
“The times they are a-changin,” Bob Dylan once sang.(1) Dylan’s song may have been from 1964, but the lyrics can be applied to the present day. Very recently, the world, and the United States in particular, has seen rapid changes in political landscapes.
For instance, America has seen an increase in anti-transgender legislation over the last several years, but also in the past few weeks and months. Many of these laws seek to ban gender-affirming care for transgender, gender non-conforming, and non-binary people, youth in particular., Another bill was introduced just 1 week prior to this post that would make it illegal to identify as transgender on legal documents in Texas, calling it “gender identity fraud,” and carrying with it potential felony charges and jail-time.(2)
What many don’t know is that in addition to charges like the one above, many of these bills also contain exceptions that allow for non-consensual surgeries to be performed on intersex infants and children. The Human Rights Watch states that these procedures on intersex children “are justified by decision-makers on the grounds that they will reduce stigma and prevent gender dysphoria, but they often have the opposite effect and also carry risks of scarring, loss of sensation, lifelong sexual dysfunction, urinary incontinence, psychological trauma, and permanent sterilization.”(3)
For example, in January 2025, an Executive Order from the United States government stated that it would “not fund, sponsor, promote, assist, or support” gender-affirming care for children under the age of 19 “and it will rigorously enforce all laws that prohibit or limit” gender-affirming procedures and treatments.(4) Many American hospitals immediately paused surgical and hormonal gender-affirming treatments for patients under the age of 19 following the order.(5) However, it was found by March 2025 that despite gender-affirming surgeries being paused, non-consensual surgeries were allowed to continue and were still being performed on Intersex infants and children during that time. These non-consensual Intersex procedures were performed by many of the same providers at hospitals who had stopped performing the gender-affirming procedures.(6)
On January 16, 2025, the United States Department of Health & Human Services released the Advancing Health Equity for Intersex Individuals report. This report affirmed the rights of Intersex people to bodily autonomy and informed consent, mentioned health equity barriers for Intersex people, and said that “health care providers and parents can work together to decide that it is in the best interest of the child to delay any non-emergent medical interventions until an intersex child is old enough to be involved in the decision-making about their sexual and reproductive health.”(7) InterACT Advocates for Intersex Youth, called the HHS report, “a victory for the right of intersex children to make their own choices about their own bodies.”(8)
Just days after the release of the HHS report, new government Executive Orders were issued that redefined words like “male,” “female,” “woman,” “man,” and “sex.”(9) This order was intended to impact the transgender and gender diverse communities. However, these Executive Orders impact the Intersex community, as well, as Intersex people can have any gender identity. InterACT says that “many grow up with a gender identity that does not align with their assigned sex at birth – meaning that there is overlap among transgender and intersex communities.”(10) These orders impact cisgender Intersex people, as well. According to InterACT, as “a woman with Complete Androgen Insensitivity (CAIS) may be assigned female at birth, and identify as a woman all her life, while having internal testes – yet the Order would define her sex by her gonads and the reproductive cells they produce.”(10)
***It’s important to note that with the introduction of the new Executive Order, the HHS report has been removed from the HHS and other government websites. InterACT saved the HHS report, and it is accessible on InterACT’s website at this time.***
As laws, reports, and orders are quickly shifting, the healthcare world is rapidly transforming with it. We may not know what local, national, or global changes are on the horizon for the world of politics, the world of healthcare, or the world in general. But one thing that we do know is that healthcare providers need to continue to be advocates for and continue to provide the best evidence-based healthcare to all of our patients, including those who are intersex or transgender.
To learn more about how to be an ally in healthcare and provide better evidence-based care to intersex folx, come take Intersex Patients: Rehab & Inclusive Care with me on May 3, 2025!
Resources
- Dylan, B. (1964). The Times They Are A-Changin [Album]. Columbia Records.
- Yurcaba, J. (2025, March 10). Texas Bill Would Make Identifying as Transgender a Felony Punishable By Jail. NBC News. https://www.nbcnews.com/nbc-out/out-politics-and-policy/texas-bill-identify-transgender-state-felony-rcna195642.
- Human Rights Watch. (2022, October 26). S. Anti-Trans Bills Also Harm Intersex Children. https://www.hrw.org/news/2022/10/26/us-anti-trans-bills-also-harm-intersex-children.
- The White House. (2025, January 28). Protecting Children from Chemical and Surgical Mutilation. https://www.whitehouse.gov/presidential-actions/2025/01/protecting-children-from-chemical-and-surgical-mutilation/.
- Betts, A. (2025, February 3). U.S. Hospitals Suspend Healthcare for Transgender Youth After Trump Order. The Guardian. https://www.theguardian.com/us-news/2025/feb/03/trans-youth-healthcare-hospitals-trump.
- Rodriguez, B., & Sosin, K. (2025, March 10). Hospitals that Paused Youth Gender-Affirming Care Continued Controversial Intersex Surgeries, Group Says. The 19th*. https://19thnews.org/2025/03/hospitals-intersex-surgery-gender-affirming-care-youth/.
- S. Department of Health & Human Services Office of the Assistant Secretary for Health. (2025, January 16). Advancing Health Equity for Intersex Individuals. InterACT Advocates for Intersex Youth. https://interactadvocates.org/wp-content/uploads/2025/01/intersex-health-equity-report.pdf.
- (2025, January 16). Intersex Health Equity Report. https://interactadvocates.org/hhs-supports-bodily-autonomy/.
- United States Presidential Actions. (2025, January 20). Defending Women from Gender Ideology Extremism and Restoring Biological Truth to the Federal Government Executive Order. https://www.whitehouse.gov/presidential-actions/2025/01/defending-women-from-gender-ideology-extremism-and-restoring-biological-truth-to-the-federal-government/.
- InterACT Advocates for Intersex Youth. (2025, January 21). Trump’s Executive Order Ignores Science to Push Discriminatory Agenda. https://interactadvocates.org/trumps-executive-order-ignores-science-to-push-discriminatory-agenda/.
AUTHOR BIO
Molly O’Brien-Horn, PT, DPT, CLT, PCES
 Molly O’Brien-Horn, PT DPT, CLT, PCES graduated from Rutgers School of Biomedical & Health Sciences (formerly the University of Medicine & Dentistry of New Jersey) with her Doctor of Physical Therapy degree. She is a Pelvic Health Physical Therapist, a Certified Lymphedema Therapist and an LSVT BIG Parkinson’s Disease Certified Therapist. Molly is also a sex counselor, a trained childbirth doula, and a trained postpartum doula. Molly is a member of the American Physical Therapy Association Academy of Pelvic Health Physical Therapy and is also a Teaching Assistant with the Herman & Wallace Pelvic Rehabilitation Institute.
Molly O’Brien-Horn, PT DPT, CLT, PCES graduated from Rutgers School of Biomedical & Health Sciences (formerly the University of Medicine & Dentistry of New Jersey) with her Doctor of Physical Therapy degree. She is a Pelvic Health Physical Therapist, a Certified Lymphedema Therapist and an LSVT BIG Parkinson’s Disease Certified Therapist. Molly is also a sex counselor, a trained childbirth doula, and a trained postpartum doula. Molly is a member of the American Physical Therapy Association Academy of Pelvic Health Physical Therapy and is also a Teaching Assistant with the Herman & Wallace Pelvic Rehabilitation Institute.
Molly is passionate about providing accessible healthcare to pelvic health patients of all age ranges, all gender identities, all sexualities, all body variations, and all ability levels.
She also has experience in a variety of physical therapy settings over the years, including pediatric and adult oncology, school-based pediatrics, inpatient and intensive care unit hospital-based settings, skilled nursing facilities, outpatient and sports-based orthopedics, and wound care.

As of February 2025, 574 bills that restrict the rights of transgender people have been introduced in 48 states.1 Many of these bills seek to limit the inclusion of transgender and nonbinary people, including limiting educational discussions (both anti-LGBTQ+ and gender-focused) and limitations on access to public places or services (e.g., bathrooms). Twenty-five states have now banned best practice medical and surgical treatments for transgender youth2. More notably, in six of these states, providing some of these best practice treatments is now a felony2.
These legislative actions directly contradict the clear positions of leading medical groups, including but not limited to the American Medical Association, the American Academy of Pediatrics, and the World Health Organization, all of which support access to gender-affirming care. The impact of these anti-transgender laws is devastating. Young transgender and nonbinary people living in these states with bans on gender-affirming care are suffering, with suicide attempts spiking by 7% to 72% over the prior year.3 Transgender adults are not immune to the effects of these regressive laws, as they are also experiencing increased rates of depression and anxiety.
Furthermore, while these laws are aimed at impacting transgender and gender diverse populations, they are negatively impacting intersex populations as well. Many of these laws restrict gender-affirming care for transgender, gender nonconforming, and nonbinary (TGD) people, but there are exceptions within these laws that allow non-consensual, non-medically necessary, usually genital-based, surgeries on intersex infants and children to continue. Per the Human Rights Watch, “These surgeries have been deemed human rights violations by the United Nations High Commissioner for Human Rights, the World Health Organization, and other authorities.”6
Not only are transgender laws impacting intersex youth, but recent government orders are as well. In January 2025, the United States government released an executive order that redefined what the words “sex,” “male,” and “female” mean.7 InterACT Advocates for Intersex Youth issued a statement that this order “disrespects the complexity of gender by reducing it to the production of eggs and sperm, entirely fails to consider the existence of intersex people.”5
InterACT further mentions that even cisgender intersex folx may be impacted by this Executive Order stating “Notably, the Executive Order may invalidate a cisgender intersex person’s understanding of their own gender, too. A woman with Complete Androgen Insensitivity (CAIS) may be assigned female at birth, and identify as a woman all her life while having internal testes – yet the Order would define her sex by her gonads and the reproductive cells they produce.”5
Intersex folx historically have had their existence and identities erased, pathologized, and stigmatized. InterACT says that “All people, including young intersex and transgender people, deserve to be respected for who they are.”5 The remote course, Intersex Patients: Rehab and Inclusive Care led by Molly O'Brien-Horn, PT, DPT, CLT, addresses how to be an ally in healthcare to and how to provide better, intersex-affirming healthcare to Intersex folx. The next course offering is on May 3, 2025.
 The American Civil Liberties Union (ACLU) published a research brief on the impacts of these laws and policies stating in part, “These anti-transgender laws are accomplishing exactly what they were designed to do, i.e. prevent youth from obtaining gender-affirming care, reduce gender-affirming care access for adults, prevent transgender and nonbinary people from using correct facilities or participating in sports, or censor education. These impacts are concerning enough; however, the collateral consequences of these laws are also devastating. A growing body of research indicates that these restrictive laws and the surrounding rhetoric are instilling fear, reducing safety, and increasing violence against LGBTQ+ people and their allies.“ Although it can seem frightening and daunting to step up and be an ally, it is what the world needs of all of us, especially in unprecedented times.
The American Civil Liberties Union (ACLU) published a research brief on the impacts of these laws and policies stating in part, “These anti-transgender laws are accomplishing exactly what they were designed to do, i.e. prevent youth from obtaining gender-affirming care, reduce gender-affirming care access for adults, prevent transgender and nonbinary people from using correct facilities or participating in sports, or censor education. These impacts are concerning enough; however, the collateral consequences of these laws are also devastating. A growing body of research indicates that these restrictive laws and the surrounding rhetoric are instilling fear, reducing safety, and increasing violence against LGBTQ+ people and their allies.“ Although it can seem frightening and daunting to step up and be an ally, it is what the world needs of all of us, especially in unprecedented times.
As access to vital care is being challenged, pelvic rehabilitation practitioners have a powerful role in supporting transgender, intersex, and gender diverse people. We can be thoughtful listeners to our patients’ stories, and we can use their chosen names and pronouns. If you’re someone new to chosen names and pronouns, be reassured that no one expects perfection from you when you start out. We all get better with practice. If you need a refresher, check out this simple refresher from the Gay, Lesbian & Straight Education Network. The Herman & Wallace course, Inclusive Care for Gender and Sexual Minorities instructed by Brianna Durand, is also an excellent starting point in learning up-to-date, in-depth knowledge of the various terminology while emphasizing clinical interactions, available research, and professional accountability.
When it comes to pelvic health interventions for trans people who have not had genital surgery, I often encourage clinicians to focus on the basics. The vast majority of pelvic health concerns improve with breathing activities, trunk coordination and strengthening, and mindfulness training. Feel empowered to reach out to rehabilitation forums or mentors for assistance in selecting or adjusting interventions. Also, know who the prescribing medical providers are in your community. Some patients need more testing than PTs and OTs can do. Make yourself part of a strong team.
Clinicians who are ready to be leaders in gender-affirming rehabilitation can take additional training to better understand the nuances of surgery recoveries and interventions. The remote course, Transgender Health for the Rehab Professional: Genital Gender Affirming Surgery Considerations, led by Sandra Gallagher, PT, DPT, WCS and Ken McGee, PT, DPT is a great step. Typical coursework covers dilator progression after vaginoplasty, return to activity after gender-affirming surgery, and understanding the impacts of hormones on pelvic function. The next offering is on April 12, 2025.
If you are looking for more ways to get involved, consider joining the PT Proud Special Interest Group of the Academy of Leadership and Innovation. Protecting and advancing gender-affirming care requires advocacy outside the clinic. The current legislative climate might seem daunting, but the recent court rulings favoring bodily autonomy and the proliferation of shield law for healthcare workers providing gender-affirming care is heartening.
Each of us has the power to make a meaningful difference in the lives of transgender, intersex, and gender-diverse clients. Let’s commit to our ethical duty of justice—ensuring fair and equitable treatment for all, regardless of gender identity—and beneficence—promoting the well-being of every individual we serve.

References
- 2025 Anti-Trans Bills: Trans legislation tracker. 2025 Anti-Trans Bills: Trans Legislation Tracker. Accessed February 22, 2025. https://translegislation.com/.
- Bans on Best Practice Medical Care for Transgender Youth. Movement Advancement Project. February 2025. Accessed February 22, 2025. https://www.lgbtmap.org/equality-maps/healthcare_youth_medical_care_bans.
- American Civil Liberties Union. (2024, September 11). The Impacts of Anti-Transgender Laws and Policies: Evidence from Empirical Research. https://www.aclu.org/publications/the-impacts-of-anti-transgender-laws-and-policies-evidence-from-empirical-
- Lee WY, Hobbs JN, Hobaica S, DeChants JP, Price MN, Nath R. State-level anti-transgender laws increase past-year suicide attempts among transgender and non-binary young people in the USA. Nat Hum Behav. 2024;8(11):2096-2106.
- InterACT Advocates for Intersex Youth. (2025, January 21). Trump’s Executive Order Ignores Science to Push Discriminatory Agenda. https://interactadvocates.org/trumps-executive-order-ignores-science-to-push-discriminatory-agenda/.
- Human Rights Watch. (2022, October 26). S. Anti-Trans Bills Also Harm Intersex Children. https://www.hrw.org/news/2022/10/26/us-anti-trans-bills-also-harm-intersex-children.
- United States Presidential Actions. (2025, January 20). Defending Women from Gender Ideology Extremism and Restoring Biological Truth to the Federal Government Executive Order. https://www.whitehouse.gov/presidential-actions/2025/01/defending-women-from-gender-ideology-extremism-and-restoring-biological-truth-to-the-federal-government/.
By taking a step BACK we can take a step FORWARD to assist individuals with eating disorders. Use your toolbox to build theirs.
Eating disorders are mental health conditions characterized by severe and persistent disturbance in eating behaviors with associated distressing thoughts and emotions that affect an individual’s physical, psychological, and social function. Eating disorders are serious mental illnesses with physical manifestations and serious and sometimes life-threatening medical complications. Common eating disorders are Anorexia Nervosa (AN), Bulimia Nervosa (BN), Binge Eating Disorder (BED), Otherwise Specified Feeding and Eating Disorders (OSFED), and Avoidant Restrictive Food Intake Disorder (ARFID). Pica and Rumination Disorder are also included in the Diagnostic and Statistical Manual of Mental Disorders Text Revision (DSM TR).
Bowel, bladder, and pelvic dysfunction are common with individuals with eating disorders. Fertility and negative effects on both baby and birthing parent are also common. Research is scant regarding pelvic rehabilitation interventions for this important group of individuals. More research is emerging, showing pelvic and gastrointestinal dysfunction with this population; however, pelvic-based rehabilitation has not been readily explored as an option for these individuals until last year.
Dr. Monica Williams, an Occupational Therapist, and colleagues from the ACUTE Center in Denver, Colorado published the first evidence of positive benefits from pelvic rehabilitation approaches with individuals with Anorexia Nervosa in May of 2024. Williams et al. performed a respective cohort study with 193 patients, which demonstrated positive effects in reducing pelvic symptomatology as indicated with improvements in the PFDI-20 (Pelvic Floor Distress Inventory) with one to only a few pelvic-focused sessions. Interventions utilized in this study were aimed at improving function of the pelvic floor musculature, including education, bladder habit retraining, pelvic floor stretches, and biofeedback. This study is an excellent first step in demonstrating that interventions can be helpful even with limited treatment visits and intervention regions. The abdominal region was not a focus of this study.
Pelvic rehabilitation therapists have the skills to assist the patient with strategies to improve comfort and function with urinary, bowel, pelvic, and GI pain and dysfunction. We ALSO have skills to observe, ask questions, support, and advocate for our patients. We may be the first health care professionals who notice signs of an eating disorder or disordered eating. We may be the first to even ask questions to our patients. We can guide an individual to connect with helpful resources. We do NOT have to have all the answers… we just need to LISTEN, SUPPORT, and REFER OUT for additional support. We can also communicate with their permission to their health care providers to provide insight, awareness, and recommend the facilitation of a multidisciplinary team including a skilled mental wellness provider, dietician, and medical provider trained and skilled with individuals with eating disorders. We can also provide health care providers with resources about gaining more information and insight in assessment and treatment for those with suspected disordered eating or eating disorders. There are resources available for primary care providers from the Academy of Eating Disorders to assist with guidance for medical testing and recommendations for patients. (see reference below for downloadable booklet)
We, as pelvic health providers, do NOT treat eating disorders – rather, we provide support and advocate for patients, AND we are able to assist with improving function and comfort related to bowel, bladder, pelvic and gastrointestinal dysfunction and pain. We can utilize the tools we have in our toolbox that we use in our treatments every day.
If we look at ALL individuals through the lens of a “whole package” as compared to a “pelvic box,” this will guide our treatment program…
What’s in YOUR toolbox?
Does an individual present with closed posturing and decreased excursion of the diaphragm? If so, we can work on this! We can provide chest openers, postural instruction, seated modification, costal mobility (caution with impaired bone density), breathing education, and practice. Alas, a way to allow the diaphragm to dance and move to massage the bowels and to stimulate our wonderful vagus nerve.
Does an individual present with urinary or bowel dysfunction or pelvic pain? We have tools to assist with relaxation and re-education of pelvic floor through mindfulness, breathing, manual techniques (direct and indirect techniques), nerve gliding, modalities (heat, TENS, IFC, shockwave, dry needling, pelvic wands, vaginal trainers, etc), biofeedback (for awareness, relaxation and activation of abdominal wall and PF), anorectal balloon training, stretching, positioning, pelvic retraining, toileting strategies, and the list goes on and on!
Does an individual present with abdominal wall dysfunction? We have tools to assist with this including (but not limited to) scar mobilization, colon massage, visceral techniques, soft tissue mobilization, fascial mobilization, strain and counterstain, nerve mobility and gliding, postural education, lymphatic stimulation, vagus nerve facilitation, modalities (heat, IFC, TENS), biofeedback on commode for effective evacuation strategies. You may have other helpful tools in your toolbox – use them!
Does an individual have pelvic girdle or low back pain? We have tools to assist the patient with stretching, manual soft tissue mobilization, myofascial techniques, muscle energy, education, strengthening, postural modification, taping, bracing, etc.
In summary, let’s look at all of our patients as a whole person – and a multifaceted individual. Please take the time to listen, observe, ask questions, advocate, and use YOUR TOOLS to assist building the individual’s own toolbox. Whatever you can provide these individuals to assist with bladder, pelvic, and GI/bowel dysfunction will provide additional comfort and relief. If you have the ability to pursue performing research in this area – please consider this need!
Please join me to expand your toolbox!
- HWConnect 2025 in Seattle WA on March 28-30, 2025. I am a featured speaker on Sunday morning and will be speaking about “Eating Disorders and Disordered Eating: Putting the Pieces Together, and the Hope Pelvic Rehabilitation Can Provide.”
- In my upcoming remote course, Eating Disorders and Pelvic Health Rehabilitation: The Role of a Rehab Professional scheduled for April 26 and 27.
References
- American Psychiatric Association. (2022). Diagnostic and Statistical Manual of Mental Disorders. Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision (DSM-5-TR), 5(5). https://doi.org/10.1176/appi.books.9780890425787
- Baenas, I., Etxandi, M., & Fernández-Aranda, F. (2023). Complicaciones médicas en anorexia y bulimia nerviosa. Medicina Clínica. https://doi.org/10.1016/j.medcli.2023.07.028
- Gibson, D., Watters, A., & Mehler, P. S. (2021). The intersect of gastrointestinal symptoms and malnutrition associated with anorexia nervosa and avoidant/restrictive food intake disorder: Functional or pathophysiologic? A systematic review. International Journal of Eating Disorders, 54(6), 1019–1054. https://doi.org/10.1002/eat.23553
- Guarda, A. (2023, February). What Are Eating Disorders? American Psychiatric Association. https://www.psychiatry.org/patients-families/eating-disorders/what-are-eating-disorders
- Inside Out Institute. (2013). DSM-5 Diagnostic criteria for Eating Disorders. https://insideoutinstitute.org.au/assets/dsm-5%20criteria.pdf
- Medical Care Standards Guide - Academy for Eating Disorders. (2021). Www.aedweb.org. https://www.aedweb.org/resources/publications/medical-care-standards
- Moore, C. A., & Bokor, B. R. (2023). Anorexia Nervosa. National Library of Medicine; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK459148/
- National Institute of Mental Health. (2017, November). Eating disorders. Www.nimh.nih.gov. https://www.nimh.nih.gov/health/statistics/eating-disorders
- Ng, Q. X., Lim, Y. L., Loke, W., Chee, K. T., & Lim, D. Y. (2022). Females with Eating Disorders and Urinary Incontinence: A Psychoanalytic Perspective. International Journal of Environmental Research and Public Health, 19(8), 4874. https://doi.org/10.3390/ijerph19084874
- Şahmelikoğlu Onur, Ö., & Teksin, G. (2023). CLINICAL FEATURES OF WOMEN WITH GENITO-PELVIC PAIN, PENETRATION DISORDER AND DISORDERED EATING ATTITUDES: A CROSS SECTIONAL STUDY. Archives of Neuropsychiatry. https://doi.org/10.29399/npa.28313
- Williams, M., Blalock, D., Foster, M., Mehler, P. S., & Gibson, D. (2024). Pelvic Floor Dysfunction in People with Eating Disorders and the Acute Effect of Different Interventions – A Retrospective Cohort Study. Clinical and Experimental Obstetrics & Gynecology, 51(5). https://doi.org/10.31083/j.ceog5105116
AUTHOR BIO
Carole High Gross, PT, MS, DPT, PRPC

Carole High Gross, PT, MS, DPT, PRPC (she/her) earned her Doctorate of Physical Therapy from Arcadia University in 2015 and her Masters of Science in Physical Therapy in 1992 from Thomas Jefferson University. Carole earned her Pelvic Rehabilitation Practitioner Certification and enjoys working as a Pelvic Clinical Rehabilitation Specialist for Lehigh Valley Health Network. Carole serves as a Lead Teaching Assistant for the Herman and Wallace Pelvic Rehabilitation Institute for pelvic floor education courses. She is also an instructor with the Herman and Wallace Institute for Eating Disorders and Pelvic Health Rehabilitation: The Role of a Rehab Professional. Carole serves on the Pelvic Workgroup of the Ehlers-Danlos International Consortium. Carole has a special interest in working with individuals living with eating disorders and hypermobility throughout the pregnancy and postpartum journey. In addition, Carole enjoys working with all genders with pelvic, bowel, bladder, and abdominal issues. Carole is passionate about lifelong learning. She resides in Bucks County, Pennsylvania, and enjoys spending time with her family and pups.
Regular exercise during pregnancy offers health benefits to both the mother and baby. However, existing evidence suggests that despite being beneficial, the current recommendations of exercise are not being met by many women during pregnancy (Downs 2003, Rebelle 2022). A reason for this could be a lack of guidance. A study by Nascimento showed that less than half of women receive exercise guidance during prenatal care meetings, and nearly half of exercising women stop their participation in exercise during pregnancy.
The American College of Obstetricians and Gynecologists (ACOG) Guidelines of 1985 are still commonly recommended to patients with a hard cut-off of 15 minutes of exercise and a heart rate of 140. However, there has been a significant shift in the mindset of professionals advocating for continued exercise in pregnancy. A hard cut-off for heart rate is difficult to adhere to as maternal heart rate and cardiac output both increase in pregnancy (Tan 2013), and in 2020 the ACOG updated its Guidelines to recommend using both the BORG RPE scale and maternal heart rate. Exercise intensity should be perceived as fairly light to somewhat hard on the Borg Rating of Perceived Exertion (RPE) scale, which ranges from 0 (which is no exertion) to 20 (which is maximal exertion). An easy and practical way to monitor intensity is with the Talk Test.
The current ACOG recommendations encourage 150 minutes of moderate aerobic activity per week during pregnancy and allow for prior levels of physical activity to be continued with OB approval in the absence of medical complications and contraindications. Those initiating exercise in pregnancy need to start slowly with 5 minutes of activity per day and increase slowly by 5 minutes weekly until they are able to exercise 30 minutes per day. Contact sports, activities that may carry a risk of falling or cause the body to become overheated, skydiving, scuba diving, and activities at over 6000 feet are not encouraged during pregnancy (Gascoigne 2023, ACOG 804 opinion).
Running is one way of maintaining exercise during pregnancy, however, many runners discontinue running during pregnancy. In one study, it was found that half the participants who ran before pregnancy reported stopping during pregnancy. During a 2022 study, pregnant runners shared reasons they stopped running, including nausea, fatigue, fear of miscarriage, anxiety, nervousness, and fear. Other factors included discomfort related to baby size and position, along with symptoms of pelvic floor dysfunction (James 2022). Current data suggests that the benefits of regular physical activity in an uncomplicated pregnancy include the possibility of increased uteroplacental blood flow at rest (Clapp 2006), a positive effect on the fetus’s autonomic cardiac regulation (Son 2020), a reduction in the risk of postpartum depression (Vargas- Terrones 2019), and a positive influence on neuro and language development in the first 18 months of age (Nino Cruz 2018).
Gait biomechanics change significantly in pregnancy with a wider step width, reduced hip flexion and extension, decreased stride length, and reduced trunk ROM commonly observed. A lot of these changes are thought to be in response to changes in the center of mass/center of gravity and to maintain balance. Increased ankle stiffness is also noted but is thought to actually have beneficial effects on balance during pregnancy (Conder 2019). Not a lot of research has been conducted on the actual kinematics exhibited by pregnant runners, however, there was a recent study that showed pregnant runners not only run slower but also have decreased trunk and pelvic rotation with increased activation of the Gluteal muscles (Bagwell 2024).
When treating pregnant runners, it may be necessary to make changes to speed (decrease), cadence (increase), and trunk lean in order to continue running. Gluteal muscle function during running is especially important in the pregnant runner. There is evidence that in pregnancy, there is an increase in foot width, shoe size, and dynamic overpronation of the feet (Segal 2010, Segal 2023, Heronemus 2020, Ramachandra 2016). In light of these changes, it is very important to consider new footwear. Other changes to allow continued running include wearing suitable abdominal support garments, braces, and good breast support, especially in the second and third trimesters. Pelvic support may also be necessary and could either be internal (pessary) or external in terms of compression/pelvic support garments.
Some pregnant runners may have pelvic symptoms (incontinence, pressure, heaviness, etc.) and other factors that do not permit them to continue running through pregnancy, but pelvic therapists can do a lot to encourage and support a patient who is pregnant and wants to continue running. Pelvic therapists can not only do a pelvic floor assessment at an appropriate time but can also perform a running form assessment, hip/knee/trunk muscle strength/mobility/kinematic assessment, and offer support via braces, pressure garments, and proper footwear recommendations.
If this topic interests you, then consider signing up for The Runner and Pelvic Health on April 12th. This is a beginner-level, one-day remote course designed to expand the participants’ knowledge of the pelvic floor with running athletes. Through lecture and labs by video and participation, participants will learn what normal and abnormal running mechanics are and how the muscles work simultaneously during running. This course includes advanced assessments to help diagnose the reason for movement dysfunction and is applicable for patients who present with pelvic pain, incontinence, constipation, prolapse, postpartum, and lumbar pain.
References
- Rebelle, Christiana & Jette, Shannon & Mills, John & Tinius, Rachel. (2022). Physical Activity Beliefs and Behaviors during Pregnancy and their Association with Provider Counseling among Women in the Southern United States. Physical Activity and Health. 6. 287. 10.5334/paah.210.
- Symons Downs D, Hausenblas HA. Women's exercise beliefs and behaviors during their pregnancy and postpartum. J Midwifery Womens Health. 2004 Mar-Apr;49(2):138-44. doi: 10.1016/j.jmwh.2003.11.009. PMID: 15010667.
- James, Megan & Moore, Isabel & Donnelly, Grainne & Brockwell, Emma & Perkins, Joanna & Coltman, Celeste. (2022). Running During Pregnancy and Postpartum, Part A: Why Do Women Stop Running During Pregnancy and Not Return to Running in the Postpartum Period? Journal of Women's Health Physical Therapy. Publish Ahead of Print. 10.1097/JWH.0000000000000228.
- Physical Activity and Exercise During Pregnancy and the Postpartum Period: ACOG Committee Opinion, Number 804. Obstet Gynecol. 2020 Apr;135(4):e178-e188. doi: 10.1097/AOG.0000000000003772. PMID: 32217980.
- Gascoigne, Emily L. et al. Physical activity and pregnancy outcomes: An expert review American Journal of Obstetrics & Gynecology MFM, January 2023, Volume 5, Issue 1, 100758
- Tan EK, Tan EL. Alterations in physiology and anatomy during pregnancy. Best Pract Res Clin Obstet Gynaecol. 2013;27:791–802. doi: 10.1016/j.bpobgyn.2013.08.001.
- Nascimento SL, Surita FG, Godoy AC, Kasawara KT, Morais SS. Physical Activity Patterns and Factors Related to Exercise during Pregnancy: A Cross-Sectional Study. PLoS One. 2015 Jun 17;10(6):e0128953. doi: 10.1371/journal.pone.0128953. Erratum in: PLoS One. 2015 Jul 15;10(7):e0133564. doi: 10.1371/journal.pone.0133564. PMID: 26083416; PMCID: PMC4470997.
- Conder R, Zamani R, Akrami M. The Biomechanics of Pregnancy: A Systematic Review. J Funct Morphol Kinesiol. 2019 Dec 2;4(4):72. doi: 10.3390/jfmk4040072. PMID: 33467386; PMCID: PMC7739277.
- ACOG Physical activity and exercise during pregnancy and the postpartum period. Obstet Gynecol. 2020;135:e178–88. doi: 10.1097/AOG.0000000000003772
- Heronemus MJ, Rabe K, Tolstykh I, Gross KD, Wise BL, Nevitt MC, Lewis CE, Hillstrom HJ, Segal NA; MOST Study Group. The Association of Parity with Greater Dynamic Pronation of the Feet. PM R. 2021 Feb;13(2):144-152. doi: 10.1002/pmrj.12381. Epub 2020 May 11. PMID: 32281293; PMCID: PMC7554144.
- Segal N, Eagles MS. The effects of pregnancy on shoe size and knee laxity. Am J Phys Med Rehabil 2010; 89:S41.
- Rabe KG, Segal NA, Waheed S, Anderson DD. The Effect of Arch Drop on Tibial Rotation and Tibiofemoral Contact Stress in Postpartum Women. PM R 2018; 10(11):1137–1144.
- Segal NA, Boyer ER, Teran-Yengle P, Glass NA, Hillstrom HJ, Yack HJ. Pregnancy leads to lasting changes in foot structure. Am J Phys Med Rehabil 2013; 92(3):232–240.
- Ramachandra, Preetha & Kumar, Pratap & Kamath, Asha & Maiya, Arun. (2016). Do Structural Changes of the Foot Influence Plantar Pressure Patterns During Various Stages of Pregnancy and Postpartum? Foot & ankle specialist. 10. 1938640016685150. 10.1177/1938640016685150
- Clapp JF. Influence of endurance exercise and diet on human placental development and fetal growth. Placenta. 2006. Jun‐Jul;27(6‐7):527‐34.
- Son JS, Zhao L, Chen Y, et al. Maternal exercise via exerkine apelin enhances brown adipogenesis and prevents metabolic dysfunction in offspring mice. Sci Adv. 2020;6(16).
- Niño Cruz GI, Ramirez Varela A, da Silva ICM, Hallal PC, Santos IS. Physical activity during pregnancy and offspring neurodevelopment: A systematic review. Paediatr Perinat Epidemiol. 2018. 32(4):369‐79
- Vargas‐Terrones M, Barakat R, Santacruz B, Fernandez‐Buhigas I, Mottola MF. Physical exercise programme during pregnancy decreases perinatal depression risk: a randomised controlled trial. Br J Sports Med. 2019. 53(6):348‐53.
AUTHOR BIO
Aparna Rajagopal, PT, MHS, WCS, PRPC, CAPP-OB-Certified
 Aparna Rajagopal PT, MHS, WCS, PRPC, Capp -OB Certified (she/her) holds a Bachelor of Science degree in Physical Therapy from India and a Master of Health Sciences from the University of Indianapolis. She developed a growing interest in treating pregnant and postpartum patients in 2003. The birth of her daughter in 2006 served as the driving force behind her passion for the field of pelvic dysfunction. She treats men, women, and children with urological, gynecological, and colorectal issues. Her work with female athletes led her to realize the importance of correct breathing techniques in rehabilitation and led her to co-author the breathing and diaphragm class.
Aparna Rajagopal PT, MHS, WCS, PRPC, Capp -OB Certified (she/her) holds a Bachelor of Science degree in Physical Therapy from India and a Master of Health Sciences from the University of Indianapolis. She developed a growing interest in treating pregnant and postpartum patients in 2003. The birth of her daughter in 2006 served as the driving force behind her passion for the field of pelvic dysfunction. She treats men, women, and children with urological, gynecological, and colorectal issues. Her work with female athletes led her to realize the importance of correct breathing techniques in rehabilitation and led her to co-author the breathing and diaphragm class.
She serves as lead therapist for the pelvic dysfunction program at Henry Ford Macomb Hospital, where she mentors and teaches other pelvic therapists. She is a consultant for the hospital's Sports Therapy team for the athletic triad syndrome. She frequently presents and educates physicians, residents, physical therapists, and community support groups on physical therapy treatment for pelvic floor dysfunction. She serves as co-chair of the continuing education committee at her hospital system, where she helps to write and develop courses.
One of my favorite things as the instructor of the Menopause Transitions course is when participants ask questions. Whether it is something about their own menopause journey or when a patient is struggling with symptoms, it thrills me to provide resources and clarity to help them make informed decisions.
The following are some of the questions that have come up in class or that have been brought to my attention via email after participants are back in the clinic:
Given the many benefits of hormone therapy, should every patient take it during or after perimenopause for the prevention of chronic disease?
This is an excellent question! Based on recommendations from The Menopause Society, hormone therapy is approved for the treatment of vasomotor symptoms, genitourinary symptoms, and the prevention of osteoporosis.
Hormones are often lauded as a benefit for reducing both heart disease and dementia. While it has shown some benefit for heart disease, it is not recommended as a preventative treatment. The same holds true for prevention of neurodegenerative disease. The research on the benefits of hormones in cardiovascular and neurodegenerative disease reductions is often looking a different outcomes.
Each study may use a different type of estrogen. An oral estrogen blend (Premarin), an estradiol patch, and an oral estradiol can all have different effects on the body. You simply cannot extrapolate data from one study to the next if the type of estrogen studied was different. In addition, some research shows no benefit. Based on the current data, hormones are not a slam dunk for the prevention of heart disease and dementia. More studies with the types of hormones that are currently being prescribed are needed before recommending them as prevention.
Hormone therapy is very effective for improving bone density. Osteoporosis is a painless process of bone loss. If a person is not experiencing hot flashes and is concerned about their risk for osteoporosis, they could opt for a DEXA scan and then make an informed decision with their provider regarding hormone therapy.
Is there a dose of estrogen that is more beneficial for treating osteoporosis?
In the 2021 position statement for the management of osteoporosis, the Menopause Society cites a study that shows improved bone density with increased dosage. Oral estradiol doses of .02mg, .05mg, and .075mg after 2 years of treatment correlated with an improvement in lumbar spine bone density of .4%, 2.3%, and 2.7% (Greenwald et.al, 2005). While improvement can be gained from a smaller dose, a higher dose does have more benefit. Once again, informed decision-making with a knowledgeable provider is needed.
What are your go-to resources for all things menopause?
Based on the answers to the two previous questions, I think you can see that The Menopause Society is the gold standard when it comes to all things menopause. The position statements are available on their website and can be accessed for free. This includes guidelines on hormones, non-hormonal treatments, genitourinary syndrome of menopause, and osteoporosis. They also have monthly practice pearls, which include many pertinent topics on current treatments and health concerns for the patient in the transition.
Another great resource is Jen Gutner’s The Vagenda. While complete articles require a subscription to her Substack, she does offer a free email version that shares information about many of the topics flying around in the social media sphere. Her opinions are not always popular, but they are always research-based.
A final resource would be Women Living Better. This website was started by women frustrated with their own perimenopause experience and has resources for patients wanting to know more about options for treatment and symptoms experienced during this time. The founders have also been responsible for some interesting research regarding a survey of 3200 women in perimenopause. This is also available on their website.
Keep in mind that there are many social media influencers with millions of followers who also offer information. They have YouTube channels, Instagram, and websites. Menopause seems to be everywhere! While it is extremely valuable to get the message out there, the conclusions offered are often oversimplified in the attempt to push a quick and easy narrative. If I have learned anything in my knowledge journey, it is that there is no one-size-fits-all answer. Treatment is very individualized based on health status, risk factors, and personal preferences. Nuance is the key when it comes to offering the best outcomes.
If you would like to learn more on this topic, then join me on April 26-27, 2025, in Menopause Transitions and Pelvic Rehabilitation to understand more about the physiological consequences to the body as hormones decline and how to assist our patients in lifestyle habits for successful aging.
References:
- The 2020 genitourinary syndrome of menopause position statement of The North American Menopause Society. Menopause, 2020. 27(9): p. 976-992.
- Management of osteoporosis in postmenopausal women: the 2021 position statement of The North American Menopause Society. Menopause, 2021. 28(9): p. 973-997.
- The 2022 hormone therapy position statement of The North American Menopause Society. Menopause, 2022. 29(7): p. 767-794.
- Greenwald, M.W., et al., Oral hormone therapy with 17beta-estradiol and 17beta-estradiol in combination with norethindrone acetate in the prevention of bone loss in early postmenopausal women: dose-dependent effects. Menopause, 2005. 12(6): p. 741-8.
- The Nonhormone Therapy Position Statement of The North American Menopause Society" Advisory, P., The 2023 nonhormone therapy position statement of The North American Menopause Society. Menopause, 2023. 30(6): p. 573-590.
AUTHOR BIO
Christine Stewart, PT, CMPT
 Christine Stewart, PT, CMPT (she/her) graduated from Kansas State University in 1992 and went on to pursue her master’s degree in physical therapy from the University of Kansas Medical Center, graduating in 1994. She began her career specializing in orthopedics and manual therapy, then became interested in women’s health after the birth of her second child.
Christine Stewart, PT, CMPT (she/her) graduated from Kansas State University in 1992 and went on to pursue her master’s degree in physical therapy from the University of Kansas Medical Center, graduating in 1994. She began her career specializing in orthopedics and manual therapy, then became interested in women’s health after the birth of her second child.
Christine developed her pelvic health practice in a local hospital with a focus on urinary incontinence and prolapse. She left the practice in 2010 to work at Olathe Health to further focus on pelvic rehabilitation for all genders and obtain her CMPT from the North American Institute of Manual Therapy. She completed Diane Lee’s Integrated Systems Model education series in 2018. Her passion is empowering patients through education and treatment options for the betterment of their health throughout their lifespan. She enjoys speaking to physicians and to community-based organizations on pelvic health physical therapy.

What do you know about the Americans with Disabilities Act (ADA)? You may be thinking that you are a pelvic health provider, so you don’t need to worry about laws, rules, and regulations. You may need to know more about the ADA than you thought.
Scenario: Your patient calls and requests an American Sign Language interpreter during their pelvic health evaluation. You don’t know much about this. You start to research online, and here is what you find…
Google search answer: “Yes, under the Americans with Disabilities Act (ADA), if your practice is a place of public accommodation (e.g., a healthcare provider), you are generally required to provide effective communication, which may include an ASL interpreter when necessary. However, the law considers "undue burden," meaning if the cost is too high relative to your resources, alternative accommodations (like written communication or remote video interpreting) may be acceptable. You cannot charge the patient for the interpreter.”
You do more research and find out the Americans with Disabilities Act (ADA) is a landmark civil rights law enacted in 1990 that prohibits discrimination against individuals with disabilities in various aspects of public life. It ensures that people with disabilities have the same rights and opportunities as everyone else, covering areas such as employment, public accommodations, transportation, government services, and telecommunications.
Under the ADA, as a pelvic health provider, you will have to provide public accommodations. You may work for a location or be a private business owner, but in either setting, you’ll have to be able to make accommodations. This means being ready to cover physical accessibility (ramps, elevators, bathrooms) and accommodations for people with visual, hearing, or other impairments.
How does this relate to ethics?
Consider the scenario above. You find out that in-person ASL interpreters charge $60 - 90/hour, have a two-hour minimum, and also include paid travel. This means that each visit will cost you between $130 and $250 for just the interpreter. Virtual visits are $1.99 - $2.99 per minute, and the company tells you most deaf people prefer in-person when given the option. The companies you talk to explain that not all deaf people can even use a virtual interpreter. The cancellation windows vary from 48 business hours to 5 business days. You now know that based on the ADA, you have to provide this if you take on this patient, AND you have to pay for this service. What do you do?
An ethical dilemma is the choice between two “right” options. There isn’t a straightforward right versus wrong as there is with an ethical problem. This puts more pressure on the therapist or manager (if the therapist is in a larger organization) to make a judgment call.
The decision you make will likely be based on a few different factors. These are the questions that come to mind for making a decision on this ethical dilemma.
- What is my practice model - fee for service or insurance based?
- How much will I be reimbursed for the therapy session?
- Will this session take more time than other sessions?
- What is my profit margin like?
- Do I have the financial cushion to take on a patient that may actually have my practice losing money?
- How long will the patient need to be seen?
- Is there anyone else in the community I can refer this patient to who may have better resources to accommodate this patient?
- Is the interpreter going to be HIPPA compliant?
- Is the patient going to be comfortable with the interpreter in the room?
- Am I confident the patient will attend appointments regularly?
What would you do as a provider?
I can tell you what our clinic did when this happened. When this patient called, we told them we’d need to take a moment to do some research to find out if we were able to accommodate them. We did our research and were able to find a friend of a friend who was qualified but had better rates than the bigger agencies. We looked at what we HAD to provide and compared that to what we COULD provide, and we decided to take on this patient. Financially, the visit would “net zero,” meaning we wouldn’t make any money, but we also wouldn’t lose money if the patient attended regularly. We felt our clinic was best able to accommodate this patient of the providers in the area. We weighed the pros for the clinic vs. the cons and did the same for the patient and made our decision. That is what we must do every day as a providers. Choosing to refer the patient to an equally qualified location that could accommodate the patient might also have been a good choice.
For pelvic health practitioners, understanding the ADA is crucial when working with individuals who may have disabilities. Some key considerations include:
- Ensuring clinic accessibility (ramps, door widths, exam tables) for individuals with mobility challenges
- Providing communication accommodations for those with speech, hearing, or cognitive impairments
- Offering reasonable modifications to treatment plans for patients with disabilities
- Knowing how legal protections apply when treating patients and ensuring compliance in documentation and practice policies
Ethical dilemmas don’t come with easy answers.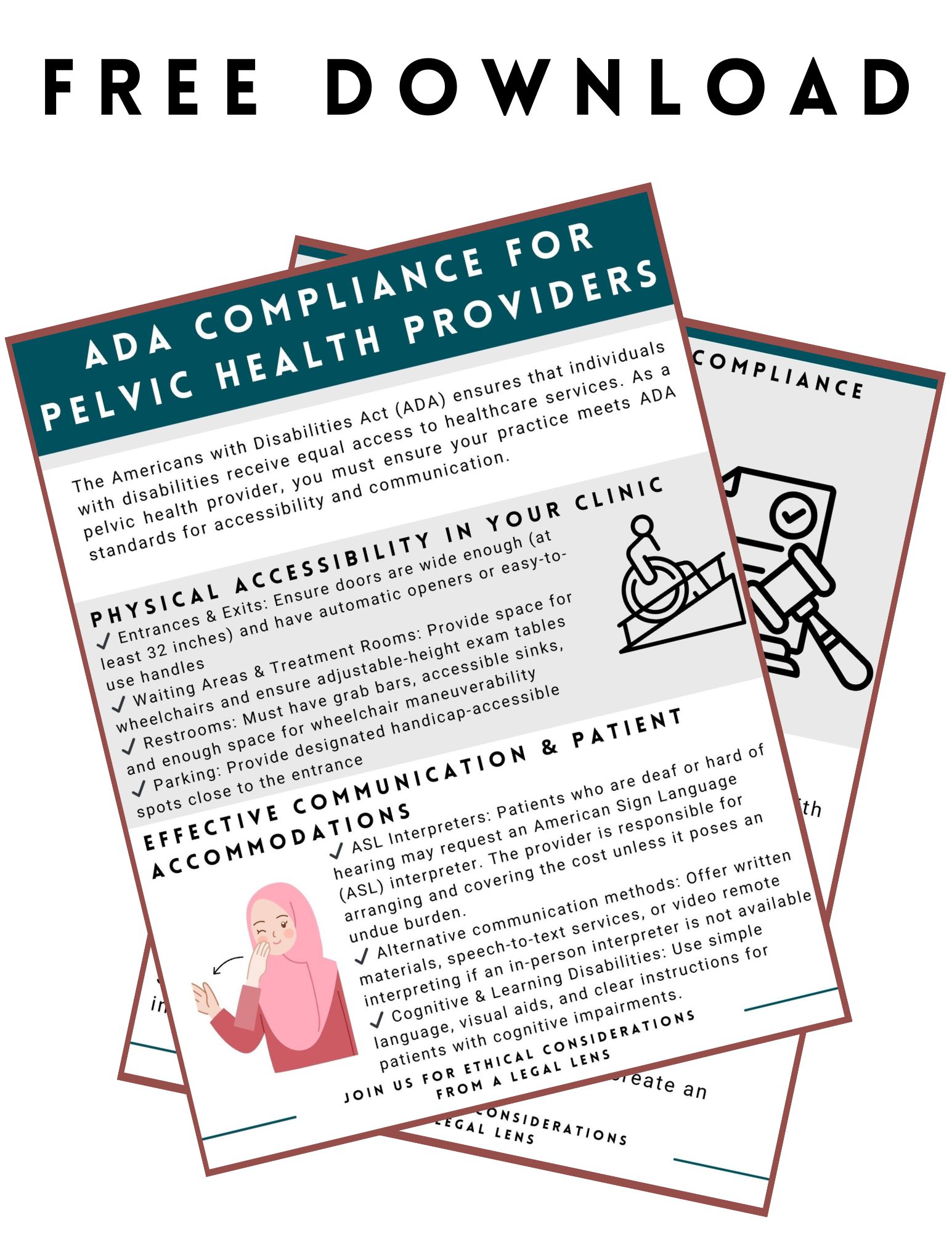 That’s why ongoing education is critical for pelvic health providers. Understanding both the ethical and legal implications of our work ensures that we protect our patients, our licenses, and our professional integrity.
That’s why ongoing education is critical for pelvic health providers. Understanding both the ethical and legal implications of our work ensures that we protect our patients, our licenses, and our professional integrity.
For those looking to deepen their knowledge in this area, the Ethical Considerations from a Legal Lens course is a must-attend event. Taking place remotely on April 12, 2025, this course is designed to provide pelvic health practitioners with the tools they need to navigate real-world ethical challenges with confidence.
What You’ll Gain from the Course
- A deeper understanding of legal considerations in pelvic health practice
- Strategies to navigate informed consent and patient autonomy
- Insights into trauma-informed care and how to approach sensitive patient cases
- Tools to manage professional boundaries and ethical decision-making
- Interactive discussions and case studies to help apply concepts in real scenarios
As providers, we want to deliver the best care possible while ensuring that our practice remains ethical, respectful, and legally sound. Education is the key to making that happen. If you’re ready to strengthen your ethical knowledge and enhance your practice, sign up for the Ethical Considerations from a Legal Lens course today!
Freebie:
ADA Compliance for Pelvic Health Providers - Free Download Reference
AUTHOR BIO
Mora Pluchino, PT, DPT, PRPC
 Mora Pluchino, PT, DPT, PRPC (she/her) is a graduate of Stockton University with a BS in Biology (2007) and a Doctorate of Physical Therapy (2009). She has experience in a variety of areas and settings, working with children and adults, including orthopedics, bracing, neuromuscular issues, vestibular issues, and robotics training. She began treating Pelvic Health patients in 2016 and now has experience treating pelvises and ages with a variety of Pelvic Health dysfunctions. There is not much she has not treated since beginning this journey, and she is always happy to further her education to better help her patients meet their goals.
Mora Pluchino, PT, DPT, PRPC (she/her) is a graduate of Stockton University with a BS in Biology (2007) and a Doctorate of Physical Therapy (2009). She has experience in a variety of areas and settings, working with children and adults, including orthopedics, bracing, neuromuscular issues, vestibular issues, and robotics training. She began treating Pelvic Health patients in 2016 and now has experience treating pelvises and ages with a variety of Pelvic Health dysfunctions. There is not much she has not treated since beginning this journey, and she is always happy to further her education to better help her patients meet their goals.
Dr. Pluchino strives to help all of her patients return to a quality of life and activity that they are happy with for the best bladder, bowel, and sexual functioning they are capable of at present. In 2020, she opened her own practice called Practically Perfect Physical Therapy to help meet the needs of more clients. She has been a guest lecturer for Rutgers University's Blackwood Campus and Stockton University for their Pediatric and Pelvic Floor modules since 2016. She has also been a TA with Herman & Wallace since 2020 and has over 150 hours of lab instruction experience. Mora has also authored and instructs several courses for the Institute.

Pilates has always had a place in rehab and was used frequently by those (think ballet dancers and performers) who needed a system of exercise that could challenge the neuromuscular system to bring them back to a high level of function. But Joseph Pilates created his “Method” to heal himself—he suffered from asthma, rickets, and rheumatic fever—and in doing so, made it suitable for all types of people at all stages of health and wellness.
Do you long to try that Reformer in your clinic but feel you have not had the training necessary to use it safely beyond a glorified squat machine? Come experience Pilates movement in my new course, Pilates Therapeutic Exercise in Pelvic Health, scheduled for May 3-4, 2025. By using your therapeutic exercise training, we will choose appropriate traditional Pilates exercises to apply to common pelvic floor and pelvic girdle dysfunction. This course is meant to focus on specific diagnoses like prolapse prevention, urinary incontinence, and postpartum abdominal wall activation. This is not Pilates training—there are many suitable courses for this goal - but rather it is to whet your appetite to further your training and give you explicit examples of Pilates exercises to help your patient.
We will review how to safely set up the reformer for patients and see how select exercises can transform core activation by doing rather than telling folks about the movement. Using the Reformer is a wonderful neuro reeducation tool -- utilizing springs, one can instantly create tension that will act as an active assist for muscle groups or modify it to be one that is resistive, creating activation of muscle contraction. Additionally, you can access many developmental postures on the Reformer that can help your patient succeed. Combined with good verbal and tactile cues, the Reformer is a go-to for my pelvic floor patients with pain, ROM issues, and/or weakness, and I can’t wait to share!
AUTHOR BIO
Pam Downey, PT, MSPT, DPT, WCS, BCB-PMD, PRPC
 Pam Downey, PT, MSPT, DPT, WCS, BCB-PMD, PRPC (she/her) is a Board Certified Clinical Specialist in Women’s Health Physical Therapy and Board Certified in Biofeedback for Pelvic Muscle Dysfunction. Owner of Partnership in Therapy, a private practice in Coral Gables, Florida, she treats pelvic floor dysfunction, related urogynecological and colorectal issues, spine dysfunction, osteoporosis, and complaints associated with pregnancy and the postpartum period. Her mission is to educate and integrate healthy lifestyles for patients on the road to wellness.
Pam Downey, PT, MSPT, DPT, WCS, BCB-PMD, PRPC (she/her) is a Board Certified Clinical Specialist in Women’s Health Physical Therapy and Board Certified in Biofeedback for Pelvic Muscle Dysfunction. Owner of Partnership in Therapy, a private practice in Coral Gables, Florida, she treats pelvic floor dysfunction, related urogynecological and colorectal issues, spine dysfunction, osteoporosis, and complaints associated with pregnancy and the postpartum period. Her mission is to educate and integrate healthy lifestyles for patients on the road to wellness.
Dr. Downey has been honored to teach with the Herman & Wallace Institute since 2006. She is an Adjunct Professor in the Physical Therapy Program at the University Of Miami Miller School of Medicine in Coral Gables, Florida, and Nova Southeastern University in Fort Lauderdale, Florida. A certified Polestar Pilates Educator, she utilizes Pilates and therapeutic exercise interventions specifically designed for patients with pre/post-natal, pelvic floor muscle, and other lumbo-pelvic pain-related dysfunctions.
Dr. Downey received her Bachelor of Arts from Sarah Lawrence College and her Master of Science and Doctorate in Physical Therapy from the University of Miami School of Medicine. She is actively involved in professional activities of the Section on Women’s Health of the American Physical Therapy Association, presently sitting as Coordinator of Research Submissions for annual meetings and as a manuscript reviewer for the Journal of Women’s Health. Dr. Downey has lectured nationally and internationally at professional conferences and is the author of multiple published research articles and a book chapter on chronic pelvic pain in the medical text, Women’s Health in Physical Therapy.

Hi, I’m Deb Gulbranson, co-creator of the course Osteoporosis Management: An Introductory Course for Healthcare Professionals. Along with my partner, Frank Ciuba, we have created a program based on the works of Sara Meeks, whom we taught with for many years.
We know that posture is important, and we may include it in our evaluations, but how do we objectively measure it? How much time do we spend on education, training, exercises, and return demonstration? Chances are, not as much as we should.
Optimal alignment affects our breathing, balance, efficiency of gait, digestion, AND bone density.
In order to increase bone density, we need to weight bear through the skeleton, not in front of it. Compression fractures occur along the anterior aspect of the vertebral bodies. Strengthening the back extensors has also been shown to increase bone density. Therefore, someone with a hyper-kyphotic posture of the thoracic spine is at risk for fracture due to increased pressure anteriorly and overstretched, weakened musculature posteriorly. Statistics show that 1:2 women and 1:4 men will have a fragility fracture due to low bone mass.
How do we objectively measure and describe a person’s alignment?
 A quick and simple way is using a wall and measuring tape. Have your patient stand with their heels, sacrum, and thoracic apex of the spine against the wall. There are two options to measure using the OWD or the TWD. Occiput to Wall Distance or Tragus to Wall Distance. The Tragus is the small bump of cartilage in front of the ear canal. Both OWD and TWD have a positive relationship with the Cobb angle, and although they’re not as specific, they are both equally effective. It’s a matter of preference. Frank prefers the TWD since it’s easier to see and measure. However, the score does not tell you how far away from the wall the head is. There will always be a positive number based on the size and shape of the head.
A quick and simple way is using a wall and measuring tape. Have your patient stand with their heels, sacrum, and thoracic apex of the spine against the wall. There are two options to measure using the OWD or the TWD. Occiput to Wall Distance or Tragus to Wall Distance. The Tragus is the small bump of cartilage in front of the ear canal. Both OWD and TWD have a positive relationship with the Cobb angle, and although they’re not as specific, they are both equally effective. It’s a matter of preference. Frank prefers the TWD since it’s easier to see and measure. However, the score does not tell you how far away from the wall the head is. There will always be a positive number based on the size and shape of the head.
I prefer the OWD because whatever the measurement is, it tells me how far forward the head is. 0 equals optimal alignment. The downside is that it’s a little harder to pinpoint the most prominent point of the occiput.
In both cases, the measurement gives us a baseline to measure against. These can be used as screens in a health fair, during a PT screen for patients without a diagnosis of low bone density, and certainly as part of a full eval for patients with known osteoporosis, a compression fracture, or even osteopenia.
These measures, taken periodically, can be very motivating for patients. Generally, we see not only a decrease in the hyper-kyphosis distance but also an increase in height.
This is only one of several ways to assess and describe posture and alignment. We hope you’ll consider joining us to learn more about the treatment protocols and exercise programs in our upcoming Osteoporosis Management course on April 26th.
AUTHOR BIO
Deb Gulbrandson, PT, DPT
 Deb Gulbrandson, DPT (she/her) has been a physical therapist for over 49 years with experience in acute care, home health, pediatrics, geriatrics, sports medicine, and consulting to business and industry. She owned a private practice for 27 years in the Chicago area specializing in orthopedics and Pilates. 5 years ago, Deb and her husband “semi-retired” to Evergreen, Colorado where she works part-time for a hospice and home-care agency, sees private patients as well as Pilates clients in her home studio and teaches Osteoporosis courses for Herman & Wallace. In her spare time, she skis and is busy checking off her Bucket List of visiting every national park in the country- currently 46 out of 63 and counting.
Deb Gulbrandson, DPT (she/her) has been a physical therapist for over 49 years with experience in acute care, home health, pediatrics, geriatrics, sports medicine, and consulting to business and industry. She owned a private practice for 27 years in the Chicago area specializing in orthopedics and Pilates. 5 years ago, Deb and her husband “semi-retired” to Evergreen, Colorado where she works part-time for a hospice and home-care agency, sees private patients as well as Pilates clients in her home studio and teaches Osteoporosis courses for Herman & Wallace. In her spare time, she skis and is busy checking off her Bucket List of visiting every national park in the country- currently 46 out of 63 and counting.
Deb is a graduate of Indiana University and a former NCAA athlete, where she competed on the IU Gymnastics team. She has always been interested in movement and function and is grateful to combine her skills as a PT and Pilates instructor. She has been certified through Polestar Pilates since 2005, a Certified Osteoporosis Exercise Specialist through the Meeks Method since 2008, and a Certified Exercise Expert for the Aging Adult through the Geriatric Section of the APTA.

According to the Parkinson’s Foundation, orthostatic hypotension (OH) affects 15 to 50% of people with Parkinson disease (PWP). The medical definition of orthostatic hypotension is a drop in systolic blood pressure of greater than 20 mmHg or a drop in diastolic blood pressure of greater than 10 mmHg within 3 minutes of standing. Additionally, consideration is taken to the heart rate increase upon standing and if less than 10-15 beats per minute, it may be indicative of OH.
One of the many lifestyle modifications given is to increase fluid intake. Increasing fluids for blood pressure management to reduce dizziness, syncope, and fall risk from OH can be very challenging for this population. Many PWP present with significant self-imposed fluid restrictions as they try to manage common issues with bladder urgency frequency. Getting ½ their body weight in ounces or the traditional recommendation of 8 glasses a day may feel overwhelming. A common recommendation from their neurologist or other health care providers is to have 16 ounces of fluid right away in the morning. Research has shown this to help individuals with autonomic nervous system/baroreflex dysfunction to have rapid symptomatic improvement eliciting a water-induced pressure response and raising their blood pressure. In PWP with autonomic dysfunction, the baroreceptors, which constrict to increase heart rate and blood pressure upon standing, are sluggish to respond similar to the slowness of movement observed in a PWP. Individualized and creative daytime urge control techniques, bladder retraining, timed voiding, measured bladder diary assessment, constipation management strategies, and neuromodulation strategies are crucial to maintaining quality of life in coordination with fall safety related to OH.
For those with OH who also struggle with nocturia, the shifting of fluids to earlier in the day may require closer monitoring of blood pressure to ensure our advice is safe. The Wisconsin Parkinson Association’s director of medical advising and education, Dacy Reimer, APNP, describes the recommended blood pressure tracking methods for reporting back to neurology. With the use of an electronic blood pressure cuff, blood pressure, pulse, and symptoms can be recorded after sitting for 5 minutes and a second blood pressure after standing for 3 minutes. This can be regularly tracked once in the morning and once at night. If we are giving advice for fluid management changes to modify bladder behavior, we may want our patients to monitor this at additional times throughout the day. Many of my patients who report nocturia at their evaluation, have already tried the common recommendation of stopping fluids 2-3 hours before bed without a change in their symptoms. A more aggressive fluid shifting plan, where the person will still be asked to get their recommended fluids each day, but achieve that goal much earlier, with a more dramatic tapering at the end of the day has clinically shown benefit. Trying to fill the bladder more during the day to allow for sensory training/larger fill volumes as well as to flip the circadian rhythm for urine production is the goal. Monitoring blood pressure as an additional component of the bladder diary, while your patient makes suggested changes, can ensure their safety.
If additional nuances to the pelvic health complexities involved in Parkinson disease interest you, come delve into it with me even further in my course - Parkinson Disease and Pelvic Rehabilitation scheduled for April 25-26 2025.
Resources:
- Ramsay, S., & Zagorodnyuk, V. (2023). Role of circadian rhythms and melatonin in bladder function in heath and diseases. Autonomic neuroscience, 246, 103083.
- Shannon, J. R., Diedrich, A., Biaggioni, I., Tank, J., Robertson, R. M., Robertson, D., & Jordan, J. (2002). Water drinking as a treatment for orthostatic syndromes. The American journal of medicine, 112(5), 355-360.
AUTHOR BIO:
Erica Vitek, MOT, OTR, BCB-PMD, PRPC
 Erica Vitek, MOT, OTR, BCB-PMD, PRPC (she/her) graduated with her master’s degree in Occupational Therapy from Concordia University Wisconsin in 2002 and works for Aurora Health Care at Aurora Sinai Medical Center in downtown Milwaukee, Wisconsin. Erica specializes in female, male, and pediatric evaluation and treatment of the pelvic floor and related bladder, bowel, and sexual health issues. She is board-certified in Biofeedback for Pelvic Muscle Dysfunction (BCB-PMD) and is a Certified Pelvic Rehabilitation Practitioner (PRPC) through Herman and Wallace Pelvic Rehabilitation Institute.
Erica Vitek, MOT, OTR, BCB-PMD, PRPC (she/her) graduated with her master’s degree in Occupational Therapy from Concordia University Wisconsin in 2002 and works for Aurora Health Care at Aurora Sinai Medical Center in downtown Milwaukee, Wisconsin. Erica specializes in female, male, and pediatric evaluation and treatment of the pelvic floor and related bladder, bowel, and sexual health issues. She is board-certified in Biofeedback for Pelvic Muscle Dysfunction (BCB-PMD) and is a Certified Pelvic Rehabilitation Practitioner (PRPC) through Herman and Wallace Pelvic Rehabilitation Institute.
Erica has attended extensive post-graduate rehabilitation education in the area of Parkinson disease and exercise. She is certified in LSVT (Lee Silverman) BIG and is a trained PWR! (Parkinson’s Wellness Recovery) provider, both focusing on intensive, amplitude, and neuroplasticity-based exercise programs for people with Parkinson disease. Erica is an LSVT Global faculty member. She instructs both the LSVT BIG training and certification course throughout the nation and online webinars. Erica partners with the Wisconsin Parkinson Association (WPA) as a support group, event presenter, and author in their publication, The Network. Erica has taken a special interest in the unique pelvic floor, bladder, bowel, and sexual health issues experienced by individuals diagnosed with Parkinson disease.

Any pelvic floor rehabilitation provider knows that pregnancy can lead to changes in the pelvic floor and the abdominal wall. In the postpartum period, many individuals would like to strengthen their pelvic floor and abdominal muscles in an attempt to return to fitness and previous exercise routines. Is there a difference in how someone approaches training these muscles in the postpartum period? Will activating the muscles cause harm for our patients? This can be controversial amongst pelvic rehabilitation providers. I have heard some clinicians say that once a patient has had a pregnancy and vaginal birth, then they should never do sit-ups again, instead they should work the abdominal muscles in different ways. Others argue it depends on the individual patient.
A recent study examined the effects of different types of abdominal contractions on the positioning of the pelvic organs in nulliparous and postpartum women. Six different pelvic floor and abdominal contractions were tested, and the bladder positioning was examined using ultrasound imaging. There was significantly more lift of the bladder base when a submaximal contraction of the pelvic floor and transverse abdominis were performed with an elongation of the back. With a curl-up contraction, there was a significant amount of descent of the bladder base (Martinez-Bustelo, 2021). This increased descent of the bladder demonstrates that the choice of abdominal activation does make a difference and influences the pelvic organs. However, the overall individuality of the patient makes a difference as well. The overall management of the internal pressure system for the individual can influence the descent of the pelvic organs positively or negatively. Additionally, patients who have a diastasis recti abdominis may have additional precautions when wanting to exercise their abdomen and core.
How can clinicians observe the supportive component of the pelvic floor?
Ultrasound imaging can be performed quickly and easily, allowing the practitioner to view the pelvic organs and their response to different types of contractions. This can allow us to customize a program for post-partum individuals that are wanting to return to fitness and exercise activities and make sure that the patient is not exerting pressure into their pelvic area in a way that is not ideal. Ultrasound imaging also allows clinicians to treat postpartum patients sooner. We can treat them immediately in the postpartum period. We do not need to wait until the patient is cleared for internal work or deal with lochia for an external assessment. We are able to immediately help our post-partum patients through abdominal imaging.
You can learn to use ultrasound imaging through Herman & Wallace’s Rehabilitative Ultrasound Course. This course guides you through the process of learning to use ultrasound imaging transabdominally and transperineally to assist your post-partum patients in regaining core and pelvic organ strength. This tool is also useful for other diagnoses including anyone with lumbopelvic pain, pelvic floor weakness, and pelvic organ prolapse. Join us this April to learn more about ultrasound imaging!
Upcoming course details:
- Rehabilitative Ultrasound Imaging - Pelvic Health and Orthopedic Topics is a 3-day course that presents both ideal and abnormal responses of real-time imaging of the transverse abdominals, rectus abdominis, deep multifidus, levator ani, bladder, bladder neck, urethra, and vagina during contraction and Valsalva. Imaging methods used during labs will consist of transabdominal viewing as well as transperineal/translabial viewing methods. Prior experience with perineal and vaginal assessments is required to take the course.
- Rehabilitative Ultrasound Imaging - Orthopedic Topics is a 2-day course that presents both ideal and abnormal responses of real-time imaging of the transverse abdominals, rectus abdominis, deep multifidus, levator ani, bladder, and bladder neck.
- You can also meet Allison and get a hands-on demonstration of rehabilitative ultrasound at HWConnect.
Reference:
- Martínez-Bustelo, S., Ferri-Morales, A., Corral-Gómez, L. et al. Transabdominal ultrasound to assess the displacement of the bladder base during abdominal and pelvic floor contractions in continent parous versus nulliparous women. Int Urogynecol J 33, 2257–2266 (2022). https://doi.org/10.1007/s00192-021-04756-4
AUTHOR BIO
Allison Ariail, PT, DPT, CLT-LANA, BCB-PMD, PRPC
 Allison Ariail has been a physical therapist since 1999. She graduated with a BS in physical therapy from the University of Florida and earned a Doctor of Physical Therapy from Boston University in 2007. Also in 2007, Dr. Ariail qualified as a Certified Lymphatic Therapist. She became board-certified by the Lymphology Association of North America in 2011 and board-certified in Biofeedback Pelvic Muscle Dysfunction by the Biofeedback Certification International Alliance in 2012. In 2014, Allison earned her board certification as a Pelvic Rehabilitation Practitioner. Allison specializes in the treatment of the pelvic ring and back using manual therapy and ultrasound imaging for instruction in a stabilization program. She also specializes in women’s and men’s health including conditions of chronic pelvic pain, bowel and bladder disorders, and coccyx pain. Lastly, Allison has a passion for helping oncology patients, particularly gynecological, urological, and head and neck cancer patients.
Allison Ariail has been a physical therapist since 1999. She graduated with a BS in physical therapy from the University of Florida and earned a Doctor of Physical Therapy from Boston University in 2007. Also in 2007, Dr. Ariail qualified as a Certified Lymphatic Therapist. She became board-certified by the Lymphology Association of North America in 2011 and board-certified in Biofeedback Pelvic Muscle Dysfunction by the Biofeedback Certification International Alliance in 2012. In 2014, Allison earned her board certification as a Pelvic Rehabilitation Practitioner. Allison specializes in the treatment of the pelvic ring and back using manual therapy and ultrasound imaging for instruction in a stabilization program. She also specializes in women’s and men’s health including conditions of chronic pelvic pain, bowel and bladder disorders, and coccyx pain. Lastly, Allison has a passion for helping oncology patients, particularly gynecological, urological, and head and neck cancer patients.
In 2009, Allison collaborated with the Primal Pictures team for the release of the Pelvic Floor Disorders program. Allison's publications include: “The Use of Transabdominal Ultrasound Imaging in Retraining the Pelvic-Floor Muscles of a Woman Postpartum.” Physical Therapy. Vol. 88, No. 10, October 2008, pp 1208-1217. (PMID: 18772276), “Beyond the Abstract” for Urotoday.com in October 2008, “Posters to Go” from APTA combined section meeting poster presentation in February 2009 and 2013. In 2016, Allison co-authored a chapter in “Healing in Urology: Clinical Guidebook to Herbal and Alternative Therapies.”
Allison works in the Denver metro area in her practice, Inspire Physical Therapy and Wellness, where she works in a more holistic setting than traditional therapy clinics. In addition to instructing Herman and Wallace on pelvic floor-related topics, Allison lectures nationally on lymphedema, cancer-related changes to the pelvic floor, and the sacroiliac joint. Allison serves as a consultant to medical companies, and physicians.
By accepting you will be accessing a service provided by a third-party external to https://hermanwallace.com/









































