If you are familiar with the work of Diane Lee, you may have noticed the term “driver” used throughout descriptions of patient assessment techniques. One definition of “driver” is “a factor that causes a particular phenomenon to happen or develop.” When it comes to a patient’s pelvic dysfunction, we know that there may be a dramatic number of factors driving the symptom, so what is the value of trying to determine the level of significance of various factors?
 Let’s imagine that we meet a female patient who presents with pelvic pain, urinary incontinence, and difficulty holding back gas. In addition to providing a thorough subjective interview, screening for underlying medical conditions requiring attention, examining her neuromusculoskeletal system, and learning more about her daily habits, we need to figure out the best place to start with her care. What if, even though this particular patient has only experienced one major episode of leakage (after which all other symptoms started) you complete the exam to find that she is holding her pelvic muscles tense continuously? Perhaps you share this observation with the patient, only to hear her say that she is “so afraid of leaking again that she keeps her muscles tight to prevent it.” This type of rehabilitation sleuthing can help us get to the heart of the matter with our patients, regardless of the presenting complaints. For example, if we can educate this patient about the potential negative consequences of her fear of having another embarrassing episode (fear leads to muscle guarding which leads to pelvic pain and potentially dysfunctional voiding) then her thoughts can positively contribute to the other therapeutic recommendations we make.
Let’s imagine that we meet a female patient who presents with pelvic pain, urinary incontinence, and difficulty holding back gas. In addition to providing a thorough subjective interview, screening for underlying medical conditions requiring attention, examining her neuromusculoskeletal system, and learning more about her daily habits, we need to figure out the best place to start with her care. What if, even though this particular patient has only experienced one major episode of leakage (after which all other symptoms started) you complete the exam to find that she is holding her pelvic muscles tense continuously? Perhaps you share this observation with the patient, only to hear her say that she is “so afraid of leaking again that she keeps her muscles tight to prevent it.” This type of rehabilitation sleuthing can help us get to the heart of the matter with our patients, regardless of the presenting complaints. For example, if we can educate this patient about the potential negative consequences of her fear of having another embarrassing episode (fear leads to muscle guarding which leads to pelvic pain and potentially dysfunctional voiding) then her thoughts can positively contribute to the other therapeutic recommendations we make.
Other examples may include meeting a patient with pelvic dysfunction whose true “driver” is a kyphotic thoracic spine that compresses the abdominal organs, or a habit of wearing pants with a waistband so tight that bowel function is compromised (true story), foot pain that creates increased loading on the now painful side of the pelvis, or even emotions and thoughts such as fear and shame. I’m sure you can think of many other examples based on your own clinical experience. If you are a newer therapist, or perhaps wish to work through further examples of not only how to evaluate but to treat for finding the primary contributors to a patient’s dysfunction, check out Pelvic Rehabilitation Institute faculty member Elizabeth Hampton’s continuing education course that focuses on this Finding the Driver in Pelvic Pain.
The next opportunity to take this course is in Houston in November of this year or March in San Diego.
Have you ever tried to make a fitted sheet reach all corners of a mattress when there is a small, defective seam stitched into the middle of the fabric? No matter how much you pull or tug, the sheet won’t hug the last corner just right. If you get it to stay, the opposite corner flips off from the extra tension. Unless you release the snag the stitching created, you won’t ever get the sheet to fit smoothly. This is like the myofascial system in the body, where a snag in one area can affect another proximally or distally when normal movement tries to occur.
 Even the pelvic floor can get myofascial restrictions and trigger points; however, this area is often ignored and seemingly insignificant when not fully understood. Pelvic floor fascial restrictions and trigger points can have paramount implications for the pelvic, abdominal, hip, and lumbar regions. This why pelvic rehabilitation practitioners should be equipped to evaluate and treat myofascial snags.
Even the pelvic floor can get myofascial restrictions and trigger points; however, this area is often ignored and seemingly insignificant when not fully understood. Pelvic floor fascial restrictions and trigger points can have paramount implications for the pelvic, abdominal, hip, and lumbar regions. This why pelvic rehabilitation practitioners should be equipped to evaluate and treat myofascial snags.
Pastore and Katzman (2012) published an article stating that 14%-23% of women with chronic pelvic pain have myofascial pelvic pain, and up to 78% of women with interstitial cystitis have myofascial trigger points. Once a trigger point in pelvic floor musculature is identified through palpation, it can refer pain to the perineum, vagina, urethra, and rectum, which seems obvious; however, pain may also refer to the abdomen, back, trunk, hip, buttocks, and lower leg. If palpation can provoke a referral pattern of pain, stretching and/or contraction of the musculature with that myofascial restriction will surely provoke a cascade of symptoms. How can we as clinicians just let statistics like this slide and figure “someone else should do that examination and fix it?” To demonstrate the efficacy in treating myofascial trigger points in pelvic musculature, consider the following study. Anderson et al (2015) had 374 patients follow a protocol of pelvic floor myofascial release of trigger points with an internal trigger point wand along with paradoxical relaxation therapy for 6 months. The goal was to see if patients with chronic pelvic pain syndrome could reduce their medication after following the protocol. At 6 months, a 36.9% reduction in medication use was noted in a complete case analysis, and a 22.7% reduction was revealed in the modified intention to treat (mITT) analysis. Patients no longer needing to take medication significantly correlated with the reduction of overall symptoms from following the protocol.
Knowing how to find and treat pelvic floor myofascial trigger points can lead to reduction of pain in women (and men) and even help reduce the need for medication for their chronic pelvic pain symptoms. Stop trying to make a bed without discerning if the base layer is free of snags. Learning how to go deeper to feel what’s under the covers can help unveil a source of potentially chronic, disabling pain. You can learn how to skillfully treat the “hidden” dysfunction by attending a Myofascial Release for Pelvic Dysfunction course with Ramona Horton.
References:
Pastore, E. A., & Katzman, W. B. (2012). Recognizing Myofascial Pelvic Pain in the Female Patient with Chronic Pelvic Pain. Journal of Obstetric, Gynecologic, and Neonatal Nursing : JOGNN / NAACOG, 41(5), 680–691. http://doi.org/10.1111/j.1552-6909.2012.01404.x
Anderson , R., Harvey, R., Wise, D., Smith, J., Nathanson, B., Sawyer, T. (2015 March). Chronic Pelvic Pain Syndrome: Reduction of Medication Use After Pelvic Floor Physical Therapy with an Internal Myofascial Trigger Point Wand. Applied Psychophysiology and Biofeedback. Volume 40, Issue 1, pp 45-52
The concept of patient compliance, or adherence (a more preferred term), has been the subject of many medical studies, and adherence in pelvic rehabilitation is an aspect of rehab of critical interest. Recently published results of a survey questioning providers and the public about adherence in pelvic floor muscle training offers an insightful perspective. Researchers Frawley, Dumoulin, and McClurg conducted a web-based survey which was published in published in Neurourology and Urodynamics. The survey was completed by 515 health professionals and by 51 individuals from the public. Interestingly, but perhaps not surprisingly, health professionals and public respondents placed different value on which factors related to rehabilitation contributed the most to adherence.
 Data collected in the study included topics such as barriers to adherence in pelvic floor muscle training (PFMT), perception of potential benefit of PFMT, therapy-related factors including therapeutic relationship, socioeconomic factors, and issues surrounding short-term versus long-term adherence, for example. For the providers, poor motivation was rated high as a barrier to short-term adherence, whereas the patients rated perception of minimal benefit from PFMT as the most important barrier. Facilitators of pelvic muscle training included aspects of access such as having appointments outside of the typical workday, or having childcare available, transportation, and not being bored by the exercise program or feeling that the therapist has adequate training and skills.
Data collected in the study included topics such as barriers to adherence in pelvic floor muscle training (PFMT), perception of potential benefit of PFMT, therapy-related factors including therapeutic relationship, socioeconomic factors, and issues surrounding short-term versus long-term adherence, for example. For the providers, poor motivation was rated high as a barrier to short-term adherence, whereas the patients rated perception of minimal benefit from PFMT as the most important barrier. Facilitators of pelvic muscle training included aspects of access such as having appointments outside of the typical workday, or having childcare available, transportation, and not being bored by the exercise program or feeling that the therapist has adequate training and skills.
As suggested by the authors, perhaps that most important variable agreed upon by both providers and public is that of perceived benefit. In other words, patients need to believe that the exercise program can alleviate symptoms and that what they are doing in their particular program is going to achieve positive results rather than wasting time on a home program that will not be effective. This issue is one that can be easily remedied through appropriate patient education, communication with the patient about whether or not they understand the potential value and expected recovery through program participation, and adequate training of the therapist that allows for proper diagnosis and treatment planning. The study concludes by emphasizing that health providers “need to be aware of the importance of long-term patient perception of PFMT…”
If you are interested in advancing your diagnostic or treatment planning skills, check out the pelvic floor series of continuing education courses and the many specialty courses that the Institute offers.
Oftentimes in the blog we address specific populations, perhaps involving pediatrics, post-prostatectomy patients, or patients who have oncology-related issues. Another population that deserves more focus is the geriatric population. If we consider who and where the women are who may be dealing with the highest level of pelvic dysfunction, we are led to the women in their later decades of life. A major challenge for geriatric women is that many pelvic rehab therapists are not reaching them: outpatient clinics tend to cater to younger patients, and for the women who are in living settings other than their own home, there are few therapists trained to address pelvic floor dysfunction such as incontinence or prolapse. Now seems like a great time to remedy these issues, as the Institute has created a course specific to geriatric patients.
What is different about pelvic floor evaluation and intervention in the geriatric population? This is a broad question with a range of important answers, but we can start with this one: what is different about the pelvic floor exam for women of geriatric age? Following are a few key thoughts. (You can find even more information about recommendations for pelvic exams and the use of speculums in the medical clinic in this article published in the Journal of Women’s Health.
 Geriatric patients may require assist for positioning on the examining table, including use of a high-low table or assistive devices for transitions. If a patient cannot tolerate the supine hooklying position for an exam, she may be able to tolerate either a frog-leg position (supine with with bent, heels together, knees abducted) or left sidelying with an assistant holding the top leg in a position for best viewing. Women of older age may have atrophic vaginitis, or thinning of the tissues that creates fragility, and a pelvic muscle assessment may need to be completed externally via observation, palpation, or with external sensors and biofeedback. Age-related changes such as difficulty with vision, hearing, or with complex instructions may require adaptations in exam strategies and sequencing.
Geriatric patients may require assist for positioning on the examining table, including use of a high-low table or assistive devices for transitions. If a patient cannot tolerate the supine hooklying position for an exam, she may be able to tolerate either a frog-leg position (supine with with bent, heels together, knees abducted) or left sidelying with an assistant holding the top leg in a position for best viewing. Women of older age may have atrophic vaginitis, or thinning of the tissues that creates fragility, and a pelvic muscle assessment may need to be completed externally via observation, palpation, or with external sensors and biofeedback. Age-related changes such as difficulty with vision, hearing, or with complex instructions may require adaptations in exam strategies and sequencing.
Another article which summarized guidelines for pelvic exams and cancer screening in women over age 65 discusses the importance of screening women of all ages. Because, as the authors point out, women over 65 are more likely to develop “late stage diagnoses of cancers, pelvic organ disease, incontinence, and infections…”, practitioners should encourage women to continue to seek expert care for screening of such diseases and conditions. The article also discusses the lack of access to gynecologic care in settings like nursing homes and assisted living, leaving women at risk for not having routine exams and screening.
There is much to learn about the pelvic rehabilitation process for geriatric patients of all genders. Herman & Wallace faculty member Heather Rader has offered her expertise in the field of geriatric pelvic rehab and is prepared to discuss not only the common conditions, modifications to evaluation and intervention, but also nuts and bolts topics like documentation, billing, and all things Medicare! You still have time to schedule a warm, sunny break for the coming winter as the continuing education course will take place in Florida in January!
Coccyx pain is a frequently encountered condition in pelvic rehabilitation practices. Although sitting is one of the primary limitations for patients who present with coccyx pain, or coccygodynia, defecation can be included in the list of functional complaints. This brings to mind the question: what does the coccyx do during defecation?
Coccygeal mobility was examined using MRI in this study by Grassi and colleagues. The authors included 112 subjects for the dynamic MRI research in positions of maximal contraction as well as straining for evacuation. Included in the study were subjects who complained of constipation, sense of incomplete evacuation of bowels, pain (not coccyx pain), organ prolapse, and minor trauma. Although the MRI was completed with the patient in supine (a non-functional defecation position), the authors reported that during a straining maneuver, the coccyx moves into extension, or backwards.
What if the coccyx does not move into extension during a straining maneuver? Is it possible for the coccyx to interfere with defecation? This appears to be true for a patient who appeared as the subject in the Journal of Medical Case Reports. The patient presented with an anteverted coccyx, and complained of “…worsening rectal pain developing an hour before defecation and lasting for several hours afterwards.” Pain was also reported during sitting on a hard surface. (See the linked article for an interesting image of the coccyx position and what is described as “rectal impingement.”) The patient was treated with coccygectomy which appeared to significantly reduce the symptoms (there are no outcomes tools reported in the case study, so progress reported is vague.) Although removal of the coccyx was the treatment in this particular case, the authors state that first-line treatment for coccyx pain includes conservative measures such as seat cushioning, coccygeal massage, stretching and manipulation, and injections, and that the majority of patients will respond favorably to these interventions.
There is more to learn about the coccyx and its role in defecation, sitting, and other daily functions. Faculty member Lila Abbate teaches a great course called Coccyx Pain, Evaluation & Treatment and it is a great opportunity to learn some new evaluation and treatment techniques. Join her this October 25-26 in Bay Shore, NY.
We're excited to have the chance to interview Lisa Odabachian, MPT, BSN, RN, PRPC, this week's featured Certified Pelvic Rehabilitation Practitioner! Lisa earned her certification in May of 2015 and she was kind enough to share her thoughts with us. Thank you for your contributions to the field of pelvic rehab, Lisa, and congratulations on your certification!

What motivated you to earn PRPC?
For patients and referring providers to have confidence that I have expertise in treating pelvic floor dysfunctions.
What makes you the most proud to have earned PRPC?
That I have evolved into a practitioner that can make a difference in this patient population’s quality of life.
What advice would you give to physical therapists interested in earning PRPC?
Take as many courses with hands on lab work that you can so you can treat with a broad base of knowledge to get the best outcome for your patients!
Tell us a little about your clinical practice:
I am a full-time clinician at a well-known and well-respected hospital-based outpatient women's clinic. I have been at the Beaumont's Women's Urology Center, a multidisciplinary clinic focusing exclusively on women's health, for the past 5 years. incontinence, pelvic organ prolapse, urinary urgency and frequency, chronic pelvic pain conditions (painful intercourse, interstitial cystitis, vulvodynia, abdominal pain), post-surgical pain and weakness, colo-rectal dysfunctions (fecal incontinence, constipation, rectal pain). I have been in clinical practice treating women and men with pelvic dysfunctions for over 14 years at Beaumont Hospital. Prior to that I was a clinical nurse treating patients in a variety of settings. I am currently an ABPTS candidate to sit for the 2016 WCS specialist certification examination in Women's Health physical therapy.
How did you get involved in the pelvic rehabilitation field?
Through the years of being a nurse, family member and friend I have heard many stories from women and men who have had symptoms that were unsuccessfully or only partially helped with medications and/or surgical interventions. When I learned that there were specially trained physical therapists who treat bladder, bowel and sexual problems by providing the patients self-help education and rehabilitation techniques to help resolve these issues, I became charged up to get my master’s in physical therapy so I could then specialize in treating pelvic floor dysfunctions.
What/who inspired you to become involved in pelvic rehabilitation?
When I learned that there were specially trained physical therapists who treat bladder, bowel and sexual problems by providing the patients self-help education and rehabilitation techniques to help resolve these issues, I became charged up to get my master’s in physical therapy so I could then specialize in treating pelvic floor dysfunctions.
What patient population do you find most rewarding in treating and why?
The patients who are motivated in helping themselves by being compliant in their rehabilitation by doing their home exercise program and asking questions are the patients who typically have the best outcomes.
If you could get a message out to physical therapists about pelvic rehabilitation what would it be?
There are so many women and men who could benefit from a skilled pelvic floor physical therapist. Many patients with pelvic floor dysfunction have difficulty being appropriately evaluated and referred to pelvic floor physical therapy, and then if that occurs they often have to travel long distances to find a proficient provider.
What has been your favorite Herman & Wallace Course and why?
I have learned so much from each and every course I have taken. My first course was in Akron Ohio in May 2001 with Holly Herman and Kathe Wallace, so of course that is my most memorable course because it was like opening a Pandora’s Box, in a good way! It all made sense!
What lesson have you learned from a Herman & Wallace instructor that has stayed with you?
Perform a good orthopedic evaluation first
What do you find is the most useful resource for your practice?
I often refer to course/lab course notes.
What is in store for you in the future?
My application has been approved to sit for the 2016 specialist certification examination in Women’s Health in physical therapy to obtain WCS credentials through the APTA.
What role do you see pelvic health playing in general well-being?
It’s huge! When people have bladder, bowel and/or sexual dysfunction, their relationships, social, career, education, emotional, recreational and/or psychological, etc. well-being is affected to varying degrees. People often do not even know they have pelvic floor muscles until there is pain or a functional impairment.
 The Herman & Wallace Pelvic Rehabilitation Institute was founded nearly a decade ago by physical therapists and educators Kathe Wallace and Holly Herman. The Institute has served as a platform for foundational to advanced pelvic rehabilitation coursework that covers a wide variety of topics. Included in some of the newer coursework is content directed at more general orthopedics or women’s health topics, such as:
The Herman & Wallace Pelvic Rehabilitation Institute was founded nearly a decade ago by physical therapists and educators Kathe Wallace and Holly Herman. The Institute has served as a platform for foundational to advanced pelvic rehabilitation coursework that covers a wide variety of topics. Included in some of the newer coursework is content directed at more general orthopedics or women’s health topics, such as:
- Biomechanical Assessment of the Hip and Pelvis
- Rehabilitative Ultrasound Imaging: Orthopedic Topics
- Physical Therapy for the Breast Oncology Patient
- Neck Pain, Headaches, Dizziness, and Vertigo
- Manual Therapy for the Lumbo-Pelvic-Hip Complex.
Occasionally, as we have continued to expand our offerings at the Institute, participants have expressed concern that a few of the courses are “not pelvic floor” related. We wanted to take a moment to share our perspective regarding that concern:
1. Most pelvic rehabilitation providers are not exclusively working with patients who have pelvic floor dysfunction.
When we completed a survey of job task analysis among pelvic rehabilitation therapists, we learned that many therapists are not working with patients who have pelvic dysfunction 100% of their time, and that general musculoskeletal care makes up a large part of many pelvic rehab therapists’ caseload. Unfortunately, many patients aren’t often dealing with only one dysfunction, so our patients who present with urinary incontinence may also have foot pain, or headaches, for example.
2. Many pelvic rehabilitation providers also describe themselves as orthopedic therapists.
The majority of therapists who responded to our job analysis survey (and those who attend our courses) work in either an outpatient facility or a hospital-based outpatient facility. In fact, many of the respondents are board-certified in orthopedics. Outpatient facilities typically require that a therapist can work with any part of the body, in addition to the pelvis.
3. General orthopedic rehabilitation is closely related to pelvic rehabilitation.
There are an overwhelming number of ways that a patient’s comorbid conditions can be related to the pelvic floor. For example, a patient with foot pain may unload the involved side, placing increased strain on the hip, pelvis, and low back on the opposite side. Another patient who has poor balance may decrease their degrees of freedom by holding the trunk and pelvic muscles tense in order to compensate for a balance difficulty. A patient who has migraines may have to spend a significant amount of time lying flat when she has migraines, potentially leading to discomfort in other joints.
4. We have not decreased the amount of pelvic courses we offer in exchange for general, orthopedic courses. On the contrary, the Institute has continued to add more focused pelvic rehabilitation courses such as Post-Prostatectomy Patient Rehabilitation, Assessing and Treating Women with Vulvodynia, and Geriatric Pelvic Floor Rehab.
In short, we have chosen to offer some coursework that is not solely focused on the pelvis, because these courses can provide benefits to the therapists and to the patients they serve. The Institute is always interested in participant feedback, and is willing to try out new courses to gauge interest level and satisfaction with new courses. As always, you will be provided with the best in pelvic rehabilitation education, and have opportunities to take courses from instructors who offer additional skills and expertise. If you have any questions, or suggestions about course content, please let us know by filling out the Contact Us form on the website. And if you have an idea for a new course you’d like to teach that adds to our existing offerings, we’d love to hear from you- please fill out this form if you have a new course idea.
The abdominal canister is a model that we have used in rehab for a number of years, especially when it comes to discussing the (often controversial) topic of core stability. Traditionally regarded as encompassing the pelvic floor, diaphragm, deep abdominal muscles (particularly Transversus Abdominus), our definitions of ‘the canister’ or ‘core’ have of late expanded to include psoas, obturator internus, quadratus lumborum and the osseous components of the pelvic girdle (Chaitow 2012).
 Often, we in pelvic rehab bemoan the fact that the pelvic floor is not given the attention it deserves (when we know it really is the answer to everything…) but I do believe that we, as pelvic health specialists are just as guilty of not paying enough attention to the ‘roof’ of the canister, the diaphragm.
Often, we in pelvic rehab bemoan the fact that the pelvic floor is not given the attention it deserves (when we know it really is the answer to everything…) but I do believe that we, as pelvic health specialists are just as guilty of not paying enough attention to the ‘roof’ of the canister, the diaphragm.
The diaphragm and the pelvic floor are bound together structurally and functionally by both fascial and muscular connections (Chaitow 2012). The anatomical link between the diaphragm, psoas and the pelvic floor has been explored by Gibbons in 2001 ‘…The diaphragm’s medial arcuate ligament is a tendinous arch in the fascia of psoas major. Distally, the psoas fascia is continuous with the pelvic floor fascia, especially the pubococcygeus’. Newell in 2005 discussed the relationship between the diaphragm and transversus abdominus and Carriere in 2006 concluded that psoas spasm may influence diaphragmatic mechanics, and conversely that abnormal tensions in the medial arcuate ligament of the diaphragm may irritate psoas.
Paul Hodges has also concluded in his 2007 paper that breathing and continence may be more connected to low back pain than levels of activity or BMI, reinforcing Smith’s 2006 study looking at the link between breathing disorders, pelvic floor dysfunction and back pain in over 38,000 Australian women.
Of course, breathing, like pelvic floor functioning, can also be linked to psychological factors: when we are stressed, our breathing tends to become more apical (and our pelvic floors may hold excess tension). When that becomes habitual rather than a temporary stress response, a sub-optimal breathing pattern may develop, which disrupts the abdominal muscle balance and makes both back and pelvic pain more likely, with the added risk of pelvic venous congestion (Chaitow 2012). Myofascial trigger points may also develop because of restricted breathing patterns. We also know the opposite is true – such as using controlled breathing to calm down, to let go of tension and even to modify pain and autonomic responses (Busch 2012). Athletes may be at a particular risk of dysfunction, competing at high levels of intensity, both physically (in competition?) and psychologically (fear of losing a college scholarship?) Although more research is needed to confirm or disprove these connections, theoretically normalizing breathing patterns may improve outcomes in cases of low back or pelvic pain.
In my specialist course ‘The Athlete & the Pelvic Floor’ in Denver next month, we will look at specific manual therapy interventions for the diaphragm and its allies, the psoas and quadratus lumborum. As with any manual therapy techniques, we must always follow up with a clinical and home exercise program, or the effects will be only temporarily beneficial (Coronado 2011, Hegedus 2012) and so we will look at breath re-patterning, integration with the pelvic floor and how this is an often overlooked step when it comes to managing athletes with pelvic floor dysfunction. Hope to see you there!
References:
1. Chaitow, L & Jones, R (Eds) ‘Chronic Pelvic Pain and Dysfunction 2012 Elsevier Churchill Livingstone
2. Gibbons, S.G.T. 2001 The model of Psoas Major stability function. In: Proceedings of 1st International Conference on Movement Dysfunction, Sept 21-23 Edinburgh, Scotland
3. Newell, R. 2005 Anatomy of the post-laryngeal airways, lungs and diaphragm. Surgery 23 (11) 393-397
4. Carriere, B 2006 Interdependence of Posture and the Pelvic Floor. In: Carriere, B The Pelvic Floor, Thieme New York
5. Hodges, P, Sapsford, R, Pengel, L 2007 Postural and respiratory functions of the PFMs. Neorourol. Urodyn. 26 (3), 362-371
6. Smith, M, Russell, A, Hodges, P., 2006 Disorders of breathing and continence have a stronger association with back pain than obesity and physical activity. Aust. J. Physiother. 21(52) 11-16
7. Coronado, R, Bialosky, J & Cook, C. 2010 The temporal effects of a single session of high-velocity, low-amplitude thrust manipulation on subjects with spinal pain Physical Therapy Reviews Volume 15, Issue 1 (01 February 2010), pp. 29-35
This week we get to feature Katie Tredo, DPT, PRPC, one of the first people to earn her Pelvic Rehabilitation Practitioner Certification! Katie co-owned a private practice in Maryland, and has recently relocated to the Milwaukee area to practice her trade. She was kind of enough to offer her insights with the Pelvic Rehab Report today.
![]() Hi Katie! Tell us a little bit about your clinical practice
Hi Katie! Tell us a little bit about your clinical practice
I recently joined the staff at Health In Balance Physical Therapy in Mequon, WI. Our team is made up of experienced physical therapists with a variety of interests and specialties. Along with two of my coworkers, my practice is focused on treating men, women, and children with pelvic dysfunctions. I think a practice with such a skilled and diverse set of physical therapists allows us to better serve our patients.
What patient population do you find most rewarding in treating and why?
I find treating patients with pelvic dysfunctions, especially pelvic pain, to be extremely rewarding. Pain, incontinence, and other pelvic dysfunctions can leave patients feeling very isolated and hopeless. Watching my patients open up about their issues then progress toward their goals, returning to their previous activities and relationships without pain or dysfunction is amazing. There are so many quality of life issues that go along with pelvic dysfunctions and I am honored to be a part of each of my patient’s journey to recovery.
If you could get a message out to physical therapists about pelvic rehabilitation what would it be?
I would encourage physical therapists to get comfortable asking about bowel, bladder, and sexual dysfunction on their initial intake forms. Many people will not think to report these issues without being asked and a pelvic dysfunction can be a major component of a hip or back issue. If your patient reports a pelvic dysfunction, be comfortable acknowledging it and make an appropriate referral for them. I enjoy working closely with and sharing patients with other physical therapists so that we can maximize our patients’ recovery.
What role do you see pelvic health playing in general well being?
In the past discussing pelvic dysfunctions was considered embarrassing or taboo. In the past few years, I have seen more and more of my patients educating themselves, discussing their issues with other men or women, and finding themselves the help they need. Many patients are going into their referring physicians and requesting to receive help instead of waiting for their doctor’s suggestion. Patients are becoming more empowered over their own care. I see pelvic health becoming more and more of a focus in people’s lives and that fewer patients will be content living with their dysfunction.
Within 1 week, I examined 2 women with the diagnosis of lumbar pain who each happened to mention having a hip labral tear. Of course, neither woman volunteered information about the pelvic floor dysfunction she has lived with since having children. When I took the extra step and openly asked if they had any “issues” in the pelvic floor region, both women initially looked surprised and then relieved as they shared (perhaps for the first time) the problems they’ve had. I started to wonder about the contribution of pelvic floor dysfunction to acetabular labral tears, or vice versa, and I knew each problem had to be addressed for the referring diagnoses to be treated completely and effectively.
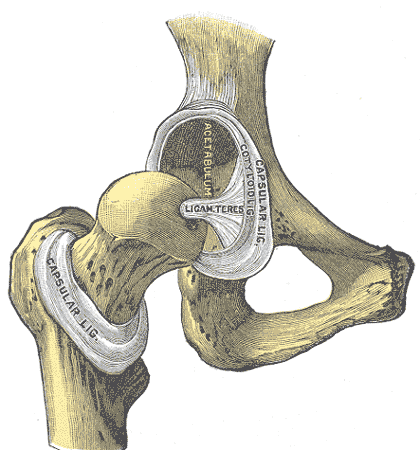
Considering the anatomy of the acetabular labrum in relation to the pelvic floor structures, there is undeniably a connection. A thorough review of pelvic anatomy is given in the Functional Applications in Pelvic Rehabilitation course by Kathe Wallace. Just briefly, the acetabulum is the depression in the pelvis (os coxae) where the femoral head articulates. The labrum sits in the acetabulum, which faces anteriorly along with the femoral head, requiring the anterior aspect of the labrum to stabilize this portion of the hip that lacks bony contact. The obturator internus muscle, which is a deep hip external rotator and abductor, attaches to the posterior aspect of the obturator foramen and inserts on the medial surface of the greater trochanter. When this muscle is in spasm or inhibited, the pelvic floor and the hip can suffer.
 In 2009, Groh and Herrera published a review of hip labral tears, and the general consensus was that labral tears “occur more frequently in women than in men.” The fact that women have more hip dysplasia than men has been suggested as a cause for this finding; however, many of the women with labral tears do not have concomitant hip dysplasia. Alas, Hunt et al (2007) pointed out that women have a generally higher incidence of pelvic-floor pain, which could contribute to the higher incidence of labral tears.
In 2009, Groh and Herrera published a review of hip labral tears, and the general consensus was that labral tears “occur more frequently in women than in men.” The fact that women have more hip dysplasia than men has been suggested as a cause for this finding; however, many of the women with labral tears do not have concomitant hip dysplasia. Alas, Hunt et al (2007) pointed out that women have a generally higher incidence of pelvic-floor pain, which could contribute to the higher incidence of labral tears.
Interestingly, in a study by Brooks and Domb (2012), 10 women over 2 years presented post-partum with anterior hip pain and required labral surgery. The excessive hip external rotation needed for natural delivery was implicated in the pathology, and the authors encouraged obstetricians to have women evaluated prior to delivery and mobilized properly so they could prevent the tears. Hormonal changes in the ligaments as well as the posture assumed by pregnant women with increased lordosis placing more shearing on the anterior aspect of the hip are also factors to consider. Not to mention, the pelvic floor connection to the acetabular labrum certainly seems a reasonable culprit for making the labrum more susceptible to injury during pregnancy and/or delivery.
With the improved technology to diagnose acetabular labral tears, more are being found and treated surgically. The higher incidence of labral pathology in women makes the contribution of pelvic floor dysfunction a serious possibility to consider. If the labrum gets fixed but the pelvic floor is still an issue, becoming completely asymptomatic is less likely. Seeing 2 patients in 1 week who each presented with low back pain, labral tear, and pelvic floor dysfunction when I only work part time makes me think we cannot deny the importance of our subjective examination in uncovering all the possible causes of any suspected tissue in lesion.
Herman & Wallace faculty member Ginger Garner teaches an excellent course called "Extra-Articular Pelvic and Hip Labrum Injury: Differential Diagnosis and Integrative Management" which explores acetabular labral tears in depth. Join Ginger next May in Rochester, NY to learn some great evaluation and treatment techniques!
References:
Groh, M. M., & Herrera, J. (2009). A comprehensive review of hip labral tears.Current Reviews in Musculoskeletal Medicine, 2(2), 105–117. doi:10.1007/s12178-009-9052-9.
Hunt D, Clohisy J, Prather H. (2007). Acetabular tears of the hip in women. Phys Med Rehabil Clin N Am.,18(3):497–520.
Brooks AG, Domb BG. (2012). Acetabular labral tear and postpartum hip pain. Obstet Gynecol. 120(5):1093-8.
By accepting you will be accessing a service provided by a third-party external to https://hermanwallace.com/












































