
Stacey Roberts is an expert on shockwave therapy and joins Herman & Wallace to present her course Shockwave Treatment: Therapeutic Interventions in Pelvic Health & Demystifying the Research. Over the last year, Stacey Roberts has been analyzing shockwave research extensively to develop clear and concise therapeutic applications in the rehabilitation setting for pelvic health, sexual health, and muscular-skeletal patients. She is finding extraordinary results with her patients using this modality in her practice.
Stacey sat down with us at The Pelvic Rehab Report to answer some of the most asked questions that she gets about shockwave therapy.
What is a Shockwave?
A shockwave is an interesting phenomenon and can be both natural and manmade. The Encyclopedia Britannica defines a shockwave as "a strong pressure wave in an elastic medium such as air, water, or a solid substance, produced by supersonic aircraft, explosions, lightning, or other phenomena that create significant changes in pressure.”
What is Shockwave Therapy?
Shockwaves used in therapeutic settings are produced by modalities that create supersonic waves. These waves penetrate the human tissue and can travel to areas of the body, producing a biological effect. The first therapeutic use of shockwave therapy was lithotripsy. This procedure was first used in the 1970s and utilizes high-energy high-intensity shockwaves to break apart kidney stones without surgical intervention.
Clinics now use low-intensity focused and unfocused shockwaves to exhibit a form of energy within the tissues. The shockwaves are made up of 3 phases: a mechanical phase, a chemical phase, and a biological phase. A true shockwave device impacts the tissue and can increase blood flow, activate connective tissue, modulate the inflammatory response, and contribute to pain relief.
Is there just one type of Shockwave device?
No, there are 3 types of true shockwave devices.
- Electrohydraulic (deepest penetration)
- Electromagnetic (minimal to moderate penetration)
- Piezoelectric (minimal penetration)
Why is Shockwave therapy beneficial?
When a true shockwave device is used, patients often note faster improvement than with manual therapy alone or with other standard modalities such as ultrasound, laser, and radial wave therapies.
In my experience, the depth of penetration also allows my skills as a manual therapist to be used more effectively. By using shockwave therapy, I can now treat an area in 5 minutes that previously would have taken 10-15 minutes. It also tends to be much more comfortable for the patient.
Are radial, pneumatic, or EPAT true shockwave devices?
No, they have been lumped in under the Shockwave umbrella but do not produce the force or effect of a true shockwave. These devices have therapeutic value for superficial musculoskeletal injuries including plantar fasciitis and lateral epicondylitis. However, the energy produced by the mechanical pounding of the tissue from a radial wave device does not produce a shockwave.
The energy produced by radial pneumatic devices disseminates just below the surface of the skin. An electrohydraulic shockwave device can produce energy up to four to six inches from its point of contact, making this particular type of shockwave device is especially useful for pelvic floor therapy.
Electromagnetic shockwave devices can penetrate approximately two inches. This is approximately the same depth as the piezoelectric shockwave device.
I see ESWT in the research a lot. Is that shockwave therapy?
ESWT stands for Extracorporeal Shockwave Therapy. This is a common abbreviation used in the literature that originally was meant to label shockwave devices. However, other non-shockwave devices, such as radial devices, also use ESWT in research studies.
In the true sense of the word, and shockwave definition, a radial device is NOT a true shockwave. There is much confusion in the research that takes time to unravel, so I have dedicated a portion of the Shockwave course to tease out the differences. Many clinicians own a radial device and were told that it was a shockwave device. Unfortunately, that is not completely accurate, according to the International Society for Medical Shockwave Treatment.
What can be treated with true Shockwave therapy related to Pelvic Rehab?
True shockwave therapy has shown to be beneficial for the following issues:
- Erectile Dysfunction
- Peyronie’s Disease
- Chronic Prostatitis
- Chronic Pelvic Pain
- Incontinence
- Urgency
- Cystitis
- Vaginismus
- Vulvodynia
- Vestibulodynia
- Persistent Genital Arousal Disorder (PGAD)
Other areas of research:
- Dysmenorrhea
- Endometriosis
- Testicular Pain and Dysfunction
- Premature ejaculation
- Urinary retention
How is shockwave different from ultrasound?
A wave produced by ultrasound is a sinusoidal wave versus a shockwave that has a strong positive pressure followed by a longer negative pressure wave. See chart:
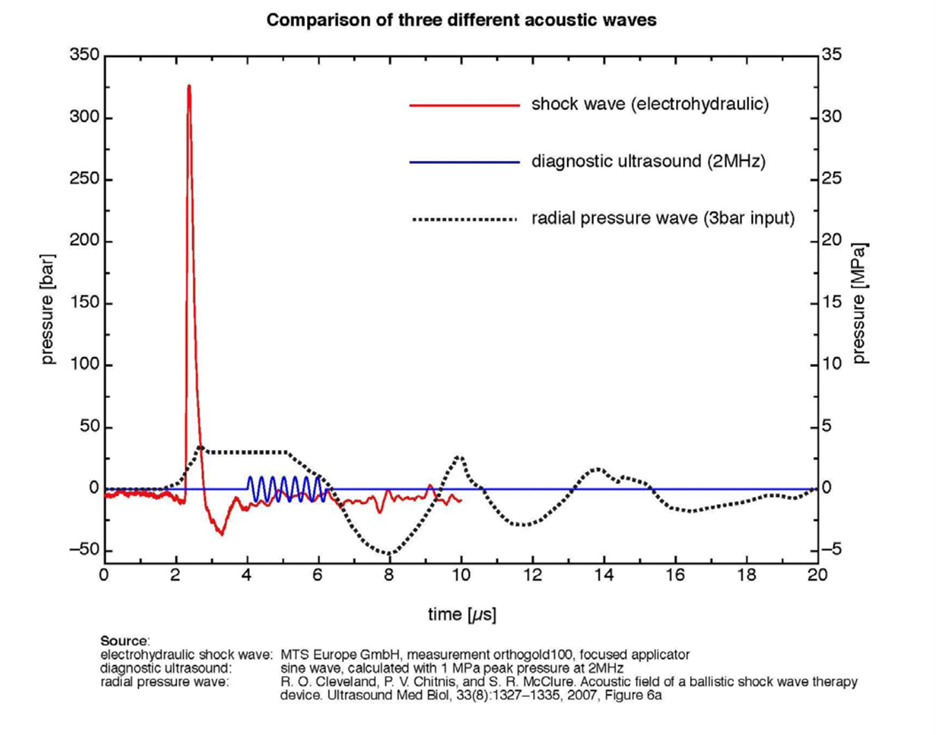
This results typically in larger cavitation bubbles around the cellular structures and fewer treatments to reach patient goals. Continuous ultrasound produces its effect by heating the tissue, whereas a shockwave device does not cause any heating of the tissue to produce its therapeutic effect.
Is shockwave therapy covered by insurance?
Like other valuable modalities, insurance does not typically cover low-intensity shockwave therapy. However, in times of decreasing reimbursement, patients are increasingly more than willing to pay out of pocket for treatments that result in positive outcomes in shorter periods.
Why should I take your course Shockwave Treatment: Therapeutic Interventions in Pelvic Health & Demystifying the Research?
You should take this course if you are interested in:
- Learning how one of the most effective non-invasive treatment modalities of our time related to pelvic and sexual health produces its results
- Understanding how this modality produces its results and how it is being utilized in clinics to improve treatment outcomes related to pelvic health
- How this modality can enhance results when combined with manual treatment techniques
- How to review the research efficiently without combing through data that may or may not be actual Shockwave research
- Being able to differentiate one machine from another to make an educated decision on which shockwave device may fit into your clinic
- What questions to ask company sales reps that are selling devices to make sure you are talking about a true shockwave device
If you would like to learn more about incorporating shockwave therapy into your daily practice, then join H&W Shockwave Treatment: Therapeutic Interventions in Pelvic Health & Demystifying the Research. This course is scheduled for February 20th and June 26th of 2022.
Allison Ariail is one of the creators of the Herman & Wallace Oncology of the Pelvic Floor Course Series. Practitioners who took the main Pelvic Floor course still weren’t sure how to handle oncology tissues, what they could do, or how to treat these patients. Thus the oncology series was created to provide additional instruction for treating pelvic cancer patients.
Allison Ariail is a physical therapist who started working in oncology in 2007 when she became certified as a lymphatic therapist. She worked with breast cancer, lymphedema patients, head and neck cancer patients, and the overall oncology team to work with the whole patient to help them get better. When writing these courses, Allison was part of a knowledgeable team that included Amy Sides, Nicole Dugan, Tina Allen, Jennafer Vande Vegte, and Megan Pribyl.
The Oncology Series is comprised of three different courses, with the first course, Oncology of the Pelvic Floor Level 1, designed as an overview of the oncology world. Allison explains that the reason level 1 is an introduction is that “this is because the oncology medical world is so different from what a lot of rehab professionals are used to.”
Oncology of the Pelvic Floor Level 2A addresses colorectal cancers, anal cancers, and cancers that affect male genitalia. New information about how to treat prostate cancers is also discussed. The third course, Oncology of the Pelvic Floor Level 2B, is being launched this year in 2022 and covers gynecological cancers and bladder cancers. The tentative launch will be in November 2022.
There are a lot of labs in all of these courses that are specific to the side effects that these patients have after going through radiation and other surgical treatments. Oncology patients can have a range of problems from radiation fibrosis, range of motion issues, and weakness. While these patients may be seeing a certified lymphatic therapist, that CLT is not going to have time to address these additional issues. Allison Ariail explains, “that is where this knowledge from these courses comes in. Not just as a supplement for that patient, but as a completely different treatment, where that patient really needs to see both therapists. One for lymphedema and one for radiation fibrosis, or weakness, or other side effects, that can affect their quality of life.”
Certified Lymphatic Therapists can skip OPF1 or dive in at OPF2A or OPF2B as long as they have taken the main Pelvic Floor Level 1 course prior.
Oncology of the Pelvic Floor Series 2022 Schedule
Oncology of the Pelvic Floor Level 1
Oncology of the Pelvic Floor Level 2A
Oncology of the Pelvic Floor Level 2B
- TBD – course launch is tentatively scheduled for November 2022
- If you are interested in attending this course, please contact us!

Another circle around the sun.
Another covid pandemic run.
Courses scheduled all year round.
Remote Courses. Live Events, and Satellites abound.
From Oncology and the Pelvic Floor Level 1and Pregnancy Rehabilitation.
To Pain Science for the Chronic Pelvic Pain Population.
Instructors are ready.
With TAs aplenty.
Prove your advanced expertise
And sit for the PRPC.
Our resolution here at Herman & Wallace is to provide even more course content for you! Our plan is to have a total of 22 new courses from 2021-2022 available and over 400 course events/satellites scheduled! In addition, we at H&W want to take the time to let our faculty, teaching assistants, hosts, and students know how much we appreciate you! As the pandemic continues into 2022, know that we see you. We appreciate all that you do and the efforts that you go to.
The best way to make an attainable New Year's Resolution is to use SMART goals. Most of us have seen SMART goals used for work and business decisions. Keep the specific, measurable, and time-specific aspects of goal setting while making sure they are attainable and realistic.
Did you set any New Year's Resolutions yet? If not, then here are 5 suggestions!
- Learn something new. Have fun while challenging yourself to take the next step in your pelvic rehab journey. H&W offers courses that are beginner, intermediate, and advanced levels.
- Build your confidence. Whether it is in gaining confidence in internal exams, or in treating the lumbar nerve H&W has a course for you.
- Meditate & Practice Mindfulness in your personal life and practice. H&W recommends joining Restorative Yoga for Physical Therapists or Boundaries, Self-Care and Meditation.
- Try something that scares you. Push yourself to try things that are out of your comfort zone. Take a new course for a different patient demographic to incorporate into your daily practice such as Bowel Pathology and Function or Transgender Patients: Pelvic Health and Orthopedic Considerations
- Volunteer. Give back to the Pelvic Rehab Community by TA'ing for a satellite course.
Herman & Wallace wishes you a fresh start with renewed energy and confidence throughout the New Year. Happy 2022!

Pelvic rehab therapists and physiatrists both focus on the return to life and function. In a recent interview, Allyson Shrikhande shared, “Physiatrists are extensions of physical therapy. We analyze and treat the muscles, nerves, and joints of the pelvis non-operatively.” Physiatrists bring a holistic viewpoint and are trained to look at the interplay between the different organ systems with each other, as well as the muscles, nerves, and joints.
Dr. Shrikhande is joining H&W to bring in the New Year with her short format course, Working with Physiatry for Pelvic Pain, on January 11th. This 4-hour course delves into diagnosis and non-operative treatment options for Chronic Pelvic Pain (CPPS). Allyson believes in an interdisciplinary team approach to treating patients and spends time discussing the interplay between professions for the betterment of patients.
Physiatrists often work with an interdisciplinary team of rehabilitation experts to coordinate a treatment plan that is based on each patient’s personal needs, abilities, and goals. Members of this interdisciplinary team can include several practitioners:
- Rehabilitation nurses
- Physical therapists
- Occupational therapists
- Respiratory therapists
- Gynecologists
- Dieticians
You can find many clinics and healthcare systems that incorporate a variety of professionals and share a multidisciplinary approach. Multidisciplinary typically means that there are multiple providers but not working together in the same way as interdisciplinary teams. The interdisciplinary approach differs from the multidisciplinary approach by focusing on the common patient and team goals, compared with a discipline-specific focus. It emphasizes regular and effective communication, coordination, and integration of care. Interdisciplinary medical teams are able to work together for functional outcomes (1).
Patients with Chronic Pelvic Pain Syndrome (CPPS) typically experience pain in the abdomen, lower back, and genitals. These patients often experience frequent urination, pain when sitting, and even pain during or after sexual intercourse and impair the function of organs such as the bladder and bowel.
CPPS is a multifaceted disorder. It is a challenge to health care providers because of its unclear etiology and complex natural history. In this case, a pelvic physiatrist may lead an interdisciplinary team including a gynecologist, psychologist, and physical or occupational therapist. In her course, Dr. Shrikhande shares how important it is to understand the pathophysiology of pain. “Experiencing pain for a long period of time changes how the brain receives and processes pain signals. Essentially there is this amplification of pain. This really describes neuroplasticity. The rehab world is founded on neuroplasticity, meaning your peripheral and central nervous system can change in a positive direction or a negative direction.”
Dr. Shrikhande delves into the important role of the physiatrist and pelvic therapist in CPPS treatment in her course Working with Physiatry for Pelvic Pain. Physical and occupational therapists are trained in the clinical features of common musculoskeletal pathology and musculoskeletal examination and develop treatment plans, exercise programs, and physical modalities (including heat, cold, TENS). As a pelvic therapist, an evaluation for CPPS is not just of the pelvic floor. It includes other structures including the abdomen, hip complex, diaphragm, ribcage, low back and looks for weakness, difficulty of coordination, and assessing breathing dysfunction.
As stated by the American Academy of Physical Medicine and Rehabilitation, "Physiatrists, on the other hand, make and manage medical diagnoses and prescribe the therapies that physical and occupational therapists perform. Despite these differences, both therapists and psychiatrists collaborate and communicate to ensure patients are receiving appropriate treatment (2)."
If you have taken Pain Science for the Chronic Pelvic Pain Population, Pudendal Neuralgia and Nerve Entrapment, Yoga for Pelvic Pain, Nutrition Perspectives for the Pelvic Rehab Therapist, Biofeedback for Pelvic Muscle Dysfunction - Satellite Lab Course, or Male Pelvic Floor Function, Dysfunction, and Treatment - Satellite Lab Course you may be interested in attending this course (Working with Physiatry for Pelvic Pain).
Upcoming Working with Physiatry for Pelvic Pain Courses
References:
- Poduri K. R., Vanushkina M. Epidemiology of Aging, Disability, Frailty and Overall Role of Physiatry. Geriatric Rehabilitation. 2018; Pages 1-17. https://doi.org/10.1016/B978-0-323-54454-2.00001-7
- American Academy of Physical Medicine and Rehabilitation. The Medical Student's Guide to PM&R. https://www.aapmr.org/career-support/medical-student-resources/a-medical-students-guide-to-pm-r/what-is-the-difference-between-physical-therapy-and-physiatry

Happy Holidays to all of you from Herman & Wallace!
Herman & Wallace has more than 55 different courses with over 200 individual course events scheduled throughout the year to choose from. Our course catalog is growing all the time with new courses, new instructors, more course dates, and even more satellite locations!
In 2022 there are already six BRAND NEW courses available, with more to be planned. H&W is kicking off the new year strong with Dr. Michael Hibner on January 9th with Pudendal Dysfunction: The Physician's Perspective. Kristina Koch is back in 2022 with her newly updated and reformated course, Pharmacologic Considerations for the Pelvic Health Provider which is scheduled for April 10, July 9, and November 19th.
Do you live near Salt Lake City, Utah? Our first live, in-person course since the pandemic will be there on March 12-13, 2022: Dry Needling and Pelvic Health.
- Disclaimer: Due to the nature of this course content, it will be delivered in the traditional "in-person" manner. This means the course instructors will be teaching at a single location, and it will not be possible to join the course remotely via video conference. As with all Herman & Wallace courses, this course content is only intended for practitioners who are licensed appropriately, and for whom dry needling is within their scope of practice. It is the responsibility of every course registrant to check with their state boards to ensure that the content of a Herman & Wallace course that they attend is within their state-specific scope of practice.
Interested in women's health? There are 3 new courses appearing this year:
- Perinatal Mental Health: The Role of Pelvic Rehab Therapist - February 5, 2022
- Menopause Transitions and Pelvic Rehab - March 5-6, 2022
- Pregnancy and Postpartum Considerations for High-Intensity Athletics - May 21, 2022
Are you thinking about taking a course, but not sure if it is for you? H&W courses are for licensed practitioners interested in the field of pelvic rehabilitation. The most common registrants that we see in our courses include:
- Doctor of Osteopathic Medicine (DO)
- Doctor of Chiropractic (DC)
- Nurse-Midwives (CNM)
- Nurse Practitioners (ARNP)
- Occupational Therapists (OT)
- Occupational Therapists Assistants (OTA)
- Physical Therapists (PT)
- Physical Therapists Assistants (PTA)
- Doctor of Medicine (MD)
- Physicians Assistants (PA)
- Registered Nurses (RN)
H&W courses are classified as Beginner (no prerequisites), Intermediate (one prerequisite), or Advanced (two or more prerequisites). A Beginner course can be taken by a licensed practitioner without prior coursework requisites. Therapists interested in registering for an Intermediate or Advanced course must review the prerequisites on the course description and honestly assess/report their fulfillment of the published prerequisites.
For example, courses that have Pelvic Floor Level 1 as a prerequisite require a working knowledge of performing internal assessments. It is never recommended that a participant skip this introduction without prior training or experience performing an internal exam. Some courses are part of a series and it is not recommended that they be taken out of order. On the Continuing Education Courses page, you can click the Experience Level tab to see courses organized by level of difficulty.
Clinical experience or alternative coursework may be a substitute for the published course requirements, and it is recommended that a therapist considering opting out of a published prereq review the objectives of the required course and assert that said objectives have been met. Review the Course Overview and Objectives on each course page and ask yourself what your treatment goals (in both the long and short term) are and what patient population you are targeting. All courses list the learning objectives, which will give you a lot of information about what you'll be learning at a given course.
If you would like additional guidance on which course offering best fits your goals and target patient population, please contact us! We are here to guide you into an event that best suits your needs.

In an excerpt from a conversation with The Pelvic Rehab Report, Tara Sullivan discusses her course, Sexual Medicine in Pelvic Rehab. She imparts, "As rehab professionals, we are in a unique position to bridge the gap between disciplines with our extensive time for exams and differential diagnoses. Many causes of dyspareunia, vestibulodynia, and IC-type symptoms can be diagnosed by careful observation and testing of the vestibule. This is often the missing link in resolving the patient's symptoms of burning, itching, urgency, and pain."
Sexual Medicine in Pelvic Rehab covers lecture topics that are often taboo in Western cultures, such as hymen myths, female squirting, G-spot, sexual response cycles, hormone influence on sexual function, anatomy and physiology of pelvic floor muscles in sexual arousal, and orgasm. She also discusses vaginismus, dyspareunia, erectile dysfunction, hard flaccid, prostatitis, and post-prostatectomy issues.
So what is Vestibulodynia? Vestibulodynia is a localized form of vulvodynia. The Baylor College of Medicine defines vestibulodynia as "chronic pain or discomfort that occurs in the area around the opening of the vagina, inside the inner lips of the vulva. This area is known as the vestibule."
Tara Sullivan shares, "The vestibule is considered the forgotten organ. Most disciplines completely bypass it in their exams." So how is vestibulodynia treated, especially if there are no visible symptoms? The patient should discuss their symptoms with their primary practitioner to rule out medical issues such as yeast infection or cancer. Pelvic specialists can perform a physical pelvic exam, with patient consent, to examine the vestibule, vulva, and vagina. A cotton swab touch test can also be used to pinpoint areas of sensitivity.
The treatment strategies for vestibulodynia focus on relieving the pain and discomfort of the patient. These strategies include lifestyle changes (looser clothing, changing personal routines), including the use of lubrication or local anesthetic creams for intercourse, and therapy or sexual counseling. Vestibulodynia patients can be referred to a pelvic rehab therapist to learn how to relax the affected muscles and control painful spasms. This therapy can include the use of diaphragmatic breathing, biofeedback, pelvic wands, or pelvic dilators.
Vestibulodynia is only one of the topics that Tara Sullivan discusses in her course, Sexual Medicine in Pelvic Rehab. Participants will learn how to confidently treat sexual dysfunction related to the pelvic floor, refer to medical providers as needed, and instruct patients in the proper application of self-treatment and diet/lifestyle modifications. 100% of participants surveyed in the last class answered YES to "Do you feel this course instructed immediately-applicable knowledge and skills that could be used in the clinic with patients?"
Sexual Medicine in Pelvic Rehab is scheduled for 2022 on January 8-9, April 9-10, July 16-17, and October 15-16.
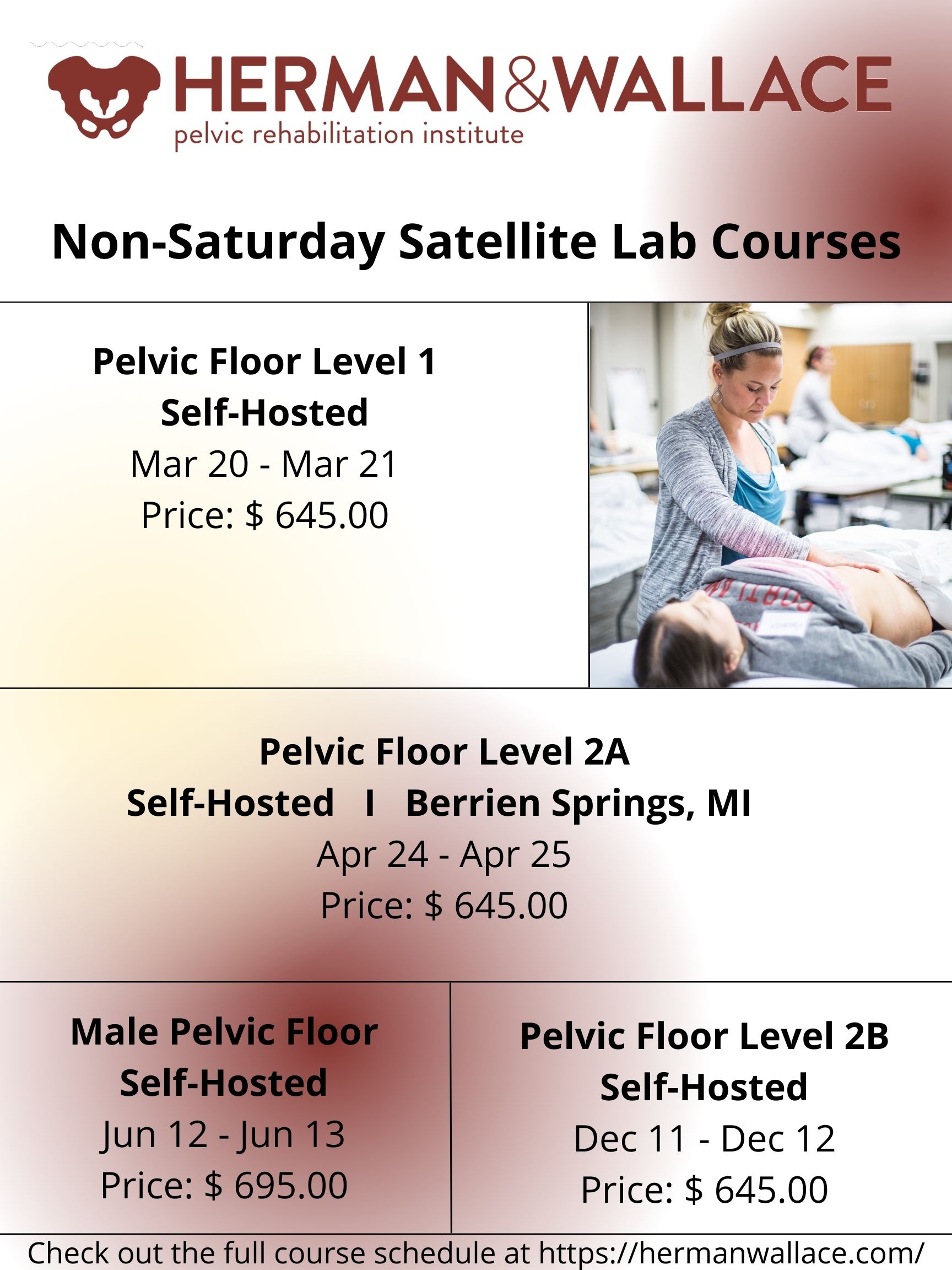
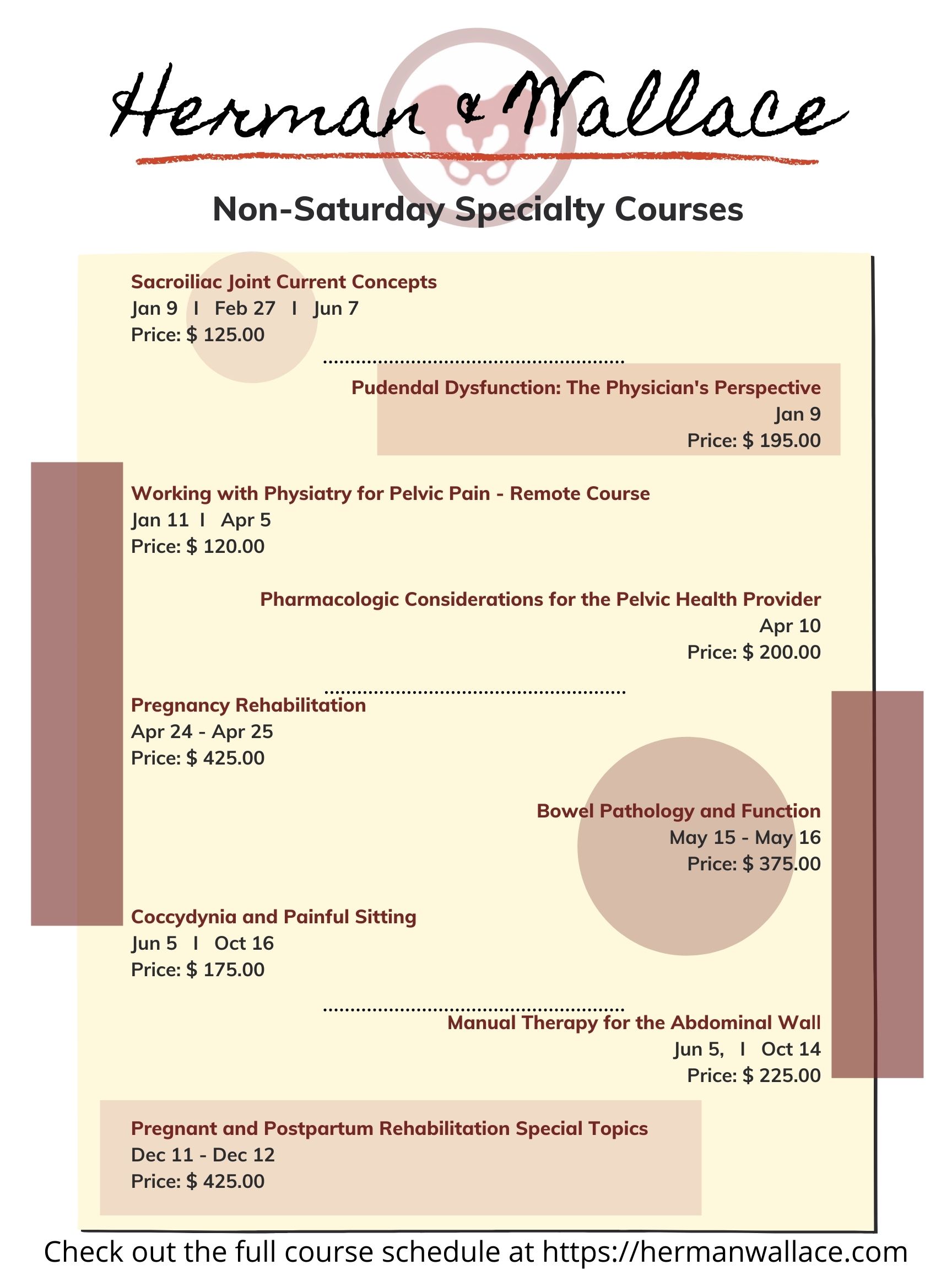
Did you know that Herman & Wallace provides continuing education courses for other weekdays than Saturday?
There is a wide selection of courses that fall on other weekdays. From Pelvic Floor Level 1 scheduled March 20-21, 2022 on Sunday and Monday to our specialty courses such as Working with Physiatry for Pelvic Pain scheduled for Tuesday, January 11, 2022.
Are you interested in attending a satellite lab course, but don't see a satellite available? Do you know a clinic that would be able to host? Feel free to reach out to us through the Host A Course form online.
Generally, H&W is looking for locations to host that have the following:
- Room for about 10-14 therapists to gather (with social distancing)
- Space for folks to sit six feet apart during lecture
- Roughly one lab table for every two participants (5 tables for a 10 person group)
- The following AV equipment:
- LCD projector and table for projector
-
- Laptop with Zoom downloaded - plugs into the projector and plays the instructor teaching live on Zoom
- Projection screen
- Speakers - Bluetooth or plug into the laptop. These do not have to be fancy, but they need to be loud enough that everyone can hear
We look forward to seeing you in one of our courses in the upcoming year!
Dr. Michael Hibner is an international expert on pudendal neuralgia and chronic pelvic pain. Dr. Hibner joins Holly Tanner to discuss his new exclusive course with H&W titled Pudendal Dysfunction: The Physician's Perspective.
Pudendal neuralgia is a painful, neuropathic condition involving the dermatome of the pudendal nerve. This condition is not widely known and often goes unrecognized by many practitioners. Dr. Hibner runs The Arizona Center for Chronic Pelvic Pain (AZCCPP), a comprehensive center for treating chronic pelvic pain, and places a heavy emphasis on working as part of a care team with physical therapists and other pelvic rehab providers.
In this interview Dr. Hibner discusses how he treats pudendal neuralgia, “I treat patients with all reasons for pelvic pain but mostly pudendal neuralgia or patients with mesh injury or had an injury caused by pelvic mesh… I work very closely with physical therapists and I am a great, great believer in physical therapy. I am very happy that you are allowing me to share my perspective on Pudendal Neuralgia, and my perspective on physicians working with physical therapists.”
If I had pudendal neuralgia and I had a choice between surgery, injections, physical therapy, or medication. I would for sure have chosen physical therapy every time…there is no doubt in my mind. You can’t treat the PN without addressing the pelvic floor. What I tell patients is this. The number one thing for repetitive injury is to stop what you’re doing. The number two thing is to choose physical therapy over anything else. By far the majority of patients are helped by appropriate pelvic floor physical therapy.
Pudendal Dysfunction: The Physician's Perspective is scheduled for January 9, 2022. Course topics include pathoanatomy and clinical presentations, basics of surgical techniques, and terminology. The latter half of the course focuses on the physician and the rehab therapist working together and features case studies and clinical pearls from Dr. Hibner, a pioneer, and leader in the field.

This blog includes portions of an interview with Ramona Horton. Ramona serves as the lead therapist for her clinic's pelvic dysfunction program in Medford, OR. Her practice focuses on patients with urological, gynecological, and colorectal issues. Ramona has completed advanced studies in manual therapy with an emphasis on spinal manipulation, and visceral and fascial mobilization. She developed and instructs her visceral and fascial mobilization courses for the Herman & Wallace Pelvic Rehabilitation Institute, and presents frequently at local, national, and international venues on topics relating to women’s health, pelvic floor dysfunction, and manual therapy.
How did you start in pelvic rehabilitation and visceral mobilization?
My PT training was through the Army-Baylor program, I was all in for orthopedics and sports medicine until October of 1990. I gave birth to my second child, an adorable, but behemoth, 9lb 9oz baby boy. His delivery, a VBAC (vaginal birth after cesarean) was very traumatic on my pelvis, I sustained pudendal nerve injury and muscular avulsion. When I queried the attending OB-GYN about my complete lack of bladder control his response and I quote “do a thousand Kegels a day, and when you’re 40 and want a hysterectomy, we’ll fix your bladder then.” As for the desire to study visceral mobilization, that reflects back to my PT training through the US Army which was 30 years ago, when the MPT was just getting started. It was an accelerated program, to say the least. We received a master's in physical therapy with 15 months of schooling. Given the very limited timeline, which included affiliations and thesis, the emphasis in our training was on critical thinking and problem solving, not memorization and protocols which in 1985 was not the norm. I can still hear the words of our instructors “You have to figure it out, I am not going to give you a cookbook."
Following my initial training in the field of pelvic dysfunction in 1993 I started treating patients. I had a problem, I could not wrap my head around how I was to effectively treat bowel and bladder dysfunction…. without treating the bowel and bladder? I knew that there was more to this anatomy than just pelvic floor muscles and the abdominal wall, but at the time that is what was being treated. Once I started learning VM principles and applying the techniques to my patients I saw a vast improvement in my outcomes. I realized that the visceral fascia is a huge missing link in this field and that somewhere along the line the physical therapy community forgot one simple fact. We are not hollow; the visceral structures attach to the somatic frame through ligaments and connective tissue and have an influence on the biomechanics of said frame.
Why is the adoption of visceral mobilization so rare amongst practitioners who aren’t pelvic specialists?
Most likely several reasons, first they do not deal with dysfunctions that have visceral structures involved the way pelvic health therapists do. The second is a paucity of higher levels of evidence on the effectiveness of VM for musculoskeletal conditions. The third and most difficult issue to deal with is the broad-based claims that VM can be an effective treatment for issues ranging from acute trauma to emotional problems. One website called VM “bloodless surgery”. The problem simply is when anyone purports their technique to be a virtual panacea for all that ails mankind, without adequate evidence to back up the claims, the clinical world raises its collective antennae. These critical remarks are coming from a practitioner, published author, and educator in the VM field. The reality of evidence-based medicine is talk is cheap, research is not.
Why do you believe fascial mobilization is such an important aspect of clinical practice?
Most importantly because fascia is ubiquitous, it is EVERYWHERE throughout the body and it contains a vast neurological network to include nociceptors, mechanoreceptors, and proprioceptors just to name a few. The fascia was that stuff that we all dissected out of the way in anatomy lab so we could learn the assigned structures that soon would have a pin with a number stuck in it that we needed to know for a lab practical. We need to move beyond the “myofascia” and understand that the fascial system has multiple layers in the body starting at the panniculus which blends with the skin, the investing fascia surrounding muscles and forming septae, the visceral fascia which is by far the most complex and the deepest layer of fascia, the dura surrounding the central nervous system. All fascial structures, regardless of layer or location have their origin in the mesoderm of early embryologic development.
Ramona Horton's Fascial Mobilization Series 2022 Course Schedule
Mobilization of the Myofascial Layer: Pelvis and Lower Extremity Satellite Lab Course
Mobilization of Visceral Fascia: The Urinary System Satellite Lab Course
Mobilization of Visceral Fascia: The Gastrointestinal System Satellite Lab Course
September 30 - October 2, 2022
Mobilization of Visceral Fascia: The Reproductive System Satellite Lab Course
By accepting you will be accessing a service provided by a third-party external to https://hermanwallace.com/










































