Obturator Internus & Making Connections
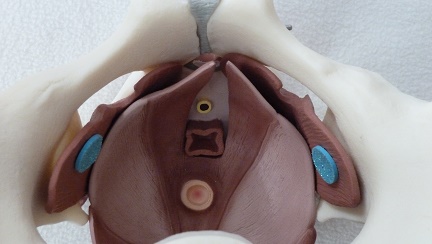
As a physical therapist I am continually amazed at the myriad of ways the parts of our bodies are connected (and even more so by our brain/body connections, but that is another blog post.) Take one of my favorite muscles for example, the obturator internus. This amazing muscle is known for its relationship to the hip as one of the external rotators, and it’s anatomy is impressive! What other muscle sharply turns ninety degrees from its attachment to its origin? The obturator internus traverses the inside of the pelvis and attaches mid-belly to an important tendon, the Arcuate Tendon Levator Ani (ATLA) , which becomes the means by which the obturator connects to the pelvic floor. (I love to show patients how their hip literally connects to their pelvis!) The ATLA connects with the Arcuate Tendon Fascia Pelvis which connects to the fascia supporting the bladder and urethra.
We know that in our patient who have pelvic pain too much tension or trigger points in the obturator internus can create symptoms of urinary urgency or frequency, pain in the bladder, vagina, rectum, abdomen, pelvic floor and hip. But what happens when the obturator internus is uptrained to treat women with stress urinary incontinence (SUI)? An article in the May/August 2014 Journal of Women’s Health looked at the role of strengthening the obturator internus and the adductors and compared the effects to working the pelvic floor for the treatment of women with SUI. The results were quite interesting.
This research was a pilot study comparing two randomly assigned groups of community dwelling women with SUI. A group of 12 completed resisted hip rotation (RHR) and a group of 15 completed pelvic floor muscle training (PFMT). Each group exercised at home for six weeks with a weekly recheck. Outcome measures included subjective reports of improvement, leak frequency, and scores from the Incontinence Impact Questionnaire (IIQ) and the Urogenital Distress Inventory (UDI). The exercise routines were supposed to take about 5 minutes and be performed twice a day. Subjects were instructed to sit with good posture and with their feet on the floor. The pelvic floor muscle group performed 5-second holds for 20 reps followed by 20 quick contractions. The RHR group exercised by 1) rotating internally and externally with diaphragmatic breathing for 10 breaths , 2) 10 repetitions of resisted hip external rotation with a green band and 5 second work/rest cycle and 3) 10 repetitions of hip internal rotation/adduction against a 9 inch ball with the same 5 second squeeze and rest cycles.
The results of the study showed that BOTH groups had significant and equal improvement in outcome measures by the end of the six weeks, but that the RHR group showed improvements sooner than the PFMT group. The authors discuss the limitations of their study: small sample size, large ranges of participant ages, patients were not medically examined, outcome measures were subjective, and the pelvic floor group only received verbal instruction. This study was thought provoking to me for several reasons. First, it gives me a great platform to talk with my non-pelvic health colleagues about treating pelvic floor weakness dysfunctions with indirect pelvic floor treatment. Virtually any patient could sit and roll their legs in and out against resistance! This exercise could be easily incorporated into a routine for people with bladder leakage or at risk for bladder leakage. Secondly, we often see patients with non-functioning pelvic floor muscles. My typical protocol before discussing the treatment option of electrical stimulation is to uptrain (increase muscle activity) with hip rotation, adduction and transverse abdominus muscle exercises. I have often found that I don’t need to address the pelvic floor directly when the accessory muscles are appropriately engaged. This study points out the importance of muscles outside of the pelvic floor in providing support for continence.
Thirdly, can we extrapolate the benefit of resisted hip exercise into more functional or more challenging exercises for our high level athletes or moms who want to jump on the treadmill with their kids? Would this approach be helpful? I know many of us are already doing this. Could this idea be a future research project? Lastly, John Delancey published in an anatomy study of cadavers that the muscle fibers around the striated urethral sphincter decrease in density and number at a rate of 2% a year after the age of 35!!! The process might go a little faster with higher parity and slightly slower in women who have never been pregnant. Could this mean that our reliance on our accessory muscles increases with age? Perhaps using both pelvic floor and resisted hip strengthening will lead to improved outcomes in older women.
One reason I love to read research is because it gets my brain thinking not only about how interconnected our bodies are, but I also ask myself what else I want to know about this subject and how can this information be used. We may not have the research-validated information we want yet, but applying critical reasoning to our clinical practice is the first step in further understanding.
You can join faculty member Jennafer Vande Vegte at an upcoming intermediate PF2B course. Keep in mind that these pelvic floor continuing education courses sell-out months in advance! With courses on both coasts and in the middle of the US, hopefully you can find a location that works best for you!
By accepting you will be accessing a service provided by a third-party external to https://hermanwallace.com/