Prolapse and Rehabilitation Part II: Position of Testing for Prolapse
Measuring pelvic floor function and dysfunction is an emerging clinical science. Researchers and clinicians including Kari Bo, physiotherapist from Norway, have contributed tremendously to the field of pelvic rehabilitation. In an article by Bo and Sherburn published in the Journal of Physical Therapy, the authors describe methods of evaluating pelvic floor function as being divided into measuring of contraction ability (clinical observation, vaginal palpation, ultrasound, MRI, or electromyography (EMG)), and measuring of strength quantification (manual muscle test via vaginal palpation, manometry, dynamometry, or cones.) The authors state that while each method has their place in rehabilitation, each also has limitations. In addition to understanding the best methods for examining pelvic muscle function, we can also consider the techniques that are most useful in examining pelvic organ prolapse.
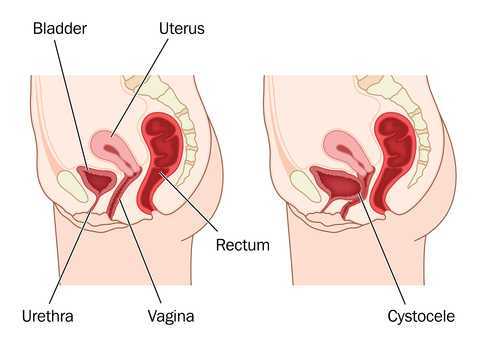
In standing, gravity exerts increased force on the tissues of the pelvis and pelvic floor, therefore, prolapse may be more easily and accurately identified in the standing position. Frawley and colleagues have pointed out that because the provocation of prolapse is higher in standing than in sitting for most patients, rehabilitation testing in standing may be more reflective of functional pelvic floor muscle activity. Research has also concluded that digital (using an examining finger) pelvic organ prolapse examination in supine is unreliable. In standing, however, the same article reports that quality of life and symptom impairment do correlate with digital pelvic floor muscle testing.
Although it has been established that physiotherapists can reliably utilize the pelvic organ prolapse quantification (POP-Q) protocol, POP-Q staging and ordinal scale staging (scoring on a 0-4 scale) have been found to be similar in identifying prolapse. This brings us to the question of how to clinically evaluate for pelvic organ prolapse in standing. Therapists use a variety of strategies for assessing a patient in standing, including:
- Ask patient to sit or squat over opening in table (you may or may not have such a table)
- Palpate digitally while patient is in standing position
- Use a mirror on the floor or hold a mirror under the patient's perineum
- Position yourself under the patient while testing
- Have patient sit on a bedside commode with the center piece open
- Ask the patient to stand on a table (consider safety of this option!)
While it may be useful to test patients for prolapse in supine, research points us to the need to also test patients in positions that will reflect the most significant symptoms. Considering the patient's functional needs as well as anatomic variations, this position may be in quadruped, prone, squatting, or standing, and we must figure out how to incorporate these functional positions into our training.
By accepting you will be accessing a service provided by a third-party external to https://hermanwallace.com/





































