
Menopause represents a transformative phase in a woman’s life, and as pelvic health practitioners, it’s an opportunity for us to make a significant impact. Rather than being the “beginning of the end,” menopause can usher in a new era of freedom and empowerment. Women spend a significant portion of their lives post-menopause, free from the limitations of periods, pain, and hormonal fluctuations, but only if we, as clinicians, provide the tools and education necessary to thrive during this transition.
Historically, women’s health during menopause has been overlooked. In the past century, limited life expectancy meant menopause healthcare and research were rarely prioritized. Combine that with the research gap in women’s health and well-documented medical misogyny, and one can see how generations of women’s health has been neglected. However, with advancements in healthcare and advocacy, that’s changing—and we need to lead the way in reframing menopause management, starting with conservative pelvic health approaches before defaulting to hormonal therapies.
The Overlooked Connection: Hormones, Voice, and Pelvic Floor Health
Among the myriad symptoms of menopause, the interplay between hormonal changes, the voice, and the pelvic floor often goes unnoticed. Hormonal shifts, especially decreasing estrogen levels, significantly impact voice quality, including reduced pitch range, vocal endurance, and an increase in vocal fatigue and dryness. These changes mirror similar phenomena in the pelvic floor, where decreased tissue elasticity, sarcopenia, and altered pressure management can result in incontinence, prolapse, or pain.


Caring for patients who have experienced trauma requires a skillset beyond basic knowledge of pelvic health assessment and intervention. With one-third of women experiencing intimate partner violence, and estimates of rape reports to formal agencies (e.g., police, medical professionals) ranging from only 5–33% (Fisher, Cullen, & Turner, 2000; Kilpatrick et al., 2007; Krebs et al., 2007; Rennison, 2002), we can safely say that the gender-based violence women uniquely experience is likely grossly under-reported.
Additionally, the World Health Organization reports that violence and sexual violence against women is a major global public health problem. Estimates published by WHO indicate that globally about 1 in 3 (30%) of women ages 15-49 worldwide have been subjected to either physical and/or sexual intimate partner violence or non-partner sexual violence in their lifetime.
In terms of violence, the vast majority is, sadly, intimate partner violence; that is, violence committed by your own partner. Further, the overall risk of any gender reporting intimate partner violence is 1 in 7 for people who identify as men, and 1 in 5 for people who identify as female, according to the last reported statistics from the CDC.
For trauma risk in general, the chance of any gender experiencing trauma, including ACEs, or Adverse Childhood Experiences, is as high as over 70%. The first comprehensive study on PTSD (post-traumatic stress disorder) and trauma in the US was not conducted until 1990, which reported that 60.7% of men and 51.2% of women reported at least one exposure to trauma. From there, the estimated population lifetime prevalence of 5.7% for men and 12.8% for women (Kilpatric et al 2013).
The statistics on violence against the LGBTQIA community are even more alarming. A survey found that transgender people (16+) are victimized over four times more often than cisgender people and that transgender women and men had higher rates of violent victimization than cisgender women and men. Overall, about 50% of the violent victimizations were not reported to police. A separate 2022 survey showed that LGBT people experienced 6.6 violent hate crime victimizations per 1,000 persons compared with non-LGBT people's 0.6 per 1,000 persons (odds ratio = 8.30, 95% confidence interval = 1.94, 14.65).

Note: If you missed my last post, read about the three diaphragm (voice-to-pelvic floor) approach here: https://hermanwallace.com/blog/the-voice-of-pelvic-healthbuilding-a-3d-treatment-toolbox
How well can you speak when you are nervous? How well can a person sing if they are crying? What happens to the pelvic floor if someone is nervous or crying, or both? It doesn’t take too much investigation to realize that the health of our voice and pelvic floor are intimately intertwined – and tied to – our stress response.
We know the way we respond to stress impacts our performance. So, when we ask what makes someone a pelvic floor athlete – the answer is – anything that person does that impacts their stress response. If the voice is intimately tied to the stress response as well, then the sport of voicing, or singing, qualifies as an athletic event for the pelvic floor. Thankfully, we have a long string of evidence-base to support the impact of breathing on the pelvic floor, but what about voicing?

Faculty member Ginger Garner PT, DPT, ATC/L is offering a new short course, The Voice and The Pelvic Floor. This course introduces foundational concepts needed to be able to use vocal techniques to treat the pelvic floor and core. Dr. Garner is a clinician, educator, and longtime advocate committed to making physical therapy services accessible, affordable, and equitable, especially for pelvic health.
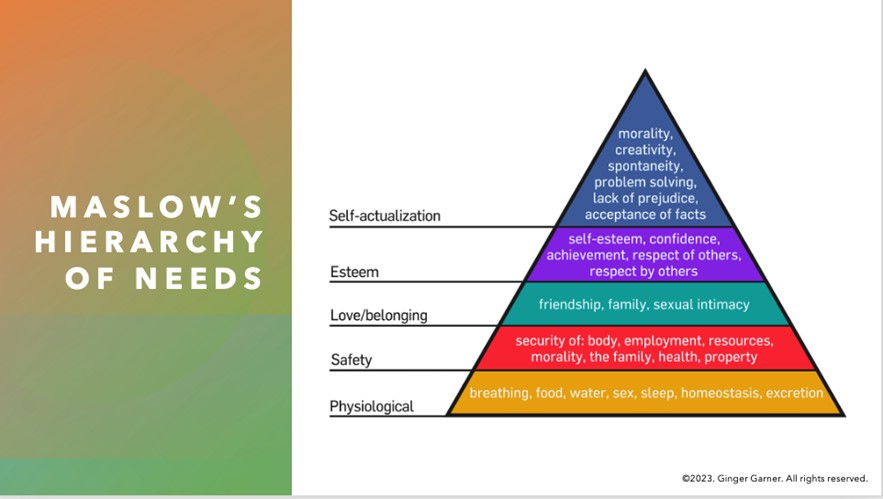
When you think of pelvic health, what comes to mind? Obvious variables like the pelvic floor & girdle, abdominals and related synergists, mental health, and gut and respiratory health are probably at the top of your list.

Yoga offers a compelling mind-body approach to maternal care that is forward thinking and aligns with the World Health Organization and Institute of Medicine’s recommendations for patient-centered care. But let’s take a look at WHY postpartum care MUST change in order to establish need for the entry of yoga into postpartum care.
Maternal Health Track Record
The United States and similarly developed countries have a very poor track record for postpartum care. The record is so poor that the problem in the US has been labeled a “human rights failure.”1
On its own, the US has the worst track record for not only postpartum care, but for maternal and infant mortality and first-day infant death rate in the developed world (Save the Children 2013). Between 1999-2008, global mortality rates decreased by 34% while the US’s rates doubled for mothers.1
Patient satisfaction also suffers under the current model of care, with many more mothers experiencing postpartum depression, a significant risk factor for both mother and baby during and after pregnancy.
The increase in mortality and poor outcomes can, in part, be attributed not to underuse, but overuse of medical intervention during pregnancy and birth. 2,3,4 Countries that have “access to woman-centered care have fewer deaths and lower health care costs”; and, hospital system reviews in the US show that reducing medical interventions are both reducing cost and improving outcomes.1,4,5
The notorious lack of accountability (reporting system) in maternal health care also plagues the US and suggests that maternal deaths are even higher than currently reported, leading to Coeytaux’s conclusion that the “United States is backsliding.”1
Improving Postpartum Outcomes with Integrated Physical Therapy Care
In After the Baby’s Birth, maternal health advocate Robin Lim writes,
"All too often, the only postpartum care an American woman can count on is one fifteen minute appointment with her doctor, six weeks after she has given birth. This six-week marker ends an arbitrary period within which she is supposed to have worked out most postpartum questions for herself. This neglect of postpartum women is not just poor healthcare, it is abusive, particularly to women suffering from painful physical and/or psychological disorders following childbirth."
Physical therapists can be instrumental change agents in improving current postpartum care, especially through the integration of contemplative sciences like yoga. Yoga can be the cornerstone of holistically-driven, person-centered care, especially in comorbid conditions such as pelvic pain and depression, where pharmacological side effects, stigma, can severely diminish adherence to biomedical interventions.6 Coeytaux, as well as other authors, clearly correlate the reduction of maternal mortality with improved postpartum care. The World Health Organization recommends that postpartum checkups should include screening for:
- Back pain
- Incontinence (stress)
- Hemorrhoids
- Constipation
- Fatigue
- Breast pain
- Perineal pain
- Depression
- Painful or difficult intercourse
- Headaches
- Bowel problems
- Dizziness or fainting
A physical therapist is a vital team member in not only screening for many of the
listed problems above, but in managing them. It is important to note that other countries, like France, deliver high quality postpartum rehab care plus in-home visits, all while spending far less than the US on maternal care.
The World Health Organization, however, clarifies the vital importance of postpartum care delivery by making a significant recommendation for a paradigm shift in biomedical care.7
Yoga as a “Best Care Practice” for Postpartum Care
The WHO recommends the use of a biopsychosocial model of care, which yoga is ideally suited to provide via its ancient, multi-faceted person-centered philosophy. Medical Therapeutic Yoga is a unique method of combining evidence-based rehabilitation with yoga to emerge with a new paradigm of practice. MTY:
- Addresses the mother as a person, not as a condition or diagnosis.
- Empowers mothers with self-care strategies for systems-based, not just musculoskeletal or neuromuscular, change.
- Addresses all domains of biopsychosocial impairment.
- Teaches interdisciplinary partnership-based theory, which is integral to creative collaborative discourse and innovation in postpartum care.
- Equips clinicians with business service, website development, practice paradigm, and social media campaign tools to fully develop the new clinical niche of Professional Yoga Therapy practice.
- Promotes patient advocacy, health promotion, and public health education via mainstreaming yoga into rehabilitative and medical services.
- Provides the gender context for prescription that traditional yoga is lacking.
- Evolves yoga for use in prenatal and postpartum care.
Physical therapy screening and intervention in the postpartum is vital, but the addition of yoga can optimize postpartum care and has enormous potential to be a “Best Care Practice” for postpartum care in rehabilitation.
As a mind-body intervention, yoga during pregnancy can increase birth weight, shorten labor, decrease pre-term birth, decrease instrument-assisted birth, reduce perceived pain, stress, anxiety sleep disturbances, and general pregnancy-related discomfort and quality of life physical domains.8-9
In addition to the typical physical therapy intervention for postpartum physical therapy, the MTY paradigm provides:
Faculty member, Ginger Garner PT, L/ATC, PYT will be giving 2 lectures at this year’s annual Montreal International Symposium for Therapeutic Yoga, or MISTY for short, in Montreal, Quebec. The first is a 2-hour lecture titled, Vocal Liberation, and the second is a 4-hour lecture titled, Hip Preservation: Yoga Reconsidered, Visit http://www.homyogaevents.com to learn more.
Yoga is, unarguably, a popular contemplative science, enjoying 36.7 million practitioners in the US alone, up from 20.4 million in 2012.1 A 16 billion dollar industry, yoga is one of the most widely utilized methods of complementary and integrative medicine in America today. In 2008, the editor of Yoga Journal declared “yoga as medicine” as the next great wave. That was right in the middle of the Great Recession, when the last thing on the collective healthcare industry’s mind was yoga.
What happened during the same time frame as the interest in yoga surged?
Herman & Wallace Pelvic Rehabilitation Institute faculty member, Ginger Garner PT, L/ATC, PYT, will be giving 2 lectures at this year’s annual Montreal International Symposium for Therapeutic Yoga, or MISTY for short, in Montreal, Quebec. The first is a 2-hour lecture titled, Vocal Liberation, and the second is a 4-hour lecture titled, Hip Preservation: Yoga Reconsidered, Visit http://www.homyogaevents.com to learn more. Read below as Ginger shares why the voice is a linking science.
The Voice as a Linking Science for Clinical and Business Efficacy
Your voice can be the key to your success. Forbes magazine’s #3 habit in an article, Five Habits of Highly Effective Communicators, is “Find your own voice.” London’s think tank Tomorrow’s Company declares in a recent report on efficacy in business leadership, “Having a voice really matters for employees today.” The director of the Involvement and Participation Association (IPA) and vice-chair of the London-based MadLeod Review on employee engagement says, “Voice is extremely important because there are many changing business concepts and one of the essential ones is trust. Our voice is one of the things we really need to change old management paradigms and build trust in an organization.”
If you are an instructor, teacher, educator, therapist, or all four, having a voice is synonymous with having a job. You can’t do your job without a voice. And yet, we don’t spend much time thinking about vocal physiology, much less how to maintain and even improve it.
The following post comes to us in part from Ginger Garner, PT, ATC, PYT, who teaches three yoga courses for Herman & Wallace; Yoga for Pelvic Pain, Yoga as Medicine for Pregnancy, and Yoga as Medicine for Labor and Postpartum. Check out her poster at the Combined Sections Meeting this weekend in Anaheim!
Maternal health care in the United States is abysmal. Especially wretched is care and support of women post-partum. Our insurance system is partially to blame by dictating that women receive only one visit with the provider who participated in the delivery of their baby 6 weeks after the baby is born, no matter the method of delivery. This is often after most of the scary, unexpected side effects of delivery, like heavy bleeding, nipple pain, urinary incontinence, difficulty with bowel movements, scar pain and tremendous mood swings have begun to ease. Only the women who are the most persistent, or those who have chosen unique care models (like out of hospital births with midwives), seem to get real support post-partum, leaving marginalized and less self-driven women to fend for themselves.
What if research could show that immediately treating some of the side effects of birth, like diastasis recti abdominus, which occurs in 50-60% of post-partum women, could result in improved outcomes in the long run? What if someone could prove that retraining and strengthening the abdominal wall as part of a biopsychosocial model empowering women could change the costly effects of prolapse and urinary incontinence treatment later on in life? What if that research aimed to show that treating women in partnership will all care providers was the most effective? These are big questions, but through research beginning with Diastasis Recti Abdominis (DRA), some Women’s Health Physical Therapists trained in Medical Therapeutic Yoga are hoping to highlight some answers.
The following is contributed by faculty member Ginger Garner, who teaches the Hib Labrum Injury course. You can read more about that course on the Herman & Wallace course page.
Hip labral injury (HLI) is a relatively new diagnosis in the last 10 years of orthopaedic and rehabilitative care. However, just because HLI is a new diagnosis doesn’t mean the injury is new. In fact, HLI is posited to be responsible for the premature aging and osteoarthritis of the hip joint and pelvis that leads to hip replacements. HLI is also a major source of hip pain, with groin pain being the most common subjective complaint.However, groin pain is not the only complaint that is associated with HLI. Pelvic pain commonly goes hand-in-hand with hip pain.
What does this mean for patients? If you have hip or pelvic pain you should be evaluated by an HLI specialist, which can be a PT, surgeon, or osteopath who has received additional training on managing HLI. It is critical that you see someone who specializes in HLI. If HLI or other hip or pelvic injury is suspected, it is important that you follow up with a physical therapist who has had advanced training in HLI rehab for the best chance of recovery.
In our weekly feature section, Pelvic Rehab Report is proud to present this interview with Herman & Wallace instructor Ginger Garner, PT, MPT, ATC.
How did you get started in pelvic rehab?
My entry point into pelvic rehab was a bit unorthodox and as a result, my colleagues at the time (back in the 90’s), considered my practice quite eccentric and frankly, a bit strange.
In fact, although I can see lots of humor in it now, I was actually pushed out of a practice because what I was doing was “too individualized” and patient specific. Of course, that “eccentric” entry point into pelvic rehab was integrative medicine, using a yoga-based biopsychosocial model of practice.
Who or what inspired you?
To answer that question I think you first have to be able to recognize and appreciate times when you have not been well supported or inspired, kind of like having to know adversity before you can recognize and value success.
Here’s my short story:
Early on in my education (in sports medicine, athletic training, physical therapy, yoga, and pilates) I realized that the biomedical model, although stellar at handling life-threatening emergencies, was not always so great at addressing chronic conditions and preventing disease processes and injury. So the answer to what inspires me – is the privilege of being able to be on the prevention end of injury and disease.
Back in the 90’s, I had a faculty instructor who encouraged me to keep pursuing my passion – in spite of the pushback I got from many directions, including within the department at the university. She found a way for me to pursue lateral work in the School of Public Health, which I felt was necessary in order for me to become a successful patient advocate. It was a great experience where I was able to work with the Governor’s Council on Physical Fitness and Health and conduct a pilot study. Her encouragement inspired me to keep following my dream, which is why I strongly believe in this quote by Mark Twain,





































