Pelvic Organ Prolapse and Levator Avulsion
What's the evidence, and what's the answer?
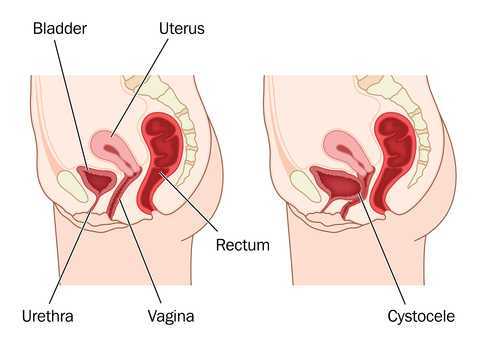
In getting ready to teach my Menopause course in Minneapolis next month, I always like to do a review of the evidence, to see what’s new, or what’s changed. What has changed over the past few years – more and more evidence to support the role of skilled rehab providers, using evidence based assessment techniques to gauge the grade of pelvic organ prolapse and assess the risk of levator avulsion. What hasn’t changed enough – the level of awareness of the benefits of pelvic rehab in managing, or in some cases even reversing, the effects and symptoms of prolapse.
 Dr Peter Dietz, from the University of Sydney, writes ‘…although clinical anecdote suggests some physiotherapists recognize other characteristics suggesting muscle dysfunction (e.g. holes, gaps, ridges, scarring) or pelvic floor dysfunction (e.g. width between medial edges of pelvic floor muscle) with palpation it is difficult to find any literature describing the techniques needed to do this or their accuracy or repeatability. Mantle (in 2004) noted that with training and experience a physiotherapist might be able to discern muscle integrity, scarring, and the width between the medial borders of the pelvic floor muscles, with palpation. It is not clear to what extent physiotherapists are able to do this reliably or how such characteristics are to be recorded.’
Dr Peter Dietz, from the University of Sydney, writes ‘…although clinical anecdote suggests some physiotherapists recognize other characteristics suggesting muscle dysfunction (e.g. holes, gaps, ridges, scarring) or pelvic floor dysfunction (e.g. width between medial edges of pelvic floor muscle) with palpation it is difficult to find any literature describing the techniques needed to do this or their accuracy or repeatability. Mantle (in 2004) noted that with training and experience a physiotherapist might be able to discern muscle integrity, scarring, and the width between the medial borders of the pelvic floor muscles, with palpation. It is not clear to what extent physiotherapists are able to do this reliably or how such characteristics are to be recorded.’
Dr Dietz describes a palpation technique to assess the integrity of the pubovisceral muscle insertion, by checking the gap between the urethra centrally and the pubovisceral muscle laterally. On levator contraction this gap should be little wider than your index finger, otherwise an avulsion injury is very likely.
There is another aspect of levator assessment that can yield important information on clinical examination. The size of the levator hiatus can be estimated by determining the sum of the genital hiatus (gh) and perineal body (pb) in the context of the ICS POP-Q examination. Gh + pb, ie., the distance between the external urethral meatus and the centre of the anus, when measured on maximal Valsalva with a simple ruler, is highly predictive of symptoms and signs of prolapse, and it is very strongly correlated with hiatal area on Valsalva (Khunda et al., 2011).
Using this research, in the lab sessions of the Menopause course, we will review these palpation and measurement skills to give therapists the skills they need to confidently assess risk of levator avulsion and its impact on pelvic organ prolapse, and to use this information to devise a functionally appropriate rehab program.
Come and join the conversation in my course, Menopause Rehabilitation and Symptom Management!
Khunda A1, Shek KL, Dietz HP., Am J Obstet Gynecol. 2012 Mar;206(3):246.e1-4. doi: 10.1016/j.ajog.2011.10.876. Epub 2011 Nov 7. Can ballooning of the levator hiatus be determined clinically?
By accepting you will be accessing a service provided by a third-party external to https://hermanwallace.com/









































