Over the past 28 years, my pelvic floor has endured at least 20,000 miles of running, including racing on the collegiate level and then completing 10 marathons. Add to the high-impact sport two 8.1 pound natural childbirth deliveries 26 months apart, and you can imagine why I accepted the invitation to blog for this well-respected institute. One of my elderly patients once told me my uterus was going to drop out from so much running (which, thankfully, has NOT happened); however, I have to admit, urinary stress incontinence and frequent urination were unwelcome enough consequences! On the positive side, it all initiated my journey to understanding the pelvic floor.
![By Mike Baird [CC BY 2.0 (http://creativecommons.org/licenses/by/2.0)], via Wikimedia Commons](/images/photos/Blog/Female_jogger.jpg)
In 2014, Poswiata et al used the Urogenital Distress Inventory (UDI-6) to assess how prevalent stress urinary incontinence may be among elite female skiers and runners. Of the 112 female athletes in the study, 50% reported leaking a small amount of urine. Coughing and sneezing provoked leakage for 45.54% of those women, indicating stress incontinence, and 58.04% of the women in the study reported frequent urination. Are those acceptable statistics? I would have to say no.
Research results can be comforting so athletes can be told they are not alone regarding a quite personal aspect of their lives. When I could supposedly empty my bladder, stand to wash my hands and have to go again, walk down the hall to put on my sneakers and go once again before heading out the door for a run, it was nice to know someone else was probably experiencing the same issue that morning. Just because it is common, though, does not make it “normal.” We are not meant to leak just because we stress our bodies beyond normal ADLs.
A very recent study by Luginbuehl et al (2015 July 21), just published online, attempted to explore the electromyography (EMG) activity of pelvic floor muscles with variable running speeds (7, 9, and 11km/h) over 10 steps. The highest pelvic floor muscle activity was recorded at 11km/h, which would sensibly suggest the muscles produce a greater contraction the faster someone runs. If a runner has developed a decreased ability to activate the pelvic floor muscles, stress urinary incontinence will likely become a highly irritating problem with fast running speeds over time. But how do they know, and where do they go?
Without health practitioners trained in rehabilitation of pelvic floor dysfunctions, consider how chronic an issue urinary stress incontinence would be for a large athletic population. So many women (and men) do not even recognize their leakage or frequent urination as treatable “issues” and never mention them to anyone. Often times, we are treating an athlete for a hip or lumbar injury and purposefully yet discretely have to ask the right questions and then educate the patient how some of their symptoms are secondary to pelvic floor deficits. Someone has to explain what is normal, and, better yet, someone HAS to make an effort to fix what is “broken” and restore the pelvic floor to a higher level of function. With the proper training, perhaps that someone can be you.
References:
1. Poświata, A., Socha, T., & Opara, J. (2014). Prevalence of Stress Urinary Incontinence in Elite Female Endurance Athletes. Journal of Human Kinetics,44, 91–96. doi:10.2478/hukin-2014-0114.
2. Helena Luginbuehl, Rebecca Naeff, Anna Zahnd, Jean-Pierre Baeyens, Annette Kuhn, Lorenz Radlinger (2015 July 21). Pelvic floor muscle electromyography during different running speeds: an exploratory and reliability study. Archives of Gynecology and Obstetrics. doi: 10.1007/s00404-015-3816-9.
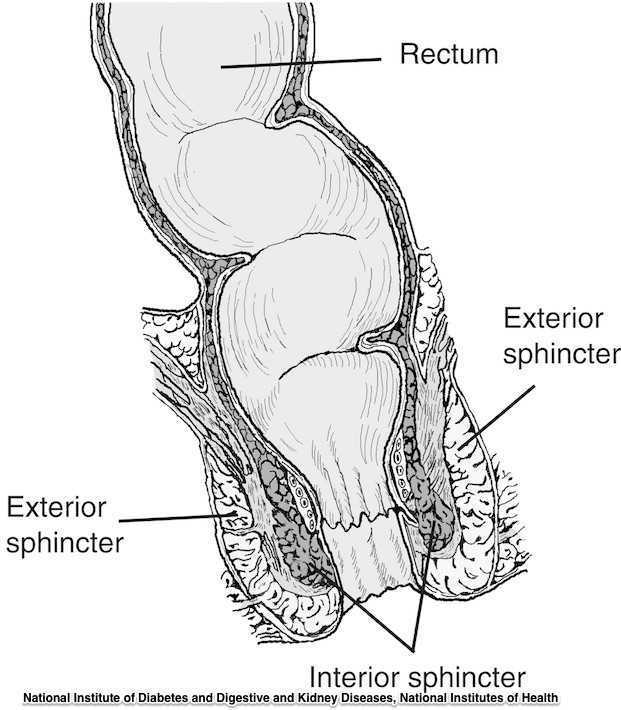
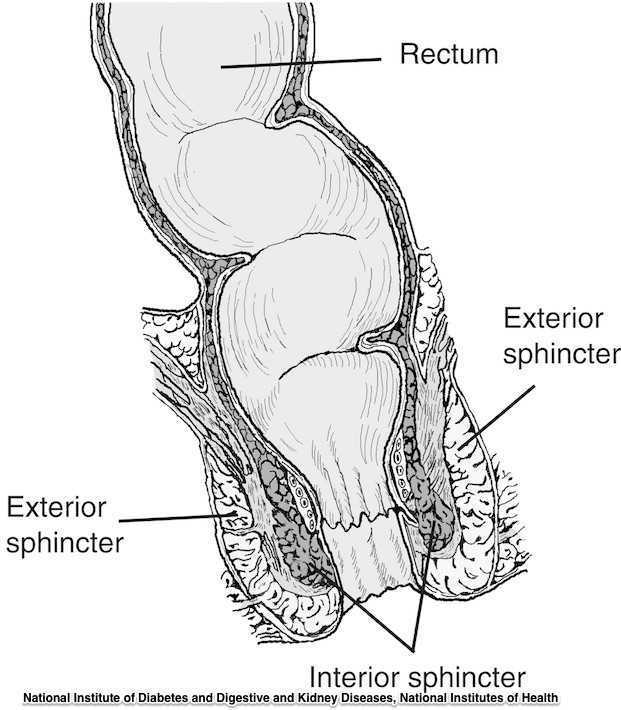
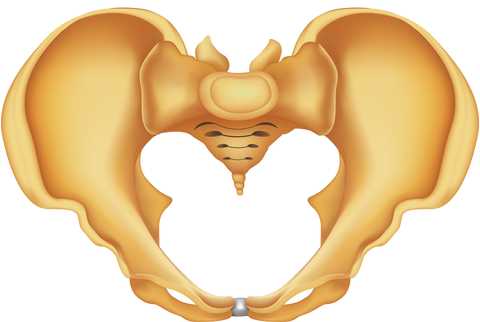
The phrase “rectal prolapse” may be easily confused with the term “rectocele” yet they may be very distinct clinical presentations. A rectocele refers to a prolapse of the posterior wall of the vagina that allows the rectum to bulge forward towards the posterior vaginal wall. This condition occurs most often in women rather than men. A rectal prolapse is a protruding of the rectum itself outside of the anal verge or opening. An overview article published in 2013 in the Journal of Gastrointestinal Surgery provides information about the condition that may assist the pelvic rehabilitation provider with valuable clinical concepts. Prior to becoming a full external prolapse, an internal intussusception may occur (and observed on defecography) and progress to include an external mucosal prolapse. Rectal prolapse may occur with or without other conditions of pelvic organ descent such as a cystocele or uterine prolapse. Although the prevalence of complete rectal prolapse is low, and occurs more often in women or in elderly patients, interference with quality of life may be significant.
Symptoms can include pain, difficulty emptying the bowels, bloody and or mucous discharge, urinary incontinence, and fecal incontinence or constipation. Patients may also complain of a lump or a bulge in the rectum that may or may not improve following a bowel movement. A complete rectal prolapse can be described as a full-thickness protrusion of the rectum through the anus. A more serious consequence of this condition is strangulation of the bowel. Features of a rectal prolapse often include a redundant sigmoid colon, levator ani muscle diastasis, and loss of the vertical position of the rectum, according to the article.
Treatment of a rectal prolapse may include surgery. Prior to surgery, a physical exam, colonoscopy, anoscopy, and possibly manometry and defecography may be completed. The surgical goals are to correct the prolapse, improve any complaints of discomfort, and to resolve bowel dysfunction. Surgical approaches may include abdominal or perineal approaches, minimally invasive versus open surgery, and techniques can include posterior versus ventral and rectopexy with or without sigmoidectomy. For more details about the specific approaches for rectal prolapse repair, see the linked article. The authors of this overview article point out that because “…there is a paucity of data evaluating the effectiveness and appropriateness of the various surgical techniques…”, there is not one single management strategy for each patient.
Nonsurgical recommendations for management of a rectal prolapse include appropriate daily fluid and fiber, suppositories or enemas if needed, biofeedback training, and pelvic floor muscle exercises. A patient may benefit from education in all of these concepts, before and/or following surgery. Pelvic rehabilitation providers are well poised to offer conservative management in these conditions prior to and following any needed surgery.
To learn more about rectal prolapse and related dysfunctions, join Dr. Lila Abbate, PT, DPT, MS, OCS at Bowel Pathology, Function, Dysfunction and the Pelvic Floor this November in New York, NY!
Varicoceles are enlarged veins that occur in the scrotum. They can be common in adolescent boys and men, with an incidence rate of approximately 15%. Because up to 1/3 of men dealing with infertility have a varicocele, a repair of this venous herniation may be a first line treatment for male fertility. Varicoceles are sometimes referred to as feeling like a "bag of worms" due to the distended veins that coil through the area (the U.S. National Library of Medicine provides a useful illustration). Although varicoceles may be painless, they are thought to be symptomatic in up to 10% of men. Symptoms can be dull, aching, throbbing, and can worsen with physical activity. Conservative care includes scrotal support, limiting physical activity, and using anti-inflammatory medications.

Pelvic rehabilitation providers may work with a male patient who complains of scrotal pain, and who has a known diagnosis of a varicocele. If the patient is unsure of such a diagnosis, questioning the patient about prior discussions with his medical providers may reveal that he was told about “enlarged veins in the scrotum” or similar description. Visual inspection may reveal the tell-tale appearance of distended veins inside the scrotum, and palpation may reveal a significant difference among sides (unless both sides are involved of course.) Physical examination for a varicocele is usually completed in supine and standing positions and may be palpable with or without Valsalva maneuver. Keeping in mind that the differential diagnosis for pain in the scrotum can include medical conditions such as testicular torsion, epididymitis, inguinal hernia, testicular tumor, hydrocele, epididymal cyst, or sperm granuloma, patients who have complaints must see an appropriate medical provider to rule out such conditions. It is also possible for a patient’s condition to change or worsen if a period of time has passed, with communication with the referring provider recommended. Post-surgical complications that should also be considered are inguinal hernia repair for nerve entrapment or vasectomy.
Because of the nerves traveling in the same pathway as the involved veins, we can also consider the neural tension potentially created from the increased venous distension creating either (or both) compression and drag. Surgical options may be discussed by the medical provider, and these might include a microsurgical ligation or a varicolectomy. According to Park & Lee (2013) “A varicocelectomy should be considered in patients with no alleviation of their pain after conservative management, including resting, scrotal elevation, and nonsteroidal anti-inflammatory analgesics.” Conservative management is exactly where we can fit in as providers of pelvic rehabilitation. Including a condition such as a varicocele in our differential diagnosis and treating planning can further our success with patients.
Herman & Wallace offers it's popular Male Pelvic Floor Function, Dysfunction and Treatment course next month in Denver, CO. See you there!
References
Park, Y. W., & Lee, J. H. (2013). Preoperative predictors of varicocelectomy success in the treatment of testicular pain. The world journal of men's health, 31(1), 58-63.
Shridharani, A., Lockwood, G., & Sandlow, J. (2012). Varicocelectomy in the treatment of testicular pain: a review. Current Opinion in Urology, 22(6), 499-506.
Dr. Susane (Susie) Mukdad is the founder of Healing Hands Physical Therapy, Inc., located in Willow Springs, IL.
Being a new mom is such a blessing, a new chapter in a woman’s life filled with joy, happiness, and many surprises! But giving birth can also bring about many changes in a woman’s physical, emotional, and social health. Increased level of sex hormones can result in physiological, cognitive, and musculoskeletal changes. These fluctuations continue to occur after birth, placing a new mom, who is now faced with many physical and emotional challenges at risk for burn out. In addition, new moms have to worry about their careers and relationships, suffer sleep deprivation, and the availability for support from their family and friends all of which can affect a new mom’s self-esteem, mood, and most importantly parenting ability.
According to a recent CDC survey, approximately 8-19% of women experience postpartum depression. In most cases, this occurs during the first 3 mo postpartum.
So, how can a new mom improve her well-being after having a baby?
"The number of women who were 'at risk' for postpartum depression prior to the treatment, dropped by nearly 50% at the end of treatment"
A recent study published in the Journal of the American Physical Therapy Association reports that participating in an individualized exercise and education program can significantly improve postpartum well-being. The researchers performed a Randomized Control Trail that looked at 161 new moms all of which were randomly selected into two groups: 1) Mom & Baby Program + Education 2) Education Only. The Mom & Baby Program consisted of an individualized postpartum exercise regimen for 60 min/1x per week conducted by a licensed physical therapist. In addition, participants received 30-minute educational sessions from various healthcare professionals that included, physical therapist, health psychologists, nutritionists, midwives, and speech pathologists. The Education Only group received informational material mailed to them over an 8-week period. Treatment lasted for a total of 8 weeks.
When the two groups were compared, the results were significant! Moms that were in the Mom & Baby Program + Education group reported significantly better well-being and depressive scores and the number of women who were “at risk” for postpartum depression prior to the treatment, dropped by nearly 50% at the end of treatment.
So what does this all mean?

It means that having a support group, someone coaching you through a safe exercise program and educating you on the ins and outs of being a new mom can be extremely beneficial to your health and overall well-being, reducing your risk of the postpartum blues. Having a team of well rounded healthcare practitioners such as physical therapists, doulas, midwives, and nutritionists can significantly improve your experience of being a new mom and provide you with the lasting support that you need to not only take care of yourself, but also your new baby.
For more on postpartum patient health, consider attending Herman & Wallace's Care of the Postpartum Patient course. The next event will be in Seattle, WA on March 12-13, 2016.
Norman, et al. An Exercise and Education Program Improves the Well-Being of New Mothers: A Randomize Control Trial. PHYS THER. 2010; 90:348-355

What are you saying when giving directions to men during pelvic floor muscle training, and how do those instructions affect the effectiveness of a contraction? These questions are tackled in a study that is very interesting to therapists working in pelvic dysfunction. 15 healthy men ages 28-44 (with no prior training in pelvic floor training) were instructed to complete a submaximal effort pelvic muscle contraction. Tools utilized to acquire data in the study include those below:
| Assessment tool | Measuring |
| Transperineal ultrasound | displacement of pelvic floor landmarks |
| Surface EMG (electromyography) | abdominal, anal sphincter muscle activation |
| Nasogastric transducer | intra-abdominal pressure (IAP) |
| Fine wire electromyography (3 participants only) | puborectalis, bulbocavernosus muscles |
Participants sat upright on a plinth (backrest reclined at ~20 degrees with their knees extended). Directions for the submaximal efforts were given by telling the men to produce a level 3/10 effort with 10 being a maximal contraction. The men were instructed to hold the contraction for 3 seconds, and they were given 10 seconds rest between each of the 4 contractions using different verbal cues. (This series of 4 contractions was repeated with randomization for verbal cues, with a 2 minute rest in-between.) Verbal instructions were intended to target specific contractile tissues as described below- some of this theory could be validated via the fine wire EMG.
| Verbal cue | Targeting |
| "tighten around the anus" | anal sphincter |
| "elevate the bladder" | puborectalis |
| "shorten the penis" | striated urethral sphincter |
| "stop the flow of urine" | striated urethral sphincter, puborectalis |
Displacement, IAP, and abdominal/anal EMG were compared for the different verbal instructions. The greatest dorsal displacement of the mid-urethra and striated urethral sphincter activity was noted with the instruction to "shorten the penis." "Elevate the bladder" encouraged the greatest increase in abdominal EMG and IAP, while "tighten around the anus" induced the greatest anal sphincter activity. Displacement of pelvic landmarks correlated with EMG readings of the muscles thought to produce the targeted movement. The authors conclude that the therapist's choice of verbal instructions can influence the muscle activation and urethral movement in men. They suggest "shorten the penis" and "stop the flow of urine" for optimal activation of the striated urethral sphincter. They also point out the fact that by using the fine wire EMG and correlating muscle activation to observations with the transperineal ultrasound, the study validates the use of the less invasive method. If you are ready to jump into more education about male pelvic rehabilitation, join us in Denver in early August, or Seattle in November.
Visceral therapy is increasingly used by manual therapists, and research continues to emerge that attempts to explain the underlying mechanisms of the techniques. A study published in the Journal of Bodywork & Movement Therapies in 2012 reports on the effects of visceral therapy on pressure pain thresholds. Osteopathic visceral mobilization was applied to the sigmoid colon in 15 asymptomatic subjects. Pressure pain thresholds were measured at the L1 paraspinal muscles and 1st dorsal interossei before and after intervention. Pressure pain thresholds at the level assessed improved significantly immediately following the visceral mobilization. The effect was not found to be systemic. Hypoalgesia, therefore, may be a mechanism by which visceral mobilization affects patients who are treated with this technique.
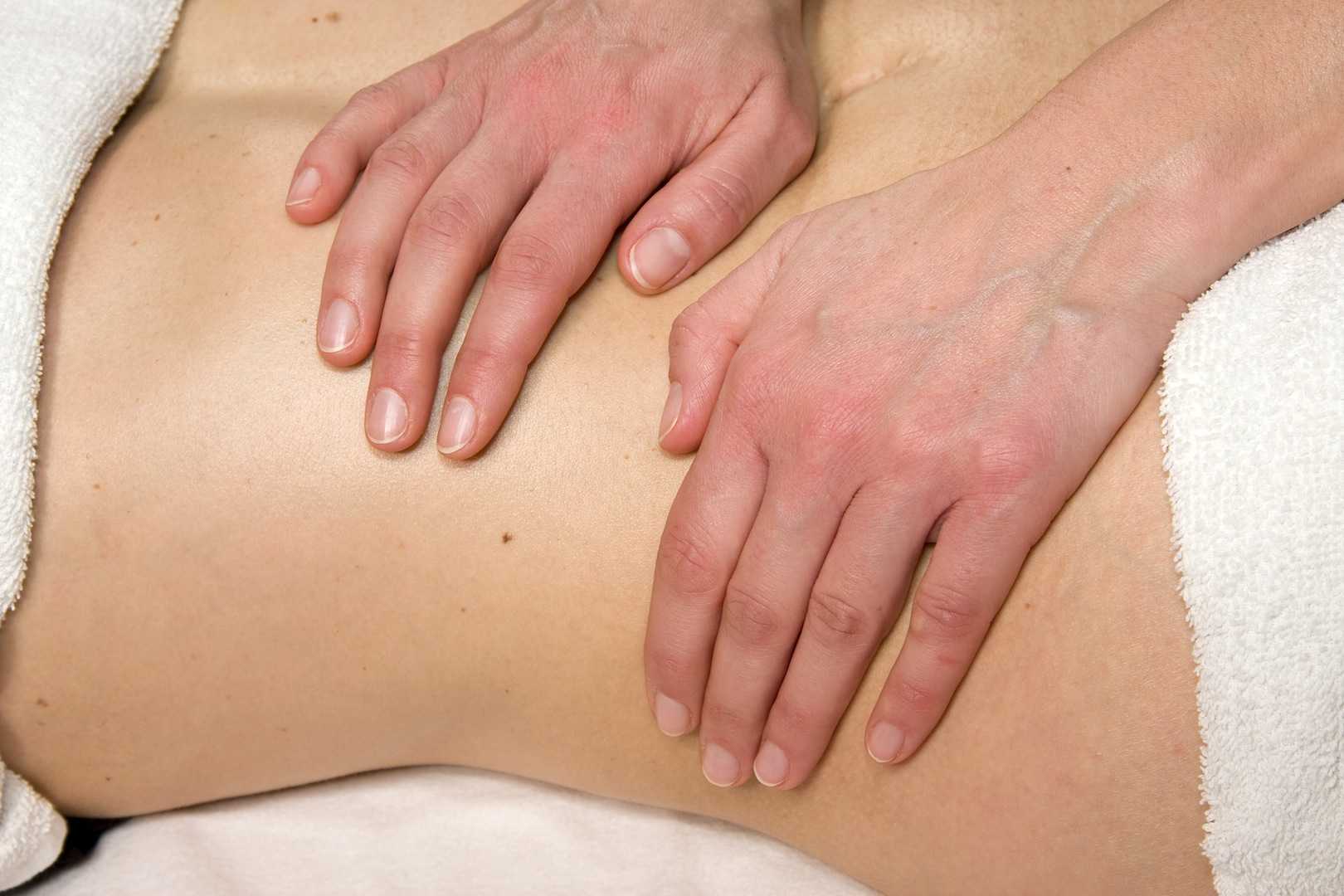
Another research study that aimed to assess the effects of visceral manipulation (VM) on low back pain found that the addition of VM to a standard physical therapy treatment approach did not provide short term benefits. However, when the 64 patients were reassessed at 2, 6, and 52 weeks following treatment, the patients in the group with visceral manipulation were found to have less pain at 52 weeks. The patients were randomized into 2 equal groups and were provided physical therapy plus a placebo visceral treatment or a visceral treatment in addition to physical therapy. The authors propose that there may be long-term benefits of including visceral therapy in rehabilitation approaches.
If you would like to learn more about visceral techniques as well as theory and clinical application, check out the schedules for Ramona Horton's Visceral Mobilization 1 (VM1): The Urologic System, and Visceral Mobilization 2 (VM2): The Reproductive System. The first opportunity to take VM1 is in November in Salt Lake City and VM2 is scheduled in September in Ohio.
The research on pelvic pain and specifically on sexual dysfunction has focused on heterosexual women, leaving a large gap in the clinically-based evidence. A study published last year in the Journal of Sex & Marital Therapy aimed to narrow this gap by studying the characteristics of vulvar pain in women in a variety of relationships. The associations between qualities such as love and communication were evaluated in relation to the participants' perceptions of how pain influenced their relationships. Within the research report, the authors establish that pelvic pain commonly causes pain and limitation with sexual function, and that queer women (defined in their work as women who identify as something other than heterosexual) also experience pain with sexual function.
"Of the 839 women, 31% reported genital pain, with 12% of the women with genital pain in a same-sex relationship, 67% in a mixed-sex relationship, and 21% being single"
The women in the study provided information about demographics, experiences of genital pain and pain characteristics. They completed surveys including the Dyadic Trust Scale (measures trust in a close relationship), the Rubin Love Scale (assesses level of romantic love), and the Communication Subscale of Evaluation and Nurturing Relationship Issues, Communication and Happiness Marital Satisfaction Scale (measures level of communication). Participants' average age was 25, and of the 77% who were in a relationship, most (60%) were in a mixed-sex relationship. Average length of relationships was 3 years, with nearly 84% of the women being white with some level of higher education.
Of the 839 women, 31% reported genital pain, with 12% of the women with genital pain in a same-sex relationship, 67% in a mixed-sex relationship, and 21% being single. Of the 260 women reporting genital pain, 39% identified as heterosexual, 15% identified as lesbian, and 46% identified as bisexual. The most common pain locations reported were inside the vagina (48%), in the pelvis or abdomen (45%), at the vaginal opening (39%), and 21% of the women reported global vulvar pain. From the data, the authors also report that women in same-sex relationships were likely to report that tampon insertion was painful.
The authors point out that challenges to healing for women who identify outside of heterosexual are many, and can include:
- homonegativity and heterosexism at a medical provider's office
- failure to disclose sexual identity due to fear of negative interaction
- fear that a symptom is linked to a sexual practice
- being in an unsupportive relationship or having poor adjustment within relationship
The limited research on sexual pain in women in same sex relationships has highlighted strengths within the relationships as well. Women in same sex relationships have been noted to have more effective communications skills, which may in turn foster better understanding of conditions such as pelvic pain. The authors concluded that while the characteristics of vulvar pain were similar across groups, there was a difference in the perception of pain impact on relationships. Better communication for same-sex couples and more love for mixed-sex couples was positively associated with impact on relationship. Of the women reporting pain, nearly half of the participants indicated that the pain negatively impacted their relationship in general, and 64% reported that the pain interfered with sexual health.
This type of research provides insight for pelvic rehabilitation clinicians and adds to our data base of considerations when working with women. The truth is that most of us were not provided adequate training in how to evaluate and manage issues of sexual health, nor were we provided with the means to value our own sexuality as a normal and healthy part of being. This lack requires education to fill in our own gaps, so that we can be of best service to our patients. If we are able to be present and nonjudgmental, our patients can in turn share openly and provide information that can direct best care. Holly Herman, co-founder of the Pelvic Rehabilitation Institute, offers a 2-day course in Sexual Medicine, so that providers can learn more about healthy sexuality as well as how to dialog with our patients.
Michelle Lyons is instructor of "Oncology and the Female Pelvic Floor: Female Reproductive and Gynecologic Cancers", among other Herman & Wallace courses. We thought you might like to hear her expert analysis of current research going on in the field of gynecologic oncology, and the benefits therapeutic yoga can have on patient rehabilitation. Take it away, Michelle!

More than 65,000 women are diagnosed with gynecologic cancers (vulvar, vaginal, cervical, ovarian, endometrial) in the United States each year (Sohl et al 2012). Treatment options for these women include surgery, chemotherapy, radiation and hormone therapy – all of which have the potential to have local, regional and global effects on a woman’s body. The pelvic rehab specialist is in a unique position to hugely improve quality of life issues for these women – dealing with issues directly associated with pelvic health (urinary, sexual and bowel function and dysfunction) as well as more global issues such as bone health, peripheral neuropathies and musculoskeletal dysfunctions.
Yoga has enormous potential as a therapeutic tool for gynecologic cancer survivors and as exercise prescription experts, we can add yoga as a multi-purpose tool to our skill-set.
Empirical research on therapeutic yoga has been ongoing for several decades, including several recent studies conducted with cancer patients and survivors. Although most of the research looking at the benefits of yoga for cancer survivors has been done in the context of breast and prostate cancers, we can safely extrapolate many of the benefits associated with oncology rehab yoga, including its immediately obvious ability to improve flexibility, strength, balance, but also the impact yoga can have on decreasing inflammation, improving sleep and raising quality of life scores in pelvic cancer survivors.
Recent papers by Dewhirst et al showed how moderate exercise can improve the efficacy of chemotherapy and radiation by decreasing tumour hypoxia – they also discovered that this may limit metastatic aggression.
We also know that exercise can be potent medicine when it comes to dealing with the effects of cancer treatments, especially fatigue, bone health and cardiovascular function, which may disrupt return to exercise (Kerry et al 2005). But pelvic cancer patients may face extra barriers when it comes to returning to exercise, such as pelvic pain and concerns about continence, as well as diminished flexibility, balance and strength. But as Blaney et al concluded in their 2013 paper ‘…however, the main barriers reported were those that had the potential to be alleviated by exercise.’ And in my opinion, this can be achieved by integrating yoga into our pelvic oncology rehab programs.
These recent and exciting research findings have encouraged me to add a therapeutic yoga lab session to my Oncology & the Pelvic Floor course, which I will be teaching in NY next month. This is the last chance to catch this course stateside this year so I hope you will join me in White Plains to explore the many ways we can make a serious impact on pelvic cancer survivorship (Bring your yoga mat!)
References:
Psychooncology. 2013 Jan;22(1):186-94.
Cancer survivors' exercise barriers, facilitators and preferences in the context of fatigue, quality of life and physical activity participation: a questionnaire-survey. Blaney JM1, Lowe-Strong A, Rankin-Watt J, Campbell A, Gracey JH.
Annals of Behavioral Medicine
April 2005, Volume 29, Issue 2, pp 147-153
A Longitudinal Study of Exercise Barriers in Colorectal Cancer Survivors Participating in a Randomized Controlled Trial
Kerry S. Courneya Ph.D., Christine M. Friedenreich Ph.D., H. Arthur Quinney Ph.D., Anthony L. A. Fields M.D., Lee W. Jones Ph.D., Jeffrey K. H. Vallance M.A., Adrian S. Fairey M.Sc.
JNCI J Natl Canc
Allison S. Betof, Christopher D. Lascola, Douglas H. Weitzel, Chelsea D. Landon, Peter M. Scarbrough, Gayathri R. Devi, Gregory M. Palmer, Lee W. Jones, and Mark W. Dewhirst
Modulation of Murine Breast Tumor Vascularity, Hypoxia, and Chemotherapeutic Response by Exercise
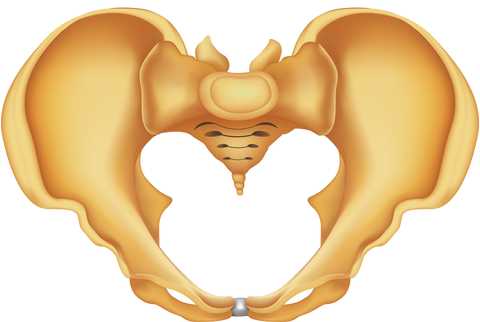
Pelvic rehabilitation providers commonly treat a variety of conditions associated with peripartum pelvic girdle dysfunction. This list of conditions includes coccyx pain, and a recent study aimed to identify risk factors which may lead to coccyx pain in the postpartum period. Dr. Jean-Yves Maigne, who is well known for providing foundational research on the topic of coccyx pain, and colleagues completed a case series of 57 postpartum women presenting to a specialty coccydynia clinic. Dynamic x-rays were taken to assess mobility of the coccyx, and data about delivery methods were collected. (A control group of 192 women were comprised of women who also presented to the clinic but who had coccyx pain from other causes.)
The authors found that the women reported immediate postpartum pain in the coccyx with sitting. Instrumentation was a common finding in regards to the patients’ deliveries. 50.8% of the deliveries utilized forceps while 7% were vacuum-assisted. An additional 12.3% of the deliveries were spontaneous and were described as “difficult.” A subluxation of the coccyx was observed in 44% of the women who developed coccyx pain after childbirth as compared to 17% of the controls. A fractured coccyx occurred in 5.3 % of the women. Body mass index (BMI) of more than 27 and having 2 or more vaginal deliveries was also associated with a higher prevalence of a subluxation of the coccyx.
Being unable to sit comfortably following childbirth could make a new parent’s life very difficult with limitations in activities such as sitting to feed the baby. Socially, being unable to sit comfortably can also limit many activities. The women in this study reported immediate tailbone pain with sitting, which can alert providers to a condition requiring both immediate and follow-up attention. Risk factors such as having a difficult delivery or use of forceps may also signal a patient history that may lead to coccyx pain.
If you are interested in learning more about managing coccyx pain, join Lila Abbate at Coccyx Pain Evaluation and Treatment in Bay Shore, NY on October 25-26! You may also be interested to learn more about treating patients during the postpartum period, in which case Care of the Postpartum Patient is right up your alley!
Today we get the opportunity to hear from Herman & Wallace faculty member Elizabeth Hampton PT, WCS, BCIA-PMB! Elizabeth has been kind enough to offer her insights about the diagnosis of pelvic rehabilitation patients. Join Elizabeth at Finding the Driver in Pelvic Pain this November in Houston, TX in order to learn evaluation tools for complex pelvic pain clients!
 Having taught for Herman and Wallace since 2006, I have a few observations that have been consistent over the years. Clinicians want their clients to get better, so much so that they are ready to jump in to treatment before having a solid problem list and validated findings. I can understand this: after a 3 day course we have clients Monday morning at 8 a.m. who have been waiting for us to take this course so we can get them better! We had better be smart ASAP! But what do we do when we are treating symptoms rather than understanding the primary, secondary and tertiary factors in their condition?
Having taught for Herman and Wallace since 2006, I have a few observations that have been consistent over the years. Clinicians want their clients to get better, so much so that they are ready to jump in to treatment before having a solid problem list and validated findings. I can understand this: after a 3 day course we have clients Monday morning at 8 a.m. who have been waiting for us to take this course so we can get them better! We had better be smart ASAP! But what do we do when we are treating symptoms rather than understanding the primary, secondary and tertiary factors in their condition?
Finding the Driver in Pelvic Pain is a course that is a foundational first step in screening the pelvic pain client. It is a great place to start. I developed the course because there was no evidence based comprehensive factors that had been established as fundamentals for screening a pelvic pain client.
The other thing I have learned after teaching Pelvic Floor Function, Dysfunction, & Treatment – Level 2B for 9 years is that the majority of clinicians who take this intermediate level course cannot perform a precise vulvar and intrapelvic muscle mapping assessment. Close your eyes and pretend you are mapping a client’s left iliococcygeus: can you place your finger in the proper orientation and know 100% you would be palpating it? Indeed, this takes training and repetition. Internal pelvic floor muscle mapping is a key part of the Finding the Driver screening system.
What do you do when you have a pelvic pain client on your schedule and a 45-60 minute slot? How do you screen findings and get the plan of care within such a short period of time? Finding the Driver is a comprehensive pelvic floor and musculoskeletal screening to rule in or rule out drivers of the pain from all sources including spine, pelvic ring, neural entrapment, intra-articular hip, load transfer, biomechanics and motor control. There is a clear flow to the screening process and an emphasis on how to organize that information, as we know with pelvic pain, it is the copious amount of information that is the challenge. We have two case studies with either participants or clients of a local Physical Therapist who come in and we go through the entire screen, prioritize treatment and provide that treatment during the course. The participants walk away with clear clinical reasoning for their treatment and prioritization of treatment as primary, secondary, and so on. The goal of the course is to help the clinician sort through the extraordinary amount of information we gather on our pelvic pain client and organize it in a way that we can explain to the client as well as create our plan of care. Treatment is not linear, as we are frequently treating many aspects at the same time. However being able to organize the information is key in designing that plan of care. For example, with a prone knee bend that reproduces labial pain, we find that the genitofemoral nerve is causing referred pain. However that referral may be due to constipation, irritable bowel, inguinal entrapment due to hernia surgery, intra-abdominal adhesions due to endometriosis, osteitis pubis or facilitated segment at the upper lumbar spine. How do we tease that out? How do you sequence nerve glide, visceral work, soft tissue mobilization, joint mobilization and dietary components for colonic motility? The treatment with all of those components are very different indeed. Finding the Driver is a hands on course with systematic screening tools and, with case studies, we go through treatments appropriate to that client. The focus is on what we, as physical therapists, can do to understand the drivers.
At the last Finding the Driver course in Milwaukee, WI, we had two case studies in pelvic pain. One client reported chronic psoas and adductor tightness with deep left sided pelvic pain. As a professional aerialist, she was extraordinarily flexible and demonstrated positions of tightness that concerned her, which included lateral splits with her hips in slight horizontal abduction and extension (yes, yikes!) When she reported that her adductor felt tight in this position, I explained it was because it was trying to keep her leg attached to her body! She was 9/9 on the Beighton scale and had severe multidirectional instability in her hips, impaired load transfer through her pelvis, respiratory dysfunction with efforts at pelvic floor and transverse abdominis contraction, as well as repeated choice of activities that were profoundly provoking. Interestingly, she was better at load transfer during handstands (bilateral or unilateral) vs. in standing and we discussed her course of treatment addressing the primary, secondary and tertiary aspects of her condition. Another client had severe labial pain, and despite multiple abdominal and intravaginal surgeries, her symptom onset was 4 months prior. She certainly had visceral, postural, joint restrictions, movement dysfunction and many other factors. But her primary driver was a labral tear in her hip and she needed surgery. After surgery, her pain was 100% resolved and in her post op rehab, the other factors could be addressed.
It is safe to say that it can be difficult to perform a comprehensive screen in 45-60 minutes on ALL clients. We all know that many of our clients need to tell their story and because of fear or previous negative history, we may choose as clinicians how to spend that session to best honor the needs of the client. That being said, Finding the Driver is a course which provides a solid start in differential diagnosis so you can drill down into more specifics on subsequent visits.