With PF1 Durham just around the corner, and PF1 Seattle in January sold-out with a 20-person wait list, our next PF1 is filling up quickly.
PF1 in Maywood, IL from March 1-3 is over half-full, and additional registrations are rolling in each day. If you are interested in joining us for PF1 in Maywood, do not hesitate to register. We expect this course to fill up before the holidays are upon us, so act quickly.
Once PF1 in Maywood is full, the next available PF1 is in Houston, TX in early May 2013. If you'd like to take this popular course before May of 2013, we suggest registering for the Maywood course today!
Stay tuned this week for a big announcement that we have coming up. We are adding a new highly requested feature to our website, which we are confident women's health physical therapists will find very helpful!

Congratulations to Herman & Wallace faculty member, Peter Phillip, who was recognized in his community for his stellar work as a therapist. The New Canaan Advertiser writes, "if you end up at Philip Physical Therapy on Vitti Street, you’re in good hands". (Read the full article HERE)
Peter developed two courses which he instructors through Herman & Wallace, Sacroiliac Joint and Pelvic Ring Evaluation and Treatment and Differential Diagnostics of Chronic Pelvic Pain: Interconnections of the Spine, Neurology and the Hips. Peter is also an item writer and Subject Matter Expert developing our Pelvic Therapy Practitioner Certification Exam.
Way to go, Peter!
"Movember," a men's health movement that began in Australia, has found its way around the globe. In this campaign, men grow mustaches (starting out November 1st clean-shaven) for one month to raise awareness about men's health issues, with particular emphasis on prostate and testicular cancer. Check out some of these images on the website to see for yourself how awesome these staches are.
This is a serious fundraising effort- in 2011 the organization raised over 126 million in US dollars. This money is spent on increasing awareness of male cancers and also on improving the response of the medical community to these conditions. Funds are also directed to organizations such as The Prostate Cancer Foundation.The organization's strategic goals as outlined on their website are to fund survivorship initiatives, increase awareness and education, fund research including clinical trials and research that informs health policy. The first item on the group's list of values is "fun" and we can easily see why this event attracts repeat crowds.
So what if you can't grow a mustache? You can still attend a Movember event sporting a faux such as a mustache-on-a-stick. Learn how to make your own here. Women engaged in the movement are known as Mo Sistas, and certainly men's health issues are issues for all families, as are women's health issues. In the presence of cancer, as we know, early detection can improve survival and allow for more treatment options. If you would like to find an event near you, check out this interactive map. If you live in Seattle or in Orange County, you can attend a "Running of the Mo's" event!
Regardless of your level of participation, what a terrific organization to celebrate and share with others. Consider hosting or attending a Movember event, and consider engaging someone in a dialog about men's health screening as well as pelvic rehab options. (Mustache optional.)
At the annual conference of the California Biofeedback Society last week, a new device was described for the treatment of jaw pain. The SleepGuard biofeedback headband can be worn by the user and when the band senses that the jaw is clenched, an alarm will sound to deter the patient from the clenching. It makes sense that a patient can re-train the body to avoid muscle tension with such a device.
So what can we do about the butt grippers? Although some clever and potentially not-so-comfortable ideas come to mind in relation to biofeedback sensors and the pelvis during sleep, how do we educate our patients who tend to clench at night to let go and avoid that morning pain? If you are unfamiliar with the concept of "butt gripping," please check out the work of Diane Lee, from whom I first heard the term. In an article on her website, Diane discusses the concept of gripping with the chest, back, or butt. Chances are, you can think of a patient who fits one of the categories. (Not that any of us have movement dysfunction, but you might have "a friend" who could use some guidance in re-training one of the gripping patterns.)
Patients who tend to clench any muscle all night will be creating compression in nearby joints, and the muscles will not be getting proper recovery and rest time during sleep. These patients will often wake with increased pain in the area of tension or muscle guarding. The first step in treating a condition of gripping is awareness: if you have no idea that you are creating tension in a muscle, the re-training of the muscle won't happen. Help your patients understand that a tendency to tighten a muscle group may be a habit brought up by the body guarding a region for various purposes. Consider the patient who has low back pain- tightening or splinting the area with muscle contractions may be a useful strategy early in the injury. Once a patient is aware of the tension that may aggravate a painful area or promote a dysfunctional movement pattern, creating new strategies is critical. Your patients may require soft tissue or joint mobilization, muscle balancing techniques, movement re-training (to include functional patterns or tasks), and general awareness or relaxation techniques.
Let's think of the patient who goes to bed and maintains tension in the gluteals, pelvic floor, or pelvic area. What can she do at bedtime? There may be a few stretches that loosen the muscles, breathing and awareness exercises, general relaxation or meditation activities, or some contract/relax to improve the muscle state. She might also have a self-massage or trigger point technique, complete a self-massage or partner-assisted massage, take a warm bath, or apply some heat or cold to the area of tension. Once in bed, what position does your patient adopt for sleep? Is she in supine with a posterior pelvic tilt, in sidelying with the thighs pressed tightly together? You can help the patient recognize the postures, positions, and patterns of holding that may be worsening the condition. Many patients find that completing some simple pelvic tilts or rocking prior to falling asleep can decrease guarding.
As an observational skill, recognizing patterns of gripping can aid in development of a rehabilitation program that looks for static or dynamic postures that need re-training. Butt gripping is one such pattern that will increase tension and muscle dysfunction in the pelvic floor and often in the hips and low back. There are many courses offered by the Pelvic Rehab Institute that incorporate these concepts into rehabilitation principles. If you are unable to attend a live course, or are interested in getting started in pelvic rehabilitation, check out the on-line MedBridge course created by the Institute co-founder, Kathe Wallace. The course is full of examination and intervention techniques that will benefit patients who have pelvic dysfunction.
So, when did you last really think about the modalities you applied to your patient?
As I sat through the last few lectures in a physical therapy "Interventions" class that includes training in various modalities, I am reminded that there is quite a lot of science behind the modalities we have in the clinic. What I am also reminded of is the fact that it is easy to get in a groove and do what is easy in the clinic versus process the sometimes painful clinical reasoning that is required for electromodalities. Today's lecture at the College of St. Scholastica, from where I graduated and now am honored to assist in an adjunct role, given brilliantly by faculty member Karen Swanson, consisted of terminology that frankly gets a bit mind-boggling unless you have some lecture material in front of you. There is direct current, alternating current, microcurrent, interfering current that happens before leaving the machine, interfering current that happens in the body, and specific ranges of current that produce specific effects.
Regarding electrical stimulation, have you ever made the following errors?
1. Applied premodulated bipolar interferential current and used 4 electrodes instead of 2?
2. Applied a TENS unit, using the 4 electrodes in an "x" fashion thinking the treatment area is between all 4 electrodes?
3. Kept the electrodes closer together to allow the current to be applied more deeply?
4. Applied Russian stimulation, telling the patient (as it was described by its inventor) that it is "painless?"
The title of this post, in the current mode of LOL cats and "Ur Doin' It Wrong" humor is not meant to point fingers, rather my goal is to stimulate some thought about why we are doing what we are doing in the clinic.A clinical approach I hear that astounds me is the complete dismissal of all modalities that require a plug-in. "There's no research..." is one of the more common excuses that I hear. When was that information last confirmed? Ultrasound in particular has received a bad rap in the clinic, however, the articles that were relied upon to conclude that ultrasound has no merit were later found to not be considered worthy research articles. Also of note is the updated information that unless you are treating a scar or trigger point in the muscle, applying ultrasound over a muscle belly is not recommended. Rather, the tissue heating effects of ultrasound are best applied over tendons and ligaments.
How do we stay current in the clinic when it comes to modalities? Attending a session at a national conference, or a continuing education course is a great place to start. Another option is to rely upon the students or new graduates who are hopefully making their way into your workplace. Ask them to give an inservice, or invite your local modalities representative in and request recent research. The next time that you apply a modality that has optional settings, ask yourself why you are applying the modality at those settings? You can also invest in an updated copy (5th Edition!) of Michlovitz's Modalities for Therapeutic Intervention (just updated this year.) In our profession, there are few situations that rely upon a cookbook approach, and we must rely upon clinical reasoning skills rather than habits. And if you are a new graduate, don't allow a more experienced therapist to enforce upon you his or her bad habits, and be sure to share all the updated, good bits you have learned in your extensive training!
Grab your passports, colleagues, and head up (or down as it may be) for the 1st Pelvic Health Symposium to be offered in Toronto, Canada. The symposium will feature expert lecturers and topics that are relevant for pelvic health practitioners. The symposium is titled Beyond The Basics: Pelvic Pain and Incontinence, and topics include pudendal neuralgia, interstitial cystitis/painful bladder syndrome, vulvodynia, mindfulness, hormone therapy, and compounded medications for pelvic pain. In this one day symposium you can hear from a neurologist, urologist, gynecologist, psychiatrist, staff physician at a clinic for menopause, and a compounding pharmacist. You can access the program brochure, information about the speakers, as well as registration at the Pelvic Health Solutions website.
Pelvic Health Solutions is a practice created by Nelly Faghani and Carolyn Vandyken, two physiotherapists who are committed to providing excellent rehabilitation for pelvic dysfunctions through continuous learning, mentoring and teaching. In addition to creating practice environments that support patients with pelvic dysfunction, their website serves as an excellent resource for both clinicians and patients. Check out one of their pages here.
Because the drive to learn is so strong among pelvic health practitioners, we seem to be constantly traveling to attend workshops and increase our level of knowledge to share with our patients. Take advantage of this one-day symposium and then enjoy the beautiful and culturally diverse city of Toronto!
Pelvic Rehab Report from Guest Blogger, Jillian Beaulieu, DPT, CYT

OK, before I discuss the inspiration for the title of this blog, a brief anatomy and physiology lesson:
In terms of anatomical location, the ovary is deeply embedded and protected within the ovarian fossa in the crowded lateral wall of the pelvis on either side. Each ovary is fairly small, each one being only approximately 3-5 cm during childbearing years. Female ovaries are analogous to male testes in that they are both gonads and endocrine glands that play a big role in reproductive function. Several paired ligaments support the ovaries. The ovarian ligament on either side connects the uterus directly to the ovary. The posterior portion of the broad ligament forms the mesovarium, which supports the ovary and houses its arterial and venous supply. The suspensory ligament of the ovary (infundibular pelvic ligament) attaches the ovary to the pelvic sidewall. Nerve supply to the ovaries runs via the suspensory ligament of the ovary provided through the ovarian, hypogastric, and aortic plexuses. Superior to the ovary lies the small intestine and cecum (right) or sigmoid (left). The bladder and round ligament reside anterior to each ovary. Inferiorly there is the broad ligament and parametrium. The rectum and ureters are behind each ovary. Laterally, the suspensory ligament, obturator nerve, ureters, iliac vessels are found and medially the fundus of the uterus. Wow!
Physiologically, the two small ovaries have a big job to accomplish every month in two phases, follicular and luteal. The follicular phase involves follicle development and growth with the goal of releasing a mature follicle to be fertilized within the uterine tube. Additionally, the ovaries are responsible for the production of female sex hormones estrogen and progesterone. They are busy factories that are constantly in movement and require a significant amount of organ mobility within the pelvic cavity. Given the latter information and without discussion of the many possible underlying causes of ovarian pain, there is no wonder that connective tissue and mechanical tightness or adhesion in the periovarian and surrounding structures may cause ovarian pain and dysfunction.
Thank goodness Ramona Horton, MPT recently taught me how to address these issues through Mobilization of Visceral Fascia for the Treatment of Pelvic Dysfunction: Level II!
Recently I found myself with quite a few patients with diagnoses involving ovarian pain and dysfunction that led to an endless list of other concerns for them. For three of my patients I have found the techniques that I learned in this course to be particularly valuable, and that is only in the three weeks since I took the course! For the patients I first ruled out kidney, bladder, small intestine, and large intestine involvement and treated with techniques such as pubovesical ligament mobilization and ileocecal valve induction as appropriate. I also looked at the kidneys, obturator nerve, and uterus/cervix due to their direct connections. I found techniques such as broad ligament mobilization and cervical-ovarian mobilization profound for freeing the periovarian structures. Finally, I have been concluding each treatment with tubo-ovarian induction for establishing motility of the periovarian structures by “surfing the wave.” Interested and intrigued? I cannot recommend taking this course enough!
Have you ever wished that you could impart all that you have learned about pelvic pain to your female patients? Starting from simple concepts such as how one insult or injury to the tissues can start a cascade of events over time, and progressing to the amazing knowledge that keeps pouring in about the brain's involvement in chronic pain states? And don't we always hear from patients how difficult it can be to establish a team of professionals who are all on the same page related to treatment options discussed in a compassionate manner?
The Institute recently heard from such a team of experts who have joined together to offer a weekend program for women who have chronic pelvic, sexual and genital pain. Diagnoses included in the above categories can include Interstitial Cystitis (IC), vulvodynia, vestibulitis, Irritable Bowel Syndrome (IBS), pelvic floor dysfunction, pudendal neuralgia, lichen sclerosis, endometriosis, and other pelvic and genital pain disorders. The experts who will provide an entire weekend of education for patients (and interested partners) consists of two physicians, Dr. Robert Echenberg, Dr. Deborah Coady, a physical therapist, Amy Stein, and two counselors, Nancy Fish and Alexandra Milspaw.
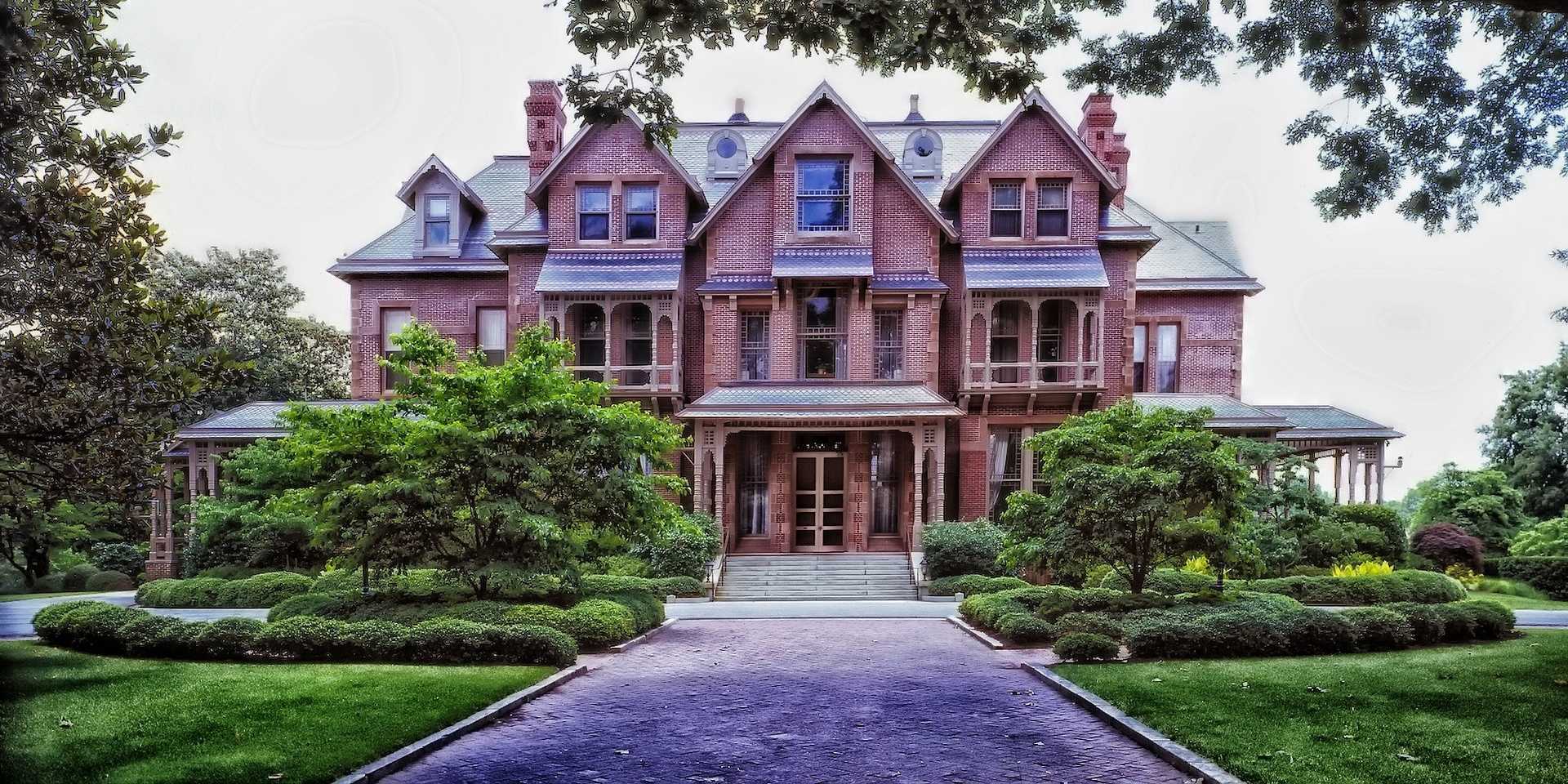
The weekend goals are to provide a safe environment in which a person can learn skills that can be immediately applied for self-care. You can be assured that with the group of practitioners involved your patients will be addressed in a holistic manner, and that the knowledge gained can be used in conjunction with a patient's current home program or concurrent therapies. The workshop is scheduled for April 27-28 of 2013, and located in Bethlehem, Pennsylvania. Participants can register at the website www.allianceforpelvicpain.com.
The cost of the retreat itself including several meals is only $450 if registered prior to December 1st of this year (price increases to $475 after December 1st.) What a reasonable price for a patient who can travel (or perhaps lives nearby) and who is interested in expanding her knowledge of how to live with and heal her chronic pelvic pain.
Our partners at Medbridge Education are offering the chance to watch one chapter of our course on pelvic floor exercise cueing for free.
In this clip, Institute founder Kathe Wallace demonstrates techniques and instructs on how to confidently cue exercises for your next pelvic rehabilitation patient. Each cue helps patients identify where they need to contract or relax their pelvic musculature.
Click HERE to watch this chapter for free and learn more about the full list of online offerings available through Herman & Wallace and Medbridge Education.
Last night as I spoke to an arthritis support group about myofascial and chronic pain, I was able to share information about the research that has taken place over the last decade that describes associations between the brain and pain. The simple idea that being "distracted" by a task eases the perception of pain brought about a story from an attendee about how riding a horse, because it required focused, unwavering attention and because it was immensely enjoyable, was an activity that reduced the rider's pain dramatically. Mentioning that playing with grandchildren or pets could be a wonderful distraction brought about smiles and nods of agreement.
Within the realm of pelvic rehabilitation, we face many patient scenarios that include chronic pain and the need for education about the brain's ever-present role in pain. A recent literature review for a pharmacology course confirmed that research continues to present fascinating advances in imaging and brain changes in response to such pain. Here is a link to a full text article about distraction and pain and the response to functional MRI (neurofeedback) with attempts to modify pain.
According to Apkarian and colleagues (who have completed pioneering work in this field) some of the topics that have been studied in relation to brain structural changes include back pain, fibromyalgia, chronic regional pain syndrome, knee pain, irritable bowel syndrome, headaches, female and chronic pelvic pain. Here is a terrific article by Apkarian that summarizes much of the development of the evolving theories about pain and the brain. The basic summary of the article includes the thought that chronic pain causes abnormal changes in the gray and white mater, and in the relationship between the two. Lorimer Mosely wrote an interesting post about Dr. Apkarian back in May, you can access it here.
Different types of chronic pain will shape the pain uniquely, and the changes can take place rather quickly or over a period of several years. In women who have endometriosis, As-Sanie and colleagues demonstrated that women with chronic pelvic pain have brain changes in multiple areas associated with pain processing, and that women with chronic pelvic pain (and not endometriosis) have changes in a separate site. The exciting news is also that within the research, reducing the pain also appears to positively affect the brain changes.
As professionals involved in helping our patients understand the complex and remarkable experience that is healing, we have a responsibility to continue to learn ourselves and to figure out how to include the brain in our approaches to pain. The Neuro Orthopaedic Institute (www.noigroup.com) has supplied various educational opportunities and resources that assist in accomplishing this type of education. There is a new resource from NOI about graded motor imaging, worth checking out in addition to the patient education book titled "Explain Pain" with which many of you are already familiar. While teaching in Seattle over the weekend, experienced course participants generously shared their strategies for educating patients in concepts of pain and healing. Here is a highly recommended video available on YouTube that explains common pain concepts while using great visual sketches to get the ideas across.
By accepting you will be accessing a service provided by a third-party external to https://hermanwallace.com/