Do you work with osteoporosis patients? This may be a trick question because you probably do whether you know it or not- even if you are a pediatric therapist! Osteoporosis is defined by the World Health Organization1 as a systematic skeletal disease characterized by:
- Low bone mass
- Micro-architectural deterioration of bone tissue
- Consequent increase in bone fragility and susceptibility to a fracture
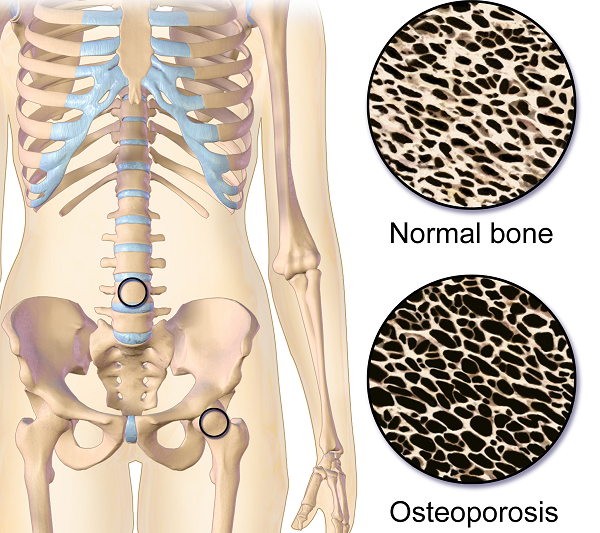 Osteoporosis occurs in men, women and even children. It is sometimes called the “silent disease” because often people don’t know they have it until they break a bone. And even then, compression fractures are painful only 20-30% of the time. Old fractures are often found on x-rays when a person is imaged for illnesses such as pneumonia. According to the National Osteoporosis Foundation2, about one in two women and one in four men over the age of 50 will suffer a fracture due to bone fragility. At this point in time, it is estimated 80% of patients entering Emergency Departments with a fragility fracture (a fall from a standing height) are never followed up for care.
Osteoporosis occurs in men, women and even children. It is sometimes called the “silent disease” because often people don’t know they have it until they break a bone. And even then, compression fractures are painful only 20-30% of the time. Old fractures are often found on x-rays when a person is imaged for illnesses such as pneumonia. According to the National Osteoporosis Foundation2, about one in two women and one in four men over the age of 50 will suffer a fracture due to bone fragility. At this point in time, it is estimated 80% of patients entering Emergency Departments with a fragility fracture (a fall from a standing height) are never followed up for care.
As therapists, we see patients for a variety of diagnoses with co-morbidities but osteoporosis may not be listed. This could be because they have never been identified. We are in a prime position to screen for signs associated with the disorder. Below are the top 3 signs to look for:
- History of fracture from minimal trauma (fall from a standing height, sneeze, lifting groceries, etc.) The typical fracture areas are wrist, hip, and spine although fragility fractures can happen anywhere in the body.
- Hyper-kyphosis. Note, I said hyper-kyphosis, not kyphosis. We are meant to have a thoracic kyphosis but an excessive curve, particularly when it hinges around T8 area may indicate a collapse of the anterior portion of the vertebral bodies. This is the pie shaped wedging seen on x-rays and further increases the stress on the anterior aspect of the spine. Observe your patients’ sagittal posture for proper alignment.
- Loss of height. Ask your patient their tallest height remembered; then measure them. A loss of 4 cm (1.5 inches) or more may indicate fractures in the spine.
Remember pain may or may not accompany a compression fracture. Patients may complain of a “catch” or muscle spasm or nothing at all. These quick and simple screens can alert the healthcare provider and may help prevent further disintegration of the bones. Research is showing that not only weight bearing exercises but a site specific back and hip strengthening program decreases the risk of fracture.3
1. World Health Organization. www.who.int
2. National Osteoporosis Foundation. www.nof.org
3. Current Osteoporosis Reports. Sept, 2010. The Role of Exercise in the Treatment of Osteoporosis. Sinaki M, Pfeifer M, Preisinger E, Itoi E, Rissoli R, Boonen S, Geusens P, Minne HW.
Part 3: Carefully Choosing to Say Yes or No (or The Summer that Almost Wasn’t)
*Disclaimer: this essay is meant to be read in a voice of complete transparency and humility.
 Two summers ago I was anxiously anticipating a break. I was wrapping up home school for my girls and had scheduled some down time from writing my contribution to “Boundaries, Meditation and Self-Care” when I got the call…
Two summers ago I was anxiously anticipating a break. I was wrapping up home school for my girls and had scheduled some down time from writing my contribution to “Boundaries, Meditation and Self-Care” when I got the call…
Rewind a bit. Two years prior I also got a call. Would I be interested in writing a chapter in a Urology textbook on alternative care for pelvic pain conditions…edited by and partnering with a big name in pelvic floor rehab? Oh yes indeed I would! I have always dreamed of seeing my name in print. Was I scared out of my mind? Heck yes! I was working 20 hours a week, part time home schooling my girls and teaching for Herman & Wallace. I had one day a week to myself for cleaning, errands, the occasional book reading or interacting with friends. I decided I could spend my next year of Fridays researching, writing and editing said chapter. Oh, I also started therapy for the anxiety increase that came with the project. My therapist suggested I hire help with house cleaning, which I did. She also suggested meditation, mindfulness and using essential oils. I opted not to enact these suggestions. It was a crazy year, but I learned a ton and was proud of my contribution to the publication.
In the brief time that I caught my breath from the book chapter, I was invited to be part of the team writing the Pelvic Floor Capstone course. What an honor! I had always wanted to try writing a course and this would be a perfect opportunity to collaborate with others on such a big project. I committed, worsening my anxiety with heart palpitations which escalated to a level that required medication. My Fridays and evenings were again occupied for quite some time. Luckily, I still had the cleaning help and the therapist which were really just the skinniest strings that were maintaining my sanity.
While teaching our first Capstone class, although both of us were struggling with burnout, Nari Clemons and I had a moment of euphoria, seeing everything come together and watching students learn. We decided we would design and write another course and put together an outline and a plan for Boundaries, Self-Care and Meditation.
I think you might be getting a picture of my prior lifestyle. If there was time, I filled it. If there was an opportunity, I took it. If I did something once, I could do it again. But applying the concepts of our boundaries course to myself changed everything.
Nari and I knew we were burning out and needed change. I have always had anxiety, but it had escalated to the point of requiring both therapy and medication. I was giving my all, my best, to everyone else and my family got my scrappy leftovers, the worse of me. I had been functioning in these patterns my whole life and had no idea how to get off the hamster wheel.
As we developed Boundaries, Meditation and Self Care I became my own research study, incorporating the material we would be teaching into my own life. I finally started setting priorities and boundaries that helped put my family first and give them the best of me. I said no to a variety of opportunities that I then delegated to colleagues who were delighted to step up. I started meditating, practicing mindfulness and using essential oils as part of my self-care as my therapist suggested a year ago. I even enrolled my kids in full time school for the upcoming year. I was feeling so much better!
So when the next call came, I was prepared.
The editor and famous pelvic floor PT I had worked with on the book chapter was in need of an editor for an article that was going to be published in a medical journal. There was a lot of editing that needed to be done and time was of the essence. My contribution as editor would list me as a co-author. How many of you also dream of seeing your name attached to an article in a peer reviewed medical journal? Because of what I had learned through therapy and practiced with meditation I had the ability to pause, reflect, and make an informed choice that considered how this opportunity lined up with my priorities. I replied with much gratitude for the offer, but this time I said no. It was difficult to say no, and I had to work through some regret, but in the end I made the right choice and we had a great summer.
Life is funny sometimes and lessons in humility are plentiful. Back track again to when the urology text came out a few years ago. I excitedly ordered a print copy. When I opened to the chapter which I contributed, I discovered another person’s name had accidently been printed where mine should have been. The mistake was corrected for the ebooks but more paper copies were not printed. I may never see my name in print, but the Summer That Almost Wasn’t taught me that there are more important things in life.
If you find yourself struggling with boundaries, saying no, and prioritizing the things that are important to you personally and as a therapist, know that you are not alone, and you can get support. Consider talking with your supervisor, a counselor, reading a good book on the subject or taking Boundaries, Meditation and Self Care, a course offering through Herman and Wallace that was designed to help pelvic health professionals stay healthy and inspired while equipping therapists with new tools to share with their patients.
We hope you will join us for Boundaries, Meditation and Self Care this November 9-11, 2019 in San Diego, CA.
Childbirth fear is associated with lower labor pain tolerance and worse postpartum adjustment.1,2 In addition, psychological distress during pregnancy is associated with adverse consequences in offspring, including detrimental birth outcomes, long-term defects in cognitive development, behavioral problems during childhood and high levels of stress-related hormones.3 These negative consequences of fear and stress during pregnancy have inspired both interest and research into the role of mindfulness training during pregnancy to reduce fear and stress and improve outcomes.
In a randomized controlled trial, first-time mothers in the late 3rd trimester of pregnancy were randomized to attend either a 2.5-day mindfulness-based childbirth preparation course offered as a weekend workshop or a standard childbirth preparation course with no mind-body focus.4 Participants completed self-report assessments pre-intervention, post-intervention, and post-birth, and medical record data were collected. Compared to standard childbirth education, those in the mindfulness-based workshop showed greater childbirth self-efficacy and mindful body awareness, reduced pain catastrophizing and lower post-course depression symptoms that were maintained through postpartum follow-up. Participants in the mindfulness workshop also demonstrated a trend toward a lower rate of opioid analgesia use in labor.
In a qualitative study, researchers conducted in-depth interviews at four to six months postpartum with ten mothers at increased risk of perinatal stress, anxiety and depression and six fathers who had participated in a Mindfulness Based Childbirth and Parenting Program (MBCP).5 The MBCP program integrates mindfulness training into childbirth education. Participants meet for eight 2 hour and 15 minute weekly sessions and a reunion after babies are born. Specific mindfulness practices introduced include body scan, mindful movement, sitting meditation and walking meditation. Also, methods to integrate mindfulness into pain management, parenting and activities of daily living are introduced. Participants are asked to practice at home for 30 min per day in between sessions supported by audio guided instructions and informative texts.
Participants in the MBCP Program described gaining new skills for coping with stress, anxiety and pain, as well as developing insight and self-compassion and improving communication. Participants attributed these improvements to an increased ability to focus and gain a wider perspective as well as adopt attitudes of curiosity, non-judging and acceptance. In addition, they described mindfulness training to be helpful for coping with childbirth and parenting, including breastfeeding troubles, sleep deprivation and stressful moments with the baby.
These findings demonstrate potential therapeutic outcomes of integrating mindfulness training into childbirth preparation. Although this is a young field and more research is warranted, there is substantial research demonstrating mindfulness training improves stress management, pain management and decreases physiological markers of stress in a wide range of patient populations.6, 7 While the interventions in the above two studies introduce mindfulness in a group format, I have also found that patients can greatly benefit from being taught mindful principles and practices in one-on-one treatment sessions.
Carolyn will share her over-30 years of training and experience teaching mindfulness to patients both individually and in group settings in her course, Mindfulness-Based Pain Treatment, coming up on October 26 and 27 in Houston, TX. Participants will return to the clinic with skills to not only help patients, but to also help themselves be less stressed, more mindful providers!
1. Alehagen S, Wijma K, Wijma B. Fear during labor. Acta Obstet Gynecol Scand. 2001;80(4): 315–320.
2. Laursen M, Johansen C, Hedegaard M. Fear of childbirth and risk for birth complications in nulliparous women in the Danish national birth cohort. Br J Obstet Gynaecol. 2009:116(10): 1350–1355.
3. Isgut M, Smith AK, Reimann. The impact of psychological distress during pregnancy on the developing fetus: Biological mechanisms and potential benefits of mindfulness interventions. J Perinat Med. 2017 Dec 20;45(9):999-1011.
4. Duncan LG, Cohn MA, Chao MT. The benefits of preparing for childbirth with mindfulness training: a randomized controlled trial with an active comparison. BMC Pregnancy Childbirth. 2017. May 12;17(1):140.
5. Lonnberg G, Nissen E, Niemi M. What is learned from Mindfulness-Based Childbirth and Parenting Education? – Participants’ experiences. BMC Pregnancy Childbirth. 2018; 18: 466.
6. Hilton L, Hempel S, Ewing BA, et al. Mindfulness meditation for chronic pain: Systematic review and meta-analysis. Ann Behav Med. 2017;51(2):199-213.
7. Pascoe MC, Thompson DR, Jenkins ZM, Ski CF. Mindfulness mediates the physiological markers of stress: Systematic review and meta-analysis. J Psychiatr Res. 2017;95:156-78.
Often pelvic floor therapists see men for post-prostatectomy urinary leakage. However, at least for me, that quickly led to seeing male patients for pelvic pain and sexual dysfunction. Male sexual dysfunction is a broad category and can consist of erectile dysfunction (ED), ejaculation disorders including premature ejaculation (PE), and low libido -- often there is a pelvic floor muscle (PFM) dysfunction component. Conservative treatment frequently consists of pharmacological and lifestyle changes for this population.
In normal sexual function, the male superficial pelvic floor musculature (bulbocavernosus and ischiocavernosus) work together to create increased intracavernosus pressure by limiting venous return, resulting in an erection. Ejaculation is created by rhythmic contractions of the bulbocavernosus muscle.
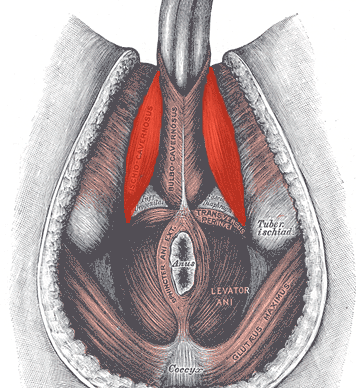 The authors of this systematic review were curious if pelvic floor muscle training was effective for treating erectile dysfunction and premature ejaculation diagnoses, and if so to determine whether there is a treatment protocol. Ten studies were found that met the inclusion criteria, five that focused on ED and five that focused on PE. In total, there were 668 participants ranging in age from 30-59 years old. Studies were excluded if participants were post-prostatectomy and/or had a neurological diagnosis. The intervention was a pelvic floor program, and pelvic floor muscle contractions were either taught or supervised. Studies also included supportive treatment including biofeedback, lifestyle changes, and electrical stimulation.
The authors of this systematic review were curious if pelvic floor muscle training was effective for treating erectile dysfunction and premature ejaculation diagnoses, and if so to determine whether there is a treatment protocol. Ten studies were found that met the inclusion criteria, five that focused on ED and five that focused on PE. In total, there were 668 participants ranging in age from 30-59 years old. Studies were excluded if participants were post-prostatectomy and/or had a neurological diagnosis. The intervention was a pelvic floor program, and pelvic floor muscle contractions were either taught or supervised. Studies also included supportive treatment including biofeedback, lifestyle changes, and electrical stimulation.
The studies focused on erectile dysfunction listed a combination of hormonal, psychogenic, arteriogenic, and venogenic causes. The pelvic floor training ranged from 5-20 visits over 3-4 months and included a home exercise program. Pelvic floor training was similar in all studies and consisted of maximal quick contractions over one second and submaximal endurance holds over 6-10 seconds. Compliance to home exercise program was not assessed. Between 35% and 47% of participants reported a full resolution of symptoms. Subjective improvements were supported by improved maximal anal pressure and intracavernosus pressure. One study used the International Index of Erectile Function (IIEF) and showed significant improvement (p<0.05).
The studies focused on premature ejaculation noted participants had either lifelong or secondary PE. The pelvic floor training in these studies ranged from 12-20 sessions over 1-3 months. All studies used electrical stimulation as part of the pelvic floor muscle training. Four studies also used biofeedback. Only one study listed a home exercise program but did not report on compliance. The pelvic floor muscle training was compared to nothing in three studies, and to a selective serotonin reuptake inhibitor (SSRI) in the other two studies. Patient reported full resolution of symptoms was 55-83% in two studies, and there was a significant improvement in delay in heterosexual penetrative ejaculation (p<0.05) in three studies.
For both erectile dysfunction and premature ejaculation, pelvic floor muscle exercise prescription was 2-3 times per week with pelvic floor muscle contractions both maximal quick contractions and submaximal endurance holds. Significant results were shown with participants who were taught pelvic floor muscle contractions through a combination of verbal and physical means (typically biofeedback). Specific verbal cues were not reported. The authors suggest that electrical stimulation was helpful for training recruitment patterns; however, there was not a significant difference in outcomes for those with ED when using electrical stimulation. The authors suggest that pelvic floor muscle training can be part of a conservative treatment. It may be used with oral pharmacology for quick results, and may be beneficial with electrical stimulation and biofeedback, though more research is indicated.
If you are interested in learning more about treating male patients, consider attending Male Pelvic Floor: Function, Dysfunction, and Treatment!
Myers, C., Smith, M. “Pelvic floor muscle training improves erectile dysfunction and premature ejaculation: a systematic review” Physiotherapy 105 (2019) 235–243
As more and more patients seek care for pelvic floor dysfunction, the need for more qualified practitioners is becoming apparent. Many patients prefer to see a clinician who they identify with, which is why it is important for practitioners of all genders to learn to treat pelvic floor dysfunction. Because much of the public's awareness of pelvic rehab comes out of women's health, the vast majority of pelvic health practitioners are women.
There is currently a shortage of male pelvic health practitioners. To help us understand why it is so important to fix that, we reached out to several male clinicians who have attended the Male Pelvic Floor: Function, Dysfunction, and Treatment course to ask them about the need for more men in the field. Here are some answers to the question:
“Why is it important to have male providers available to treat male patients in the field of pelvic health?”
Grant Headley of Bridgetown Physical Therapy of Portland, Oregon (www.bridgetownpt.com)
While as PT’s we all approach our patients with interest in helping them as individuals, some of our patients feel more comfortable sharing certain details with a provider of the same gender. Many of the hang-ups some men have about receiving care from a female provider are related to an older generation, to certain traditional or religious cultural beliefs, or to certain beliefs about propriety related to receiving care.
As acknowledged in our coursework, generally men have cultural barriers that traditionally do not permit sharing of vulnerability or weakness, especially in the sexual domain. Here are a few unsolicited statements I feel encapsulate what my own male patients have told me: Some heterosexual men feel more comfortable sharing the details of their dysfunction with a man because they find it difficult to admit vulnerability in the presence of a female. Some men prefer not to relay the clinically pertinent details of dysfunctional sexual encounters with a female because they do not wish to make the female practitioner uncomfortable. Many men feel that they can relay more detail about the mechanics of the sexual dysfunction or signs of improvement to a male provider. Some men have told me that they felt their sexual dysfunction was minimized or that they have been treated with patronizing language by a female pelvic PT in the past. Unfortunately, these patients attribute this negative experience to the PT being female, and they are not comfortable having a second opinion with a female.
 Although we strive to present as open-minded and neutral to our patients, they may have an affinity for a male provider. This could foster a more constructive clinical partnership towards working on their goals if they perceive fewer communication barriers. I can offer my own experience as a past patient suffering with pelvic floor dysfunction; I was so desperate for help and I felt so grateful that there was a physical therapist in my city at all that was willing to help me. I did not care that she was female and that I had to receive treatment at a women's health clinic for new mothers in the University Hospital. Many female therapists reading this article have likely transferred lifesaving PT care to scores of men. This organization of H&W that does so much good for a sensitive aspect of men's care is dominated by women- this needs to be acknowledged as a net positive but also appreciated that much of the education and application of care is an adaptation from what has worked for women in the past. Many men will be so grateful to receive care and get better. Some men unfortunately will have barriers to receiving care and for those patients, we can seek out and encourage our male colleagues to get involved in pelvic rehab so we can all provide more access to care.
Although we strive to present as open-minded and neutral to our patients, they may have an affinity for a male provider. This could foster a more constructive clinical partnership towards working on their goals if they perceive fewer communication barriers. I can offer my own experience as a past patient suffering with pelvic floor dysfunction; I was so desperate for help and I felt so grateful that there was a physical therapist in my city at all that was willing to help me. I did not care that she was female and that I had to receive treatment at a women's health clinic for new mothers in the University Hospital. Many female therapists reading this article have likely transferred lifesaving PT care to scores of men. This organization of H&W that does so much good for a sensitive aspect of men's care is dominated by women- this needs to be acknowledged as a net positive but also appreciated that much of the education and application of care is an adaptation from what has worked for women in the past. Many men will be so grateful to receive care and get better. Some men unfortunately will have barriers to receiving care and for those patients, we can seek out and encourage our male colleagues to get involved in pelvic rehab so we can all provide more access to care.
Lance Frank of Flex Physical Therapy in Atlanta (www.flexptatl.com)
Personally, as a male provider in pelvic health, I find that the men I treat are much more comfortable and at ease discussing topics like erections (or lack thereof) and sexual dysfunction, as well as incontinence, or pelvic pain. In a female dominated sub-specialty of physical therapy, sometimes as a male it can be intimidating and even embarrassing for some men to discuss these topics at all, let alone with a female; so having the option to speak and be treated by another male who may better understand the changes, anatomy, and problems they’re experiencing may feel a bit less daunting. Our culture has made male masculinity fragile and I think some populations of men who need pelvic floor rehab may feel embarrassed to be treated by a female clinician if their perception of being seen by a female is emasculating. Ultimately, I think there needs to be more men in this field because there needs to be better visibility of male pelvic health providers in general, as well as better representation of men acknowledging that male pelvic floor disorders exist and are willing and able to treat them.
Eddie Gordon of Flow Rehab in Seattle (www.flowrehab.com)
There are far fewer male physiotherapists treating men with pelvic floor dysfunctions, but I am hopeful this will change for the better. Lack of access to male pelvic physios is a relative barrier to care because some men are more comfortable seeing a male pelvic provider the same way most women would prefer seeing a female pelvic physio. In general, men do not typically seek treatment as frequently or early enough the way most women do. If male pelvic physios are not available, then men may more likely delay treatment, which could potentially worsen their problem. Ironically, when it comes to men with pelvic floor dysfunctions, men are underrepresented, but I am hopeful that more male PT’s will be joining the movement to educate the male population.
Milan Patel of Comprehensive Therapy Services in San Diego (comprehensivetherapy.com)
I believe it's important to have male providers in the pelvic health field for many reasons, one being the opportunity for connection. I think we connect best with reflections of ourselves and for men seeking out a pelvic health provider that can be hard to find. In my experience, pelvic physical therapy works best when your patient can be open and honest, and establishing a strong connection between therapist and patient is the first step. Another reason is that people should have options for the provider they want. In San Diego I am the only male pelvic physical therapy provider which means most men seeking pelvic floor therapy have no choice but to see a female. If you switched the genders in the last sentence you could see how that is problematic. Many women prefer to have their pelvic PT be a female, I just think guys should get the same choice.
Steven Lavender of The Physical Therapy Practice NYC in New York (thephysicaltherapypractice.nyc)
In my experience as a gay male practitioner practicing pelvic floor physio on only men:
Gay male patients usually prefer a gay provider because they feel like they don’t have to explain lifestyle issues and choices, they may be unused to being touched by women, and maybe misogynistic.
Some straight men have told me that they think a male practitioner would know more about their pelvic issues than a woman. Some men don’t think women are strong enough nor have long enough fingers to get to the places they need to be. Some straight men report they might be attracted to a female therapist and get an erection or feel embarrassed about appearing unmanly with their particular pelvic condition.
For some men being touched by a woman is a religious issue so many males of the Jewish and Muslim faiths prefer to see a male practitioner.
Some men could not care less who sees them as long as they get better.
One woman called me for advice or for an appointment from some distance because they "figured a gay man in New York City just might know more about my ass and ass pain than any local jack-assed doctor in my neck of the woods." True story.
If you are interested in learning to treat male patients, the Male Pelvic Floor: Function, Dysfunction, and Treatment course is a great place to start! The course is taking place twice more in 2019, this September 13-15, 2019 in Pasadena, CA, and again in Fort Myers, FL on October 19-21, 2019. We are already booked four times in 2020 as well, so be sure to check out the full course schedule for all available dates.
I recently found this article from the Psychology Research and Behavior Management Journal. I found myself curious about how other healthcare disciplines treat a diagnosis that often presents in conjunction with pelvic floor dysfunction. Irritable bowel syndrome, or IBS, affects nearly 35 million Americans. It is considered a ‘functional’ condition meaning that symptoms occur without structural or biochemical pathology. There is often a stigma with functional diagnosis that the symptoms are “all in their heads”, and while there are many theories about what predisposes individuals to IBS, the experts now think of IBS as a “disorder of gut brain interaction”. Generally, there are 3 subtypes of IBS where people note either constipation dominant, diarrhea dominant or mixed. In order to be diagnosed an individual must report abdominal pain at least 1 day per week in the last 3 months which is related to stooling and a change in frequency or form. Other symptoms that are common are bloating, nausea, incomplete emptying, and urgency.
The author suggests a biopsychosocial framework to help understand IBS. An interdependent relationship between biology (gut microbiota, inflammation, genes), behavior (symptom avoidance, behaviors), cognitive processes (“brain-gut dysregulation, visceral anxiety, coping skills”), and environment (trauma, stress). The brain-gut connection by a variety of nerve pathways is how the brain and gut communicate in either direction; top down or bottom up. Stress and trauma can dysregulate gut function and can contribute to IBS symptoms.
Stress affects the autonomic nervous system that contributes to sympathetic (fight/flight) and parasympathetic (rest/digest). Patients with IBS may have dysfunction with autonomic nervous system regulation. Symptoms of dysregulated gut function can present as visceral hypersensitivity, visceral sensitivity, and visceral anxiety. Visceral hypersensitivity is explained as an upregulation of nerve pathways. The author sites studies that note that IBS patients have a lower pain tolerance to rectal balloon distention than healthy controls. Visceral sensitivity is another sign of upregulation where IBS patients have a greater emotional arousal to visceral stimulation and are less able to downregulate pain. The author notes that the IBS population show particular patterns of anxiety with visceral anxiety and catastrophizing. Visceral anxiety is described hypervigilance to bowel movements and fear avoidance of situational symptoms. For example, fear of not knowing where the bathroom is located.
Cognitive behavioral therapy (CBT) has been shown to be an effective treatment to decrease the impact of IBS symptoms. CBT is focused on modifying behaviors and challenging dysfunctional beliefs. CBT can be presented in a variety of ways, however most include techniques consisting of education of how behaviors and physiology interplay for example the gut and stress response; relaxation strategies, usually diaphragmatic breathing and progressive relaxation; cognitive restructuring to help individuals see the relationship between thought patterns and stress responses; problem-solving skills with shift to emotion focused strategies (“acceptance, diaphragmatic breathing, cognitive restructuring, exercise, social support”) instead of problem focused strategies, and finally exposure techniques to help the individual slowly face fear avoidance behaviors. So much of the techniques are similar to what pelvic floor therapists try to educate our patients in. It is reassuring to me that through we may be different disciplines we are on the same team are moving towards the same goal. The author recommends a 10 session treatment duration, and notes that may be a barrier for some. Integrated practice with other healthcare professionals is also recommended. The more we can know about what our other team members are doing to help support patients the more effective we all are.
Kinsinger, Sarah W. “Cognitive-behavioral therapy for patients with irritable bowel syndrome: current insights” Psychology research and behavior management vol. 10 231-237. 19 Jul. 2017, doi:10.2147/PRBM. S120817
Ultrasound imaging is being used more frequently in the physical therapy clinical setting. Physical therapists are using ultrasound (US) imaging in varying ways. Some are using it as a training tool for the patient to learn neuromuscular control. Others are using it to guide needle placement while performing dry needling. In a recent article authored by several well-known physiotherapists, the various uses of US imaging were defined, as well as discussions regarding the scope of practice, and training for physiotherapists using ultrasound imaging.
 Four uses of US imaging have been reported by physical therapists. The first and most common use of US imaging is the evaluation of muscle structure and function to aid in neuromuscular control. Essentially, the US images are being used as a source of biofeedback. This has been coined Rehabilitative Ultrasound Imaging (RUSI). Additional uses have emerged in recent years including Diagnostic US imaging which is the diagnosis and monitoring of pathology; and interventional US imaging which is using the US images to guide percutaneous procedures involving dry or wet needling. These three categories are performed during clinical care and fall under the umbrella term “point of care ultrasound.” The last category of US imaging use in physical therapy is paired with performing research.
Four uses of US imaging have been reported by physical therapists. The first and most common use of US imaging is the evaluation of muscle structure and function to aid in neuromuscular control. Essentially, the US images are being used as a source of biofeedback. This has been coined Rehabilitative Ultrasound Imaging (RUSI). Additional uses have emerged in recent years including Diagnostic US imaging which is the diagnosis and monitoring of pathology; and interventional US imaging which is using the US images to guide percutaneous procedures involving dry or wet needling. These three categories are performed during clinical care and fall under the umbrella term “point of care ultrasound.” The last category of US imaging use in physical therapy is paired with performing research.
In this article, some thoughts and areas for improvement were brought to light regarding each type of US imaging as well as the scope of practice and training for each type of US use. It was mentioned that RUSI sits almost entirely within the scope of the physical therapy profession, however, it can be difficult for therapists to receive training for this use. Therapists interested in learning diagnostic or interventional US imaging have more options for training because these uses of US have established criteria for training, competence, and regulation outlined by the World Health Organization (WHO), as well as oversight from the World Federation for Ultrasound in Medicine and Biology. These programs often are intended for other healthcare practitioners (radiologists, and sonographers), but physical therapists are able to take the courses. However, it was stated that both diagnostic and interventional US imaging do not fall within the scope of practice for a majority of physical therapists around the world. So, although training may be more available for these types of US use; therapists taking these courses gain increased experience with non-physical therapy applications, and therefore are at risk for operating outside the scope of their practice.
The authors continued with distinct recommendations for needed training for the four different types of US imaging. Several of the listed skills were fundamental knowledge that a therapist should obtain before utilizing any of the four types of US into their practice such as basic physics for US, terminology, safety, among other knowledge. Then there were skills that were specific to the particular type of US being performed. Since point-of-care use of US is generally not included as part of entry level physical therapy education programs, this knowledge needs to be obtained in a postgraduate education format. For therapists who wish to learn diagnostic application of US imaging, there are multiple courses available from schools that train sonographers. However, according to this article, the form of US imaging that sits more within the scope of practice for physical therapists, rehabilitative ultrasound imaging, does not have as many educational opportunities as diagnostic US imaging does.
Herman & Wallace offers a course that provides fundamental skills of US imaging (such as history, and knowledge of the physics needed for US imaging), as well as specific skills for real-time ultrasound imaging. The schedule of the course includes a lot of lab time with multiple US units available so the ratio of participant to US unit low. You will leave the course being able to interpret US images and use it as an assessment tool or biofeedback tool for the patient. Using RUSI will change how you treat patients! The Rehabilitative Ultrasound Imaging course is offered three more times this year. Join me in Columbia, MO this August; Madison, WI in September; or Chicago, IL in December to learn how to use this form of ultrasound imaging in your clinical practice!
Whittaker J, Ellis R, Hodges P, et al. Imaging with ultrasound in physical therapy: what is the PT’s scope of practice a competency-based educational model and training recommendations. Br. J Sports Med. Apr. 2019; 0:1-7.
“However, at present we are all aglow with views on visceral anatomy and medical colleges are wisely establishing chairs in this department which will result in much advancement.” -Fred Byron Robinson, 1891 (Cysts of the Urachus)
The above (fabulous) quote reminds us that many came before us who were equally excited by the study of anatomy. One anatomical structure that I know never appeared in my graduate anatomy courses is the urachus. The urachus is a structure that extends from the urinary bladder to the umbilicus (highlighted blue in the image). When investigating literature about this structure I was impressed to find publications about the urachus dating from the late 19th century.
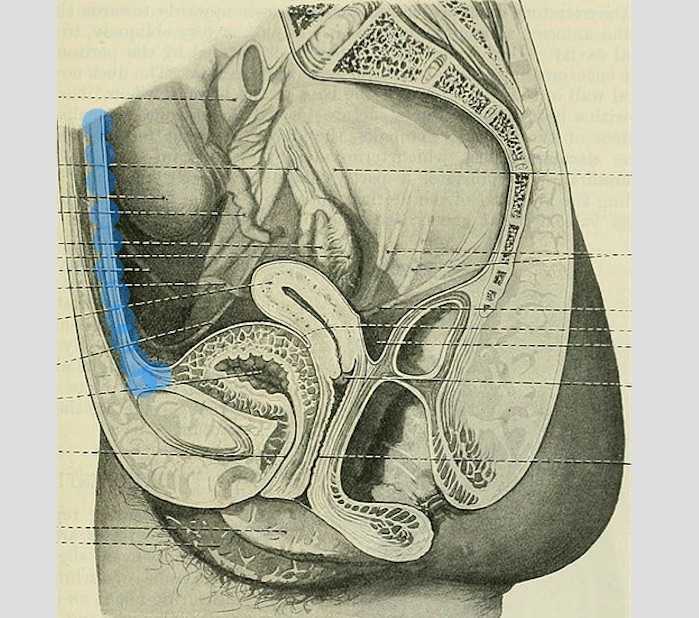
It wasn’t until several years into my career as a physical therapist that I learned about the urachus, a structure attached to the bladder, and learned how this structure could create some rather dramatic symptoms when in dysfunction. I met a woman who was in her early 30’s and who had 6 months prior undergone a laparoscopic surgery with access just below the umbilicus. She presented to rehabilitation after seeing an urologist for severe pain that occurred towards the end of voiding. The pain was absent at any other time, but was so severe towards the latter half of emptying her bladder that she would double over in pain and “nearly pass out.” Investigation revealed a healthy, well-functioning pelvic floor and abdominal wall, but a reproduction of her severe pain with palpation to the midline between the umbilicus and the pubic bone. After grabbing some anatomy texts, I supposed that the urachus, having potentially been irritated by the laparoscopic approach, might experience a tensioning of the irritated tissue as the bladder contracted to empty. This theory appeared to hold some weight, as applying gentle manual therapy to the tissues, and teaching the patient some self-release techniques allowed her to resolve her symptoms entirely after 1-2 visits.

The urachus is formed in early development from the pre-peritoneal layer, and is described as vestigial tissue. It extends from the anterior dome of the bladder to the umbilicus, varying in length from 3-10 cm, with a diameter of 8-10 mm. There are 3 layers: an inner layer of transitional or cuboid epithelial cells surrounded by a layer of connective tissue. The remains of the urachus form the middle umbilical ligament which is a fibromuscular cord. A layer of smooth muscle that is continuous with the detrusor (smooth muscle of the bladder) makes up the outer layer. This continuity of tissue may help explain some of the clinical connections we see in patient symptoms. In the past year, I have met several patients for whom the urachus is the only tissue that reproduced their symptoms. I examined a male patient who reported urethral burning that occurred with both reset and activity. Unable to produce symptoms in any other location of the thoracolumbar spine, pelvic floor and walls, or abdomen, I palpated this structure to find that it reproduced the urethral burning. Another patient presented with a keloid c-section scar. She also described a sharp pain when the bladder was full. Treatment directed to the scar and along the midline resolved this pain, again with a couple sessions.
If you are interested in learning more about distinct anatomical connections that can help you explain (and treat) issues your patients present with, come and learn with us at the 3-day Male Pelvic Floor Function, Dysfunction, and Treatment course offered four times over the 2019 and 2020 calendars. The role of the urachus in abdominopelvic dysfunction is just one of the many topics we explore. With lectures on sexual health, pelvic pain, prostate and urinary dysfunction, there is a broad range of topics and skills to offer for clinicians who are new to men’s heath and those who have been treating for years.
Begg, R. C. (1930). The Urachus: its Anatomy, Histology and Development. Journal of Anatomy, 64(Pt 2), 170–183.
Gray, H. (1918). Anatomy of the Human Body. Philadelphia: Lea & Febiger.
Sterling, J. A., & Goldsmith, R. (1953). Lesions of Urachus which Appear in the Adult. Annals of Surgery, 137(1), 120–128.
Most clinicians will agree that stress can amplify a patient’s pain and slow recovery. Mindfulness training provides patients with the ability to self-regulate their stress reaction and has been shown to reduce pain and depression and improve quality of life in patients with chronic pain conditions.1 The growing popularity of meditation training to manage stress has led to an increased interest in the physiological mechanisms by which meditation influences the body’s stress reaction. A systematic review and meta-analysis examined the results of randomized controlled trials that compared the impact meditation interventions to active control groups on stress measures. 2 Forty-five studies were included. Meditation practices examined were focused attention, open monitoring and mantra repetition. Outcome measures studied were cortisol, blood pressure, heart rate, lipid and peripheral cytokine expression. Studies had diverse participants including healthy adults, undergraduate students, army soldiers, veterans, cancer survivors, and individuals with chronic pain conditions, cardiovascular disease, depression and hypertension.
 When all meditation forms were analyzed together, meditation reduced blood cortisol, C-reactive protein, resting and ambulatory blood pressure, heart rate, triglycerides and tumor necrosis factor-alpha. The effect of meditation on:
When all meditation forms were analyzed together, meditation reduced blood cortisol, C-reactive protein, resting and ambulatory blood pressure, heart rate, triglycerides and tumor necrosis factor-alpha. The effect of meditation on:
- Cortisol and resting heart rate was considered to be high level of evidence.
- C-reactive protein, blood pressure, triglycerides and tumor necrosis factor-alpha was considered to be moderate level of evidence.
Analyzed individually:
- Open monitoring meditation reduced ambulatory systolic blood pressure, systolic blood pressure following a stress test and resting heart rate. Effects assessed as providing moderate level of evidence.
- Focused awareness reduced blood cortisol and resting systolic blood pressure. Effects assessed as providing low level of evidence.
- Mantra repetition reduced systolic blood pressure. Effects assessed as providing low level of evidence.
Authors report the primary reason for downgrading the grade of evidence when analyzing meditation practices individually was the limited number of studies available and small sample sizes. They conclude overall, when compared to an active control (relaxation, exercise or education) meditation practice leads to decreased physiological markers of stress in a range of populations.
Carolyn will offer her popular course, Mindfulness-Based Pain Treatment, in Portland OR, July 27 and 28 and again in Houston TX, October 26 and 27. We recommend these unique opportunities to train with Carolyn, a nationally recognized leader trailblazing the successful applications of mindfulness into pain treatment and the field of physical therapy. Hope to see you there!
1. Hilton L, Hempel S, Ewing BA, et al. Mindfulness meditation for chronic pain: Systematic review and meta-analysis. Ann Behav Med. 2017;51(2):199-213.
2. Pascoe MC, Thompson DR, Jenkins ZM, Ski CF. Mindfulness mediates the physiological markers of stress: Systematic review and meta-analysis. J Psychiatr Res. 2017;95:156-78.
Pain demands an answer. Treating persistent pain is a challenge for everyone; providers and patients. Pain neuroscience has changed drastically since I was in physical therapy school. This update comes from the International Spine and Pain Institute headed by the lead author Adriaan Louw, PT, PhD. If you are interested in reading more about persistent pain, I suggest reading the article in its entirety.
 This article brings together several comorbidities that pelvic physical therapists often encounter; fibromyalgia, chronic fatigue syndrome, irritable bowel syndrome, and chronic Lyme disease. The authors argue that all of these syndromes have many common symptoms and might be dependent on the provider that the individual goes to as to which diagnosis the individual receives. Often, once an individual has a diagnosis, he or she (more often she) then identifies with this label. The authors reason that once medical pathologies have been ruled out, then a more holistic, biopsychosocial approach may create better outcomes.
This article brings together several comorbidities that pelvic physical therapists often encounter; fibromyalgia, chronic fatigue syndrome, irritable bowel syndrome, and chronic Lyme disease. The authors argue that all of these syndromes have many common symptoms and might be dependent on the provider that the individual goes to as to which diagnosis the individual receives. Often, once an individual has a diagnosis, he or she (more often she) then identifies with this label. The authors reason that once medical pathologies have been ruled out, then a more holistic, biopsychosocial approach may create better outcomes.
Pain neuroscience education is a way to explain pain to patients, often with analogies, with a focus on neurobiology and neurophysiology as it relates to that individuals pain experience. To be able to educate our patients, we as providers, must be able to understand neuromatrix, output, and threat. Moseley states “[p]ain is a multiple system output activated by an individual’s specific pain neuromatrix. The neuromatrix is activated whenever the brain perceives a threat”. If that sounds like gibberish, consider watching this TEDx talk by Lorimer Moseley on YouTube (the snake bite story is a favorite of mine):
What is a neuromatrix? Essentially, it is a pain map in the brain; a network of neurons spread throughout the brain, none of which deal specifically with pain processing. The way I visualize it is to think about what goes on when you think of your grandmother. There isn’t a grandmother center in the brain, but there are sights and smells (sensory), feelings (emotional awareness), and memories that all come up when you think about her. When we are overwhelmed with pain, those regions become taxed and the individual may have difficulty concentrating, sleeping, and/or may lose his/her temper more easily. Just as each person’s grandmother is different so is a person’s pain and the neuromatrix is affected by past experiences and beliefs.
Pain is an output. It is a response to a threat. When a person is exposed to a threatening situation, biological systems like the sympathetic nervous system, endocrine system, immune system, gastrointestinal system, and motor response system are activated. When a stress response occurs, these systems are either heightened or suppressed to help cope, thanks to the chemicals epinephrine and cortisol.
What is a threat? Threats can take a variety of forms; accidents, falls, diseases, surgeries, emotional trauma, etc. Tissues are influenced by how the individual thinks and feels, in addition to social and environmental factors. The authors propose that when individuals live with chronic pain, their body reacts as though they are under a constant threat. With this constant threat the system reacts and continues to react, and the nervous system is not allowed to return to baseline levels. This can create a patient presentation with immunodeficiency, GI sensitivity, poor motor control, and more. This sounds like most patients who walk into my clinic. The authors suggest that one system may be affected more and that can influence what the patient is diagnosed with even though the underlying biology is the same for many conditions. There are theories for why that happens; genetics, biological memory, or it could be the lens of the provider that the patient sees. There is a table in the article that shows symptoms, diagnosis, and current best evidence treatment for the conditions of fybromyalgia, chronic fatique syndrome, irritable bowel syndrome, and chronic Lyme disease which is worth a look. The treatments all work to calm the central nervous system.
The authors go on to question the relationship between thyroid function and these conditions as changes in cortisol and the hypothalamic-pituitary-adrenal (HPA) axis. The HPA axis is fascinating, and confusing. Luckily, the Pelvic Floor Series Capstone course does a great job breaking it down.
Now that this hypothetical patient is in our treatment room what do we do? The authors suggest seeing these conditions for what they are: chronic pain conditions. They recommend that physical therapists see past the label that a patient may have picked up with a previous diagnosis, and keep the following in mind when treating these patients:
- They are hurting
- They are tired
- They may have lost hope
- They may be disillusioned by the medical community
- They need help
These people need the following from their medical providers:
- Compassion
- Dignity
- Respect
With empathy and understanding therapists can use skills in education, exercise and movement with the intent to improve system function (immune, neural, and endocrine), rather than fixing isolated mechanical deficits.
Louw, Adriaan PT, PhD; Schmidt, Stephen PT ; Zimney, Kory PT, DPT ; Puentedura, Emilio J. PT, DPT, PhD Treat the Patient, Not the Label: A Pain Neuroscience Update.[Editorial] Journal of Women's Health Physical Therapy. 43(2):89-97, April/June 2019.
By accepting you will be accessing a service provided by a third-party external to https://hermanwallace.com/










































