoL in this cohort. Patients do not always report these problems to their health care providers and clinicians may underestimate symptoms…In the context of having survived cancer, PFD may be seen as relatively trivial. However, in the context of resuming normal living, the symptoms experienced by the survivors may be significant’.
We know that women who are diagnosed with cancer of the vulva, vagina, cervix, endometrium or ovaries are treated with a combination of surgery, radiation or chemotherapy. However, with improving treatment and better survival rates, there is evidence that a variety of pelvic health concerns may arise for these women, both during and after treatment. (Hazewinkel et al 2010). For example, urinary incontinence is reported in 80% of women treated for endometrial cancer, with more severe symptoms and impact on quality of life in those who had adjuvant radiation (Erekson et al 2009) In Malone’s 2017 paper, ‘The patient’s voice: What are the views of women on living with pelvic floor problems following successful treatment for pelvic cancers?’, the author notes that ‘…there is currently a lack of knowledge regarding the effects of PFD on QoL in this cohort. Patients do not always report these problems to their health care providers and clinicians may underestimate symptoms…In the context of having survived cancer, PFD may be seen as relatively trivial. However, in the context of resuming normal living, the symptoms experienced by the survivors may be significant’.
This can present a clinical conundrum – often pelvic rehab therapists are nervous when working with a patient who has a current or previous gynecologic cancer diagnosis, but similarly oncology rehab specialists may have qualms about dealing with pelvic health issues, with the result that these women fall through the cracks and do not have their pelvic health issues managed properly (or at all). Theodore Roosevelt once said ‘No one cares how much you know, until they know how much you care’ and this is especially relevant for oncology pelvic rehab. Often you may be the first clinician to ask about bladder, bowel or sexual function or dysfunction. An understanding of the effects of cancer treatments on the pelvis is important but so too is the wealth of information you may already have about bladder, bowel and sexual health as well as neuroscience and pain education.
The most important thing is to ask these women about their pelvic health concerns – the National Coalition for Cancer Survivorship defined cancer survivorship as extending from ‘the time of diagnosis and for the balance of life’. An emphasis on quality of life has been emphasised – if we know that cancer survivors may not independently volunteer information about their pelvic floor dysfunction, it is our responsibility to ask the questions and comprehensively treat and advocate for these women, in order to help them live well after cancer treatment ends.
- Hazewinkel MH. Sprangers MA, Velden Jvd, Vaart CH, Stalpers LJ, Burger MP ‘Longterm cervical cancer survivors suffer from pelvic floor dysfunction symptoms: A cross-sectional matched cohort study’ Gynecol Oncol 2010;117(2):381-6
- Erekson EA, Sung VW, Disilvestro PA, Myers DL ‘Urinary symptoms and impact on quality of life in women after treatment for endometrial cancer’ Int Urogynecol J 2009;20(2):159-63
- Malone P, Danaher D, Galvin R, Cusack T ‘The patient’s voice: What are the views of women on living with pelvic floor problems following successful treatment for pelvic cancers?’ Physiotherapy Practice and Research 38(2017)93-102
 In July of this year, I was invited to present in Christchurch, New Zealand as part of a teaching tour that took in Singapore, Australia and Tasmania. The topic of my class was female pelvic pain, so we discussed Endometriosis, Vulvodynia, Sexual Health and many other sub-topics but we had several discussions about the effects of trauma on pelvic pain. For those who have visited Christchurch, it is a beautiful city but it is still reeling from a series of massive earthquakes, that started in September 2010. The most devastating was in February 2011, when 185 people were killed and 6600 people were injured. Everywhere you go in Christchurch, there are reminders – from the constant buzz of ongoing construction, to structures that are waiting demolition, like the beautiful old cathedral that was beside our hotel. Usually, when I teach, we do some ‘housekeeping’ announcements about fire drills and exits; in Christchurch it was ‘In the event of an earthquake…’. I wondered how the near constant reminders were affecting the inhabitants, so I read of how ‘…people called living with continual shaking, damaged infrastructure, insurance battles and unrelenting psychological stress ‘the new normal’. There are several ongoing research studies, looking at the effects of this trauma and how it is still having an effect on the people of Christchurch.
In July of this year, I was invited to present in Christchurch, New Zealand as part of a teaching tour that took in Singapore, Australia and Tasmania. The topic of my class was female pelvic pain, so we discussed Endometriosis, Vulvodynia, Sexual Health and many other sub-topics but we had several discussions about the effects of trauma on pelvic pain. For those who have visited Christchurch, it is a beautiful city but it is still reeling from a series of massive earthquakes, that started in September 2010. The most devastating was in February 2011, when 185 people were killed and 6600 people were injured. Everywhere you go in Christchurch, there are reminders – from the constant buzz of ongoing construction, to structures that are waiting demolition, like the beautiful old cathedral that was beside our hotel. Usually, when I teach, we do some ‘housekeeping’ announcements about fire drills and exits; in Christchurch it was ‘In the event of an earthquake…’. I wondered how the near constant reminders were affecting the inhabitants, so I read of how ‘…people called living with continual shaking, damaged infrastructure, insurance battles and unrelenting psychological stress ‘the new normal’. There are several ongoing research studies, looking at the effects of this trauma and how it is still having an effect on the people of Christchurch.
If you’ve attended Pelvic Floor Level 1 with Herman & Wallace, you’ll remember we quote a study from Van der Welde about the effects of perceived danger on muscle activity in the upper trapezius and pelvic floor muscles. We also discuss the work of Levine, of ‘Waking the Tiger’ fame, who explores the somatic effects of trauma in our bodies – and how trauma, much like pain, is whatever we say it is.
I became intrigued with the topic, so I was delighted to hear that Lauren Mansell has created a course to deal exactly with this topic. I was even more delighted when she sat down for a chat with me to explore the nuances of trauma awareness, boundary setting and self-care for therapists, especially pelvic therapists, who work with those who have experienced trauma of any kind.
I hope you find this conversation as interesting as I did! Here is our conversation:
1. ‘Vaginismus, a Component of a General Defensive Reaction. An Investigation of Pelvic Floor Muscle Activity during Exposure to Emotion-Inducing Film Excerpts in Women with and without Vaginismus’ van der Velde, J & Laan, Ellen & Everaerd, W. (2001)
2. ‘Waking The Tiger’ by Peter A. Levine (1997)
In the dim and distant past, before I specialised in pelvic rehab, I worked in sports medicine and orthopaedics. Like all good therapists, I was taught to screen for cauda equina issues – I would ask a blanket question ‘Any problems with your bladder or bowel?’ whilst silently praying ‘Please say no so we don’t have to talk about it…’ Fast forward twenty years and now, of course, it is pretty much all I talk about!
But what about the crossover between sports medicine and pelvic health? The issues around continence and prolapse in athletes is finally starting to get the attention it deserves – we know female athletes, even elite nulliparous athletes, have pelvic floor dysfunction, particularly stress incontinence. We are also starting to recognise the issues postnatal athletes face in returning to their previous level of sporting participation. We have seen the changing terminology around the Female Athlete Triad, as it morphed to the Female Athlete Tetrad and eventually to RED S (Relative Energy Deficiency Syndrome) and an overdue acknowledgement by the IOC that these issues affected male athletes too. All of these issues are extensively covered in my Athlete & The Pelvic Floor’ course, which is taking place twice in 2018.
But what about pelvic pain in athletes?
 How can we ensure that pelvic floor muscle dysfunction is on the radar for a differential diagnosis, or perhaps a concomitant factor, when it comes to athletes presenting with hip, pelvis or groin pain? Gluteal injuries, proximal hamstring injuries, and pelvic floor disorders have been reported in the literature among runners: with some suggestions that hip, pelvis, and/or groin injuries occur in 3.3% to 11.5% of long distance runners.
How can we ensure that pelvic floor muscle dysfunction is on the radar for a differential diagnosis, or perhaps a concomitant factor, when it comes to athletes presenting with hip, pelvis or groin pain? Gluteal injuries, proximal hamstring injuries, and pelvic floor disorders have been reported in the literature among runners: with some suggestions that hip, pelvis, and/or groin injuries occur in 3.3% to 11.5% of long distance runners.
In Podschun’s 2013 paper ‘Differential diagnosis of deep gluteal pain in a female runner with pelvic involvement: a case report’, the author explored the case of a 45-year-old female distance runner who was referred to physical therapy for proximal hamstring pain that had been present for several months. This pain limited her ability to tolerate sitting and caused her to cease running. Examination of the patient's lumbar spine, pelvis, and lower extremity led to the initial differential diagnosis of hamstring syndrome and ischiogluteal bursitis. The patient's primary symptoms improved during the initial four visits, which focused on education, pain management, trunk stabilization and gluteus maximus strengthening, however pelvic pain persisted. Further examination led to a secondary diagnosis of pelvic floor hypertonic disorder. Interventions to address the pelvic floor led to resolution of symptoms and return to running.
‘This case suggests the interdependence of lumbopelvic and lower extremity kinematics in complaints of hamstring, posterior thigh and pelvic floor disorders. This case highlights the importance of a thorough examination as well as the need to consider a regional interdependence of the pelvic floor and lower quarter when treating individuals with proximal hamstring pain.’ (Podschun 2013)
Many athletes who present with proximal hamstring tendinopathy or recurrent hamstring strains, display poor ability to control their pelvic position throughout the performance of functional movements for their sport: along with a graded eccentric programme, Sherry & Best concluded ‘…A rehabilitation program consisting of progressive agility and trunk stabilization exercises is more effective than a program emphasizing isolated hamstring stretching and strengthening in promoting return to sports and preventing injury recurrence in athletes suffering an acute hamstring strain’
If you are interested in learning more about how pelvic floor dysfunction affects both male and female athletes, including broadening your differential diagnosis skills and expanding your external treatment strategy toolbox, then consider coming along to my course ‘The Athlete and the Pelvic Floor’ in Chicago this June or Columbus, OH in October.
The IOC consensus statement: beyond the Female Athlete Triad—Relative Energy Deficiency in Sport (RED-S), Mountjoy et al 2014: http://bjsm.bmj.com/content/48/7/491
‘DIFFERENTIAL DIAGNOSIS OF DEEP GLUTEAL PAIN IN A FEMALE RUNNER WITH PELVIC INVOLVEMENT: A CASE REPORT’ Podschun A et al Int J Sports Phys Ther. 2013 Aug; 8(4): 462–471. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3812833/
‘A comparison of 2 rehabilitation programs in the treatment of acute hamstring strains’ Sherry MA, Best TM J Orthop Sports Phys Ther. 2004 Mar;34(3):116-25. https://www.ncbi.nlm.nih.gov/pubmed/15089024
It’s St Valentine’s day this week – you may have noticed hearts and flowers everywhere you look and a general theme of love and romance. For many women going through cancer treatment, sex may be the last thing on their mind…or not! Women who are going through treatment for gynecologic cancer are often handed a set of dilators with minimal instruction on how to use them, or as one patient reported, they are told to have sex three or four times a week during radiation therapy ‘to keep your vagina patent’. As a pelvic rehab practitioner with a special interest in oncology rehab, I know that we can (we must!) do better, in helping women live well after cancer treatment ends.
 As Susan Gubar, an ovarian cancer survivor, writes in the New York Times ‘…It can be difficult to experience desire if you don’t love but fear your body or if you cannot recognize it as your own. Surgical scars, lost body parts and hair, chemically induced fatigue, radiological burns, nausea, hormone-blocking medications, numbness from neuropathies, weight gain or loss, and anxiety hardly function as aphrodisiacs…’
As Susan Gubar, an ovarian cancer survivor, writes in the New York Times ‘…It can be difficult to experience desire if you don’t love but fear your body or if you cannot recognize it as your own. Surgical scars, lost body parts and hair, chemically induced fatigue, radiological burns, nausea, hormone-blocking medications, numbness from neuropathies, weight gain or loss, and anxiety hardly function as aphrodisiacs…’
Although sexual changes can be categorised into physical, psychological and social, the categories cannot be neatly delineated in the lived experience (Malone at al 2017). The good news? Pelvic rehab therapists not only have the skills to enhance pelvic health after cancer treatment and are ideally positioned to be able to take a global and local approach to the sexual health difficulties women may face after cancer treatment ends, but there is also a good and growing body of evidence to support the work we do. Factors to consider include physical issues leading to dyspareunia, including musculo-skeletal/ orthopaedic, Psychological issues, including loss of libido and other pelvic health issues impacting sexual function such as faecal/ urinary incontinence, pain or fatigue.
In Hazewinkel’s 2010 paper, women reported that they thought their physicians would tell them if solutions were available…most reported reasons for not seeking help were that women found their symptoms bearable in the light of their cancer diagnosis and lacked knowledge about possible treatments but when informed of possible treatment strategies ‘…women stated that care should be improved, specifically by timely referral to pelvic floor specialists’. The good news: ‘‘Pelvic Floor Rehab Physiotherapy is effective even in gynecological cancer survivors who need it most.’ (Yang 2012)
The issue therefore may be one of awareness – for both the women who need our services and the physicians and healthcare team who work in the field of gynecologic oncology. What we need is acknowledgement of the issues and confident conversation and assessment by clinicians – interested in learning more? Come and join the conversation in Tampa next month at my Oncology & the Female Pelvic Floor course!
‘Sex after Cancer’ by Susan Gubar, https://www.nytimes.com/2018/01/18/well/live/sex-after-cancer.html
Malone et al 2017: ‘‘The patient’s voice: What are the views of women on living with pelvic floor problems following successful treatment for pelvic cancers?’
Hazewinkel et al 2010 ‘Reasons for not seeking medical help for severe pelvic floor symptoms: a qualitative study in survivors of gynaecological cancer’
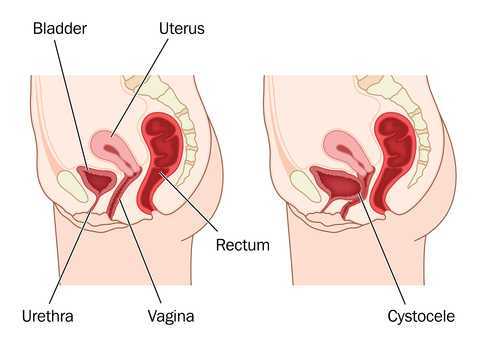
The new year is here and with it, lots of motivational posting about exercise and weight loss…but how is this desire for ‘new year, new you’ affecting peri-menopausal women with urinary dysfunction? It has been established that the lower urinary tract is sensitive to the effects of estrogen, sharing a common embryological origin with the female genital tract, the urogenital sinus. Urge urinary incontinence is more prevalent after the menopause, and the peak prevalence of stress incontinence occurs around the time of the menopause (Quinn et al 2009). Zhu et al looked at the risk factors for urinary incontinence in women and found that some of the main contributors include peri/post-menopausal status, constipation and central obesity (women's waist circumference, >/=80 cm) along with vaginal delivery/multiparity.
 Could weight loss directly impact urinary incontinence in menopausal women? In a word – yes. ‘Weight reduction is an effective treatment for overweight and obese women with UI. Weight loss of 5% to 10% has an efficacy similar to that of other nonsurgical treatments and should be considered a first line therapy for incontinence’ (Subak et al 2005) But do these benefits last? Again – yes! ‘Weight loss intervention reduced the frequency of stress incontinence episodes through 12 months and improved patient satisfaction with changes in incontinence through 18 months. Improving weight loss maintenance may provide longer term benefits for urinary incontinence.’ (Wing et al 2010)
Could weight loss directly impact urinary incontinence in menopausal women? In a word – yes. ‘Weight reduction is an effective treatment for overweight and obese women with UI. Weight loss of 5% to 10% has an efficacy similar to that of other nonsurgical treatments and should be considered a first line therapy for incontinence’ (Subak et al 2005) But do these benefits last? Again – yes! ‘Weight loss intervention reduced the frequency of stress incontinence episodes through 12 months and improved patient satisfaction with changes in incontinence through 18 months. Improving weight loss maintenance may provide longer term benefits for urinary incontinence.’ (Wing et al 2010)
The other major health issues facing women at midlife include an increased risk for cardiovascular disease, Type 2 Diabetes and Bone Health problems – all of which are responsive to lifestyle interventions, particularly exercise and stress management. In their paper looking at lifestyle weight loss interventions, Franz et al found that ‘…a weight loss of >5% appears necessary for beneficial effects on HbA1c, lipids, and blood pressure. Achieving this level of weight loss requires intense interventions, including energy restriction, regular physical activity, and frequent contact with health professionals’. 5% weight loss is the same amount of weight loss necessary to provide significant benefits for urinary incontinence at midlife.
Successful weight management depends on nutritional intake, exercise and psychosocial considerations such as stress management, but for the menopausal woman, hormonal balance can also have an effect on not only bladder and bowel dysfunction but changing metabolic rates, thyroid issues and altered weight distribution patterns. As pelvic rehab therapists, we are all aware that pelvic health issues can be a barrier to exercise participation but sensitive awareness of the other particular challenges facing midlife women can make the difference in developing a beneficial therapeutic alliance and a journey back to optimal health. If you would like to explore the topics surrounding optimal health at menopause, why not join me in California in February?
Climacteric. 2009 Apr;12(2):106-13. ‘The effects of hormones on urinary incontinence in postmenopausal women.’ Quinn SD, Domoney C. Menopause. 2009 Jul-Aug;16(4):831-6. The epidemiological study of women with urinary incontinence and risk factors for stress urinary incontinence in China’ Zhu L, Lang J, Liu C, Han S, Huang J, Li X. J Urol. 2005 Jul;174(1):190-5. Weight loss: a novel and effective treatment for urinary incontinence’ Subak LL, Whitcomb E, Shen H, Saxton J, Vittinghoff E, Brown JS. J Urol. 2010 Sep;184(3):1005-10. Effect of weight loss on urinary incontinence in overweight and obese women: results at 12 and 18 months Wing RR, West DS, Grady D, Creasman JM, Richter HE, Myers D, Burgio KL, Franklin F, Gorin AA, Vittinghoff E, Macer J, Kusek JW, Subak LL; Program to Reduce Incontinence by Diet and Exercise Group. J Acad Nutr Diet. 2015 Sep;115(9):1447-63. doi: 10.1016/j.jand.2015.02.031. Epub 2015 Apr 29. Lifestyle weight-loss intervention outcomes in overweight and obese adults with type 2 diabetes: a systematic review and meta-analysis of randomized clinical trials. Franz MJ, Boucher JL, Rutten-Ramos S, VanWormer JJ. Lean, M, & Lara, J & O Hill, J (2007) Strategies for preventing obesity. In: Sattar, N & Lean, M (eds.) ABC of Obesity. Oxford, Blackwell Publishing.
Perimenopausal pelvic health issues are, for many of us, some of the most common issues that we see in the women that we work with. Urinary incontinence is one of the most important issues for peri- and postmenopausal women. In Melville’s study1 of U.S. women, half of the participants between the ages of 50 and 90 experienced urine leakage every month. Zhu’s 2008 study2 looked at the risk factors for SUI - Multiple vaginal deliveries, Age/postmenopausal status, Chronic pelvic pain, Obesity, lack of exercise, constipation, and hypertension. But what is not often (enough) looked at in the research, is the link between urinary dysfunction and sexual dysfunction – usually because questions aren’t asked or assumptions are made. In Mestre et al’s 2015 paper3, they write ‘…Integrating sexual health in clinical practice is important. In women with pelvic floor disorders, the evaluation of the anatomical defects, lower urinary tract function and the anorectal function often receives more attention than sexual function.’
 But are they linked?
But are they linked?
In Moller’s exploration of this topic, they report that lower urinary tract symptoms (LUTS) have a profound impact on women’s physical, social, and sexual wellbeing. Unsurprisingly (to pelvic rehab specialists at least!), they found that the LUTS are likely to affect sexual activity. Conversely, sexual activity may affect the occurrence of LUTS. The aims of the Moller study were to elucidate to which extent LUTS affect sexual function and to which extent sexual function affect LUTS in an unselected population of middle-aged women in 1 year. A questionnaire was sent to 4,000 unselected women aged 40–60 years. Compared to women having sexual relationship, a statistically significant 3 to 6 fold higher prevalence of LUTS was observed in women with no sexual relationship. In women who ceased sexual relationship an increase in the de novo occurrence of most LUTS was observed. In women who resumed sexual relationship a decrease in LUTS was observed. In women whose sexual activity was unchanged no change in the occurrence of LUTS. So they rightfully concluded ‘…sexual inactivity may lead to LUTS and vice versa.’
In my Menopause course, we will explore the range of perimenopausal pelvic health issues that many women face and their inter-related nature – not just with each other but also how orthopaedic, endocrine and gastro-intestinal health issues influence pelvic health and wellness. Interested in learning more? Come and join the conversation in California in February 2018!
1. Melville JL, et al. Urinary incontinence in US women: a population-based study. Arch Intern Med 2005;165(5):537-42 - See more at: http://www.nursingcenter.com/lnc/JournalArticle?Article_ID=698029#sthash.cm8A90tS.dpuf
2. Zhu L1, Lang J, Wang H, Han S, Huang J. Menopause. 2008 May-Jun;15(3):566-9. The prevalence of and potential risk factors for female urinary incontinence in Beijing, China
3. Mestre M, Lleberia J, Pubill J, Espuña-Pons M Actas Urol Esp. 2015 Apr;39(3):175-82. Epub 2014 Aug 28. Questionnaires in the assessment of sexual function in women with urinary incontinence and pelvic organ prolapse.
What's the evidence, and what's the answer?
In getting ready to teach my Menopause course in Minneapolis next month, I always like to do a review of the evidence, to see what’s new, or what’s changed. What has changed over the past few years – more and more evidence to support the role of skilled rehab providers, using evidence based assessment techniques to gauge the grade of pelvic organ prolapse and assess the risk of levator avulsion. What hasn’t changed enough – the level of awareness of the benefits of pelvic rehab in managing, or in some cases even reversing, the effects and symptoms of prolapse.
 Dr Peter Dietz, from the University of Sydney, writes ‘…although clinical anecdote suggests some physiotherapists recognize other characteristics suggesting muscle dysfunction (e.g. holes, gaps, ridges, scarring) or pelvic floor dysfunction (e.g. width between medial edges of pelvic floor muscle) with palpation it is difficult to find any literature describing the techniques needed to do this or their accuracy or repeatability. Mantle (in 2004) noted that with training and experience a physiotherapist might be able to discern muscle integrity, scarring, and the width between the medial borders of the pelvic floor muscles, with palpation. It is not clear to what extent physiotherapists are able to do this reliably or how such characteristics are to be recorded.’
Dr Peter Dietz, from the University of Sydney, writes ‘…although clinical anecdote suggests some physiotherapists recognize other characteristics suggesting muscle dysfunction (e.g. holes, gaps, ridges, scarring) or pelvic floor dysfunction (e.g. width between medial edges of pelvic floor muscle) with palpation it is difficult to find any literature describing the techniques needed to do this or their accuracy or repeatability. Mantle (in 2004) noted that with training and experience a physiotherapist might be able to discern muscle integrity, scarring, and the width between the medial borders of the pelvic floor muscles, with palpation. It is not clear to what extent physiotherapists are able to do this reliably or how such characteristics are to be recorded.’
Dr Dietz describes a palpation technique to assess the integrity of the pubovisceral muscle insertion, by checking the gap between the urethra centrally and the pubovisceral muscle laterally. On levator contraction this gap should be little wider than your index finger, otherwise an avulsion injury is very likely.
There is another aspect of levator assessment that can yield important information on clinical examination. The size of the levator hiatus can be estimated by determining the sum of the genital hiatus (gh) and perineal body (pb) in the context of the ICS POP-Q examination. Gh + pb, ie., the distance between the external urethral meatus and the centre of the anus, when measured on maximal Valsalva with a simple ruler, is highly predictive of symptoms and signs of prolapse, and it is very strongly correlated with hiatal area on Valsalva (Khunda et al., 2011).
Using this research, in the lab sessions of the Menopause course, we will review these palpation and measurement skills to give therapists the skills they need to confidently assess risk of levator avulsion and its impact on pelvic organ prolapse, and to use this information to devise a functionally appropriate rehab program.
Come and join the conversation in my course, Menopause Rehabilitation and Symptom Management!
Khunda A1, Shek KL, Dietz HP., Am J Obstet Gynecol. 2012 Mar;206(3):246.e1-4. doi: 10.1016/j.ajog.2011.10.876. Epub 2011 Nov 7. Can ballooning of the levator hiatus be determined clinically?
A recent systematic review by Bernard et al (2016) looked at the effects of radiation therapy on the structure and function of the pelvic floor muscles of patients with cancer in the pelvic area. Although surgery and chemotherapy are often used treatment approaches in the management of pelvic cancers, this paper specifically focused on radiation therapy: ‘… is often recommended in the treatment of pelvic cancers. Following radiation therapy, a high prevalence of pelvic floor dysfunctions (urinary incontinence, dyspareunia, and fecal incontinence) is reported. However, changes in pelvic floor muscles after radiation therapy remain unclear. The purpose of this review was to systematically document the effects of radiation therapy on the pelvic floor muscle structure and function in patients with cancer in the pelvic area.’
 The paper concluded that ‘…There is some evidence that radiation therapy has detrimental impacts on both pelvic floor muscles' structure and function’ and that ‘A better understanding of muscle damage and dysfunction following radiation therapy treatment will improve pelvic floor rehabilitation and, potentially, prevention of its detrimental impacts.’
The paper concluded that ‘…There is some evidence that radiation therapy has detrimental impacts on both pelvic floor muscles' structure and function’ and that ‘A better understanding of muscle damage and dysfunction following radiation therapy treatment will improve pelvic floor rehabilitation and, potentially, prevention of its detrimental impacts.’
Pelvic floor therapists already working in the field of gynecologic oncology will be all too aware of the impacts clinically and functionally on pelvic cancer survivors’ quality of life. We are in a privileged position to provide an evidence based and solution focused approach to the pelvic health issues that are so often under-recognized, and frankly under-addressed for women undergoing treatment for pelvic cancers.
Whether it is advice on managing anal fissures (skin protection, down-training overactive pelvic floor muscles, achieving good stool consistency, teaching defecatory techniques) or dealing with dyspareunia (dilator or vibrator selection, choosing and using an appropriate lubricant, dealing with the ergonomic or orthopedic challenges that can be a barrier to returning to sexual function and enjoyment), pelvic rehab practitioners are probably the best clinicians for optimizing a return to both pelvic and global health during and after treatment for pelvic cancers.
But one of the biggest barriers we face is lack of awareness – on the part of the patients but also, unfortunately the lack of awareness in the medical and oncology community about the benefits of pelvic rehab. Happily this situation is improving – not only is the evidence base expanding from the researchers, but oncologists are recognizing that pelvic rehab is a key component of regaining quality and not just quantity of life after treatment ends. As Yang reported in his 2012 paper – pelvic floor rehab programs improve pelvic floor function (particularly urinary continence and sexual function) and overall quality of life in gynecologic cancer patients. And perhaps, most heartening of all, was his statement that "Pelvic Floor Rehab Physiotherapy is effective even in gynecologic cancer survivors who need it the most"
You can learn more about pelvic floor muscle rehabilitation for cancer patients by attending "Oncology and the Female Pelvic Floor: Female Reproductive and Gynecologic Cancers" on April 29-30, 2017 in Maywood, IL.
‘Effects of radiation therapy on the structure and function of the pelvic floor muscles of patients with cancer in the pelvic area: a systematic review.’ J Cancer Surviv. 2016 Apr;10(2):351-62. doi: 10.1007/s11764-015-0481-8. Epub 2015 Aug 28. Bernard, S. et al
‘Effect of a pelvic floor muscle training program on gynecologic cancer survivors with pelvic floor dysfunction: a randomized controlled trial.’ Gynecol Oncol. 2012 Jun;125(3):705-11. doi: 10.1016/j.ygyno.2012.03.045. Epub 2012 Apr 1. Yang EJ, et al
