In a 2018 article by Holly Tanner, she explains how managing a medical crisis such as a cancer diagnosis can be overwhelming for an individual. ‘Faced with choices about medical options, dealing with disruptions in work, home, and family life often leaves little energy left to consider sexual health and intimacy. Maintaining closeness, however, is often a goal within a partnership and can aid in sustaining a relationship through such a crisis.” Research shows that cancer treatment is disruptive to sexual health. Intimacy is a larger concept that may be fostered even when sexual activity is impaired or interrupted.
Prostate cancer treatment can change relational roles, finances, work-life, independence, and other factors including hormone levels. (1) Exhaustion (on the part of the patient and the caregiver), role changes, changes in libido, and performance anxiety can create further challenges. (1, 3, 4) Recovery of intimacy is possible, and reframing of sexual health may need to take place. Most importantly, these issues need to be talked about, as a renegotiation of intimacy may need to take place after a diagnosis or treatment of prostate cancer. (2)
If a patient brings up sexual health, or the practitioner encourages the conversation, many research-based suggestions can be provided to encourage recovery of intimacy including:
• Redefining sex to include other sexual practices beyond penetration, such as massage or touching, cuddling, talking, use of vibrators, medication, aids such as pumps (5)
• Participation in couples therapy to understand their partner’s needs, address loss, be educated about sexual function (7)
• Participation in “sensate focus” activities (developed by Masters & Johnson in the 1970s as “touch opportunities”) with appropriate guidance (6)
Holly continues to share that “Within the context of this information, there is an opportunity to refer the patient to a provider who specializes in sexual health and function. While some rehabilitation professionals are taking additional training to be able to provide a level of sexual health education and counseling, most pelvic health providers do not have the breadth and depth of training required to provide counseling techniques related to sexual health - we can, however, get the conversation started, which in the end may be most important.”
Courses of Interest:
- A colorectal or male pelvic cancer diagnosis has multiple systems that are affected by cancer treatment. The rehabilitation professional that works with the pelvic oncology patient needs to competently navigate treatment techniques for all of these systems, as well as be confident in treating a patient in a personal area. This two-day course will address specific cancer types including prostate cancer, penile cancer, and testicular cancer. Additional cancer types covered include colorectal cancer and anal cancer.
Trauma Awareness for the Pelvic Therapist - Remote Course - Apr 9-10, 2022
- Bring their increased awareness of trauma to the successful, holistic treatment of patients with pelvic pain, sexual dysfunction, bowel dysfunction, and bladder dysfunction.
Sexual Medicine in Pelvic Rehab - Remote Course - Apr 9-10, 2022
- This course provides a thorough introduction to pelvic floor sexual function, dysfunction and treatment interventions for males and females of all sexual orientations, as well as an evidence-based perspective on the value of physical therapy interventions for patients with chronic pelvic pain related to sexual conditions, disorders, and multiple approaches for the treatment of sexual dysfunction including understanding medical diagnosis and management.
Male Pelvic Floor Function, Dysfunction, and Treatment - Satellite Lab Course - April 23-24 2022
- Discuss sexual anatomy and physiology, prostate issues, and look at the research describing models of intimacy and what worked for couples who did learn to renegotiate intimacy after prostate cancer. Participants will be able to describe the relationships between pelvic muscle function and men’s sexual health, including the evidence that demonstrates pelvic muscle rehabilitation's positive impact on erectile function.
1. Beck, A. M., Robinson, J. W., & Carlson, L. E. (2009, April). Sexual intimacy in heterosexual couples after prostate cancer treatment: What we know and what we still need to learn. In Urologic oncology: seminars and original investigations (Vol. 27, No. 2, pp. 137-143). Elsevier.
2. Gilbert, E., Ussher, J. M., & Perz, J. (2010). Renegotiating sexuality and intimacy in the context of cancer: the experiences of carers. Archives of Sexual Behavior, 39(4), 998-1009.
3. Hawkins, Y., Ussher, J., Gilbert, E., Perz, J., Sandoval, M., & Sundquist, K. (2009). Changes in sexuality and intimacy after the diagnosis and treatment of cancer: the experience of partners in a sexual relationship with a person with cancer. Cancer Nursing, 32(4), 271-280.
4. Higano, C. S. (2012). Sexuality and intimacy after definitive treatment and subsequent androgen deprivation therapy for prostate cancer. Journal of Clinical Oncology, 30(30), 3720-3725.
5. Ussher, J. M., Perz, J., Gilbert, E., Wong, W. T., & Hobbs, K. (2013). Renegotiating sex and intimacy after cancer: resisting the coital imperative. Cancer Nursing, 36(6), 454-462.
6. Weiner, L., Avery-Clark, C. (2017). Sensate Focus in Sex Therapy: The Illustrated Manual. Routledge, New York.
7. Wittmann, D., Carolan, M., Given, B., Skolarus, T. A., An, L., Palapattu, G., & Montie, J. E. (2014). Exploring the role of the partner in couples’ sexual recovery after surgery for prostate cancer. Supportive Care in Cancer, 22(9), 2509-2515.
Faculty member Christine Stewart, PT, CMPT began her career specializing in orthopedics and manual therapy and became interested in women’s health after the birth of her second child. Christine joined Olathe Health in 2010 to further focus on women’s health and obtain her CMPT from the North American Institute of Manual Therapy. She also went through Diane Lee's integrated systems model in 2018. Her course, Menopause Transitions and Pelvic Rehab is designed for the clinician that wants to understand the multitude of changes that are experienced in the menopause transition and how they affect the aging process.
Menopause. The M-word, the second puberty, is the final frontier of a hormonal roller coaster when there are twelve consecutive months with no menstruation. A time of celebration, right? No more cramps, hygiene products, menstrual cups, or moodiness – FREEDOM! Not so fast my fellow clinician!
The body goes through some serious, hormonal loop-the-loops leading up to the cessation of ovulation. Perimenopause is the stretch leading up to the final cycle and this stretch can feel like yoga on steroids. It can last TEN years, not including symptoms experienced after the transition takes place. Changes in cycle length, flow, anovulation, and yes, even ovulating twice are all stages of perimenopause. (Hale et al., 2009). These changes translate into symptoms: sleeplessness, brain fog, anxiety, palpitations, fatigue, painful intercourse, and joint stiffness are just a few things that can be experienced during this time (Lewis, 2021).
This transition can begin for patients during their mid-thirties, more commonly it begins during their forties, but eventually, all people that ovulate will experience it. For some, perimenopause can be much more challenging than after menopause. The perimenopause hormone guessing game begins. Some months, progesterone makes an appearance. The next month, mostly estrogen, and some months - neither are around very much at all. If there is an abrupt change in ovulation, such as with a complete hysterectomy, the symptoms will most likely be intensified due to the abrupt loss of hormones. (Gunter, 2020). Dealing with the changes of menopause can be challenging in a variety of ways (like a two-year-old wailing for a candy bar in the checkout line), but many things can help ease this transition.
With fluctuating hormones also comes changes to many systems in the body. Estrogen receptors are everywhere, and when hormone levels are changing, so does the body’s internal workings. Glucose metabolism, bone physiology, brain, and urogenital function are just some of the systems affected (Shifren et al., 2014). Perimenopause is not just a time of altered periods. It is also a critical time in a person’s health where an increased incidence of heart disease, diabetes, and bone loss can begin (Lewis 2021).
Preparing for menopause should be on our radar for patients in their twenties, thirties, and early forties before the process starts. Establishing healthy habits earlier instead of later can help for a more successful transition, however, it is never too late! Knowing the signs and symptoms of this phase can help us guide patients and ourselves to a better understanding of what is happening with the body in this adaptation. We can make recommendations on lifestyle, exercise, and meditation, as well as refer them to other knowledgeable providers when needed.
I have had countless patients sent to me for urinary frequency, incontinence, or painful intercourse who are in this transition, but no one has talked to them about what is happening to their bodies. You may be thinking to yourself, these patients have doctors. Why aren’t they getting the information from their physician? After all, these providers have had years of training. The reality is sometimes doctors do not receive the necessary education to treat menopausal patients.
In a survey of postgraduate trainees in internal medicine, family medicine, and obstetrics/gynecology, 90% felt unprepared to manage women experiencing menopause (Reid, 2021). Insert jaw drop here. As pelvic health providers, we can help to fill this knowledge gap and be a conduit to explaining the process. We can empower patients with education, treatments, and recommendations to flourish in this critical phase of life.
The menopause transition can be a time of great uncertainty. Not only are patients’ lives transforming as their children grow and their parents age, but their bodies are changing as well. We can ease their burden in this period of adaptation. By calming their fears through education, we can assure them that indeed, they are not losing their minds.
Knowledge is power, and I am all in when it comes to empowering patients. They can learn that menopause is a phase and does not define who they are as a person. It is possible to survive and come out on the other side still thriving, while learning how to cope during the process. There is hope!
Menopause Transitions and Pelvic Rehab is an excellent opportunity to understand the physiological consequences to the body as hormones decline, in order to assist our patients in lifestyle habits for successful aging. Lecture topics include cardiovascular changes, metabolic syndrome, bone loss and sarcopenia, neurological changes (headache, brain fog, sleeplessness), Alzheimer’s risk, urogenital changes, as well as symptoms and treatment options. These include hormone replacement, non-hormonal options, dietary choices, and exercise considerations.
Menopause Transitions and Pelvic Rehab course dates include April 9-10th and August 27-28th.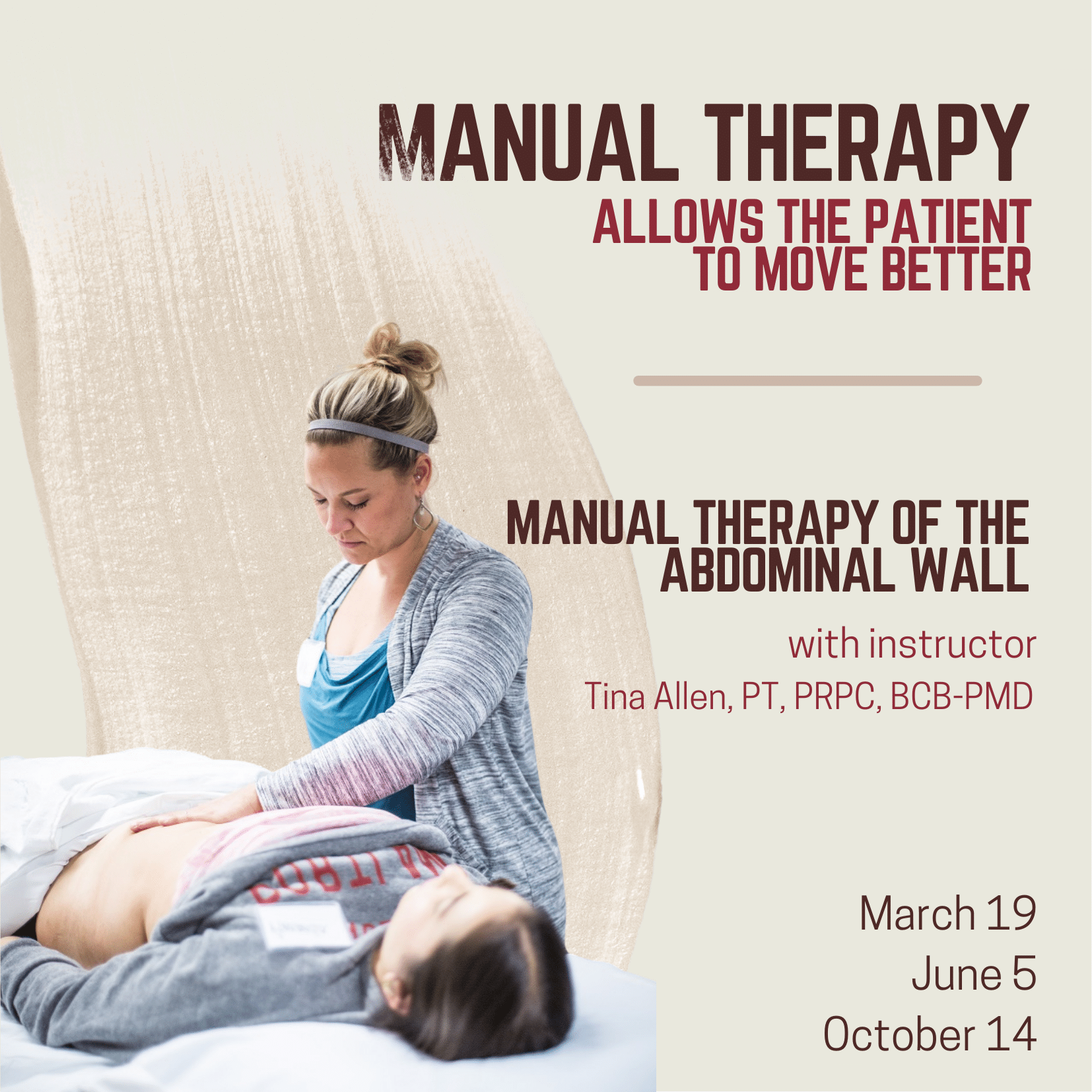
Manual Therapy for the Abdominal Wall allows practitioners to review how everything interplays within the myofascial system and apply specific techniques. These techniques include how to assess the tissue for mobility, how to treat tissues that are restricted in the abdominal wall, and how to treat scar tissue. How do we help somebody who can’t lay flat because their abdominal wall has become restricted for so long because of possible pain? Possibly due to surgery. Possibly due to fear. How do we help those patients get back to function?
Over the past 10 plus years of teaching the pelvic series with Herman & Wallace, Tina Allen noticed that for some of the participants there was a gap in confidence in palpation skills and treatment techniques applied to the pelvic floor region. For most, it’s confidence in where they are and what they are feeling on the patient. Manual Therapy for the Abdominal Wall came out of wanting to fill that gap. This course is really about taking some of those skills and then applying them to the abdominal wall.
Abdominal pain can arise from many origins including abdominal scars, endometriosis, IC/PBS, and abdominal wall restrictions that impact pelvic girdle dysfunction. An older study, back in 2007 by Geoff Harding focused on back, chest, and abdominal pain and whether it was spinal referred pain and employed manual therapy as part of his treatments for his case studies. Harding found that “More specific treatment of the origin of the pain may then include manual therapy, including mobilization (gentle rhythmic movement), … applied to the affected segment can be very effective in reducing movement restriction – and pain. These simple treatments were used in all three case studies to good effect.” (1)
This research was supported by Rice et al. in 2013 when their research on non-surgical treatment of adhesion-related small bowel obstructions showed that “those patients who underwent the manual therapy demonstrated increased range of motion … and an early return to normal activities of daily living simply enhanced the benefits.” (2) Manual therapy has no recovery time and allows patients to recover and participate in daily activities while promoting the return of normal tissue function, range of motion, and increased blood flow.
Tina Allen explains that manual therapy is about “asking for permission to touch and using our hands to help the patient integrate into their system again. The patient may not realize that they’ve been holding, that there is tension or rigidity in the tissues.” Tina continues to share that “for me, manual therapy fits in to help folks realize, or feel, what’s happening in their body again. And then allowing them to make that change. I use manual therapy to allow a patient to move better. To become more aware in their body.” The full interview with Tina can be viewed below or on the Herman & Wallace YouTube Channel.
Manual Therapy for the Abdominal Wall is a beginner-level class and is filled with practitioners just beginning their pelvic floor journey through experienced clinicians taking the course to learn something new. The techniques instructed by Tina Allen are immediately applicable in the clinic. Course dates for 2022 include:
References:
- Harding G, Yelland M (2007). Back, chest, and abdominal pain. Australian Family Physician, 36(6), 422-429.
- Rice, A. D., King, R., Reed, E. D., Patterson, K., Wurn, B. F., & Wurn, L. J. (2013). Manual Physical Therapy for Non-Surgical Treatment of Adhesion-Related Small Bowel Obstructions: Two Case Reports. Journal of clinical medicine, 2(1), 1–12.
Dustienne Miller, CYT, PT, MS, WCS instructed the H&W remote course Yoga for Pelvic Pain. Dustienne passionately believes in the integration of physical therapy and yoga in a holistic model of care, helping individuals navigate through pelvic pain and incontinence to live a healthy and pain-free life. You can find Dustienne Miller on Instagram at @yourpaceyoga
Research demonstrates multiple benefits of a yoga practice that extend beyond the musculoskeletal system. These benefits include improved mood and depression, changes in pain perception, improved mindfulness and associated improved pain tolerance, and the ability to observe situations with emotional detachment.
Do the brains of yoga practitioners vs non-practitioners look different?
A study by Villemure et al looked at the role the insular cortex plays in mediating pain in the brains of yoga practitioners. They included various styles of yoga to capture the essence of yoga across multiple styles - Vinyasa, Ashtanga, Kripalu, Sivananda, and Iyengar.
Rewind back to neuroanatomy class - remember the insular cortex? The insular cortex is responsible for sensory processing, decision-making, and motor control by communicating between the cortical and subcortical aspects of the brain. The outside inputs include auditory, somatosensory, olfactory, gustatory, and visual. The internal inputs are interoceptive (Gogolla).
Villemure et al found several interesting objective differences. The practitioners had increased grey matter volume in several areas of the brain. This increase in grey matter specifically in the insula correlated with increased pain tolerance. The length of time practiced correlated with increased grey matter volume of the left insular cortex. Additionally, white matter in the left intrainsular region demonstrated more connectivity in the yoga group.
Other differences were seen in strategies utilized to manage pain. Most folks in the yoga group expected their practice would decrease reactivity to pain, which it did. The yoga group used parasympathetic nervous system accessing strategies and interoceptive awareness. These strategies were breathwork, noticing and being with the sensation, encouraging the mind and body to relax, and acceptance of the pain. The control group strategies were distraction techniques and ignoring the pain.
The authors determine that the insula-related interoceptive awareness strategies of the yoga practitioners being used during the experiment correlated with the greater intra-insular connectivity. Therefore, the authors conclude that the insular cortex can act as a pain mediator for yoga practitioners.
The more strategies our patients have for pain management, the better! Yoga is one of several non-invasive modalities our patients can add to their healing toolbox.
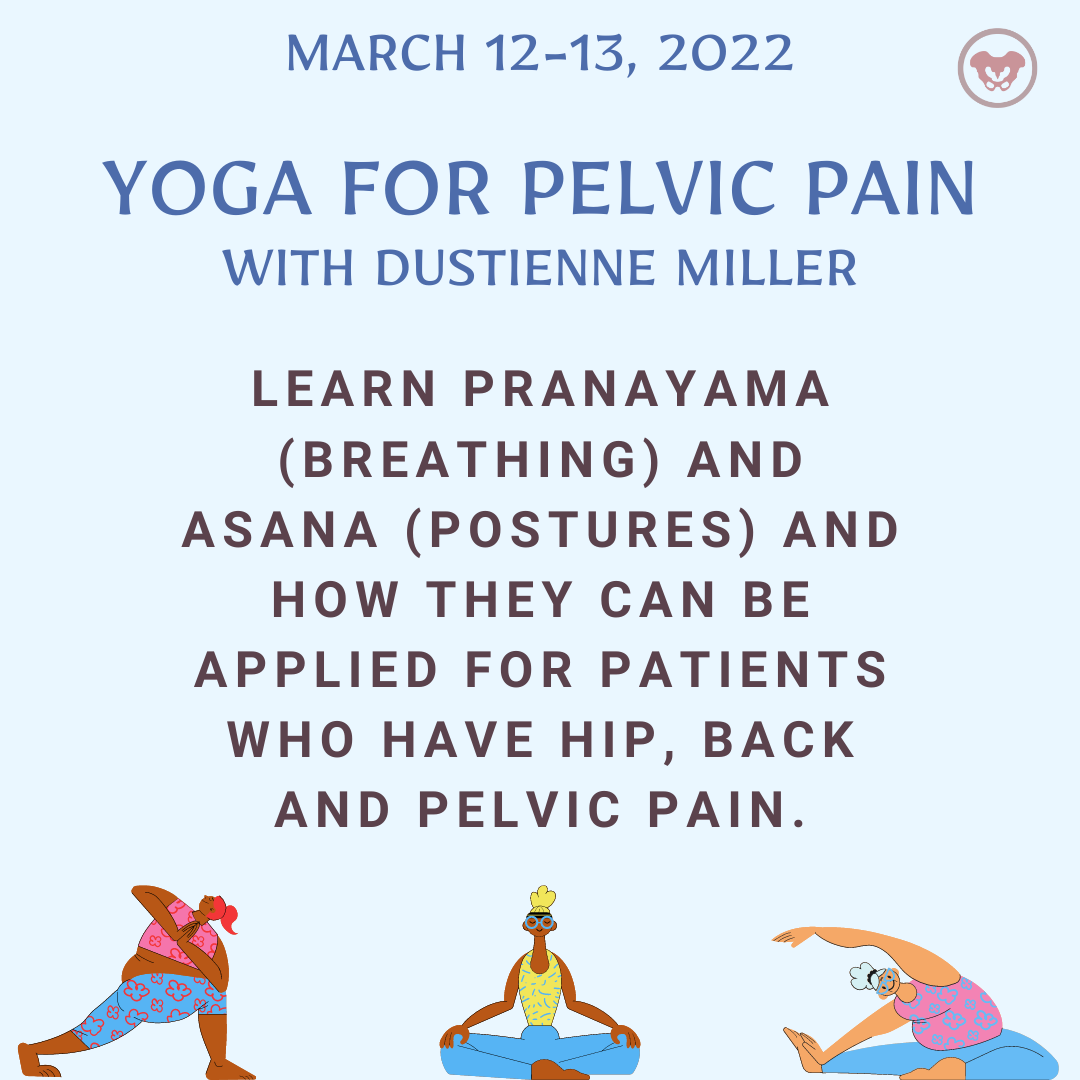
Yoga for Pelvic Pain was developed by Dustienne Miller to offer participants an evidence-based perspective on the value of yoga for patients with chronic pelvic pain. This course focuses on two of the eight limbs of Patanjali’s eightfold path: pranayama (breathing) and asana (postures) and how they can be applied for patients who have hip, back, and pelvic pain.
A variety of pelvic conditions are discussed including interstitial cystitis/painful bladder syndrome, vulvar pain, coccydynia, hip pain, and pudendal neuralgia. Other lectures discuss the role of yoga within the medical model, contraindicated postures, and how to incorporate yoga home programs as therapeutic exercise and neuromuscular re-education both between visits and after discharge.
References:
Gogolla N. The insular cortex. Current Biology. 2017; 27(12): R580-R586.
Villemure C, Ceko M, Cotton VA, Bushnell MC. Insular cortex mediates increased pain tolerance in yoga practitioners. Cereb Cortex. 2014 Oct;24(10):2732-40. doi: 10.1093/cercor/bht124. Epub 2013 May 21. PMID: 23696275; PMCID: PMC4153807.
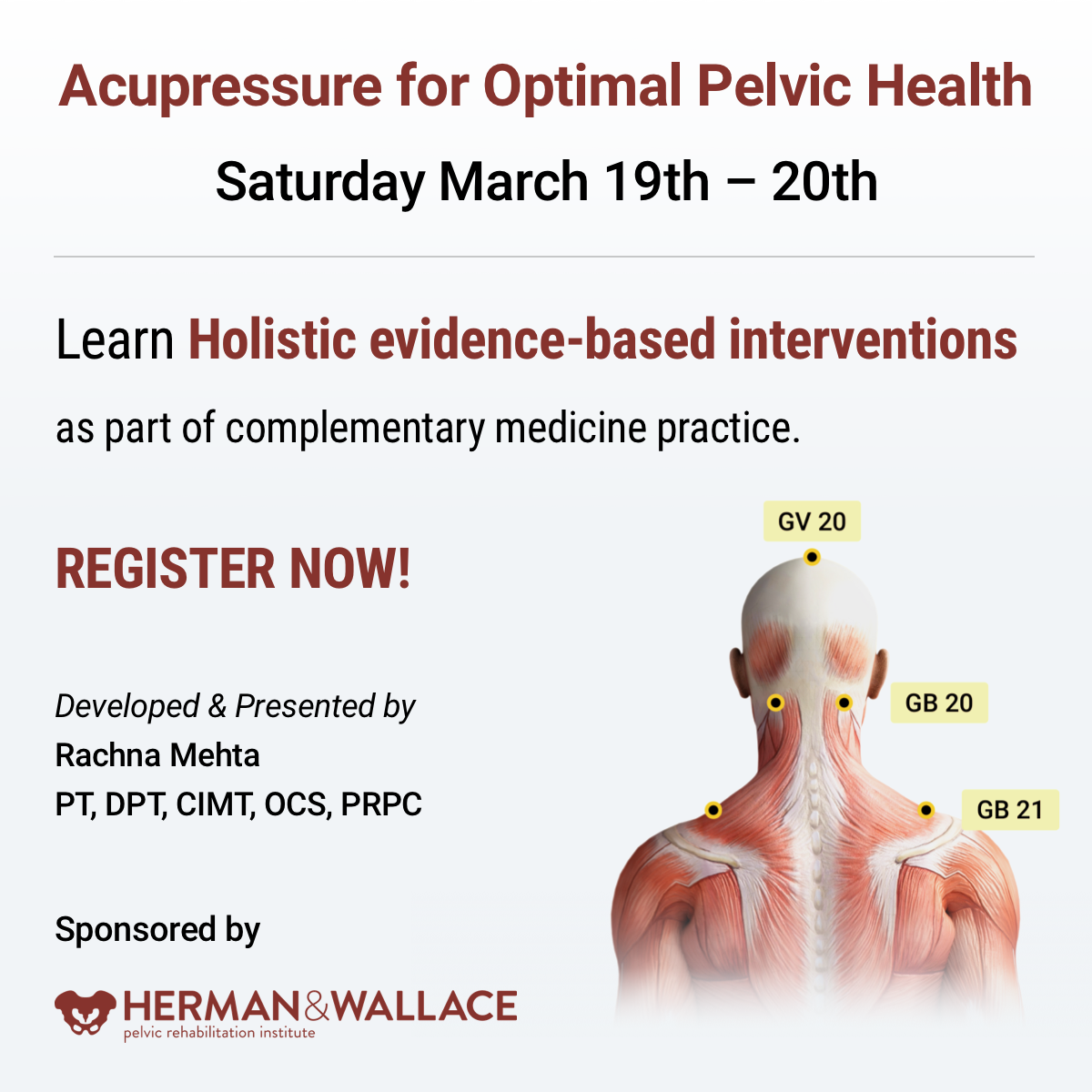
Rachna Mehta, PT, DPT, CIMT, OCS, PRPC is the author and instructor of the Acupressure for Optimal Pelvic Health course. Rachna brings a wealth of experience to her physical therapy practice and has a personal interest in various eastern holistic healing traditions. Her course Acupressure for Optimal Pelvic Health brings a unique evidence-based approach and explores complementary medicine as a powerful tool for holistic management of the individual as a whole focusing on the physical, emotional, and energy body.
What is Acupressure
According to the National Center for Complementary and Integrative Health (NCCIH), a branch of the National Institute of Health (NIH), a recent study by Feldman et al1 in the Journal of Pain showed that patients with newly diagnosed chronic musculoskeletal pain are prescribed opioids more often than physical therapy, counseling, and other nonpharmacologic approaches. A study2 by Elizabeth Monson and colleagues noted that the use of effective nonpharmacologic options is now mandated by Joint Commission Guidelines3 per updated pain management recommendations. The study also noted that there has been a growing clinical interest in Acupressure as a therapeutic modality for symptom management in Western health care.
The scientific literature presents robust evidence supporting Acupressure as an effective non-pharmacological therapy for the management of a host of conditions such as anxiety, insomnia, chronic pelvic pain, dysmenorrhea, infertility, constipation, digestive disturbances, and urinary dysfunctions to name a few.
Acupressure has roots in acupuncture and is based on more than 3000 years of Traditional Chinese Medicine (TCM). TCM supports Meridian theory and meridians are believed to be energy channels that are connected to the function of the visceral organs. Acupoints located along these meridians transmit Qi or the bio-electric energy through a vast network of interstitial connective tissue connecting the peripheral nervous system to the central viscera.
Acupressure has demonstrated the ability to improve heart rate variability, and thus decrease sympathetic nervous system activity. By decreasing sympathetic nervous system stimulation, the release of stress hormones such as epinephrine and cortisol is decreased, and the relaxation response can be augmented, which may correlate with decreasing levels of pain, stress, and anxiety2.
The Sanyinjiao (SP6) Acupoint
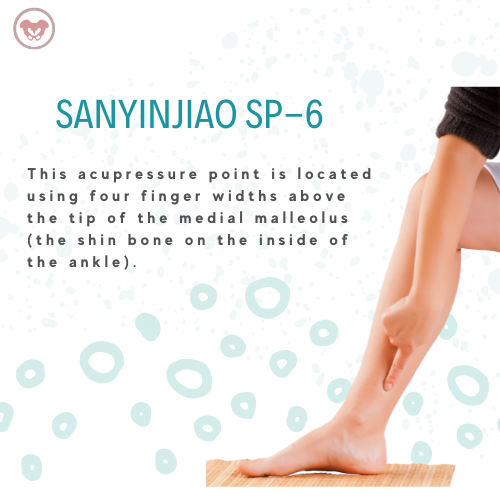
Sanyinjiao (SP6) acupoint is one of the most extensively researched points in the literature. It is located four finger-widths above the tip of the medial malleolus. Studies have found Sp 6 to be effective in relieving pain associated with primary dysmenorrhea, premenstrual syndrome (PMS), labor pain as well as symptoms of menopause. Ancient and modern acupuncture charts map the Spleen meridian as part of the principal 12 meridians which are connected to the physiological functions of key organs.
A recent systematic review published by Abarogu et al4 reviewed the available evidence for SP6 (Sanyinjiao) acupressure for the relief of primary dysmenorrhea symptoms, as well as patients' experiences of this intervention. The review included six studies with a total of 461 participants. The primary outcome was pain intensity. They found that:
- SP6 acupressure delivered by trained personnel significantly decreased pain intensity immediately after the intervention (effect size = -0.718; CI = -0.951 to -0.585; p = 0.000)
- Pain relief remained up to 3 h after the intervention (effect size = -0.979; CI = -1.296 to 0.662; p = 0.000)
The review concluded that SP6 acupressure appears to be effective when delivered by trained personnel for Primary Dysmenorrhea symptoms.
Acupressure has also been used with various types of mindfulness and breathing practices including Qigong and Yoga. Yin Yoga, a derivative of Hath Yoga is a wonderful complimentary practice to Acupressure. Yin Yoga is a calm meditative practice that uses seated and supine poses, held for three to five minutes with deep breathing. Yin poses supportively align the body to stress connective tissues along specific meridian lines thereby activating potent acupressure points that lie along those meridians. Mindfulness-based holistic interventions are the key to empowering our patients by giving them the tools and self-care regimens to lead healthier pain-free lives.
The course Acupressure for Optimal Pelvic Health brings a unique evidence-based perspective by integrating Acupressure and Yin Yoga into traditional rehabilitation interventions. It is curated and taught by Rachna Mehta. To learn how to integrate Acupressure into your practice, join the next scheduled remote course on March 19-20, 2022.
References
- Feldman DE, Carlesso LC, Nahin RL. Management of Patients with a Musculoskeletal Pain Condition that is Likely Chronic: Results from a National Cross-Sectional Survey. J Pain. 2020;21(7-8):869-880.
- Monson E, Arney D, Benham B, et al. Beyond Pills: Acupressure Impact on Self-Rated Pain and Anxiety Scores. J Altern Complement Med. 2019;25(5):517-521.
- Pain assessment and management standards for hospitals. Online document at: https://www.jointcommission.org/standards/r3-report/r3-report-issue-11-pain-assessment-and-management-standards-for-hospitals/
- Abaraogu UO, Igwe SE, Tabansi-Ochiogu CS. Effectiveness of SP6 (Sanyinjiao) acupressure for relief of primary dysmenorrhea symptoms: A systematic review with meta- and sensitivity analyses. Complement Ther Clin Pract. 2016;25:92-105.
- Chen MN, Chien LW, Liu CF. Acupuncture or Acupressure at the Sanyinjiao (SP6) Acupoint for the Treatment of Primary Dysmenorrhea: A Meta-Analysis. Evid Based Complement Alternat Med. 2013;2013:493038.
- Mehta P, Dhapte V, Kadam S, Dhapte V. Contemporary acupressure therapy: Adroit cure for painless recovery of therapeutic ailments. J Tradit Complement Med. 2016;7(2):251-263.

Part 1: Burnout
Let’s get real for a minute.
You are a highly educated professional. If you are reading this blog, I can assume you are invested in your career and your continued education. You are probably pretty skillful, and you help a lot of people.
BUT
How are you doing once you leave work?
Does your life outside of work give you joy and fulfillment?
Or do you leave your work setting completely drained, snippy with your loved ones, and too tired to care for yourself?
You have at least one advanced degree, probably some certifications, but did anyone ever teach you how to get your paperwork done on time?
Or how to leave work at work and not have your patients popping into your head day and night?
What about energy conservation? In fact, we may have been taught to give our ALL to work, to our patients, to strive for productivity and accomplishment. But where does that leave us?
BURNED OUT.
Part 2: Mindset
Taking continuing education classes was my pathway to becoming a better physical therapist.
But I had to go to therapy to learn how to survive as a physical therapist.
There were struggles.
Paperwork. I could NEVER finish in a timely way.
Timeliness. I was OFTEN running behind for patients.
Discharge. I had some patients for YEARS because I did not know how to discharge them even though they weren’t getting better. They depended on me, and I also depended on them.
Boundaries. I had none.
And here’s something that surprised me.
I had to change the way I THOUGHT before I could change my BEHAVIOURS.
I had to change my mindset.
I used to show up at work with the idea of Helping People. I felt responsible for their outcomes. If they weren’t doing well, I assumed I was missing something.
The shift looked like this:
I can show up at work to coach people who are responsible for their own outcomes. If they aren’t doing well, we can have honest communication about next steps (medical or otherwise), discharge, or resistance.
My patients are not my family, they are not my friends. I show up as a coach who is very interested in understanding their story and helping them reach their goals through a shared responsibility model of care.
My free time is sacred. I need to protect it for my mental, physical, spiritual, and emotional health. Because I am a priority, I will use 5 minutes of each treatment session to complete the patient’s treatment by doing paperwork.
Now, therapy is INVALUABLE. Don’t get me wrong, but paperwork, timeliness, discharge, and healthy boundaries are things MANY of us struggle with. So Nari Clemons and I designed a Continuing Education COURSE. We believe that therapists deserve to learn skills to preserve our wellbeing and strengthen our resilience against burnout.
Especially since the pandemic, more and more health care workers are reporting very high levels of burnout. Nari Clemons and I went through a period of burnout earlier in our careers. The tools and techniques we learned to heal ourselves and develop new patterns of delivering care are powerful. We know you might also be struggling and we want to help. So we developed a course to equip you. We would love to learn with you at Boundaries, Self-Care, and Meditation. A two-part, online journey toward experiencing a practice you enjoy and a life you love.
Boundaries, Self-Care, and Meditation is a two-part series intended to be completed in order. Participants should register for Part 1 and Part 2 at the same time, or complete Part 1 and wait to complete Part 2 at a later date. This course was developed by Nari Clemons, PT, PRPC, and Jennafer Vande Vegte, PT, PRPC and was "born out of our own personal and professional struggles and our journey to having a life and a practice that we love and can sustain." The intention of this class is deep, personal, and professional transformation through evidence-based information and practices. Both Part One and Part Two have a significant amount of pre-work to digest and practice before meeting via Zoom. Nari shares that "This sets the stage for you to find your path to experiencing more joy, energy, and balance."
Boundaries, Self-Care, and Meditation - Part 1 - Remote Course
In Part One, participants begin their process of study, meditation, and self-reflection in the weeks prior to the start of the class. Pre-work includes focusing on the neuroscience of pain, trauma, PTSD, and meditation. Participants will learn about the powerful influence both negative and positive experiences have on our nervous system’s structure and function. Personal meditation practice and instruction will create changes in the participant's own nervous system. Participants will also learn how to prescribe meditation for various patient personalities and needs, as well as analyze yourself through inventories on coping, self-care, empathy, burnout, values as well as track how you spend your time. Commitment to pre-work will facilitate rich discussion as we put what you have learned into practice around building a shared responsibility model of patient care, language to support difficult patients, and both visualizing and planning steps to create new, healthier patterns in your life and in your practice.
Boundaries, Self-Care, and Meditation - Part 2 - Remote Course
Part Two continues the focus on personal and professional growth for the participant, with a deeper dive into meditation and self-care practices. Yoga is introduced as a means of mindful movement and energy balance. Participants will learn to identify unhealthy relational patterns in patients and others, and skills on how to use language and boundaries to create shifts that keep the clinician grounded and prevent excessive energic and emotional disruptions. There is a lecture on using essential oils for self-care and possibly patient care. Learning new strategies to preserve energy, wellness, and passion while practicing appropriate self-care and boundaries will lead to helpful relationships with complex patients. This course also includes a discussion of energetic relationships with others as well as the concept of a "Higher Power". Course discussion will also include refining life purpose, mission, and joy potential, unique to the individual participant. The goal is that the participating clinician will walk away from this experience equipped with strategies to address both oneself and one's patients with a mind, body, and spirit approach.
The hip flexor muscles include the Iliopsoas group (Psoas Major, Psoas Minor, and Iliacus), Rectus Femoris, Pectineus, Gracillis, Tensor Fascia Latae, and Sartorius. When the hip flexors are tight it can cause tension on the pelvic floor. This can pull on the lower back and pelvis as well as change the orientation of the hip socket, lead to knee pain, foot pain, bladder leakage, prolapse, and so much more. The ramifications of iliacus and iliopsoas dysfunctions are discussed in a contemporary and evidence-based model with Steve Dischiavi in the Athletes & Pelvic Rehabilitation remote course.
A common issue with the iliacus and hip flexors is that they can shorten over time due to a lack of stretching or a sedentary lifestyle. When this happens, the muscle adapts by becoming short, dense, and inflexible and can have trouble returning to its previous resting length. A muscle that resides in this chronic contraction can become ischemic, develop trigger points, and distort movement in the body.
If you are treating patients with pain in their lower abdomen, sacroiliac joint, or that wraps around the lower back and buttocks, it could be because the hip flexors are tight. Traditional testing performed by medical practitioners tends to come back negative as many tests do not evaluate soft tissue issues. The best way to diagnose these concerns is through assessment with skilled palpation and structural evaluation.
One assessment test, the Thomas Test used for measuring the flexibility of the hip flexors, is discussed in the Athletes & Pelvic Rehabilitation course. In this test, the patient is supine while flexing the unaffected, contralateral leg at the hip until lumbar lordosis disappears. The length of the iliopsoas is determined by the angle of hip flexion displayed by the patient. The test is positive when the patient is unable to keep their lower back and sacrum against the table, the hip has a posterior tilt (or hip extension) greater than 15°, or the knee is unable to meet more than 80° flexion. A positive test indicates a decrease in flexibility iliopsoas muscles.
Treatment plans for the iliacus and hip flexors include stretching. An example includes the hip extension stretch or other active isolated stretches. Manual therapy, including trigger point release, can be used in conjunction with stretching to help muscle adhesion and release muscle tension. As with all treatment, the practitioner should discuss the risks, benefits, and treatment options, and obtain consent with patients. Prior to proceeding with manual therapy treatment make sure to establish a pain scale, assess the patient's range of motion and strength, and (if needed) perform the appropriate neurologic testing.
To learn more about treatment philosophies for the pelvis and pelvic floor and global considerations of how these structures contribute to human movement you can join Steve Dischiavi in the Athletes & Pelvic RehabilitationRemote Course.

You may be interested in attending this course if you have taken:
Yoga for Pelvic Pain
Sacroiliac Joint Current Concepts
Mobilization of the Myofascial Layer: Pelvis and Lower Extremity
Weightlifting and Functional Fitness Athletes

Amanda Moe, DPT, PRPC specifically treats women, men, and children with disorders of the pelvis and pelvic girdle. Amanda earned her Pelvic Rehabilitation Practitioner Certification (PRPC) in 2015 to distinguish herself as a highly qualified and specialized practitioner in the field of pelvic health and worked at Texas Children's Hospital in Houston, TX. There Amanda assisted with the development and expansion of the pediatric pelvic physical therapy program treating children with a variety of diagnoses such as bowel and bladder dysfunction, constipation, encopresis, coccydynia, abdominal/groin pain, as well as other disorders related to the pelvic girdle. Amanda enjoys assistant teaching with the Herman & Wallace Pelvic Rehabilitation Institute in her free time as well as working out, practicing yoga, and spending time with her family.
Before the Book
I started off my career in Pelvic Physical Therapy treating adult women and men as do many physical therapists entering the pelvic niche. My local children’s hospital discussed a need for pelvic physical therapy in children which, with the help of Herman and Wallace’s Adult/Pediatric courses as well as mentoring from my local Gastroenterology department, I devoted the next few years of my career to.
I aided in program development and expansion of Pediatric Pelvic Physical Therapy services at Texas Children’s Hospital in Houston, Texas. After moving out of state, I then collaborated and expanded Pediatric Pelvic Physical Therapy services in Pittsburgh, Pennsylvania—working closely with both the Urology and Gastroenterology Department at UPMC’s Children’s Hospital of Pittsburgh. While treating children with pelvic dysfunctions is similar to treating those in adults, there is much to be considered when providing education to children, parents, and even referring providers about pelvic floor dysfunction and Pediatric Pelvic Physical Therapy.
The NEED for this Book
When educating children, parents, or even referring practitioners about pelvic floor dysfunction and physical therapy, I grew frustrated with the lack of “simplified” or “child-friendly” models, illustrations, or depictions available. Specifically, I saw a need for:
- the depiction of pelvic girdle muscles and organs in a “child-friendly” format for BOTH boys and girls
- pictures of what a child’s pelvic muscle “role” or “activity” is during peeing or pooping
- what common muscle dysfunctions in children “look like” in easy-to-understand pictures
Additionally, I longed for a book or resource that described common conditions and symptoms treated in Pediatric Pelvic Physical Therapy (or Occupational Therapy) as well as what the Pediatric Pelvic PT/OT evaluation and treatment may look like. In 2021, I decided to do something about this which lead to me writing my first book: Pelvic PT for ME: Storybook Explanation of Pelvic Physical Therapy for Children.
Book Features
Do you have parents, patients, referring physicians, or other medical providers wondering exactly what Pelvic Physical Therapy for children is like—look no further! In Pelvic PT for ME: Storybook Explanation of Pelvic Physical Therapy for Children, I explain the basics all in a rhyming, child-friendly format. This book introduces the collaborative nature in resolving children’s potty or pelvic troubles and describes how Pediatric Pelvic PT/OT often works closely with gastroenterologists, urologists, pediatricians, or other providers to remedy a child’s complaints. Pelvic PT for ME has many unique features pertaining to Pediatric Pelvic Physical Therapy, some of which are highlighted below:
- Common Conditions Treated
- I discuss typical conditions that are treated in Pelvic PT such as pee leaks, poo problems (constipation, poo leaks/smears), nighttime bedwetting, pelvic pain, and many others.
- Child-Friendly Anatomy Illustrations
- Age-appropriate anatomical illustrations of muscles and organs in the pelvic girdle are utilized throughout the book to aid in explaining bowel, bladder, and pelvic functioning.
- Pelvic Floor Muscles during Peeing or Pooping
- Pelvic floor muscle anatomy, functioning, and dysfunction—as they relate to potty troubles—are discussed through the use of child-friendly images to enhance not only child but also parent and referring provider understanding.
- Common Evaluation Techniques and Treatment Interventions
- The Pediatric Pelvic Physical Therapy evaluation, as well as typical treatment interventions, are discussed and illustrated to make both children and parents excited to seek treatment!
- Inclusion of Occupational Therapy
- While the field of Pediatric Pelvic Physical Therapy in of itself is new, I briefly discuss the inclusion of Occupational Therapists also providing Pediatric Pelvic Therapy services.
Where to Purchase
My primary goal behind the creation of this book was to develop an affordable resource for every Pelvic PT/OT who treats children. Secondarily, my goal was to increase knowledge and understanding of our services to parents, children, and potential referral sources or colleagues. Pelvic PT for ME encourages parents and children to refuse the notion that potty troubles “go away with age” and empowers children to be active participants in their Pelvic PT (or OT) experience. Enjoy this comprehensive yet simple storybook explanation of Pediatric Pelvic Physical Therapy, available on Amazon for $15.
Contact
Contact me or check out my website for more information: www.pelvicphysicaltherapyandmore.com
IG/Facebook: amandampelvicpt

Bre Stuhlmuller is an LA-based doctor of physical therapy (DPT) who practices at Origin, a leading provider of virtual and in-person physical therapy for women and individuals with vaginal anatomy. Dr. Stuhlmuller is especially interested in helping women through their pregnancy/postpartum journey and strives to help her patients understand the purpose behind the therapy they are receiving so they can begin to relate to their bodies differently and take an active role in their rehabilitation process.
When Covid ramped up in 2020 and Origin began to focus more fully on virtual care, many PTs were excited about this new way to reach patients. Although the prospect of working from home piqued my interest, I was still skeptical. I dabbled in virtual care at the beginning of my time at Origin, with the occasional appointment here and there. Even still, the concept of it was hard for me to fully grasp and I couldn’t say that I loved it. It felt unknown and even intimidating. I love to connect with my patients — establishing a good rapport is one of my strong suits — and I was worried that what I did in person wouldn’t translate the same way through a screen.
Looking back, I realize my attitude was very much informed by what I’d learned in training. I had a mentor during one of my rotations who emphasized the importance of human touch, how it was integral to the healing process. What would assessment and healing look like if I couldn’t use my hands?
To be fully transparent, manual therapy had also become a fallback for me while caring for my patients. If a patient was struggling to understand a concept, I could use my hands to show them. If I found myself at a loss of what to do next, I could provide manual therapy — it was always welcomed, felt productive, and gave me time to plan. With virtual, I knew I would have to rethink how I approached my assessment and treatment strategy, and I had no idea what that might be.
New Fuel for Creativity & Connection
When it was clear I didn’t really have a choice, I gave virtual PT a try for more than just those occasional appointments. At first, as I was building up my caseload, it lived up to my not-so-positive expectations. It just wasn’t the same and I felt completely out of my element. It wasn’t until I began filling my caseload entirely with virtual visits that it began to surprise me.
As I engaged more consistently with patients on Zoom, my creativity kicked in. Without my hands to fill in the gaps, I really had to think about the cues that I was giving and how I was explaining things. Suddenly, my mind was lighting up with new ideas and ways of getting my point across. Where should the patient be focusing their attention? What should they be noticing or feeling?
I began helping patients tune into their bodies, instead of solely looking to me to give them information. Often, when I first ask “What do you feel when you do X?” a patient’s first response is vague and unsure. Then I’ll try again, talking through the concepts and movement in more detail. I’ll describe the outcome I am after and provide analogies and examples. If that doesn’t work, I’ll have them try a different position, or experiment with a new analogy that relates to their life and specific situation.
What happens next has been so encouraging — I see them have a pretty powerful ah-ha moment. (And because they’re not wearing a mask, it’s great to be able to see the understanding on their face!) They’re connecting with and learning from their body directly, which gives them so much empowerment. They tap into their own abilities instead of only relying on mine, which is exactly what we hope to give to our patients. On my side, I continue to gain clarity and hone my communication skills. I’m excited to share that despite doing all of this through a screen, my connection with patients feels as strong as ever.
That’s not to say that patients aren’t missing manual therapy! If you’re a PT who sees patients in person, you know how much they like (and often expect) it. I think they can tend to rely on it too much — and a decent number of people really want to come in and just get something like a massage. That can be a struggle. We are not massage therapists. And unfortunately, some patients think they need it in order to get better. I think that will be an ongoing struggle when it comes to getting patients to try virtual physical therapy. But, in my experience, once they do try virtual, they are quickly won over.
The Habit Building Power of Home
Another unexpected benefit of virtual physical therapy is the level of follow-through. For starters, patients cancel much less, which makes sense — it’s a lot easier to hop on a Zoom call at the last minute than it is to get in the car (and find parking). And if childcare isn’t available, they can keep an eye on their kids while we do our visit. We may not always get quite as much done, but at least we are able to do something, which I’m constantly reminding my patients is always better than nothing.
Along the same lines, in the few months since I’ve switched to solely treating virtually, I’ve been surprised to discover that patients seem more consistent with their exercises, not less. We’ll be collecting more data on this at Origin, but my guess is that being introduced to an exercise in the same environment where they’ll be doing it on their own makes a difference. When they do their exercises with me during a virtual visit, they’re creating a foundation of a habit. Later on, when it’s time to continue on their own, they can pick up right where they left off.
As much as I absolutely love our clinics at Origin — having all the equipment on hand, the music playing, and the other patients and PTs around — it is a very different experience for patients compared to being at home. At home, patients have to self-motivate and are limited to the equipment they happen to have or are willing to buy. Starting from scratch in their own space can often be a major barrier.
When we’re in a virtual visit, I can help a patient set up the space where they’ll do their exercises, and we can improvise. They may need to use a thick pillow instead of a pilates ball, or a rolled-up towel instead of a yoga block. This eliminates all those excuses along the lines of, 'I couldn't do my exercises because I didn’t have X.’ It not only helps me stretch and refine my skills as a PT, it helps patients gain more agency— it encourages patients to get into the mindset of “let’s see how I can make this work with the resources I have.”
Just as invaluable is being able to coach a patient through functional movements. I can watch a new mom lift their baby out of their crib or get up from their couch, then give tips and recommendations that are specific to their setup. Then I watch them immediately apply those tips and feel the difference. And boom, I know they’ve got it.
Tips for PTs Interested in Going Virtual
As a PT, having a separate, designated space to work is critical. At first, I was doing it in the corner of my bedroom, next to my bed, with limited lighting. Although I made it work, it was awkward to not have room to move and didn’t serve my patients the way I wanted. I have now made a space in our garage with bright lighting and a white backdrop behind me. You don’t necessarily need a whole setup, but you want to ensure that your patient can see your entire body when demonstrating movements or exercises. And of course, you need strong, reliable wifi!
One challenge that comes up is that virtual patients can be distracted at the start of or even throughout a visit. Because they’re at home and may have just stepped away from kids or work, they may need time to refocus. This is very different from being at the clinic, where the few minutes it takes to check-in and get settled helps them be more present. So I’ve learned to expect this, give them some grace, and will spend a few minutes bringing their attention back to their goals.
I also want to say that I do miss being in the same space with other Origin PTs. I miss the time in between patients when you can have those quick, but incredibly helpful conversations like “oh have you had a patient who presents like this,” or “let’s go into a room and I’ll show you how I do this.” It’s hard to recreate that kind of spontaneous interaction online. We have a shared Slack channel where PTs can chat throughout the day about our cases and although it helps to fill in that missing gap, it can also be nothing but crickets and still lacks that same feeling you get physically being in the office with your colleagues.
One major perk, however, is being able to spend more time between patients with my 2-year-old daughter. It makes being a working mama feel a little less of a sacrifice. But don’t get me wrong, it also comes with its challenges. I don’t have that same downtime driving to/from work to decompress and switch between mom mode and work mode. And it can be easy to get distracted between appointments and do chores or play with my daughter instead of cranking out my notes. At some point, I imagine I will want to split my time between the clinic and working from home. But for now, I am honestly more than content working virtually.
Origin is already working on new ways to integrate virtual and in-person therapy — thinking beyond either/or, toward a model where we can choose what works best from patient to patient and visit to visit. In the meantime, I’m excited to continue with virtual care and our patients are loving this option. My schedule has been more full in the past 4 months than it was before I went virtual, and I’m seeing more people get better under my care. It’s truly amazing to see them making so much progress, right at home.

As 2022 has gotten underway, it has already brought many of us to a place where we simply need to hear something lighthearted. The start of a new year also gives us a chance to examine priorities and make room for what matters most. “What matters most” can look different for each of us; for me, it’s my family – including two dogs – Stella and Sadie. Of course, the dogs fall in line behind my human nuclear and extended families, however, they are such a part of my daily life and contribute to my quality of life, it seems only natural to share this story with a wider audience -especially because this story revolves around one of my favorite topics – intentional nourishment!
Let me begin by telling you about our 5-year-old Golden Retriever named Stella. She came to us as one of only three puppies in a litter; a pleasantly plump pup, she was well developed, well-fed, and well-loved. According to everyone who has had the opportunity to meet her, she is the happiest dog they’ve ever met. When we brought her home at eight weeks, she topped the scale at 21 lbs.
Stella's fur was shiny, her disposition sunny; she emanated maturity and wisdom. She slept through the night with such efficiency, we hardly remember having to let her out at night as a puppy. She was content; the perfect combination of calm and energetic. She was a breeze to housetrain, has an impeccable record of only two accidents in the house, and nary an indoor fecal incontinence episode. Stella brought us so much joy that we decided on a whim to add a second puppy to the milieu.
The second puppy is our ~16-week-old Golden Retriever puppy named Sadie. This past October – by coincidence – my family learned about some surprise Goldens needing homes – 17 to be exact – and we wondered if we might be interested in one. Two weeks later, sweet Sadie came home with us.
Weighing in at only 13 lbs 6 oz at eight weeks, she was miniature compared to Stella at the same age. It didn’t take us long to figure out that not only was she smaller, but her digestive tract and elimination systems were not like Stella’s either. Sadie pooped often - what seemed like every hour – including sometimes in the house. Her bottom was sore and irritated, and she seemed frustrated and uncomfortable. My husband and I looked at each other more than once thinking the same thought: WHAT did we get ourselves into?!?
Sadie tested negative for parasites, and the vet said she was just working on adjusting to her new home and to give it time. He also suggested we might be feeding her too much. So, we fed her less - but that didn’t help. We tried adding pumpkin, that didn’t help either. Then we upped her food amount again, tried timing her foods differently, tried feeding her more often, then less often. None of these approaches helped. The messes continued.
We began to feel exasperated. I was reluctant to try adding new foods for fear of upsetting her GI tract further.
This puppy was pooping nonstop – much of it type 6 & 7 applying the Bristol Scale to dogs (1). She barely came in at 16 lbs. week 10 and alarmingly, she still weighed 16 lbs. at week 12. The vet confirmed our concerns – she was too thin and needed to put on weight.
Now I started to worry. With all the bowel troubles she had, how could she thrive? We weren’t getting any continuous hours of sleep at night which meant she wasn’t either. It was an exhausting few weeks.
Given what we had tried – with no success – we had no choice but to begin what we called “Operation Nourishment” for this little puppy. We put worries aside about adding new foods and applied what we understand about functional nutrition to help our sweet Sadie.
“Operation Nourishment” consisted of following several basic digestive principles:
- Make her food more digestible
- Feed her nutrient-dense options (dog appropriate, of course)
- Practice puppy-version mindfulness at mealtime
- Help support her puppy microbiome
#1: Make her food more digestible: Without changing the kibble she was eating, we soaked it with a bit of water before ingestion to soften it. This helped make her food easier to break down in her digestive tract and also helped S L O W D O W N her tendency to inhale food. Prior, she was definitely not chewing her food thoroughly which can result in undigested food reaching the colon and causing irritation. The softened food facilitated just the slightest bit of chewing and tripled the time it took her to finish a meal, giving her GI tract less of a shock.
#2: Feed her nutrient-dense options: We began adding an organic egg (3,4) softly cooked in a tiny bit of coconut oil (2) to her breakfast. The egg adds a whole food-based protein-containing cholesterol, vitamins, and minerals -all important for building her gut lining and nervous system. Coming from such a large litter in a somewhat stressful/chaotic environment, her gut and nervous system may not have been at their healthiest and needed extra support (4).
#3: Practice mindfulness at mealtime: The egg at breakfast has quickly become the highlight of her day.
The anticipation while watching us cook it calms her. She intently follows as the pan comes out of the cupboard and onto the stove. She watches more intently as we slowly cook the egg. Then she must wait even longer while it sits in her bowl to cool up on the countertop.
I presume this has taught her mindfulness and presence before eating – essential for thorough digestion!
#4: Help support her puppy microbiome: We gradually began to add a dollop of kefir (5) to her breakfast and dinner – knowing that even dogs have a microbiome and that cultured foods can help normalize gut flora which can help normalize stool consistency. A healthy gut helps us extract nutrients from the food we eat. It can also, fascinatingly, modulate our stress responses.
“Operation Nourishment” began to take effect almost immediately. She jumped from 16 to 24 lbs. in 3 weeks! We were so proud! She finally began to have a soft, healthy belly - and the vet was thrilled, “whatever you’re doing, keep it up!”. She began to sleep through the night – and WE were thrilled. She also began to sprout her golden retriever fur patterns and take on more shine. Brilliantly, her stools became formed – a perfect 4 on the Bristol Stool Scale (1) and had significantly less urgency which led to the elimination of accidents. We were shocked at how quickly her body adapted to a diet higher in nutrient density and digestibility– one that was safe and appropriate for puppies.
Upping her nutrient density and digestibility helped unlock her potential so she could become the best sweet version of herself. Once more deeply nourished, she happily settled into her calm, gentle nature. She and Stella have become quite the pair. And we – her humans - are finally, gratefully sleeping again (most nights), which makes us adore her even more.
How might A Tale of Two Goldens provide us with insight relevant to pelvic rehabilitation?
We acknowledge that no two people come into this world in exactly the same circumstance and that we each arrive with a certain level of built-in resiliency. Some of us come into this world with our tails wagging, ready to greet everything that comes our way. Many of us and those we serve– let’s face it –are figuratively more like Sadie. We have the potential waiting inside of us to become the best version of ourselves.
Sometimes reaching that potential takes just a little tweaking, a little coaxing, a little know-how. Maybe that tweaking, coaxing, and know-how could include principles of “Operation Nourishment” for ourselves and those we serve in the form of nourishment-focused guidance. With a little patience, time, and intentional action, we may be surprised to see how a few small changes have an enormous impact on what matters most to each of us and those we serve.
Nourishment knowledge – now more than ever – is vital.
Join us in 2022 for Nutrition Perspectives for the Pelvic Rehab Therapist to learn more about these principles and beyond. Upcoming 2022 remote offerings include Feb 26-27, April 29-30, July 23-24, August 27-28, Sept 23-24, Oct 22-23, and Nov 11-12. We welcome you to join us.
References:
- https://www.bladderandbowel.org/wp-content/uploads/2017/05/BBC002_Bristol-Stool-Chart-Jan-2016.pdf Accessed January 11, 2022.
- Alves DVS, Sousa MSB, Tavares MGB, Batista-de-Oliveira Hornsby M, Amancio-Dos-Santos A . Coconut oil supplementation during development reduces brain excitability in adult rats nourished and overnourished in lactation. Food Funct. 2021 Apr 7;12(7):3096-3103. doi: 10.1039/d1fo00086a. Epub 2021 Mar 15. PMID: 33720258.
- Avirineni BS, Singh A, Zapata RC, Phillips CD, Chelikani PK. Dietary whey and egg proteins interact with inulin fiber to modulate energy balance and gut microbiota in obese rats. J Nutr Biochem. 2022 Jan;99:108860. doi: 10.1016/j.jnutbio.2021.108860. Epub 2021 Sep 11. PMID: 34520853.
- Choi, M., Lee, J. H., Lee, Y. J., Paik, H. D., & Park, E. (2022). Egg Yolk Protein Water Extracts Modulate the Immune Response in BALB/c Mice with Immune Dysfunction Caused by Forced Swimming. Foods, 11(1). doi:10.3390/foods11010121
- Vieira CP, Rosario AILS, Lelis CA, Rekowsky BSS, Carvalho APA, Rosário DKA, Elias TA, Costa MP, Foguel D, Conte-Junior CA. Bioactive Compounds from Kefir and Their Potential Benefits on Health: A Systematic Review and Meta-Analysis. Oxid Med Cell Longev. 2021 Oct 27;2021:9081738. doi: 10.1155/2021/9081738. PMID: 34745425; PMCID: PMC8566050.
By accepting you will be accessing a service provided by a third-party external to https://hermanwallace.com/