Testicular Cancer: Seeking to Spare the Sperm
My little boy has a t-shirt with a potato telling french fries, “I am your father,” to which the french fries cry, “NO!!!!” The Star Wars spoof makes me laugh, but sometimes the struggle is real. Testicular cancer and the toxic remedies for it can potentially prevent young men from having a successful reproductive life. Survivors of the cancer may one day have to tell their children they are adopted or came from a sperm donor. With the advances in technology and research, however, testicular cancer survivors have a greater chance for their own sperm to be spared or even produced naturally years later to create their offspring.
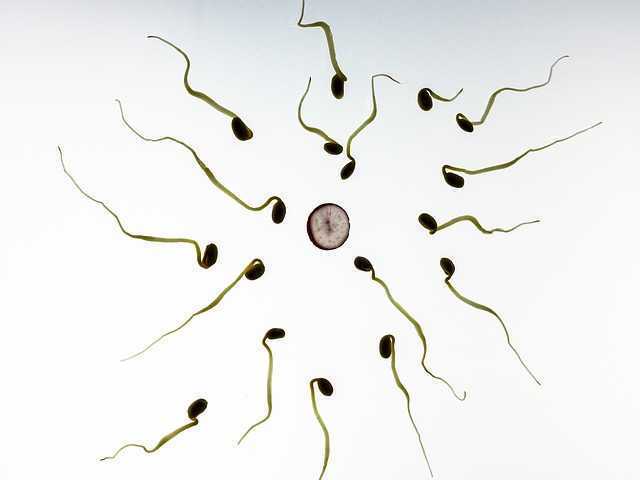 Vakalopoulos et al. (2015) discussed the impact cancer and the related treatments have on fertility of males. Better survival rates for oncology patients have made preservation of reproductive means more imperative for men. Testicular cancer represents 5% of male urologic cancers, disturbing spermatogenesis and impairing fertility. Chemotherapy, radiotherapy, and surgery can all have gonadotoxic effects in men. Thankfully, only 1 in 5000 men die from testicular cancer now with advanced treatments, but fertility does become a long term factor for survivors. This paper showed chemotherapy combined with radiotherapy was most detrimental to sperm than either treatment alone. Gonadal shielding and moving the testes out of the way to target the malignant cells can help decrease the deleterious effects of cancer treatments. Radiotherapy, however, has been shown to damage sperm up to 2 years after recovery of spermatogenesis. Regarding surgery, radical unilateral orchiectomy is the standard for testicular tumors, and within the first few months, a 50% decrease in sperm concentration occurs, and 10% of patients become azoospermic. On a more encouraging note, after receiving Hematopoietic Stem Cell Transplantation, recovery of sperm in the ejaculate was noted in 33% of patients after 1 year and 80% of patients after 7 years.
Vakalopoulos et al. (2015) discussed the impact cancer and the related treatments have on fertility of males. Better survival rates for oncology patients have made preservation of reproductive means more imperative for men. Testicular cancer represents 5% of male urologic cancers, disturbing spermatogenesis and impairing fertility. Chemotherapy, radiotherapy, and surgery can all have gonadotoxic effects in men. Thankfully, only 1 in 5000 men die from testicular cancer now with advanced treatments, but fertility does become a long term factor for survivors. This paper showed chemotherapy combined with radiotherapy was most detrimental to sperm than either treatment alone. Gonadal shielding and moving the testes out of the way to target the malignant cells can help decrease the deleterious effects of cancer treatments. Radiotherapy, however, has been shown to damage sperm up to 2 years after recovery of spermatogenesis. Regarding surgery, radical unilateral orchiectomy is the standard for testicular tumors, and within the first few months, a 50% decrease in sperm concentration occurs, and 10% of patients become azoospermic. On a more encouraging note, after receiving Hematopoietic Stem Cell Transplantation, recovery of sperm in the ejaculate was noted in 33% of patients after 1 year and 80% of patients after 7 years.
Regardless of advancements in decreasing toxicity of cancer treatments and being minimally invasive with surgery, the best guarantee for preservation of sperm is cryopreservation.
A study collecting baseline data for semen quality of cancer patients prior to any gonadotoxic treatment was performed by Auger et al. (2016). Less than 60% of the testicular cancer patients had normal sperm production prior to treatment. The study also looked at patients with Hodgkin’s disease, non-Hodgkin’s Lymphoma, Leukemia, sarcoma, Behcet’s disease, brain tumor, and Multiple Sclerosis. The motility of sperm after freezing (cryopreservation) of the cancer patients was less than half of the healthy sperm donor control group. Intra Cytoplasmic Sperm Injection (ICSI) was shown to provide the best chance of paternity for men, and the authors conclude this as a necessary step in case men do not regain any spermatogenesis after cancer treatment.
There is no perfect circumstance when it comes to cancer. Survival is the primary goal, and then quality of life becomes the “problem,” particularly when it comes to fulfilling dreams of having a family. The toxic cancer treatments are improving but cannot guarantee return of spermatogenesis. Depending on the sperm integrity prior to getting treatment, cryopreservation success can vary but is the most highly recommended step to preserving fertility. In the end, a fresh or frozen spud can still make french fries.
Herman & Wallace has two great courses which can give you the tools needed to help assess and treat male patients who suffer from cancer-related dysfunctions. Consider Oncology and the Male Pelvic Floor: Male Reproductive, Bladder, and Colorectal Cancers or Post-Prostatectomy Patient Rehabilitation for your next continuing education courses.
Vakalopoulos, I., Dimou, P., Anagnostou, I., Zeginiadou T. (2015). Impact of cancer and cancer treatment on male fertility. Hormones. 14(4):579-89. DOI: 10.14310/horm.2002.1620
Auger, J., Sermondade, N., & Eustache, F. (2016). Semen quality of 4480 young cancer and systemic disease patients: baseline data and clinical considerations. Basic and Clinical Andrology, 26, 3. http://doi.org/10.1186/s12610-016-0031-x
By accepting you will be accessing a service provided by a third-party external to https://hermanwallace.com/




































