Congratulations to Dr. Mia Fine (they/she) for achieving their Ph.D. in Clinical Sexology and on their book titled 'From Unwanted Pain to Sexual Pleasure: Clinical Strategies for Inclusive Care for Patients with Pelvic Floor Pain' for their dissertation doctoral project.
Dr. Fine was gracious enough to share a draft of their dissertation with Herman & Wallace and to answer a couple of questions about how this impacts their practice and what they hope other practitioners will take away from their book and course Sexual Interviewing for Pelvic Health Therapists.
Mia's course is for the pelvic rehab therapist and others in the medical profession who work with patients experiencing pelvic pain, pelvic floor hypertonicity, and other pelvic floor concerns and would like to learn applicable skills from the sex therapist's clinical toolkit. The next course date for Sexual Interviewing for Pelvic Health Therapists is August 13-14,

How does Trauma-Informed Care apply to the skills that you teach in your Sexual Interviewing course?
When I utilize the term ‘trauma-informed’ I am referring to therapeutic work that communicates expectations clearly (including prioritizing people’s access needs with this communication), invites clients awareness of their own agency, and is upfront about my scope of practice and my therapeutic approach, offers mutuality in inviting of questions and ongoing conversation about our work together, awareness that an individual can end therapy at any time, and share information at any time in our therapeutic space.
The modalities I utilize when working with clients who have experienced trauma include Eye Movement Desensitization and Reprocessing (EMDR), Polyvagal Theory, Somatics, and Developmental Theory. While I integrate various theories and modalities into my work with clients, the methods above are empirical in their data to support healing from trauma wounds.
Trauma-informed means humility regarding cultural, racial, gender, sexual, and other minority experiences. I will not know all of the things but I will do my best to self-educate and not leave that responsibility to my clients. When I make a mistake I will appropriately, directly, and compassionately apologize for the harm I caused and invite opportunity for repair should the client be interested. Trauma-informed means collaboration in exploring therapy together, co-creating a space that feels safer to the client and checking in with them when I notice non-verbal cues that indicate activation, honoring a client’s pacing, and bringing awareness to the reality that as a therapist I hold power and while I don’t know a person’s full story there is always the potential for me to unintentionally activate a client so to share this possibility with clients and continuously check in about how our therapy is working for them. I keep my client’s well-being at the forefront of our work and I center their needs at all times while maintaining boundaries that keep everyone as safe and secure as possible.
It is up to us as trauma-informed and inclusive providers to explore a person’s experience of pain by asking questions about onset, process, location, and impact, in addition to offering psychoeducation about anatomy, physiology (arousal, interest, desire), and self-regulation. This must be done alongside commitment to our patient’s co-regulation, normalization, and informed consent concerning the therapeutic process—all of which are needed for comprehensive trauma-informed care.
Can you explain how expanding what 'normal' is to practitioners can impact the patients and clients that they work with?
Sex is not supposed to be painful. How many people have come to me having had painful sexual intercourse for years and reported “pushing through”? The first time having intercourse does not necessarily have to be painful, but when our cultural narratives tell us “the first time having sex is painful for everyone” we end up ignoring the signals our bodies are offering because we have convinced ourselves that the pain is both okay and normal. The “pushing through” is a reflection of misogyny: people assume the first experiences people have with penetration are supposed to be painful. How is this misogynistic? Well, who benefits from a person “pushing through” pain? The partner with the penis. Important to note here as well is that enthusiastic consent is ableist and ignores the mind-body connection because it does not take into account masking or fawning which are common experiences for many.
A quarter of people who experience sexual health concerns share this with their providers. Why such a small fraction? Fear. Fear of embarrassment and shame. Fear that there is something “abnormal” about them that mutates into the shame humans tend to experience in response. Fear that the concern won’t be held or taken seriously by their provider. Fear that, if it is addressed, will be at such a high financial cost that the treatment will be unaffordable. Fear that there’s not enough time or that they won’t be taken seriously. Fear of exclusivity, feeling othered, or misunderstood by their provider. Fear of the unknown because the reality is that people are afraid of what we don’t understand.
One of the major cultural issues we have in the US is the perpetuation of sexual stigma which is largely associated with a lack of comprehensive sex education. People don’t have access to basic information about their own bodies which influences our beliefs about sex, pleasure, agency, communication, and self-awareness. Sex education should be a birthright, and yet we are so far behind the curve that it sometimes feels impossible to break down the barriers.
When I first started in this career it would often take clients months of working with me to feel comfortable enough to talk about where they felt pain during sex, but in developing the tools to co-create safety in our therapeutic relationship and the skills to ask the important questions with compassion and patience, I learned how to better hold space for healing.
Patients don’t often know what information is important for them to share with us (which is why offering visuals of where the pain is located is important). How could they know what information is important to offer when mental and sexual health are so deeply stigmatized? The stress of shame and embarrassment that people feel about their bodies is emotional pain that further exacerbates the physical pain that they came to therapy to address in the first place. It’s a terrible and self-perpetuating cycle.
I teach people the difference between a vulva and a vagina one thousand times a year. If a client does not know the terminology for labia, vulva, vagina, and clitoris, how are they supposed to know when their sexual health is of concern? If a person enters sex therapy with “sexual pain” but is unable to distinguish the difference between their labia and vagina (that they are different body parts, where they are located, and what their functions are) we cannot expect them to accurately articulate the location of pain or comprehend potential solutions. “What is your hygiene process when cleaning your vulva?” may activate the fight or flight response in clients if they do not know what their vulva is or that there could be a good hygiene process, in addition to the shame of not knowing. How are they supposed to know where or to whom they may ask for help?
An online search for “anatomical vulva”, “pelvic floor pain”, “vaginismus treatment” and 99% of the images and figures you will see are those of hairless, slender bodies with white/light skin and small labia. Racism and white supremacy are present everywhere. The anatomical depictions of vulvas are of white bodies, the people modeling in vaginismus treatment advertisements are white, and the language is geared toward and written for white people. I was intentional about not featuring white vulvas in this book because white bodies should not be the default of what is mainstream. This lack of diversity in skin tone and variation of body type is another reflection of racism called “colorism”. White and light skin bodies are viewed as more ‘normal’ and when we continue to center white bodies in visuals “because that is what is available” we perpetuate white supremacy. One goal is to disrupt the idea and practice of whiteness as the default. This is what it means to practice anti-racism and attempt to divorce ourselves from white supremacy.
The impact of shame shows up in the pervasive erotophobia rampant in our society. Erotophobia can be broadly defined as a “fear of sex” or more specifically a “fear of intercourse”. When erotophobia is judgment as a result of societal shame and stigma, we can navigate it by deconstructing the etiology and impact of messages received; when it is a result of a mental health condition such as Obsessive Compulsive Disorder (OCD) or Post Traumatic Stress Disorder (PTSD), we do deep trauma and/or anxiety/exposure work. Because of the vast impact of shame, people fear sharing sensitive information about themselves with others, including therapists who are trained to help them. Often, therapists are untrained in sexual health which also can contribute to erotophobia and shame. When therapists have not done their own work on sexuality, and remain untrained in these areas, they may be afraid to discuss sex with their clients which reinforces the belief that topics regarding sex are shameful.
When people do not have the language to articulate what is happening in their body, as significant as the pain or discomfort might be, talking about sex with a provider is often the last item on a long list of concerns they bring to a medical appointment. Symptoms of sexual pain may be hidden by other “more pressing” concerns such as anxiety, depression, PTSD, or sleep issues. While these are of course vital for a medical provider to know, having 20 minute appointments with a physician who will prioritize the “presenting concern” that they came in to seek treatment for leaves very little time to discuss unwanted sexual pain. After 15-20 minutes of a medical appointment (if it goes well), a patient might feel comfortable enough to bring up their sexual concern, but this might leave 1 minute for it to be acknowledged and no time to conduct a comprehensive assessment or develop an intentional plan. We call these last-minute oh-by-the-way’s “door-knobbing” for a reason. This is a call for medical clinics to have training in sexual health so they can create intake documentation that explores clients’ sexual health and ask the questions that are vital to gather necessary information ahead of time.
In the same way that people lack language and anatomic understanding, people also lack awareness of the mind-body relationship. Due to the ableist sex-negative culture in which we live, people are often not taught to have knowledge of or listen to our own body. We’re not taught that pain is a signal from the body telling us that something’s wrong.

Instructor Sarah Hughes, PT, DPT, OCS, CF - L2 sat down with The Pelvic Rehab Report to answer a couple of questions about treating the Crossfit and weightlifting community. Dr. Hughes earned a BS in exercise science from Gonzaga University and a DPT from the University of Washington.
Sarah's specialties include dance medicine, the CrossFit and weightlifting athlete, and conditions of the hip and pelvis such as femoroacetabular impingement and labral tears. She began coaching other PTs who wanted to start their own practices in 2017 and co-founded Full Draw Consulting with her partner Dr. Kate Blankshain.
Sarah teaches Weightlifting and Functional Fitness Athletes, which s scheduled for August 7th and October 15th of this year.
What are three things you wish you knew when you first started treating the athletic community?
First, I wish that I had had the confidence to treat these athletes the way I saw fit earlier in my career. For a long time, I felt weird treating CrossFit athletes in the clinics I worked in because I felt that my peers were judging me. My colleagues (and many PTs at the time) were wary about the sport and believed it was dangerous for patients. This is a viewpoint I am working to change in our profession.
Secondly, I wish I knew more about how to scale movements in a way that is relevant to the patients and the stimulus they are striving for. For example, if a patient wants to be able to do kipping pull-ups in a workout, giving them banded strict pull-ups as a substitute is not the only option. What about the metabolic conditioning part of the equation? What about looking at the volume and how that is impacting the tissue of concern? This is a big topic that we discuss in my course.
And finally, I wish I knew that being an effective therapist for these athletes does not mean being the top athlete in the gym. In fact, just as with coaching, you do not have to be a great athlete to be a great PT. Again, this is something that I want to change as far too few physical therapists are comfortable treating these or advertising that they treat these athletes because they are not Crossfit athletes (or are not ELITE Crossfit athletes) themselves.
What lesson have you learned in a course, from an instructor, or from a colleague or mentor that has stayed with you?
One important lesson that has stayed with me came from a colleague in Seattle who started her business a year before I started mine. She told me that I needed to listen to my gut when it came to treating these athletes. She reminded me that my experience with CrossFit as a sport, as an athlete, as a coach, and as a PT put me in a position to be an expert on how to help these folks. What I did not need was to allow other physical therapists to sway my thinking and cause me to doubt myself by insisting that we should not be condoning the sport. TRUST YOUR GUT. If you think you are doing what is right for the patients, you are. You might not be right for every patient and that is OK! I am certainly not the right therapist for everyone, but I am indeed right for the community I serve.
Weightlifting and Functional Fitness Athletes - Remote Course

When it comes to Crossfit and Weightlifting, opinions are divided among Physical Therapists and other clinicians. In this half-day, remote continuing education course, instructor Sarah Haran PT, DPT, OCS, CF-L2 looks at the realities and myths related to Crossfit and high-level weight-lifting with the goal of answering “how can we meet these athletes where they are in order to keep them healthy, happy and performing in the sport they love?"
This course reviews the history and style of Crossfit exercise and Weightlifting, as well as examines the role that therapists must play for these athletes. Labs will introduce and practice the movements of Crossfit and Weightlifting, discussing the points of performance for each movement. Practitioners will learn how to speak the language of the athlete and will experience what the movement feels like so that they may help their client to break it down into its components for a sport-specific rehab progression.
The goal of this course is to provide a realistic breakdown of what these athletes are doing on a daily basis and to help remove the stigma that this type of exercise is bad for our patients. It will be important to examine the holes in training for these athletes as well as where we are lacking as therapists in our ability to help these individuals. We will also discuss mindset and cultural issues such as the use of exercise gear (i.e. straps or a weightlifting belt), body image, and the concept of "lifestyle fitness". Finally, we will discuss marketing our practices to these patients.
Course Dates: August 7th and October 15

Faculty member Ginger Garner PT, DPT, ATC/L is offering a new short course, The Voice and The Pelvic Floor. This course introduces foundational concepts needed to be able to use vocal techniques to treat the pelvic floor and core. Dr. Garner is a clinician, educator, and longtime advocate committed to making physical therapy services accessible, affordable, and equitable, especially for pelvic health.

When you think of pelvic health, what comes to mind? Obvious variables like the pelvic floor & girdle, abdominals and related synergists, mental health, and gut and respiratory health are probably at the top of your list.
But how often do we consider the voice as a biomarker of pelvic health? It can impact all of the variables above and more.
Historically, speech-language pathologists’ study of vocal health has stopped at the respiratory diaphragm, while physical and occupational therapists’ study of pelvic health has stopped, well, in the same place. Neither has traveled beyond that until recently.
However, there is a third diaphragm beyond the respiratory and pelvic, the laryngeal diaphragm. It’s also known as the cervical, cervico-thoracic, vocal, and/or thoracic diaphragm. The three diaphragms include:
- The Laryngeal Diaphragm - is responsible for neurological optimization of stress response and physiological control of swallowing and communication; but, it also influences vagal tone for cardiorespiratory functioning and respiratory and pelvic diaphragm functioning. It contains the muscles that are responsible for phonation, which includes intrinsic variables such as the arytenoids, but also extrinsic components which have a direct impact on the vocal fold health, such as the suprahyoid muscles.
- The Respiratory Diaphragm - is the connecting point between cephalad and caudad diaphragms and is the main muscle influencing pulmonary function. However, the respiratory diaphragm exacts a major influence on mind-body health, which goes far beyond pressure regulation of the vocal and pelvic diaphragms.
- The Pelvic Diaphragm - is the terminal end of the tri-diaphragmatic (3D) system, and can bear the brunt of trauma and impairment if dysfunction is present in the two upstream diaphragms. The pelvic diaphragm contains the levator ani, coccygeus, and related synergists, pelvic fascia, and neurovascular structures, which in turn can work with or against breathing and voicing tasks.
The diaphragms are in constant movement and none work in isolation. Together, their intersectional action provides us with the key to both internal and external biopsychosocial stability and structure of the mind-body.
The laryngeal diaphragm has a supradiaphragmatic vagal impact, while the pelvic diaphragm exacts subdiaphragmatic vagal health, chiefly through afferent and efferent input, respectively. The 10th cranial nerve lives up to its namesake, “the wandering,” as it touches each of the three diaphragms on its journey, harnessing the capacity to lessen pelvic and visceral pain, while also improving vocal quality and lung function, and changing pain, mood, and digestive function.
The mind-body interface of the 3D system has been further defined in recent years, broken down into a voluntary motor system (the one we spend all our time studying and treating), and the “emotional motor system,” and the implications are profound. Anatomists and researchers tell us that in order to generate speech, we need both motor systems to function. But specifically, our emotional motor system must first perceive safety before speech can be produced or produced well.
To get a feel for your own emotional motor system health, try this brief exercise:
- Think about a recent incident that made you feel nervous, or anxious.
- How well could you breathe?
- Talk?
- Sing or hum?
- Engage in intimacy with someone?
Not very well, right? This feeling is the fallout from your emotional motor system perceiving danger or threat. It’s what Dr. Stephen Porges means by the phrase, “neuroception.” Neuroception is the ability to detect risk - but it’s not just the ability to detect it - neuroception is the ability to accurately detect risk.
Here lies the problem:
If we cannot detect external risk or internal threat accurately, aka if our neuroception wiring is faulty, then we may move to 1 of 4 default modes for behavior: fight, flight, freeze, or fawn. If we are left in this state of reactivity, courtesy of the sympathetic nervous system, then polyvagal theory predicts we will enter into a dissociative state, termed a dorsal vagal response (DVR). The DVR drives self-preservation in severe trauma states, which can preserve life; but it is also to blame for bradycardia and left unchecked, death. Especially now post-COVID, it’s imperative that all therapists understand how to recognize, screen for, and help nurture healthy self-regulatory strategies via trauma-informed care.
We must also learn how to create a therapeutic landscape conducive to healthy neuroception, one that appeals to the “safety switch” of the emotional motor system. Establishing this healthy therapeutic alliance with our patients and clients is critical in pelvic health because the same motor system that controls the creation of sound, dictates everything associated with pelvic health, including micturition, defecation, partuition, stress response, and sexual function.
Understanding the basis of “3D” neurophysiology makes targeting the voice a perfect alternate but necessary pathway for successful comprehensive pelvic health care. The ability to create sound literally determines how we interact with the world around us, and whether or not we can do so with empathy and safety. Additionally, the success of our intervention as pelvic health therapists is also determined by the degree to which we are using a biopsychosocial model, which has long been supported as the most effective and cost-effective way to manage pain and tackle chronic disease and impairment.
What does including the voice look like in pelvic health?
For starters, the first step is evaluating the orofacial and vocal health of the patient or client. Second, and perhaps surprising to some, is the evaluation of the therapist’s own voice as a therapeutic agent. These assessments work to identify red flags that place undue stress through the downstream diaphragms and stress response system. More complex assessment can include lumbopelvic ultrasound imaging as well, which provides a more comprehensive way to individualize therapy prescription.
Assessment is essentially a 4-pronged process - The first two prongs consist of building on existing evaluation skills in respiratory, core, and pelvic floor and girdle assessment. The final two include an assessment of the physiological functioning of the orofacial area and voice and an evaluation of psychosocial determinants which would influence cranial nerve and vocal functioning. The voice is an incredible tool for improving pelvic health outcomes, if we learn how to harness its frequency and power.
Join Dr. Ginger Garner for a virtual short course, The Voice and the Pelvic Floor scheduled for October 1, 2022, to learn more.
Sources
- HOLSTEGE, G., 2016. How the Emotional Motor System Controls the Pelvic Organs. Sexual Medicine Reviews, 4(4), pp. 303-328.
- HOLSTEGE, G. and SUBRAMANIAN, H.H., 2016. Two different motor systems are needed to generate human speech. The Journal of comparative neurology, 524(8), pp. 1558-1577.
- Speer LM, Mushkbar S, Erbele T. Chronic Pelvic Pain in Women. afp. 2016;93(5):380-387.
- Miciak M, Gross DP, Joyce A. A review of the psychotherapeutic “common factors” model and its application in physical therapy: the need to consider general effects in physical therapy practice. Scand J Caring Sci. 2012;26(2):394-403. doi:10.1111/j.1471-6712.2011.00923.x
- Padoa A, McLean L, Morin M, Vandyken C. The Overactive Pelvic Floor (OPF) and Sexual Dysfunction. Part 2: Evaluation and Treatment of Sexual Dysfunction in OPF Patients. Sex Med Rev. 2021;9(1):76-92. doi:10.1016/j.sxmr.2020.04.002
- Wijma AJ, van Wilgen CP, Meeus M, Nijs J. Clinical biopsychosocial physiotherapy assessment of patients with chronic pain: The first step in pain neuroscience education. Physiother Theory Pract. 2016;32(5):368-384. doi:10.1080/09593985.2016.1194651
- Porges SW. The polyvagal perspective. BiolPsychol. 2007;74(2):116-143.
Maricel Briones, DPT, CMTPT, OCS sat down with The Pelvic Rehab Report this week to discuss herself and how she came to TA for Herman & Wallace. You can find Maricel this fall TA'ing Pelvic Floor Level 2B in Virginia Beach, VA.
Hi Maricel, can you share a little bit about yourself and your clinical practice?
Hi, I'm Maricel Briones, DPT, CMTPT, OCS and I've lived in Virginia Beach, VA my whole life. I graduated from Old Dominion University with a Bachelor in Exercise Science and followed that up with a Doctorate of Physical Therapy degree. I am now a Partner, Area Director, and Co-Leader of Pelvic Health with Ivy Rehab and have been a practicing therapist since 2012. I became an Orthopedic Clinical Specialist and Certified Myofascial Trigger Point Specialist for Dry Needling and recently became a Pelvic Health Therapist in 2020. My current clinic opened in December 2021, located in the Town Center area of Virginia Beach, VA. We are in the middle of expanding. We are a mix of outpatient orthopedic and pelvic health for men and women. My whole clinic is trained to support each other with all cases, even with pelvic health, and work together as a team for each patient's visit.
What has your educational journey as a pelvic rehab therapist looked like? Where did you start?
I started in early 2020 with Herman & Wallace (H&W) Pelvic Floor Level 1 in Virginia Beach, VA, then continued and took Pelvic Floor Level 2B towards the summer. It started a little slow because of Covid but it picked up in October 2022 and has been very busy since. In 2021, I continued taking more H&W courses including Pelvic Floor Level 2A, Male Pelvic Floor, and Pelvic Floor Capstone. I continued to host around 5-7 H&W courses to review the material and encourage local ortho therapists to join the pelvic health world. I eventually became a teaching assistant (TA) for H&W and have been loving it ever since. I became a Senior TA earlier this year.
How did you get involved in the pelvic rehabilitation field?
My regional director first asked and brought it to my attention, but I declined. A year later, she further explained the impact we can have for patients with pelvic floor conditions and got me convinced. I gave it a shot in 2020 and realized it was where I should be. It's the most rewarding type of treatment we can provide for a patient. We are helping a hidden population that we did not know exists right in front of us. Helping them with critical functions needed in life, voiding, BM, sex, etc.
What patient population do you find most rewarding in treating and why?
Either the pediatric or geriatric population for urinary incontinence (UI). I enjoy teaching them good bladder habits and how to properly contract their pelvic floor muscles. My first patient was an 80-year-old who had urinary incontinence for 20 years and after 1 week of pelvic therapy, she went from changing her pad around 8 times a day to only 2. I had my first pediatric patient who had seen 4 specialists in 1 year for UI. After 2 weeks of pelvic floor rehab, she went from having 4-6 accidents a day to 1-2 every other day.
If you could get a message out to physical therapists about pelvic rehab what would it be?
Don't be afraid of the "V". A lot of PTs are uninterested and do not realize how much pelvic floor muscle training is similar to orthopedic, either stretch it or strengthen it, and provide a lot of education on habits. Also, it's all about functional movement, so connect the pelvic floor with the upper and lower body for optimal outcomes. I did an internal Ivy Rehab Ted Talk in Florida for our Director's Summit in May 2021, titled "Don't be afraid of the 'V'". What you're nervous of or afraid of, may actually be where you are meant to be or do.
What lesson have you learned in a course, from an instructor, or from a colleague or mentor that has stayed with you?
Continue to learn no matter what, and never settle. My treatment programs and assessments evolve every year because of continued learning and advice from colleagues. Always be open to different approaches and be patient with all complex cases.
What do you find is the most useful resource for your practice?
Facebook groups such as Global Pelvic Physio (run by Michelle Lyons), Pelvic PT Newbies (run by Jessica and Andrew Reale), Pelvic PT Huddle (run by PelvicSanity and Nicole Cozean), and Pelvic Floor Biofeedback (run by Tiffany Ellsworth Lee) have been my go-to for learning about cases, ideas, etc.
What is in store for you in the future as a clinician?
I plan to take the PRPC exam soon for board certification. I am also working with Ivy Rehab to create a year-long Pelvic Health Specialization program.
What has been your favorite Herman & Wallace Course and why?
Pelvic Floor Level 2B, since I learned more in-depth manual therapy for the pelvic floor and it helped nail down the anatomy of the pelvic region. I also love the manual therapy skills that we learned in Capstone.
What lesson have you learned from a Herman & Wallace instructor that has stayed with you?
Lengthen before strengthen!
What do you love about assisting at courses?
It's an information refresher. The more you hear it, the more it sticks. I also love teaching the students the concepts and anatomy that were originally confusing for me.
What is your message to course participants who are just starting their journey?
Continue to take more courses on pelvic floor rehab as there are so many different pelvic health conditions. Take the same concepts you learned about muscle training for any body part and apply them to the pelvic region. Connect the pelvic region to the whole body and focus on actively training it with function. It's not just about motor control of the pelvic floor muscles, it's coordinating it with the abdominals, hips, back, etc. Not all visits are hands-on one-on one-on-one. If you create a robust well-rounded program for them and they will progress quicker than you expect.
Alyson Lowrey, PT, DPT, OCS is the co-instructor for the H&W course Pain Science for the Chronic Pelvic Pain Population - Remote Course alongside Tara Sullivan, PT, DPT, PRPC, WCS, IF. Alyson treats the pelvic floor patient population through an orthopedic approach, working closely with pelvic floor specialists.
Pain neuroscience education (PNE) is the explanation of the neurophysiological changes in the central nervous system in patients with chronic pain. It includes how the nervous system functions and factors that influence its function such as social, psychological, and environmental factors. Pain neuroscience education aims to increase the patient’s knowledge about pain, decrease the threat of pain, and allow the patient to reconceptualize pain from a biopsychosocial perspective.
As a clinician seeing a patient with chronic and complex pain, it can be very daunting trying to determine how much education you should give the patient. Patients are generally very invested in improving their quality of life and therefore invested in learning how to treat their pain. Using techniques such as motivational interviewing is one way to determine if a patient is receptive to new information about pain and how to deliver that information. Education about pain needs to be varied and tailored to each patient based on their prior knowledge and perceptions, learning styles, their language, and their health literacy.
When a patient has an increased understanding of their pain and how their nervous system works, it can change their perspective about their pain by decreasing the threat value of their pain. PNE is the first step in the process of increasing a patient’s pain thresholds during exercise and functional activity. When patients no longer fear their pain as a sign of tissue damage, they can become empowered to re-educate their nervous system and pain processing centers in their brain. As providers, we are able to do this in several ways. We can do this by helping build new coping strategies and thought processes around their pain and dispelling misconceptions about their pain and physical ailments. We can suggest lifestyle and movement modifications that allow for more functional movement that doesn’t increase their pain activation centers. We can also adjust and modify our treatment plan around the patient's needs for success at each session. Consistently being a voice of encouragement, empowerment, and validation is also a very important component of PNE and our treatment as clinicians for our patients with chronic pain.
Pain Science for the Chronic Pelvic Pain Population - Remote Course
Course Date
October 8th-9th
Description
This course provides a thorough introduction to pain science concepts including classifications of pain mechanisms, peripheral pain generators, peripheral sensitization and central sensitization in listed chronic pelvic pain conditions; as well as treatment strategies including therapeutic pain neuroscience education, therapeutic alliance, and the current rehab interventions' influence on central sensitization. The rehab professionals who attend will be provided the understanding and tools needed to identify and treat patients with chronic pelvic pain from a pain science perspective. Lecture topics include the history of pain, pain physiology, central and peripheral sensitization, sensitization in chronic pelvic pain conditions, therapeutic alliance, pain science and trauma-informed care, therapeutic pain neuroscience education, the influence of rehab interventions on the CNS, and specific case examples for sensitization in CPP.

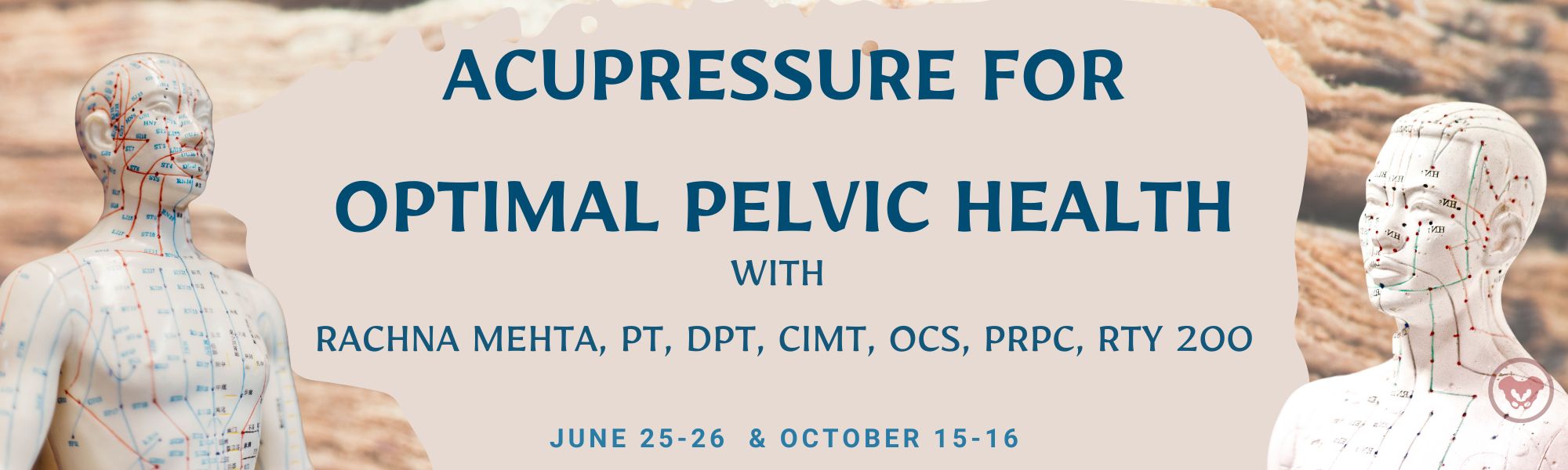
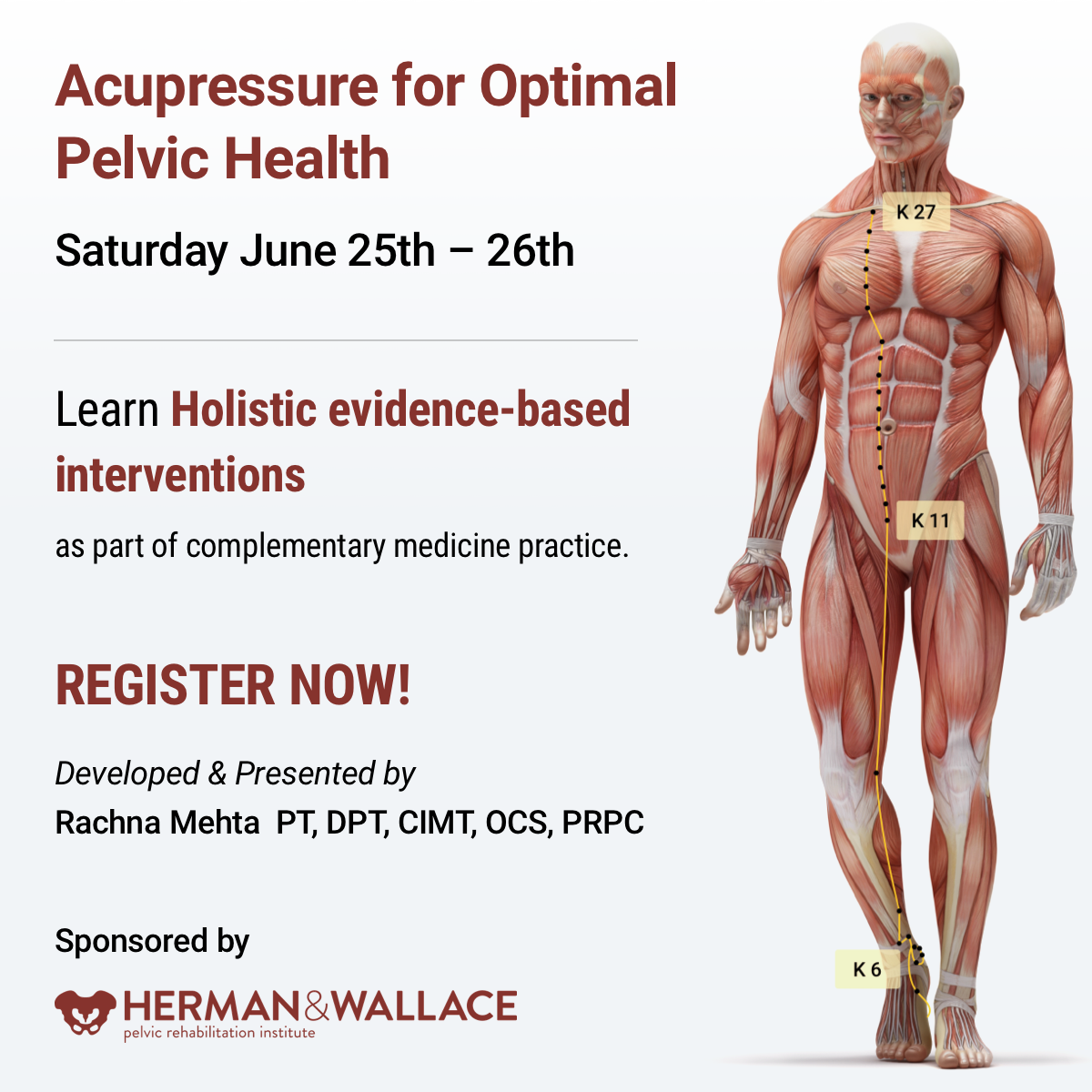
Rachna Mehta, PT, DPT, CIMT, OCS, PRPC is the author and instructor of the new Acupressure for Pelvic Health course. Rachna brings a wealth of experience to her physical therapy practice and has a personal interest in various eastern holistic healing traditions. Her course Acupressure for Optimal Pelvic Health brings a unique evidence-based approach and explores complementary medicine as a powerful tool for holistic management of the individual as a whole focusing on the physical, emotional, and energy body.
Constipation is a common functional gastrointestinal disorder, with prevalence in the general population of approximately 20%. In the elderly population, the incidence of constipation is higher compared to the younger population, with elderly females suffering more often from severe constipation (1).
Is there a magic button in the perineum that makes it easier to defecate? In case you have wondered, the answer is YES!!!
A study done recently by Dr. Ryan Abbott and colleagues at UCLA’s Department of Medicine found just that. A randomized control trial was conducted with 100 subjects who had functional constipation, half randomized to treatment and half to the control group. The treatment group received training in self perineal acupressure along with standard treatment options. The control group only received information about standard constipation treatment options.
Perineal self-acupressure technique was found to be remarkably effective with statistically significant and clinically meaningful improvements in Patient Assessments of Constipation Quality of Life (PAC-QOL All), modified Bowel Function Index (BFI), and the Short-Form Health Survey (SF-12v2). Patients in the treatment group also reported substantial satisfaction with perineal self-acupressure technique:
- 72% of the treatment group reported that the perineal pressure technique helped them to “break up, soften, or pass stools."
- 54% reported that the technique helped them to “avoid having hemorrhoid or lessened the impact of existing hemorrhoid."
- 72% reported that the technique helped them to “avoid or better manage the effects of constipation."
- 82% of the treatment group patients indicated that they would continue to use the technique, and 72% indicated that they would recommend the technique to family and friends (2).
In this study, perineal acupressure was applied at the Acupressure point Huiyin or CV 1 located at the perineum. Huiyin is used in Traditional Chinese Medicine (TCM) not only to treat constipation, but also a variety of conditions including impotence, hemorrhoids, rectal prolapse, and dysmenorrhea. In addition, there are several key Acu-points like St 36 on the Stomach meridian and CV 6 which can help with constipation and digestive disorders.
Acupressure is based on Traditional Chinese meridian theory in which acupuncture points are pressed to stimulate the flow of energy or Qi and these points reflect disorders of visceral conditions and organs.
Acupuncture meridians are believed to form a network throughout the body, connecting peripheral tissues to each other and to the central viscera. This tissue network is also continuous with more specialized connective tissues such as periosteum, perimysium, perineurium, pleura, peritoneum, and meninges (3).
Dr. Abbott’s study suggests that clinicians should consider incorporating perineal self-acupressure technique as a first-line treatment for constipation, along with conventional interventions such as increased exercise and dietary fiber intake. Benefits include being non-invasive and non-pharmacological treatment intervention for constipation with likely a lower risk for side effects and complications than commonly used medications such as stool softeners, fiber supplements, stimulants, laxatives, and lubricants (2).
As medical providers, we are uniquely trained to combine our orthopedic skills with mindfulness-based holistic interventions to empower our patients by giving them the tools and self-care regimens to live healthier pain-free lives.
The upcoming remote course Acupressure for Optimal Pelvic Health, scheduled for July 24-25, 2021, brings a unique evidence-based approach on the use of potent Acupressure points for treating a wide variety of pelvic health conditions including chronic pelvic pain, dysmenorrhea, constipation, digestive disturbances and urinary dysfunctions to name a few.
The course also offers an introduction to Yin yoga and explores Yin poses within each meridian to channelize energy through neurodynamic pathways with powerful integrative applications across multiple systems.
References
- Vazquez Roque M, Bouras EP. Epidemiology and management of chronic constipation in elderly patients. Clin Interv Aging. 2015;10:919-930.
- Abbott R, Ayres I, Hui E, Hui KK. Effect of perineal self-acupressure on constipation: a randomized controlled trial. J Gen Intern Med. 2015;30(4):434-439.
- Kaptchuk TJ. 2000. The web that has no weaver. Understanding Chinese medicine. Chicago: Contemporary Publishing Group, Inc.
5. Lee EJ, Frazier SK. The efficacy of acupressure for symptom management: a systematic review. J Pain Symptom Manage. 2011;42(4):589-603.

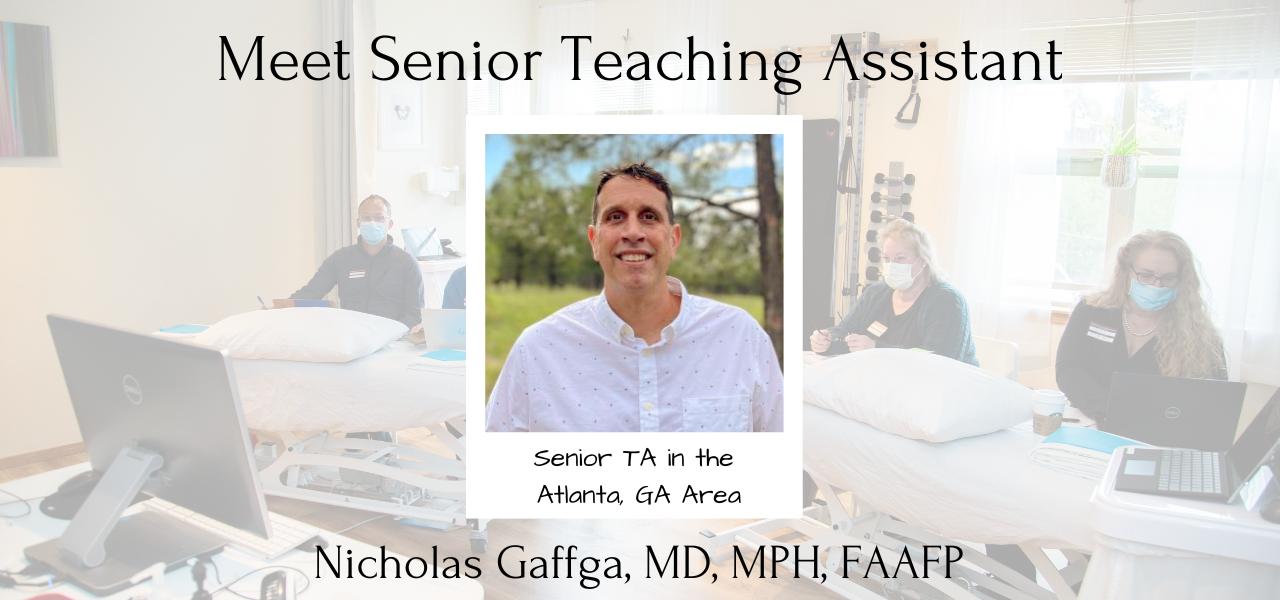
The following is an excerpt from an interview between Niko Gaffga, MD, FAAFP, MPH (NG) and Holly Tanner (HT) about why he is interested in women’s health and the menstrual experience. Niko and Amy Meehan, PT, DPT, MTC have co-authored a specialty course for H&W all about Menstruation and Pelvic Health – to learn more join us in the upcoming remote course on July 16th-17th, 2022. You can watch the full video interview below, or on the Herman & Wallace YouTube Channel.
HT – So menstruation as a topic, what is it that got you so passionate about this particular topic?
NG -Throughout my career and my training, women’s health and OB have been one of my favorite parts of my job. In recent years there was a patient who really inspired me. I came into the room, and she was sitting in the corner in the exam room of the clinic where I worked and she was crying. I came in and I asked, she only spoke Spanish…and I asked her “ How are you doing? What’s happening?” and she was very reluctant to say anything.
I found out through a little bit of discussion that she was feeling pain, and she couldn’t make the pain go away. That she had seen many doctors about it and no one had been able to help her. She was reluctant to show me where on her body – maybe it’s because I’m a man, or maybe it was because she was from a different country – she didn’t feel secure. So I drew a little picture on a piece of paper, and I said “Just point to me on this paper where you feel the pain.” After a while of pointing, talking, and smiling I got to a point where she could explain to me what was happening.
It turns out that she had painful bladder syndrome, or interstitial cystitis, and we worked over the months to get that better. And I have to say, that the next time that I walked into that the next time that I walked into that same room and she was there – she was smiling. She stood up and she gave me a hug – and I said to myself, “This is why I do medicine.”
I think really the breakthrough came when I met her where she was. I took the time to talk to her in her language, show her a piece of paper, and wait for her to say what she felt. Cause many doctors, you know how they only have two or three minutes to talk with their patients. When I met her halfway, she was able to talk to me about the pain she was feeling, about her menstrual cycles – which I don’t think she had ever discussed with any doctors before.
So that started me down the road in being interested in what can I do – what more can I do to help women. When I see women in the clinic a lot of them don’t want to say anything about their menstrual cycle, and again maybe it’s because I’m a man. Maybe it’s because it’s just a difficult topic to discuss, but I realize that in society we don’t have a lot of chance as men or women to talk about the menstrual cycle.
I feel that it is a disservice to women that they don’t have a chance to talk about things that genuinely interest them, are concerning to them, or have questions and are curious about. I feel that there is a stigma, and I think that this course will begin to address it within a small group. But I think eventually, training and working with healthcare providers is one step in making that message available to other people, and to other patients all around the country. So that is how it evolved for me.
One of the most important things for me is that talking about the menstrual experience and women’s health, in general, allows me to change, to give people information, to make decisions in their life that are in alignment with the way that they see the world. I think that not many professions can say that. You know medical professions, physical therapists, doctors, and many other professions - we help people do what they want to do for themselves, and that’s powerful. That’s very powerful.
I think that the most important thing is that I can make a difference in someone else’s life. I’ve seen it when talking to women in the clinic who I’ve seen before. Discussing their menstrual cycle and having them tell me this is the first I’ve spoken about to anyone, much less to a female or a male provider. Hearing someone say that is meaningful. It is a lot of trust that they place in someone to tell them these kinds of things because they are difficult topics. Seeing that you can make a difference in someone else’s life...it means a lot to me, and this is the reason why [I’m so passionate about women’s health and the menstrual experience].

Menstruation and Pelvic Health - July 16-17 2022
The Menstrual cycle is one of the most natural of all human processes and is experienced by half of the population of the world. At any given time, 800 million individuals are menstruating. The Menstrual cycle occurs roughly once a month for roughly 35 to 40 years in a lifetime. That ends up being almost 3000 days, or about 8 years of menses. Many menstruators experience “period shaming” and other forms of socialized stigma around the menstrual experience. It is therefore important to become familiar with this experience and provide care to patients that takes into account their Menstrual Experience.
This two-day remote continuing education course is designed for clinicians who want to obtain advanced knowledge and skills to educate patients on non-hormonal, non-surgical, and non-prescription interventions for improving the Menstrual Experience. Developed by Nicholas Gaffga, MD, MPH, FAAFP, and presented together with Amy Meehan, PT, DPT, MTC, this course is geared toward the pelvic rehab provider looking to impart Menstrual Interventions that:
- Put control in the hands of people who menstruate to identify and carry out the interventions that are appropriate to them
- Use a holistic approach and advanced knowledge and familiarity with body and mind
- Emphasize healthy practices that can positively impact the Menstrual Experience and beyond, in areas such as mental health and chronic diseases
- Discover root causes of issues, rather than quick fixes, to have benefits that are sustainable across the lifespan.

Amanda Davis, PT, DPT, PRPC can be found online at https://www.makeandmanifest.com/. She has generously shared her recent blog with The Pelvic Rehab Report. "Got 30 Minutes? 4 Underestimated Daily Practices to Make Your Lunch Break More Life-Giving" can be found in its original post on her website here: http://www.makeandmanifest.com/blog-lunchbreak/.
Hey there, I'm Amanda. Pelvic rehab therapist, endo warrior, girl mama (despite that whole endo thing), and creator of this space where I'm sharing the story of practicing what I preach and the wins and losses I gather along the way. I love early morning espresso, podcast binging, yoga pants, and scrolling Pinterest for my next obsession (heyyyy fellow libras!). My mission is to help women see the difference between "common" and "normal" and to take their physical, mental, and emotional health beyond the "that's just the way it is" mentality.
Hats off to my fellow 9-5ers who head home after a long day to jump right into their 5-9. If you’re like me, that second “career” includes (but definitely is not limited to) caregiver, dog walker, master gardener, professional organizer, chef, and housekeeper to name a few. Add in friendships that need energy, relationships that need time, those hobbies you swore you’d keep alive, and self-care you promised yourself you’d do…aaaaand the whole multi-passionate, multi-talented, multi-hyphenate thing can get overwhelming quick.
After a glorious five-month maternity leave, I’ve officially been a working mom for a year. I love my job and I love my girl, and while trying to fit both in a 24 day is challenging and exhausting, it’s what’s right for me in the season I’m in. Plus there’s something about pursuing my calling outside of the home and knowing Sloan’s watching me do it.
RELATED POST: 9 Ways to Practice Self-Love as a New Mom on Maternity Leave
We’ve all chased that ultimate goal of a *perfect* balance and ~seamless~ blend between work and home, but in full disclosure, I’ve gotta tell ya— it’s hard for me to do. I’ve found myself coming home drained, dying for a break, wishing I could just lock myself in a quiet room, and feeling guilty for all of the above. Being with my daughter is the best part of my day, but I’m often just too depleted to enjoy it.
Maybe you can relate? Maybe you’re also trying to work to live but find those words flipping themselves around more than you care to admit.
I recently took an online course called Boundaries, Self-Care, and Meditation for the Pelvic Rehab Therapist, Part 1 (part 2 is on June 12). As a PT I’m required to take continuing education to keep my skillset relevant and knowledge fresh, but the pending burnout I shared with you above led me to [this] course instead. To put it simply, it was [insert explosion sound here] mind-blowing; and call me dramatic, but I consider my practice, my patients, and myself as a person and professional forever changed because of it.
While I could write at least ten posts on all the things I learned in this class, the concept that’s been most life-altering for me was how I spend my lunchtime. Yep!…just a few tweaks to those 30 minutes mid-day and not only are my afternoons more pleasant and productive, but I’m going home refreshed, renewed, and ready to spend my time and energy on alllllllllll the other people and things that mean the most to me.
RELATED POST: Your Day Starts at Bedtime: 25 Easy Habits for a Better Night’s Sleep
What you’ll find next is how I structure my lunchtime for life-giving success— a strategy that serves me most. We all have different work environments, different physical and mental needs, and different priorities. As long as your cup feels full(er) at the end of your break, I can confirm you’re doin’ it right.
SHUT YOUR DOOR
I fully realize that not everyone has an office door they can shut during lunchtime, but as long as you can get somewhere semi-quiet and remotely alone, that should do the trick (heck…I’ve been known to go out to my car in a pinch). Creating a calm and centered environment has proven paramount to taking a true “break” from the day and will make all of my recommendations to follow that much more enjoyable.
If you’re worried about appearing “selfish” or “standoffish”…I was too. But after a week’s worth of lunches behind a closed door, I realize the positives of this practice far outweigh the negatives I was creating in my head. I’m still a team player. My coworkers still know where I am if they need me. But I’m a better colleague the other eight hours of the day when I take these 30 minutes to myself, and to my knowledge, there have been no complaints so far.
STOP TO EAT
To my fellow multi-tasking queens— if you only read one part of this post, let [this] be it as I believe this one change has made the biggest difference.
I used to spend my lunch catching up on paperwork, tending to emails, paying bills, online shopping, and then resort to scrolling social media if all of that was done. But I was eating during all of it and realized that not only was it taking me twice as long to complete tasks, but I wasn’t tasting, appreciating, or ultimately enjoying my food, all huge components of appetite, digestion, and ultimately nutrition and health.
My lunches aren’t anything fancy; in fact, 99% of the time they’re leftovers from earlier in the week (helloooooooo my trusty 3-day-old grilled chicken). But stopping to eat with intention and nothing other than a little music or podcast playing in the background has surprisingly, but positively, affected how much I consume, how my gut feels afterward, and the amount of energy I have for the rest of the day.
PS- What you eat can make a huge impact here too. I aim for whole, quality foods full of healthy fats and filling proteins to set me up for success. I’m someone who can eat the same thing again and again, so you’ll typically find my lunchbox full of that good ol’ grilled chicken, boiled eggs, fruit, cheese, and rice noodles if I’m feelin’ feisty.
LEARN
On top of that podcast I have playing while I eat, I’ve started spending ten to fifteen minutes learning during lunch. I literally set a timer, pull out a book, and read about something that fuels my brain.
In order to make these minutes a 10/10, here’s a few tips to uplevel the experience:
- Get comfortable. Find a place to prop your feet up or lean that car seat back (this is in part why I set a timer…juuuuuuuust in case I fall asleep). Have water nearby, a blanket tucked away if it’s cold, and don’t hesitate to indulge in all the ways even if for just a short period of time.
- Read about something unrelated to your occupation. For instance…I’m a pelvic rehab therapist but you won’t see me catching up on the latest research in anatomy and physiology. I typically grab a book on self-improvement, business and marketing, or homesteading, and my brain feels so much more recharged when it gets to focus on something that builds me up as a passionate person outside of my profession.
- Use a physical book. Seriously…no kindle, no phone apps, no audiobooks. Chances are you’re looking at a screen, listening to people talk, or a combo of the two all day long. Digging into an actual hard copy will access other parts of your brain that you may not be tapping into as regularly and result in faaaaaaaar more feel-good-ness.
When I became a mom I went from devouring a few books a month to being able to count my yearly reads on one hand. Reading on my lunch break has made me excited to learn again and reminded me of who I am outside of motherhood too (in turn making me a better mama). Even if reading isn’t your “thing”, at least give this one a try. Bonus if you utilize your local library because their books just smell better and we’re going for indulgent here…remember?
MOVE
Eat…ten minutes. Learn…ten minutes. If you’re like me and have ten more minutes to spare, then I encourage you to move your body with that time. While the options are endless, I try to avoid sweating too much in the middle of the work day, so walking, stretching, and even deep breathing exercises are more my speed. Whatever you decide to do, make sure you have the shoes, yoga mat, or whatever it is you need ready to go.
RELATED POST: Easy + Impactful Ways to Use Your Time Confetti to Improve Your Pelvic Floor Health
Not only does research show that movement improves your mood and elevates your energy, but there are also the physical benefits (duh!) and mental resilience that comes with knowing you’re taking care of yourself when you could be doing something else. Once fearful of wasting precious energy, I now consider my mid-day movement the boost I need to ensure I’m ready to go when I get home because let me tell ya…one year olds don’t quit.
One look at my Pinterest boards and you’ll see I’m a girl who has a lot she wants to accomplish (I see you dream house, list of must-reads, vacation itineraries, and yummy recipes just dyyyyyying to be made). But with a 24-hour day divided in thirds between work, sleep, and “other”, I have to use my time wisely to see success in a life where I’m more often than not choosing the option of (D) ALL OF THE ABOVE.
I don’t mean to be dramatic, but hacking my 30-minute lunch has ~literally~ changed my life and I’m a better physical therapist, caregiver, dog walker, master gardener, professional organizer, chef, and housekeeper (to name a few) because of it. There’s a saying that if you can’t go big, go home, but this is an instance where you can’t underestimate the power of a few minutes spent intentionally where it counts.
I’d love to hear in the comments what you do for work, if these strategies work for you, and ways you’ve made them your own. And don’t hesitate to share this one with a coworker who could use these strategies too! Nothing makes me happier than picturing us all spending half an hour in that 11-2 time frame-filling our cups for full-day success. I have a feeling you’ll be surprised at the impact this can have, and I can’t wait to watch you grow one lunchtime at a time.
Boundaries, Self-Care, and Meditation - Part 2 - Remote Course - June 12, 2022
This course focuses on personal and professional growth for the participant, with a deeper dive into meditation and self-care practices. Yoga is introduced as a means of mindful movement and energy balance. Participants will learn to identify unhealthy relational patterns in patients and others, and skills on how to use language and boundaries to create shifts that keep the clinician grounded and prevent excessive energic and emotional disruptions. There is a lecture on using essential oils for self-care and possibly patient care. Learning new strategies to preserve energy, wellness, and passion while practicing appropriate self-care and boundaries will lead to helpful relationships with complex patients. This course also includes a discussion of energetic relationships with others as well as the concept of a "Higher Power". The discussion will also include refining life purpose, mission, and joy potential, unique to the individual participant. The goal is that the participating clinician will walk away from this experience equipped with strategies to address both oneself and one's patients with a mind, body, and spirit approach.
Rachna Mehta PT, DPT, CIMT, OCS, PRPC, RYT 200 has a personal interest in various eastern holistic healing traditions, and she noticed that many of her chronic pain patients were using complementary health care approaches including acupuncture and yoga. Her course Acupressure for Optimal Pelvic Health brings a unique evidence-based approach and explores complementary medicine as a powerful tool for holistic management of the individual as a whole focusing on the physical, emotional, and energy body.
There is worldwide concern over the increasing rates of pharmacologically induced labor, opioid use, and operative birth. Women are seeking holistic non-pharmacologic options to avoid medical and surgical interventions in childbirth which has led to the popularity of Complementary and Alternative Medicine (CAM) therapies. Despite CAM existing outside of conventional heath systems, a substantial number of women have been found to use CAM to manage their health during pregnancy1.
Among CAM therapies, Acupuncture and Acupressure have been found to be helpful for pregnancy-related symptoms such as nausea, breech presentation, and labor induction with post-partum recovery considerations as well. Acupressure has roots in Acupuncture and is based on more than 3000 years of Traditional Chinese Medicine (TCM). TCM supports Meridian theory and meridians are believed to be energy channels that are connected to the function of the visceral organs. Acupoints located along these meridians transmit Qi or the bio-electric energy through a vast network of interstitial connective tissue connecting the peripheral nervous system to the central viscera.
A systematic review published by Smith et al2 looked at the use of Acupuncture or Acupressure for pain management during labor. They noted that the pain women experience during labor can be intense, with body tension, anxiety, and fear making it worse. The data included a total of 3960 women and found that Acupressure may reduce pain intensity in women experiencing labor pain.
Another RCT published by Levett et al included 176 nulliparous women with low-risk pregnancies, attending hospital-based antenatal clinics. They incorporated six evidence-based complementary medicine techniques: Acupressure, visualization and relaxation, breathing, massage, yoga techniques, and facilitated partner support. Randomization occurred at 24–36 weeks’ gestation, and participants attended a 2-day antenatal education program plus standard care, or standard care alone.
The study found a significant difference between the two groups with the study group having decreased epidural use (23.9%) compared to the standard care group (68.7%). The study group participants also reported a reduced rate of cesarean section and length of the second stage among other measures.
An article published by Debra Betts3 discusses several key considerations for promoting physiological Labor with Acupuncture. Multiple studies have cited the effectiveness of Acupressure by stimulating these powerful Acupoints as well. The author states that the suggestion of Acupoints cited below are based on both her clinical practice and midwifery feedback and are by no means an exhaustive list. The practitioner is encouraged to explore Traditional Chinese Medicine to promote efficient physiological labor in women.
Key considerations for promoting natural physiological labor include:
Is the baby in an optimal anterior position? The author states “Women can become involved in their own treatment by learning proactive positioning. This involves a woman keeping her knees lower than her hips when sitting, in order to assist gravity in moving her baby into the best possible position. Bucket‑type seats such as car seats and comfy sofas, therefore, need to be abandoned in favor of birthing balls, sitting astride chairs (with the arms resting on the back).” Key acupuncture points that can be stimulated include Bladder 60 ( BL 60), Spleen 6 (Sp 6), and Bladder 67 (BL 67). Bladder 60 (BL 60) is considered an empirical induction point. Midwifery feedback suggests that this is a useful point for promoting an optimal position of the baby for birth. Bladder 67 (BL 67) is considered an extremely important point if the baby is not in an anterior position.
Is the woman emotionally prepared for labor? While most women have some level of underlying anxiety or fear about the approaching birth, it is essential to address any significant emotional disharmony. The hormone oxytocin is released several weeks prior to labor, initially stimulating uterine contractions at night, with increasing production then aiding the transition into labor. Stress hormones such as adrenaline and noradrenaline have a direct inhibiting effect on natural oxytocin release, and therefore play a very significant role in inhibiting contractions2. Key acupuncture points that can be stimulated include Kidney 1 (KD 1), Liver 3 (Liv 3), and Pericardium 6 (P6) among others. Kidney 1 (K1) is useful for women who are experiencing fear of induction or childbirth itself. Liver 3 (Lv 3) is helps in improving Liver chi. Pericardium 6 (P6) is helpful for nausea, regulating the heart and calming.
Is the woman physically prepared for labor? Women may be physically exhausted or have pre-existing physical conditions that, once addressed, will help to promote physiological labor2. Key acupuncture points that can be stimulated include Bladder 43 (BL 43) and Stomach 36 (St 36). Bladder 43 ( BL 43) is A point that tonifies and nourishes the Lung, Heart, Kidneys, Spleen, and Stomach. Stomach 36 (ST 36) is a useful point to reinforce if the woman is exhausted, due to its qi-tonifying and blood-nourishing properties.
Stimulating contractions: Debra Betts also notes that key points of the Bladder meridian that are located on the sacrum are crucial in initiating contractions. While Traditional Chinese Medicine (TCM) does consider some Acupuncture points like Large Intestine 4 (LI 4), Gall Bladder 21 (GB 21), and Spleen 6 (Sp 6) should not be stimulated in pregnant women, the opposite is true when we want to initiate labor and these points can be additionally used to assist in stimulating contractions.
Acupressure can also be used in the post-partum period for overall generalized well-being, promoting a sense of bonding with the baby, calm, and relaxation.
Acupressure can be used to stimulate key energy points also known as Acupoints in various meridians and as hands-on musculoskeletal specialists, we can use and teach this modality to our patients. Acupressure requires no equipment, is easy for clinicians to teach and for patients to self-administer when taught correctly, and is an empowering self-care tool to promote optimal health outcomes.
The course Acupressure for Optimal Pelvic Health focuses on powerful Acupressure points in key Meridians including the Kidney, Bladder, Spleen, and Stomach meridians. It also explores Yin Yoga as an integrative intervention with Acupressure. Yin Yoga, a derivative of Hath Yoga is a wonderful complimentary practice to Acupressure. Yin Yoga is a slow and calm meditative practice that uses seated and supine poses that are held for three to five minutes with deep breathing. It stimulates the energy flow through the meridian channels by creating tension along specific meridian lines.
This course is curated and taught by Rachna Mehta. To learn how to integrate Acupressure into your clinical practice, join the next scheduled remote course on June 25- 26, 2022.
References
- Steel A, Adams J, Sibbritt D, Broom A. The Outcomes of Complementary and Alternative Medicine Use among Pregnant and Birthing Women: Current Trends and Future Directions. Women’s Health. May 2015:309-323. doi:10.2217/WHE.14.84.
- Smith CA, Collins CT, Levett KM, et al. Acupuncture or acupressure for pain management during labour. Cochrane Database Syst Rev. 2020;2(2): CD009232.
- Betts, Debra. Inducing Labour with Acupuncture–Crucial Considerations. Journal of Chinese Medicine. 2009;90: 20-25.
- Atkins KL, Fogarty S, Feigel ML. Acupressure and Acupuncture Use in the Peripartum Period. Clin Obstet Gynecol. 2021;64(3):558-571. doi:10.1097/GRF.0000000000000636.
- Levett, Kate M., Smith, C.A., Bensoussan, A. & Dahlen, H.G. Complementary therapies for labour and birth study: a randomized controlled trial of antenatal integrative medicine for pain management in labour. BMJ Open, 2016 Jul 12;6(7):e010691. DOI: 10.1136/bmjopen-2015-010691.
- Schlaeger JM, Gabzdyl EM, Bussell JL, et al. Acupuncture and Acupressure in Labor. J Midwifery Women's Health. 2017;62(1):12-28. doi:10.1111/jmwh.12545.
Acupressure for Optimal Pelvic Health
Instructor: Rachna Mehta PT, DPT, CIMT, OCS, PRPC, RYT 200
Price: $450
Experience Level: Beginner
Contact Hours: 12.5
Course Dates: June 25-26, 2022 and October 15-16, 2022
Course Description:
This continuing education course is a two-day seminar that offers participants an evidence-based perspective on the application of Acupressure for evaluating and treating a host of pelvic health conditions including bowel, bladder, and pelvic pain issues. The course explores a brief history of Acupressure, its roots in Acupuncture and Traditional Chinese Medicine (TCM), and presents current evidence that supports the use of complementary and alternative medicine as an adjunct to western medicine. TCM concepts of Meridian theory and energy channels are presented with scientific evidence of Acupoints transmitting energy through interstitial connective tissue with potentially powerful integrative applications through multiple systems.
Lectures will present evidence on the use of potent Acupressure points and combinations of points for treating a variety of pelvic health conditions including chronic pelvic pain, dysmenorrhea, constipation, digestive disturbances, and urinary dysfunctions to name a few. Key acupoints for decreasing anxiety, and stress and bringing the body back to a state of physiological balance are integrated throughout the course.
Participants will be instructed through live lectures and demonstrations on the anatomic location and mapping of acupressure points along five major meridians including the spleen, stomach, kidney, urinary bladder, and gall bladder meridians. Key associated points in the pericardium, large intestine, small intestine, lung and liver meridians as well as the governing and conception vessels will also be introduced. The course offers a brief introduction to Yin yoga and explores Yin poses within each meridian to channel energy through neurodynamic pathways to promote healing across multiple systems. Participants will learn how to create home programs and exercise sequences and will be able to integrate acupressure and Yin yoga into their orthopedic and pelvic health interventions.
Special Considerations and Lab materials
The labs for this course will involve external whole-body palpation and mapping of acupressure points. Please wear fitted t-shirt and leggings or yoga pants for acupressure point mapping. Participants should buy a pack of 1-inch diameter white circle stickers to be used in Labs for mapping acupressure points.
Participants are encouraged to use a Yoga mat if available and any other props they may have at home including yoga blocks, small blankets, towels and pillows to be used in the guided Yin Yoga Lab portion of the course.
Recommended resources: It is recommended that participants purchase an Acupressure Point Chart for ease of following the course work and labs in this course. Since the accuracy of points and content may vary on different charts, it is recommended to buy a copy at https://acupressure.com/products/acupressure-charts/
Target Audience:
This continuing education seminar is targeted to rehabilitation professionals who use manual therapy as a treatment modality. Knowledge of acupressure points with specific anatomical landmarks will enable clinicians to add to their toolbox skills for treating a variety of pelvic health conditions related to the bowel, and bladder and treatment of pelvic pain.
Prerequisites:
It is recommended that the participants have a working knowledge of the functional anatomy of pelvic floor muscles as well as various associated pelvic health conditions. Pelvic Floor 1 through Herman & Wallace is strongly recommended.
Mora Pluchino, PT, DPT, PRPC sat down this week with Holly Tanner in an interview to discuss her new courses, Ethical Concerns for Pelvic Health Professionals and Ethical Considerations from a Legal Lens. She is a pelvic therapist who works in an outpatient clinic, has her own side company (Practically Perfect PT), has written 2 books available on Amazon, and is a senior TA and faculty member with Herman & Wallace. Mora joins the Herman & Wallace faculty with her new course series in ethics: Ethical Concerns for Pelvic Health Professionals and Ethical Considerations from a Legal Lens.
What are your core values as a pelvic health practitioner? Depending on your practitioner license these may include (1):
- Accountability - Active acceptance of the responsibility for the diverse roles, obligations, and actions of the physical therapist and physical therapist assistant including self‐regulation and other behaviors that positively influence patient and client outcomes, the profession, and the health needs of society.
- Altruism - The primary regard for or devotion to the interest of patients and clients, thus assuming the responsibility of placing the needs of patients and clients ahead of the physical therapist’s or physical therapist assistant’s self‐interest.
- Collaboration - Working together with patients and clients, families, communities, and professionals in health and other fields to achieve shared goals. Collaboration within the physical therapist‐physical therapist assistant team is working together, within each partner’s respective role, to achieve optimal physical therapist services and outcomes for patients and clients.
- Compassion and Caring - Compassion is the desire to identify with or sense something of another’s experience; a precursor of caring. Caring is the concern, empathy, and consideration for the needs and values of others.
- Duty - The commitment to meeting one’s obligations to provide effective physical therapy services to patients and clients, to serve the profession, and to positively influence the health of society.
- Excellence - The provision of physical therapist services occurs when the physical therapist and physical therapist assistant consistently use current knowledge and skills while understanding personal limits, integrating the patient or client's perspective, embracing advancement, and challenging mediocrity.
- Integrity - Steadfast adherence to high ethical principles or standards, being truthful, ensuring fairness, following through on commitments, and verbalizing to others the rationale for actions.
- Social Responsibility - The promotion of mutual trust between the profession and the larger public that necessitates responding to societal needs for health and wellness.
Annual CEU requirements for license renewals don’t just look at hands-on skills. Many states also require a number of ethics credits including California, Georgia, Illinois, New Jersey, and Utah (2). In her interview, Mora Pluchino explains that one day she and her colleague were at lunch talking about course options for their ethics CEU requirement. They had taken the same course over and over at Stockton University and wanted to do something different this time. This led to Mora reaching out to Herman & Wallace and Holly Tanner who helped her start writing the course. Mora’s new courses focus on this ethics requirement, provide 6 contact hours, and registration is $175.00 for each:
- Ethical Concerns for Pelvic Health Professionals – June 18th
- Ethical Considerations from a Legal Lens – December 10th
What should you expect from an ethics course? Mora breaks down the Ethical Concerns for Pelvic Health Professionals course and shares that there is about an hour of pre-course video lectures to watch, then the live course involves “a little bit of lecture in relation to pelvic health and ethics, and then there will be some case studies and group work. After this, an ethical expert will come in and do live question/answers with us.”
These courses are to really make practitioners comfortable with these ethical and moral issues. Mora explains, “I really want practitioners who take this course to understand and know where to find information about those issues that come up with their boss, their organization, their patients, or themselves. A lot of times, ethical situations just make us just know instinctively that something doesn’t feel right.” Holly follows up with “Sometimes these situations can make us feel embarrassed, and maybe we contributed or didn’t contribute in the right way to a scenario. We don’t always bring them up to other people out of this embarrassment, or we just don’t know which pathway to take.”
A lot of common questions have an ethical component such as “How do I bill for this,” “How do I tell my boss I can’t do this,” or even “Can I reuse a biofeedback sensor?” Mora shares, “Sometimes, as a practitioner you can feel pressured to do (or not do) something, and you don’t know how to say no. With these courses, you will be able to give clear reasons such as it’s in my guidelines, in my practice act, and core values as being a PT or OT.” She further expands on this, “We have all of these people working for us in the APTA and AOTA that are creating all of these ethical guidelines and all of this information to give us the support.”
The ethics topics are broken down into two courses, with the first course Ethical Concerns for Pelvic Health Professionals focused specifically on people who treat pelvises scheduled for June 18, 2022. The second course, Ethical Considerations from a Legal Lens, is scheduled for December 10, 2022, and deals with the legalities and rights of health care providers. Some questions that are touched on during lectures include abandonment of care and discrimination. Mora also shares that a lot of the ethics courses she has taken are “from the perspective of therapists that are abusing their patients, but when you work in pelvic health world you realize it can go the other way too, or it can be a back and forth kind of thing.”
To learn more, and fulfill that ethics CEU requirement, join H&W and Mora Pluchino this summer in Ethical Concerns for Pelvic Health Professionals on June 18th or this winter in Ethical Considerations from a Legal Lens scheduled for December 10th.
Resources:
- APTA. Core Values for the Physical Therapist and Physical Therapist. HOD P06‐19‐48‐55. 9/20/2019. https://www.apta.org/siteassets/pdfs/policies/core-values-endorsement.pdf. Accessed 5/30/2022.
- Fraticelli, T. PT Progress. Physical Therapy Continuing Education: PT CEU Requirements by State. October 8, 2018. https://www.ptprogress.com/physical-therapy-continuing-education-requirements-by-state/. Accessed 5/30/2022.
Additional Resources:
o Counselors / Psychologists: https://www.apa.org/about/apa-jobs/values