Prolapse Assessment: Is One Attempt Enough?
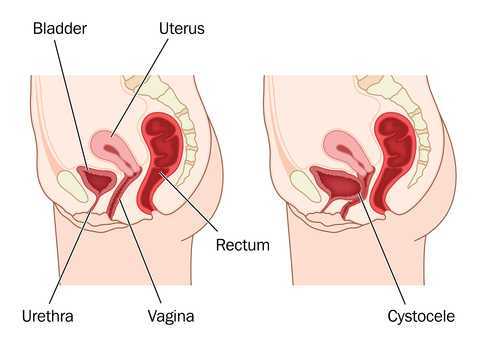
When examining a patient clinically for pelvic wall relaxation or pelvic organ prolapse, we know that verbal cues given, position of the patient, time of day, bladder fullness, and other variables can affect the outcome of the prolapse evaluation. What about the number of attempts at bearing down or straining during the examination? Is one attempt at bearing down enough to provide clear information about the level of descent or relaxation in the pelvic walls or organs? If research based on dynamic MRI's is any indication, the answer may be "no."
40 women with an anterior wall prolapse that extended at least 1 cm beyond the hymenal ring were evaluated with dynamic MRI scans. The subjects were instructed in and evaluated for their ability to properly bear down prior to the scans. Between the first, second, and third maximal efforts at bearing down, or Valsalva, bladder descent was measured during dynamic magnetic resonance imaging (MRI). In 95% of the women, prolapse measurements were more significant by the third effort at bearing down. 40% of the women demonstrated more than a 2 centimeter increase in prolapse from the first to third attempt at Valsalva. In this research study the mean age of the subjects was about 60 years old, and 80% of the women were Caucasian. Childbirth history averaged 2 vaginal births and eight of the women had a prior hysterectomy.
While the authors discuss the value of using this diagnostic information to create improved dynamic MRI protocols, there may also be implications for the pelvic rehabilitation provider. When we are assessing for the integrity of the pelvic supporting structures, are we getting a reliable effort from the patient? Are we asking for more than one attempt at bearing down? In addition to considering relevant issues like the time of day or the position of the patient during an examination, we can also consider the number of times that the testing is completed. If we ask for only one attempt at bearing down, perhaps we are not being provided with the most accurate information. What we do with that information is the next important step in developing a plan of care or communicating with the referring provider. In the Pelvic Floor Level 1 (PF1) continuing education course, therapists learn how to assess for pelvic organ prolapse, and in the PF2B course therapists learn additional information about the fascial layers that, when not intact, can contribute to pelvic organ displacement. Providing interventions that address myofascial dysfunction and functional use patterns of the trunk and limbs can help a woman overcome symptoms of prolapse, and working together with medical providers to help women with prolapse can be very rewarding.
By accepting you will be accessing a service provided by a third-party external to https://hermanwallace.com/





































