For over 25 years my practice has had a focus on children suffering from bloating, gas, abdominal pain, fecal incontinence and constipation. Functional Gastrointestinal Disorders (FGID) are disorders of the brain -gut interaction causing motility disturbance, visceral hypersensitivity, altered immune function, gut microbiota and CNS processing. (Hyams et al 2016). Did you know that children who experience chronic constipation that do not get treated have a 50% chance of having issues for life?
 The entire GI system is as amazing as it is and complicated. Its connection to the nervous system is fascinating, making it a very sensitive system. In her book GUT, Giulia Enders talks about Ninety percent of the serotonin we need comes from our gut! The psychological ramifications of ignoring the problem are too great (Chase et el 2018). Last year an 18-year-old patient of mine had to decline a scholarship to an Ivy League University because she needed to live at home due to her bowel management problem.
The entire GI system is as amazing as it is and complicated. Its connection to the nervous system is fascinating, making it a very sensitive system. In her book GUT, Giulia Enders talks about Ninety percent of the serotonin we need comes from our gut! The psychological ramifications of ignoring the problem are too great (Chase et el 2018). Last year an 18-year-old patient of mine had to decline a scholarship to an Ivy League University because she needed to live at home due to her bowel management problem.
Unfortunately, FGID conditions can lead to suicide and death. Over 15 years ago my children’s pediatrician told me about an 11-year-old boy who hung himself because he had encopresis. In 2016 a 16-year-old girl suffered a cardiac arrest and died because of constipation.
The problems with children are different than for adults and need to be addressed with a unique approach.
How do physical therapists treat pediatric FGID?
- Have a solid foundation in the gastrointestinal system
- Coordinate muscle functions from top to bottom!
- Identify common childhood patterns
- Learn treatment techniques and strategies to address the issues specifically
Study and understand gastrointestinal anatomy, physiology, function and examination techniques. The entire GI system is as amazing as it is complicated. Its connection to the nervous system is fascinating, making it a very sensitive system. Ninety percent of the serotonin we need comes from our gut! The psychological ramifications of ignoring the problem are too great.
What do the Pelvic Floor Muscles (PFM) have to do with it?
Encopresis leads to a weak internal/external anal sphincter and pelvic floor muscles and constipation leads to pelvic floor muscles that can’t relax. Confused? When the Rectal Anal Inhibitory Reflex or RAIR fails from bypass diarrhea the sphincter muscles relax, and feces leaks out. This constant leakage leads to weak sphincter and pelvic floor muscles. When it happens on a regular basis most children don’t feel it, however their peers smell it and life changes.
My course, Pediatric Functional Gastrointestinal Disorders, teaches how to coordinate the muscle function based on the tasks required.
How did this start?
One painful bowel movement can lead to withholding for the next due to fear of the pain happening again. The muscles of the pelvic floor then tighten to hold the poop in. This actually does not make the muscle strong but instead makes it confused. The muscle then is controlled by the consistency of poop being too hard and painful to let out or too loose and not able to hold in.
Managing functional GI disorders is a process. It takes the bowel a long time to re-train and it requires patience and skill to know how to do it. Many therapists and patients themselves get frustrated and compliance fails. This is mostly due to lack of knowing how to titrate medications and give the bowel what it needs (other than proper nutrition that is!) It's like retraining a person to walk after a stroke, the brain needs to relearn normal bowel sensations.
Most families don’t realize how severe constipation can be. It is an insidious problem that gets ignored until it is too late.
Typically, what I hear from parents is their child was diagnosed with constipation and was advised to take a daily laxative. So, which one is the best one? How do they all work? Once leakage occurs again the laxative is discontinued as we think the bowel must be empty and this medication is causing the leaks which is counterproductive. Now the frustrating cycle of backing up or being constipated begins again. The constipation returns, the laxative is restarted, the loose stool leaks out and the laxative is stopped and that is the REVOLVING DOOR or what I refer to as children riding the “Constipation Carousel”. The bowel is an amazingly beautiful, smart but also sensitive organ that does not like this back and forth and therefore will not learn how to be normal. In the meantime, they experience distended abdomens and dysmorphia ending up in eating disorder clinics. I had an 11-year-old girl taking Amitriptyline for abdominal pain all because of a pressure problem in the gut not knowing how to work the pelvic floor with the diaphragm and her core.
No two children are the same and no two colons are the same. Laxatives need to be titrated to the specific needs of your child’s colon and motility of their colon not their age or body weight.
The success in getting children to have regular bowel movements of normal consistency without any fecal leaks is based not only teaching how to titrate laxatives but also how to sense urge, become aware of the pelvic floor muscles and learn how NOT to strain to defecate, retrain the core and diaphragm with the ribcage and integrate developmental strategies for function. Teaching Interoception- what my body feels like when I have an urge- is an important part of this course. This is especially important for those children born with anorectal malformations or congenital problems such as imperforate anus or Hirschsprung’s Disease.
In this class we use visceral techniques, manual therapy techniques, sensory techniques and neuromuscular reeducation and coordination to retrain the entire system.
Come and explore the amazing gut with me and learn how to improve the health and well-being of your patients, in Pediatric Functional Gastrointestinal Disorders!
1. Hyams, JS, et al. Childhood Functional Gastrointestinal Disorders: Child/Adolescent. Gastroenterology volume 150, 2016;1456-1468.
2. Drossman DA. Functional gastrointestinal disorders: history, pathophysiology, clinical features and rome IV. Gastroenterology 2016;150:1262-1279
3. Robin SG, Keller C, Zwiener R, et al. Prevalence of Pediatric Functional Gastrointestinal Disorders Utilizing the Rome IV Criteria. J Pediatr 2018; 195:134.
4. Koppen IJN, Vriesman MH, Saps M, Rajindrajith S, Shi X, van Etten-Jamaludin FS, Di Lorenzo C, Benninga MA, Tabbers MM. Prevalence of Functional Defecation Disorders in Children: A Systematic Review and Meta-Analysis. J Pediatr. 2018 Jul;198:121-130.e6. doi: 10.1016/j.jpeds.2018.02.029. Epub 2018 Apr 12.
5. Zar-Kessler C, Kuo B, Cole E, Benedix A, Belkind-Gerson, J. Benefit of pelvic floor physical therapy in pediatric patients with dyssynergic defecation constipation. 2019 Dig Dis https://doi.org/10.1159/000500121/
6. Chase J, Bower W, Susan Gibb S. et al. Diagnostic scores, questionnaires, quality of life, and outcome measures in pediatric continence: A review of available tools from the International Children’s Continence Society. J Ped Urol (2018) 14, 98e107
Leeann Taptich DPT, SCS, MTC, CSCS is Co-Author of the new Herman & Wallace offering, Breathing and Diaphragm: Pelvic and Orthopedic Therapist. Leeann leads the Sports Physical Therapy team at Henry Ford Macomb Hospital in Michigan where she mentors a team of therapists. She also works very closely with the pelvic team at the hospital which gives her a very unique perspective of the athlete.
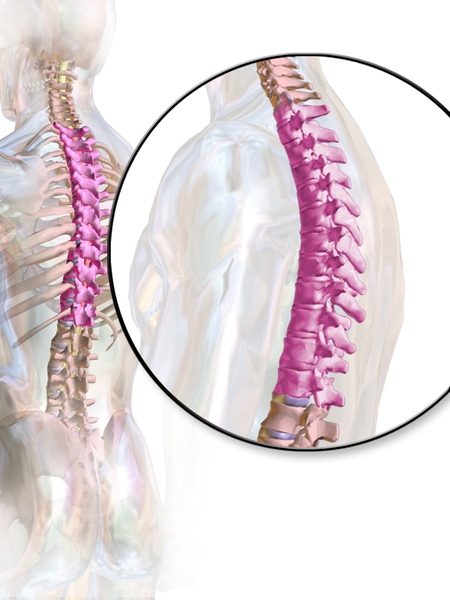 According to a paper from Manual Therapy, the thoracic spine is the least understood part of the spine, despite the huge role it plays in both movement and in regulation of our Autonomic Nervous System.1 Researchers found that the thoracic spine is the least studied of the three spinal regions; thoracic, cervical, and lumbar. I am frequently asked by fellow therapists for help in objectively assessing and treating the thoracic region which has led to the realization that even amongst experienced therapists the thoracic spine’s importance is less understood especially in terms of its function.
According to a paper from Manual Therapy, the thoracic spine is the least understood part of the spine, despite the huge role it plays in both movement and in regulation of our Autonomic Nervous System.1 Researchers found that the thoracic spine is the least studied of the three spinal regions; thoracic, cervical, and lumbar. I am frequently asked by fellow therapists for help in objectively assessing and treating the thoracic region which has led to the realization that even amongst experienced therapists the thoracic spine’s importance is less understood especially in terms of its function.
Anatomically, the thoracic spine along with the ribs and sternum provide a frame that supports and protects the lungs and heart. Despite the rigidity that is required to fulfill that function, the thoracic spine contributes significantly to a person’s ability to rotate.2
One of the biggest roles the thoracic spine plays is in the regulation of the Sympathetic Nervous System, which is a part of the Autonomic Nervous System. The sympathetic nervous system, also known as the “Fight or Flight” system is in overdrive in our patients who present with pain. One of the many complications that arise from an upregulated sympathetic system is increased respiratory rate and/or dysfunctional breathing.3 Carefully applied manual therapy techniques to the thoracic region can help regulate the Autonomic Nervous System by affecting the diaphragm, the intercostals, and other respiratory musculature.4 Specific thoracic mobilizations/manipulations can improve respiratory function.4
In the Breathing and Diaphragm course, Aparna Rajagopal and I discuss the importance of the thoracic spine from both a regional and global perspective. Thoracic spine assessment is taught along with multiple mobilization techniques and manipulations all of which will help the clinician link the thoracic spine to the treatment of pelvic pain, low back pain, and breathing pattern disorders. Join Aparna and I in either Sterling Heights, MI this March or Princeton, NJ in December for Breathing and the Diaphragm: Pelvic and Orthopedic Therapists: From Assessment to Clinical Applications for Pelvic and Orthopedic Therapists!
1. Heneghan NR, Rushton A. Understanding why the thoracic region is the ‘Cinderella’ region of the spine. Man Ther. 2016; 21: 274-276.
2. Narimani M, Arjamand N. Three-dimensional primary and coupled range of motions and movement coordination of the pelvis, lumbar, and thoracic spine in standing posture using inertial tracking device. Journal of Biomechanics. 2018; 69: 169-174.
3. Bernston GG. Stress effects on the body: Nervous system. American Psychological Association. https://www.apa.org/helpcenter/stress/effects-nervous. January 18, 2020.
4. Shin DC, Lee YW. The immediate effects of spinal thoracic manipulation on respiratory functions. Journal of Physical Therapy Science. 2016; 28: 2547-2549.
Mia Fine, MS, LMFT, CST joins the Herman & Wallace faculty in 2020 with her new course on Sexual Interviewing for Pelvic Health Therapists! The new course is launching this April 4-5, 2020 in Seattle, WA; Lecture topics include bio-psycho-social-spiritual interviewing skills, maintaining a patient-centered approach to taking a sexual history, and awareness of potential provider biases that could compromise treatment. Labs will take the form of experiential practice with Bio-Psycho-Social-Spiritual-Sexual Interviewing Skills, case studies and role playing. Check out Mia's interview with The Pelvic Rehab Report, then join her for Sexual Interviewing for Pelvic Health Therapists!
 Tell us about yourself, Mia!
Tell us about yourself, Mia!
My name is Mia Fine, MS, LMFT, CST and I’ve been a Licensed Marriage and Family therapist for four years. I am an AASECT Certified Sex Therapist and my private practice is Mia Fine Therapy, PLLC. I see these kinds of patients: folks with Erectile Dysfunction, Pre-mature Ejaculation, Vaginismus, Dyspareunia, Desire Discrepancy, LGBTQ+, Ethical Non-monogamy, Anxiety, Depression, Trauma, Relational Concerns, Improving Communication.
What can you tell us about the new course?
This course will offer a great deal of current and empirically-founded sex therapy and sex education resources for both the provider as well as the patient. This course will add the extensive skills of interviewing for sexual health. It also offers the provider a new awareness and self-knowledge on his/her/their own blind spots and biases.
How will skills learned at this course allow practitioners to see patients differently?
Human beings are hardwired for connection, intimacy, and pleasure. Our society often tells us that there is something wrong with us, or that we are defective, for wanting a healthy sex life and for addressing our human needs/sexual desires. This course will broaden the provider’s scope of competence in working with patients who experience forms of sexual dysfunction and who hope to live their full sexual lives.
What inspired you to create this course?
This course was inspired by the need for providers who work with pelvic floor concerns to be trained in addressing and discussing sexual health with their patients.
What resources were essential in creating your course?
Becoming a Licensed Marriage and Family Therapist and a Certified Medical Family Therapist requires three years of intensive graduate school. Additionally, a minimum of two years of training to become an AASECT Certified Sex Therapist and hundreds of hours of direct client contact hours, supervision, and consultation. I attend numerous sex therapy trainings and continuing education opportunities on a regular and ongoing basis. I also train incoming sex therapists on current modalities and working with vulnerable client populations.
How do you think these skills will benefit a clinician in their practice?
It is vital that providers working with pelvic floor concerns have the necessary education and training to work with patients on issues of sexual dysfunction. It is also important that providers be aware of their own biases and be introduced to the various sexual health resources available to providers and patients.
What is one important technique taught in your course that everybody should learn?
Role playing sexual health interview questions is an important experience in feeling the discomfort that many providers feel when asking sexual health questions. This offers insight not only into the provider experience but also the patient’s experience of uncomfortability. Role playing this dynamic illustrates the very real experiences that show up in the therapeutic context.
Sexuality is core to most human beings’ identity and daily experiences. When there are concerns relating to our sexual identity, sexual health, and capacity to access our full potential, it affects our quality of life as well as our holistic well-being. Working with folks on issues of sexual health and decreasing sexual dysfunction encourages awareness and encourages healing. Imagining a world where human beings don’t walk around holding shame or traumatic pain is imaging a world of health and happiness.
Pelvic pain is a common diagnosis that we see as pelvic floor therapists. Pelvic pain is pain located in the lower abdomen, but above pubic symphysis, and is associated with various causes; myofascial pain, neuropathies, endometriosis, painful bladder, and irritable bowel syndromes. A common symptom of pelvic pain is deep dyspareunia or pain with deep vaginal penetration. Vulvar pain is different, as it is below pubic symphysis, and has several sub-classifications. These sub-classifications can often be confusing. The National Vulvodynia Association has a free online education that explains the different sub-types very succinctly. This article focuses on provoked vestibulodynia, which is the most commonly studied.
 PVD or Provoked Vestibulodynia often has superficial dyspareunia which can negatively affect sexual functioning, which can lead to changes in psychological function and quality of life. Women with PVD often complain of greater pain during and after intercourse, pain catastrophization, and allodynia when compared to women with superficial dyspareunia but without PVD. These symptoms indicate central nervous system upregulation or sensitivity. This study sought to investigate the impact of these symptoms.
PVD or Provoked Vestibulodynia often has superficial dyspareunia which can negatively affect sexual functioning, which can lead to changes in psychological function and quality of life. Women with PVD often complain of greater pain during and after intercourse, pain catastrophization, and allodynia when compared to women with superficial dyspareunia but without PVD. These symptoms indicate central nervous system upregulation or sensitivity. This study sought to investigate the impact of these symptoms.
Pelvic pain encompassed a variety of complaints: “dysmenorrhea, deep dyspareunia, dyschezia, chronic pelvic pain, back pain, or diagnosed or suspected endometriosis”. Participants were excluded if postmenopausal or if self reported never sexually active.
One hundred twenty nine participants were divided into those with pelvic pain and PVD (43), and those with pelvic pain alone (87). For this study PVD was diagnosed as superficial dyspareunia (>4/10) and positive Q-tip test with a fixed pressure of 30g. Those with did not meet this criteria were considered to have pelvic pain alone.
The two groups were compared for superficial and deep sexual discomfort severity, sexual quality of life; fear avoidance, feelings of guilt, frustration, etc, physical examination of trigger points along abdominal wall (positive Carnett test), and numeric pain scale of various painful lumbo-pelvic regions.
Of the 129 participants notable findings in both the two groups include 31% had confirmed endometriosis, 40% suspected of endometriosis, and in the remaining 18% had no confirmed or suspected endometriosis. The authors found that the pelvic pain + PVD group had significantly more superficial dyspareunia (p=<.001) and deep dyspareunia (p=.001) which was rated >7/10 for both. This group was also had greater (3x more likely to have) depression symptoms, greater anxiety, and catastrophizing, and was more likely to have painful bladder syndrome than the pelvic pain alone group. There were no differences between the two groups for irritable bowel syndrome or abdominal wall tenderness.
This research is consistent with other research findings. The authors explore various causes of the findings including; cross- sensitization - where there may be cross talk of nerve signals from viscera to viscera and viscera to muscular structures that converge in the spinal cord. The authors note that the poor relationship between PVD and irritable bowel and PVD and abdominal wall tenderness limit that theory. They explore the psychological symptoms may be a consequence of pelvic pain or it may be that having anxiety/depression may make women more sensitive to developing pelvic pain and PVD. This sounds like a little chicken or egg theory. The authors suggest that those with PVD and pelvic pain may benefit from a more intensive multi-disciplinary approach including; “medical, surgical, psychological, or physical therapy approaches”.
Bao, C., Noga, H, Allaire, C. et al. “Provoked Vestibulodynia in Women with Pelvic Pain” Sex Med 2019; 1-8
Four years ago, I sat with a tiny nugget in my arms and I stared in awe of this beautiful creature. She was perfect, she was amazing, she was… hungry! And I had no idea what to do.
 Breastfeeding is at the core of our human experience and it is what defines us as mammals. Have you ever stopped to think about the link between mammal, mammary gland, and mama? And yet, for something so natural, it sure can take a lot of work to figure out.
Breastfeeding is at the core of our human experience and it is what defines us as mammals. Have you ever stopped to think about the link between mammal, mammary gland, and mama? And yet, for something so natural, it sure can take a lot of work to figure out.
In advance of the breastfeeding courses for physical therapists in Phoenix and New Jersey this year, I’ve prepared a list of my favourite myths about breastfeeding. Take a look and tag us on social media if any of them surprised you!
Myth #1: Men can’t breastfeed
We’re starting off with one that seems obvious: surely, men can’t produce milk in sufficient quantities to feed an infant. If they could, then couples around the world would split parenting duties very differently. Right?
Well…
Let’s take a deeper dive into this myth. First, it depends on how you define a man. There are trans men who give birth and then feed their infants. There are also gender nonbinary people who don’t give birth and can still lactate. The permutations of unique situations are plentiful. Some refer to this practice as breastfeeding, while others call it chestfeeding. Ask the individual about their preferred terms, just like you would talk about pronouns. For more information on gender and chestfeeding, check out this article1.
An interesting fact about men and lactation is that domperidone – one of the most common medications in breastfeeding medicine – can contribute to male lactation, even when it is being taken for a different indication2. Domperidone elevates the levels of prolactin, a hormone that signals the lactocytes in the breast to produce milk.
Myth #2: An oversupply of milk is always a good thing
If you’ve looked on postpartum Facebook groups and blogs, you’ve likely seen discussions of undersupply, not having enough milk, and the seemingly uphill battle to make more. There are countless forum posts on switch feeding, power pumping, galactalogues (medications and herbs to increase milk production), etc. Perceived insufficient milk consistently appears among the top reasons for supplementation or breastfeeding cessation3,4,5.
When I was pregnant with my daughter, I made plans to exclusively breastfeed her, pump once a day, and donate the extra milk to a local milk bank. Surely, I thought, the only consequence of making extra milk would be the work involved in making the donations. None of this actually happened but that’s a story for another day.
What I’ve come to learn from working with patients is that in the production of milk, any mismatch of supply and demand can impact a person’s quality of life. Signs of oversupply include6:
- Coughing or gagging during feeds
- Baby is fussy at the breast, possibly crying or arching their back
- Baby is gassy between feeds
- The breasts always feel full
- Recurrent breast inflammation such as blocked ducts and mastitis
- Nipple pain and tissue damage from biting
Fast milk flow can also make the task more difficult for babies with an uncoordinated suck/swallow/breathe pattern. If the mechanics or timing is off, the infant will prioritize airway protection and may appear to go on and off the breast throughout the feed.
Myth #3: For a blocked duct, point the baby’s chin toward the affected area
Have you seen it? There’s an image that makes the rounds on social media and it compares the milk-producing components of breast tissue to a flower. This imagery is beautiful, and it sparks conversation every time I see it. If you can’t picture it, think of the milk ducts as the spokes of a bicycle with lobules at the end of each one. They’re neatly arranged in a perfect circle.
 If this is how the ducts are arranged, then the infant’s mandible and tongue will draw milk from the affected area during feeds and that will help to resolve the “blockage.” In reality, though, the ducts do not follow straight paths from lobule to nipple. They wind and weave around each other, branching along the way, and milk that comes out the lateral side of the nipple may have originated in the medial part of the breast7.
If this is how the ducts are arranged, then the infant’s mandible and tongue will draw milk from the affected area during feeds and that will help to resolve the “blockage.” In reality, though, the ducts do not follow straight paths from lobule to nipple. They wind and weave around each other, branching along the way, and milk that comes out the lateral side of the nipple may have originated in the medial part of the breast7.
There’s a second reason why the chin pointing won’t resolve a blocked duct: it turns out that there’s no evidence for the existence of a blockage in the first place. We often picture a blocked duct like a coronary artery, with an obstruction that is preventing the flow of milk (or blood) through the vessel. In reality, the ducts are easily collapsible7 and localized inflammation8 and swelling can compress the ducts, preventing milk flow.
Myth #4: Mastitis means infection
Our last myth is perhaps the most pervasive of the list. Many people – including physicians – think that the difference between mastitis and blocked ducts is that mastitis involves a pathogen or infection. Depending on where you live, it may be common practice to prescribe antibiotics for all cases of mastitis.
According to the Academy of Breastfeeding Medicine and the World Health Organization, infection is only one of the causes of the condition8,9. Mastitis is defined as inflammation of the breast, which may be infectious or non-infectious in nature. Non-infectious cases can be attributed to mechanical factors such as distension of the breast alveoli and/or chemical factors like pro-inflammatory cytokines entering the parenchyma8.
What this means is that there are many cases of mastitis that can benefit from someone who can help with inflammation management. To me, that sounds like a physical therapist. We have a role to play not only in the local tissue, but also in the biopsychosocial approach that’s required in addressing a person’s pain.
Learn more aboutevidence-based management principles for breastfeeding conditions at the Herman & Wallace course Breastfeeding Conditions: Mastitis, Nipple Pain, and Maternal Factors in Lactation, taking place this year in Phoenix, AZ this March and Princeton, NJ this August. I look forward to discussing these topics and more!
1. MacDonald, T. (2018). Transgender parents and chest/breastfeeding. Retrieved from https://kellymom.com/bf/got-milk/transgender-parents-chestbreastfeeding/
2. Sanis Health Inc. (2015). Domperidone product monograph [PDF file]. Retrieved fromhttps://pdf.hres.ca/dpd_pm/00030125.PDF
3. Li, R., Fein, S. B., Chen, J., & Grummer-Strawn, L. M. (2008). Why mothers stop breastfeeding: mothers’ self-reported reasons for stopping during the first year. Pediatrics, 122(Supp. 2), S69-S76.
4. Gatti, L. (2008). Maternal perceptions of insufficient milk supply in breastfeeding. Journal of Nursing Scholarship, 40(4), 355-363.
5. Ahluwalia, I. B., Morrow, B., & Hsia, J. (2005). Why do women stop breastfeeding? Findings from the Pregnancy Risk Assessment and Monitoring System. Pediatrics, 116(6), 1408–1412.
6. La Leche League International (n.d.). Oversupply. Retrieved from https://www.llli.org/breastfeeding-info/oversupply
7. Ramsay, D. T., Kent, J. C., Hartmann, R. A., & Hartmann, P. E. (2005). Anatomy of the lactating human breast redefined with ultrasound imaging. Journal of anatomy, 206(6), 525-534.
8. World Health Organization. (2000). Mastitis: causes and management (No. WHO/FCH/CAH/00.13). World Health Organization.
9. Academy of Breastfeeding Medicine Protocol Committee. (2008). ABM clinical protocol# 4: mastitis. Breastfeeding Medicine, 3(3), 177-180.
If you work with orthopedic patients, I am sure that you have had a back-pain patient that you have discharged, only for them to return a year later suffering from another episode of pain. We all know that once someone suffers from a back injury, they are more likely to develop a chronic issue. Even patients with insidious back pain and no specific injury often develop chronic issues and can have pain that waxes and wanes after the initial episode.
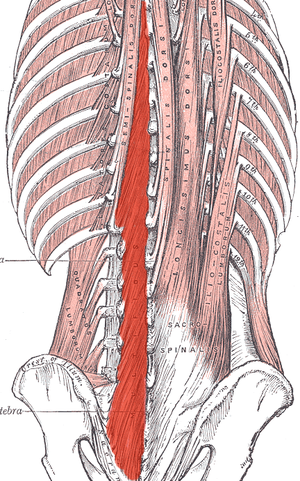 What happens in the body to cause this? Most of us have learned that the pelvic floor, transverse abdominus, and the deep fibers of the lumbar multifidus play an important role in stabilization. With injury, these muscles can become less effective in stabilizing the spine and pelvis. Studies have shown that muscle atrophy in the lumbar multifidus has been shown to occur with injuries and persist after resolution of the pain.1
What happens in the body to cause this? Most of us have learned that the pelvic floor, transverse abdominus, and the deep fibers of the lumbar multifidus play an important role in stabilization. With injury, these muscles can become less effective in stabilizing the spine and pelvis. Studies have shown that muscle atrophy in the lumbar multifidus has been shown to occur with injuries and persist after resolution of the pain.1
I recently did additional research to find out other reasons that cause these local stabilizing muscles to not function optimally. I found that these muscles also can suffer from arthrogenic muscle inhibition after an episode of low back pain.2 Arthogenic inhibition is a deficit in neural activation to a muscle. It is thought to occur due to a change in the discharge of articular sensory receptors due to swelling, inflammation, joint laxity, and damage to afferent nerves.2 EMG studies have shown reduced neural activity in the deeper fibers of the multifidus in patients with back pain.3
Another thing that fascinated me was that cortical changes in the brain also occur with low back pain. Changes in cortical representation of the multifidus and the body’s ability to voluntarily activate the muscle has been noted.4 Motor retraining has been shown to reorganize the motor cortex with regards to the transverse abdominus.5 Also, improvement in brain organization and function occurs after resolution of back pain.6
This is good news for patients! As therapists, we may not be able to do anything with respects to arthogenic inhibition. However, we can work on motor retraining for the core muscles. It has been shown that specific training that targets the multifidus can restore the neural activity to the multifidus and lead to improvement of pain and function.7,8 Training the multifidus can be difficult for therapists to teach. However, studies have found that ultrasound guided biofeedback is helpful for patients to learn to contract their multifidus.9,10
Come learn more about the multifidus and how it relates to back pain and stability. In Rehabilitative Ultrasound Imaging: Women's Health and Orthopedic Topics we will go over how to help your patients learn to activate and strengthen their multifidus. Join me on February 28 - March 1st in Raleigh, NC to learn new ways to help your patients!
1. Hides JA, Richardson CA, Jull GA. Multifidus muscle recovery is not automatic after resolution of acute, first‐episode low back pain. Spine 1996;21:2763–2769.
2. Russo M, Deckers K, Eldabe S, et al. Muscle control and non-specific chronic low back pain. Neuromodulation: Technology at the neural interface. 2018; 21 (1): 1-9.
3. D'Hooge R, Hodges P, Tsao H, Hall L, Macdonald D, Danneels L. Altered trunk muscle coordination during rapid trunk flexion in people in remission of recurrent low back pain. J Electromyogr Kinesiol 2013;23:173–181
4. Massé‐Alarie H, Beaulieu L‐D, Preuss R, Schneider C. Corticomotor control of lumbar multifidus muscles is impaired in chronic low back pain: concurrent evidence from ultrasound imaging and double‐pulse transcranial magnetic stimulation. Exp Brain Res 2015; 234:1033–1045.
5. Tsao H, Galea MP, Hodges PW. Driving plasticity in the motor cortex in recurrent low back pain. Eur J Pain 2010;14:832–839.
6. Seminowicz DA, Wideman TH, Naso L et al. Effective treatment of chronic low back pain in humans reverses abnormal brain anatomy and function. J Neurosci 2011;31:7540–7550
7. França FR, Burke TN, Caffaro RR, Ramos LA, Marques AP. Effects of muscular stretching and segmental stabilization on functional disability and pain in patients with chronic low back pain: a randomized, controlled trial. J Manipulative Physiol Ther 2012;35:279–285.
8. Goldby LJ, Moore AP, Doust J, Trew ME. A randomized controlled trial investigating the efficiency of musculoskeletal physiotherapy on chronic low back disorder. Spine. 2006;31:1083–1093.
9. Ghamkhar L, Emami M, Mohseni‐Bandpei MA, Behtash H. Application of rehabilitative ultrasound in the assessment of low back pain: a literature review. J Bodyw Mov Ther 2011;15:465–477.
10. Van K, Hides JA, Richardson CA. The use of real‐time ultrasound imaging for biofeedback of lumbar multifidus muscle contraction in healthy subjects. J Orthop Sports Phys Ther 2006;36:920–925
Herman & Wallace is excited to announce an upcoming course on pelvic rehab for the gender diverse patient, written and instructed by Dr. Laura Meihofer, DPT, ATC. As Dr. Meihofer indicated in a recent blog, "[t]he number of individuals who identify as transgender is growing each year. The Williams Institute estimated in 2016 that 0.6% of the U.S. population or roughly 1.4 million people identified as transgender (Flores, 2016)... With the rise of individuals who identify as transgender, gender non-binary and intersex, healthcare professionals have equally seen an influx of patients who require care throughout their discovery and transition."
The new course from Dr. Meihofer is called "Gender Diversity and Pelvic Health: Comprehensive Care for Transgender Men and Women", and it will be debuting on May 29-31, 2020 in Livingston, NJ.
Dr. Meihofer was kind enough to share some thoughts about the new course, her practice, and herself with The Pelvic Rehab Report. Thank you, Laura!
Tell us about yourself, Laura!
My name is Laura Meihofer and I’ve been a physical therapist for 7 years. I work at Mayo Clinic and I see patients throughout the gender spectrum who most commonly struggle with pelvic floor dysfunctions relating to overactive muscles such as: chronic and acute pelvic pain, urinary frequency/urgency/incontinence/hesitancy, constipation, pain with intercourse, low back and hip pain.
 What can you tell us about your new course, "Gender Diversity and Pelvic Health"?
What can you tell us about your new course, "Gender Diversity and Pelvic Health"?
Currently there are roughly 1.25 million transgender identified individuals in the United States and this number is growing. This course will help to dispel the idea of “other” when treating this demographic and demonstrate how much sameness there is when treating pelvic floor dysfunction.
These skills will greatly benefit any practice as this population is so underserved, they are looking for allies that are not just nice but competent. When you are able to successfully treat gender diverse patients, they spread the word about the great care they received and you now have a strong referral base. Taking this course opens up a whole new referral base of amazing people.
This course will not only feature videos from thought leaders in the field but will also highlight testimonials from patients and caregivers who have undergone their own gender transitions.
What essential skills does your course add to a practitioner’s toolkit?
I think the most important technique that attendees will learn will be how to assess a trans women and trans man after they have undergoing genital reconstruction surgery. Attendees will gain competence in the care of the gender diverse patient at any stage during their gender transition.
What was your inspiration to create this course for trans-identified patients?
Working at a major medical institution, I found that it was difficult finding providers in a patient’s area that were competent in care of a transgender patient. As I talked more and more with various physical therapists I realized they were thirsty for knowledge on how to serve these individuals. So I created the course!
What prepared you to create this course?
The most important thing I have done for this course is treat hundreds of patients who are trans identified throughout their gender journey. This allowed me to not only see all the medical interventions they went through but also to hear their personal journey of transition. These experiences expanded my empathy for what they go through and inspired me to search within myself on how I can be better for them. This desire to improve opened a creative well inside of me from which this course grew.
Discuss the effect conditions covered in your course have on a patient’s quality of life, your experience treating patients with this condition, and how their quality of life has increase after successful treatment.
Individuals who identify as transgender suffer from pelvic floor dysfunction just like our cis gender folks. There is no current data to capture the prevalence of pelvic floor issues in this specific population to date, however there is research to support the overall lack of care these individuals receive. Based on the results from the U.S. Transgender Survey which surveyed 28,000 respondents, the numbers in the health care field were staggering.
33% of respondents had at LEAST one negative experience with a health care provider in the last year due to being transgender. Negative experiences were qualified as verbal harassment, refusal of treatment or having to teach the health care provider about transgender people to receive appropriate care. 23% of respondents did not see a doctor when they needed to due to fear of being mistreated as a transgender person.
This course aims has two primary aims:
1) Educate providers on the unique concerns that transgender individuals experience related to hormone replacement and surgical techniques.
2) Equip attendees to provide competent care for this demographic
Join Dr. Meihofer for Gender Diversity and Pelvic Health this May 29-31, 2020 in Livingston, NJ!
Earlier this year, Herman & Wallace sponsored the first ever pelvic rehab course for physios in Nairobi, Kenya in partnership with The Jackson Clinics Foundation. After returning from that course, Kathy Golic, PT spent months writing a new course, adapting information from Pelvic Floor Level 1, Level 2A, and the Pregnancy and Postpartum series. This October, Kathy (along with co-instructors Casie Danenhauer and Sherine Aubert) returned to teach her follow-up course that expanded on the first module, introducing lectures and labs tailored to the community of pelvic physios in Kenya. This dispatch comes from instructor Kathy Golic, PT, who sent in this article shortly after returning from the course. Huge thanks to Kathy and her colleagues Sherine Aubert and Casie Danenhauer for doing this important work!
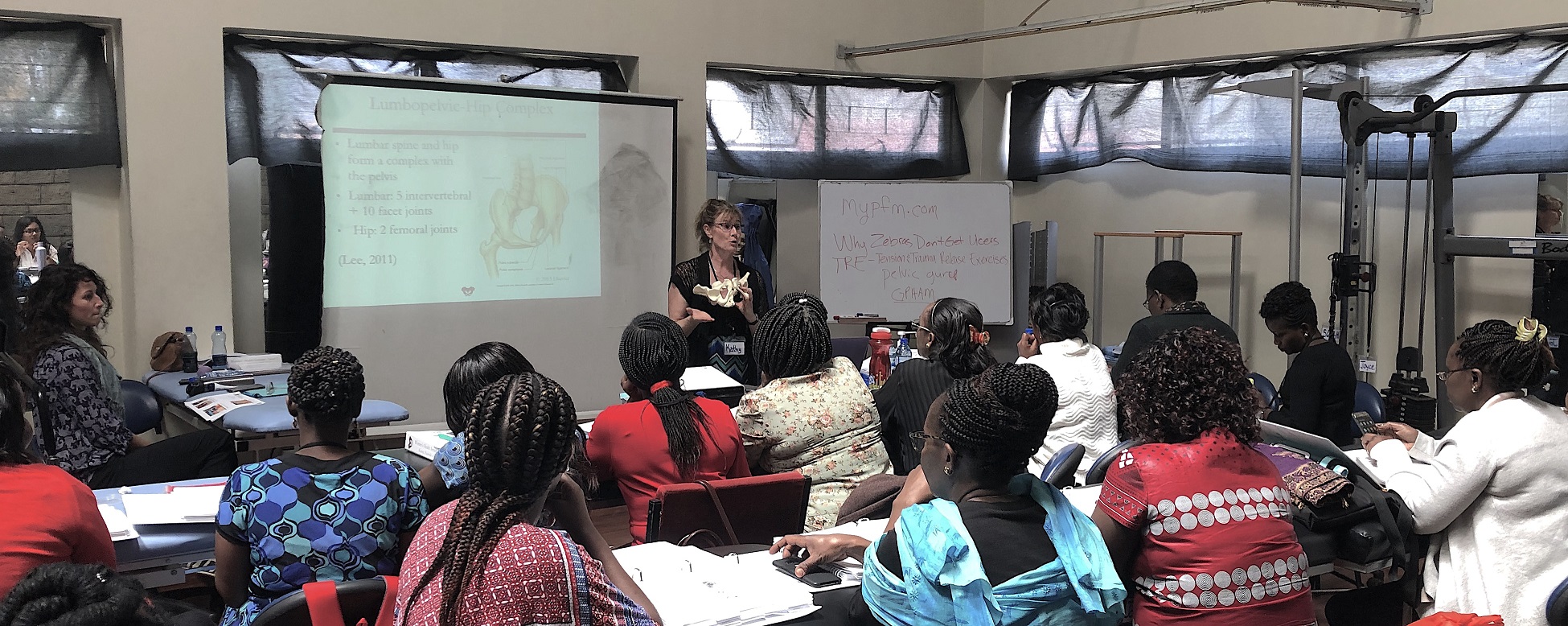 It has been a week now, and as I type looking out on the windy rainy day, it is hard to believe that I was so recently in a warm, sheltered classroom sequestered from the hustle and bustle of Nairobi. A place which has captured my heart. Really it is the people, especially my new “sisters” who I spent so much time with during this last two-week course module. Once again, I experienced chill bumps every day from witnessing the growth, the stories, the wisdom and the compassion of these bright, motivated, committed physiotherapists who came back for the 2nd module in our series to help them become experts in the field of Pelvic Health. This module covered topics of Pregnancy, Postpartum care, Prolapse, Colorectal Conditions including fecal incontinence and constipation, and Coccydynia. We had a terrific printed course manual for this 2nd in the series, thanks to the partnership of Herman and Wallace and Jackson Clinics Foundation. With my wonderful and resourceful, skilled colleagues from LA, Casie Danenhaur, and Sherine Aubert, we included comprehensive lectures, lively demonstrations, hands on creative experiential learning opportunities, and awesome supervised lab training sessions. We also had a lot of case study discussions, and live case studies where we assisted the students, who are practicing physiotherapists, in conducting thorough assessments and clinical reasoning processes to treat and make plans to further the progress of their patients.
It has been a week now, and as I type looking out on the windy rainy day, it is hard to believe that I was so recently in a warm, sheltered classroom sequestered from the hustle and bustle of Nairobi. A place which has captured my heart. Really it is the people, especially my new “sisters” who I spent so much time with during this last two-week course module. Once again, I experienced chill bumps every day from witnessing the growth, the stories, the wisdom and the compassion of these bright, motivated, committed physiotherapists who came back for the 2nd module in our series to help them become experts in the field of Pelvic Health. This module covered topics of Pregnancy, Postpartum care, Prolapse, Colorectal Conditions including fecal incontinence and constipation, and Coccydynia. We had a terrific printed course manual for this 2nd in the series, thanks to the partnership of Herman and Wallace and Jackson Clinics Foundation. With my wonderful and resourceful, skilled colleagues from LA, Casie Danenhaur, and Sherine Aubert, we included comprehensive lectures, lively demonstrations, hands on creative experiential learning opportunities, and awesome supervised lab training sessions. We also had a lot of case study discussions, and live case studies where we assisted the students, who are practicing physiotherapists, in conducting thorough assessments and clinical reasoning processes to treat and make plans to further the progress of their patients.
 All of this in itself was incredibly rewarding. But there was more. The power of sacrifice we witnessed. The power of solidarity and true generosity. Most of these women continued to have to work after class even while in this two-week module; in class from 8-4, but then going on their way, some of them through heavy Nairobi traffic, to treat patients in their offices, or to work hospital shifts. One student heading out after a Wed. afternoon class told me that she was going to work from 7- midnight, then would sleep until 4am, then back to work until 7 am, before returning to class at 8 am. She also had to miss one class to participate in her mentorship for her ortho advanced diploma, so had to make up a test with us the next day. (she aced the test!) Now for the generosity. I will share just 1 of many stories. One of the physios asked a patient of hers whom she felt she could use some help with, if she would mind traveling to the KMTC classroom where we were teaching so the other students could learn, while we the visiting instructors, would help guide in her assessment and care. This woman agreed, and got up at 3:30 am, traveled by bus for 3 hours to come for her treatment. She willingly shared her story, and it was tough to hear. She worked as a vegetable vendor carrying produce on her back, lifting it, and sitting on a stone for hours each day. She, a mother of 5 grown children with an unemployed husband. Her physio and the class did quite well in their assessment and with treatment and suggestions. She seemed pleased. Then as she prepared to leave, some of the physio students “passed the hat” and collected 7,000 kshillings (about $70.00) and presented this humble lady with the money so that she could afford transportation home. It is my understanding that most Kenyans spend 50% of their income on food, so sharing with this patient was a true sacrifice. But for these ladies, there was no question about it. This is how they live and how they work. They are themselves so grateful for the knowledge, skills and experience that they are getting through this program, and they will pay it backwards and forwards. My colleagues this time and last time, are also indebted to them for all they have taught us. It is truly an honor and privilege to be part of this great program, and I too am thankful for all the team players in this venture.
All of this in itself was incredibly rewarding. But there was more. The power of sacrifice we witnessed. The power of solidarity and true generosity. Most of these women continued to have to work after class even while in this two-week module; in class from 8-4, but then going on their way, some of them through heavy Nairobi traffic, to treat patients in their offices, or to work hospital shifts. One student heading out after a Wed. afternoon class told me that she was going to work from 7- midnight, then would sleep until 4am, then back to work until 7 am, before returning to class at 8 am. She also had to miss one class to participate in her mentorship for her ortho advanced diploma, so had to make up a test with us the next day. (she aced the test!) Now for the generosity. I will share just 1 of many stories. One of the physios asked a patient of hers whom she felt she could use some help with, if she would mind traveling to the KMTC classroom where we were teaching so the other students could learn, while we the visiting instructors, would help guide in her assessment and care. This woman agreed, and got up at 3:30 am, traveled by bus for 3 hours to come for her treatment. She willingly shared her story, and it was tough to hear. She worked as a vegetable vendor carrying produce on her back, lifting it, and sitting on a stone for hours each day. She, a mother of 5 grown children with an unemployed husband. Her physio and the class did quite well in their assessment and with treatment and suggestions. She seemed pleased. Then as she prepared to leave, some of the physio students “passed the hat” and collected 7,000 kshillings (about $70.00) and presented this humble lady with the money so that she could afford transportation home. It is my understanding that most Kenyans spend 50% of their income on food, so sharing with this patient was a true sacrifice. But for these ladies, there was no question about it. This is how they live and how they work. They are themselves so grateful for the knowledge, skills and experience that they are getting through this program, and they will pay it backwards and forwards. My colleagues this time and last time, are also indebted to them for all they have taught us. It is truly an honor and privilege to be part of this great program, and I too am thankful for all the team players in this venture.

Pelvic pain can often involve adverse neural tension. The hip and pelvic nerves wrap around like spaghetti, making diagnosis and treatment difficult. Is the pain driver boney, capsular, muscle or neurovascular? Luckily, impingement and labral tears are fairly easy to diagnosis. Nerve entrapment can be a little bit tricky to diagnosis and treat. Part of being a good pelvic floor physical therapist is appropriately diagnosing and then partnering with patients to treat symptoms, pain, and movement dysfunction.
 The authors of this study focused on hip, so this blog focuses on sciatic and pudendal nerve entrapment in the athletic population. Nerve entrapment occurs when the normal slide and glide is limited. That can be from any structure in the pelvis and hip region that cause strain or compression on the nerves in the area. Often patient’s descriptions of pain can be the first sign with complaints of ‘burning’, ‘sharp’, or changes in sensation. Evaluation for changes in reflexes and motor function are helpful. Other signs of nerve entrapment are tenderness to palpation and reproduction of pain with movements that elongate the nerve. Medical management to confirm diagnosis include nerve blocks, and diagnostic imaging, and nerve conduction velocity tests.
The authors of this study focused on hip, so this blog focuses on sciatic and pudendal nerve entrapment in the athletic population. Nerve entrapment occurs when the normal slide and glide is limited. That can be from any structure in the pelvis and hip region that cause strain or compression on the nerves in the area. Often patient’s descriptions of pain can be the first sign with complaints of ‘burning’, ‘sharp’, or changes in sensation. Evaluation for changes in reflexes and motor function are helpful. Other signs of nerve entrapment are tenderness to palpation and reproduction of pain with movements that elongate the nerve. Medical management to confirm diagnosis include nerve blocks, and diagnostic imaging, and nerve conduction velocity tests.
Specific locations of pain can help determine where the nerve is being squished. The sciatic nerve (L4-S3) can be entrapped as it passes between the piriformis and deep hip rotators. This often presents with a history of trauma to the gluteal area and limited sitting tolerance (>30 minutes). As the sciatic nerve moves down it can have ischiofemoral impingement, when the nerve gets compressed between lateral ischial tuberosity and greater trochanter at level of quadratus femoris muscle. This will often present as pain during mid- to terminal-stance during walking. Then, once the sciatic nerve clears the pelvis it can become entrapped by the proximal hamstring. There can be hamstring trauma in the history, and possible partial avulsion or thickening of the hamstring may entrap the sciatic nerve.
The pudendal nerve (S2-S4) can become entrapped in several areas and symptoms often include pain medial to the ischium and can include genital regions for all genders, perineum, and peri-rectal regions. The most common areas consist of the space between the posterior pelvic ligaments (sacrospinous and sacrotuberous) and the obturator internus muscle. History often includes bike riding, and a common complaint is pain with sitting, except a toilet seat.
Differential diagnosis for posterior nerves physical examination can include the following tests:
Sciatic Nerve
- Seated palpation: where the clinician palpates the subgluteal space (between sacrum and deep hip rotators), ischial tuberosity and hamstring attachment, and in the area medial to ischial.
- Seated piriformis stretch - involved lower extremity is adducted and internally rotated while palpating posterior hip region.
- Active piriformis - resisted lateral abduction and external rotation while palpating posterior hip region.
- Ischiofemoral impingement: the involved is placed in extension with adduction and external rotation
- Active knee flexion: this test is done seated with knee at 30° and 90° flexion. Clinician palpates ischial canal while providing knee flexion resistance for 5 seconds in both positions.
Pudendal Nerve 
- Palpation around sciatic notch, region medial ischium
- Internal palpation for obturator internus tenderness
- Internal palpation of alcocks canal
Consertative treatment including physical therapy can be helpful. Manual therapy including nerve glides and soft tissue mobilization. Nerve mobilizations require anatomical nerve pathway knowledge. Mobilizing the nerves is thought to improve blood flow within and around the nerve, decrease adhesions, and also may affect central sensitivity. Soft tissue mobilization is geared towards positively affecting scar tissue and encouraging movement that may be restricting neural movement.
Therapeutic exercises for strengthening and stretching are also helpful, however use caution to avoid aggressive stretching as it may aggravate nerves. Exercises to promote load transfer through the pelvis and lower extremities can be helpful. The authors also suggest lower extremity passive PNF (proprioceptive neurofacilitation) diagonal movements. The authors also suggest aerobic conditioning, cognitive behavioral therapy, and for the chronic pelvic pain population, pelvic floor muscle training that does not provoke symptoms.
When conservative treatment including injections produces limited results, surgical treatments are often the next step. Often surgeries where the nerves are decompressed, neurolysis, or removed, neurectomy can be helpful.
To learn more nerve assessment and treatment techniques, join Nari Clemons, PT, PRPC in her course Sacral Nerve Manual Assessment and Treatment in Tampa, FL this December 6-8, 2019!
Martin R, Martin HD1, Kivlan BR 2.Nerve Entrapment In The Hip Region: Current Concepts Review.Int J Sports Phys Ther. 2017 Dec;12(7):1163-1173.
Aparna Rajagopal, PT, MHS is the lead therapist at Henry Ford Macomb Hospital's pelvic dysfunction program, where she treats pelvic rehab patients and consults with the sports therapy team. Her interests in treating peripartum patients and athletes allowed her to recognize the role that breathing plays in pelvic dysfunction. She has just joined the Herman & Wallace faculty and co-authored the new course, "Breathing and the Diaphragm: Pelvic and Orthopedic Therapists", which helps clinicians understand breathing mechanics and their relationship to the pelvic floor.
Aparna was kind enough to introduce herself to us here on The Pelvic Rehab Report.
 Thank you for your time Aparna! To start, tell us a little bit about yourself.
Thank you for your time Aparna! To start, tell us a little bit about yourself.
My name is Aparna. I’ve been a physical therapist for 22 years. About 16 years ago I switched focus from orthopedics to treating pregnancy and postpartum patients and that’s where my initial interest in pelvic care started. In 2006 following my pregnancy and birth of my daughter, my interest in pelvic care grew with my special interest becoming pelvic pain.
I teach and mentor the pelvic health therapists within the fairly large hospital system that I work at and collaborate with our spine center team and our sports team.
What can you tell us about this new breathing course that is not mentioned in the “course description” and “objectives” that are posted online?
Physical therapy has evolved and continues to evolve as we speak. Regional inter dependence, wherein the different systems interplay, and one structure influences another, is fascinating. No longer is the body considered and treated as independent fragmented pieces. The ‘core’ with the contribution of the Diaphragm and the pelvic floor is so much more than just the Transverse Abdominis and the Multifidus working together. Fascial restrictions of the lower abdomen and the pelvis can influence how the low back feels, thoracic stiffness can influence the interplay between the various abdominal muscles by way on their insertion into the lower ribs, musculo- skeletal pain and postural deviations can stem from incorrect breathing patterns etc.
Normal breathing rate is about 10 times every minute. Breathing incorrectly reinforces wrong movement patterns tens of thousand times a day with negative consequences on the musculoskeletal system.
This course offers an in depth look at the diaphragm from the perspective of both orthopedic and pelvic therapists and attempts to tie in the diaphragm to the thoracic spine, the ribs, the pelvic floor, the core, posture and finally the athlete.
What essential skills does the breath course add to a practitioner’s toolkit?
The practitioner will walk away with the ability to view the patient as a “whole”. It offers a different perspective on neck and back pain, posture/ alignment along with the ability to assess for and connect breathing and the diaphragm to stability/ the core, continence issues and the Autonomic Nervous System.
As therapists we already do a great job of addressing strength issues, assessing and correcting posture, mobilizing etc. You can add to your treatment options by learning how the diaphragm works in concert with other muscles (especially the abdominals) and systems, identifying breathing pattern dysfunctions and postures, and movement patterns which may be linked to breathing pattern dysfunctions. This understanding is beneficial for both orthopedic and pelvic patients.
What inspired you to create this course? What void does this new offering fill?
I have used breathing and evaluation of the diaphragm as a part of pelvic care for several years now. As the mentor for the pelvic program at my hospital, and as a part of the spine team and sports team, I work with pelvic therapists, orthopedic therapists, manual certified therapists, and sports certified therapists. Through my interactions I have come to realize that although many of the therapists are aware that the Diaphragm and breathing are important, they are unsure of how to assess for dysfunctions and address those dysfunctions. I initially started conducting classes within the hospital system. At the same time Leeann who is a sports certified therapist and holds a manual therapy certificate and I started collaborating on our patients. Using a combination of her knowledge and effective manual techniques with my pelvic care and breathing techniques we realized that along with my pelvic patients; our back and neck patients, and her sports patients were all benefitting from this combined approach. We realized along the way that we had information worth sharing with our colleagues that would benefit them in treating their patients, and started classes within the hospital system and that is how this class was born!
What was your process like creating this course?
As a trained pelvic therapist, I have incorporated and used breath and the diaphragm in my treatment for over a decade. Leeann and I have created this course using a combination of our clinical experiences, our education in our respective chosen paths of patient care, and most importantly using recent and relevant research articles from journals to guide us extensively in creating this course.
Breathing and the Diaphragm: Pelvic and Orthopedic Therapists is a new course being offered next March 27-29, 2020 in Sterling Heights, MI, and again on December 11-13, 2020 in Princeton, NJ. It is created and taught by Aparna Rajagopal, PT, MHS and Leeann Taptich, PT, DPT. Come learn how the diaphragm and breathing can affect core and postural stability through intra-abdominal pressure changes. As an integrated approach, the course looks at structures from the glottis and the cervical region to the pelvic floor and helps in understanding a multi component system that works together.
By accepting you will be accessing a service provided by a third-party external to https://hermanwallace.com/










































