







Dearest Gentle Readers,
It has come to this author’s most refined attention that a most curious scandal has fluttered through the drawing rooms - or rather, the online salons - of the pelvic health world. The whispers suggest that the reputable purveyor Intimate Rose has, perhaps, been reappropriating patients from their dear therapist partners by embarking upon a bold new venture: the offering of telehealth services.
One can scarcely imagine a more titillating topic among those who prize propriety and pelvic alignment in equal measure. And thus, in the spirit of intellectual inquiry, I present to you an ethical analysis of this latest society stir: Intimate Rose versus Pelvic Floor Therapists.


Pelvic health rehabilitation has grown tremendously over the decades, expanding from a publicly viewed mentality of “just Kegels” to a comprehensive, whole-body, and whole-life approach. As rehabilitation providers, we now treat the complex interplay of muscles, fascia, organs, and the nervous system that influences bladder, bowel, and sexual health. But one area that is still underrepresented in many rehabilitation settings is pessary care.;
Pessary fitting has historically been performed by gynecologists and urogynecologists, but in more recent years, especially since the APTA released a position statement in favor of pelvic health physical therapists being able to fit pessaries in 2022, pessary care has entered the rehab scope of practice. Adding pessary fitting, management, and follow-up into a pelvic rehab practice can provide immense benefits for patients, providers, and the healthcare system at large.
Pelvic organ prolapse (POP) is incredibly common, affecting nearly half of people who have given birth. As pelvic health providers, we are not surprised to hear many patients are left with only two extremes: surgery or “wait and see.” We know that pelvic floor therapy can help POP, with things like lifestyle changes, bowel/bladder habit changes, support garments, pressure management, and exercise, but what about our patients who need more?

When Play Becomes Therapy - and Therapy Becomes Play
Pediatric pelvic floor therapy can sound intimidating to parents at first. They often imagine sterile clinics, complicated equipment, or uncomfortable exercises. But in reality, the best therapy for children often looks a lot like play. When we engage children in fun, creative, and developmentally appropriate activities, we not only help their bodies heal. We also help them gain confidence, resilience, and joy. Let’s dive into an example of a patient named “Alex.”
“Alex” is a 5-year-old who came to therapy with a history of chronic constipation, including hard, infrequent stools and painful bowel movements. Part of his assessment reveals that he has weak core strength, exhibited by his slouched posture, trouble sitting upright for long periods, and fatigue during physical play. His parents also describe “play aversion,” including avoidance of playground activities, reluctance to join peers, and resistance to movement-based games. His therapist determines that these issues didn’t just affect Alex’s health; they impacted his daily life. Alex’s family wanted their child to feel comfortable in his body, develop healthier bathroom habits, and learn to enjoy playing.
Step 1: Building a Sensory-Friendly Toilet Routine
For many children with constipation, the bathroom itself can feel overwhelming. Bright lights, cold seats, or long, uncomfortable waits can add to anxiety and resistance. For “Alex,” we started with sensory-friendly toilet sits. His family learned how to use a child-sized seat insert and footstool to support proper posture (knees slightly higher than hips, feet flat for stability). As a team, we talked with “Alex” about softening the bathroom environment with warm lighting, gentle music, or a favorite stuffed toy. In addition, we implemented keeping sessions short and predictable (e.g., sitting after breakfast for 2–3 minutes rather than forcing long waits). The focus of this stage was on making the bathroom feel safe and manageable, turning it into a place for success rather than stress.




Since its launch in the beginning of 2024, Modalities for Pelvic Function has only continued to grow. The cool thing about this class is that although the curriculum content stays mostly the same, there are always amazing products for pelvic health being released and discovered by the curriculum team. Our next class offering is in July of 2025 and we’re adding at least 3 new products to the class. Enjoy our introduction to them in the order they will appear in our course work!
New to the Myofascial Techniques Lab - The BAligned Bowtie
The BAlign® Bowtie by TheraTrain is a therapy tool designed by Dr. Jaime Loomis, a Doctor of Physical Therapy, to promote spinal alignment and alleviate musculoskeletal discomfort. The BAlign Bowtie is a compact, hard rubber device shaped like two connected ovals. Dr. Jamie gives tips on where to place it, usually the base of the spine or pelvis, and then the client lies on it for a few minutes to help realign the spine and relieve pain. This tool is particularly beneficial for individuals experiencing low back pain, hip tightness, or asymmetrical posture. It's also been reported to aid in conditions like scoliosis and improve mobility in activities such as golf and running.
I had the privilege of meeting with Dr. Jamie to talk about her product, and she gave me the insider scoop on it. This product can be used for pelvic alignment, but can also be used higher up in the spine to help with asymmetry and pain. I personally love a multifaceted tool for investment and creative purposes! She created this tool to save time in therapy sessions. Dr. Jamie noticed that patients with pelvic and shoulder asymmetries would have improvement with their alignment and pain in therapy, but then be back to baseline by their next session. She’d have to spend time in their session repeating previous work to realign things again. She found that with this tool, her patients could have something actionable at home and their return sessions in alignment and were able to focus on other areas of therapy such as strength, function, and mobility.


When we think of pelvic floor dysfunction, our minds often go straight to adults. We may even consider toddlers or children struggling with conditions like constipation or bedwetting. A population I frequently find missed is the infant! Many providers don’t realize that the pelvic floor issues that show up in infancy don’t have to be waited out.
As pediatric pelvic health providers, we have a unique and powerful role to play in helping babies who struggle with common challenges like reflux, colic, constipation, feeding difficulties, and even motor delays. At the root of many of these concerns lies the pelvic floor—an area often overlooked in traditional pediatric care. These parents will go to their providers, and they’ll be offered advice like “hold them upright for 20 minutes after feeding” or “try a lactation consultation,” but what happens if these interventions are not enough, OR what happens if a rehab provider wants to provide more support to a struggling family.
You may be thinking, “I don’t do pediatrics.” If that is your stance, I recommend you keep reading. You don’t have to be a dedicated pediatric therapist to provide families struggling with cranky or uncomfortable babies. Even if you don’t want to provide specific recommendations and treatment, you can still screen and offer referrals for support and even this step will create improvement in the quality of life of your families.
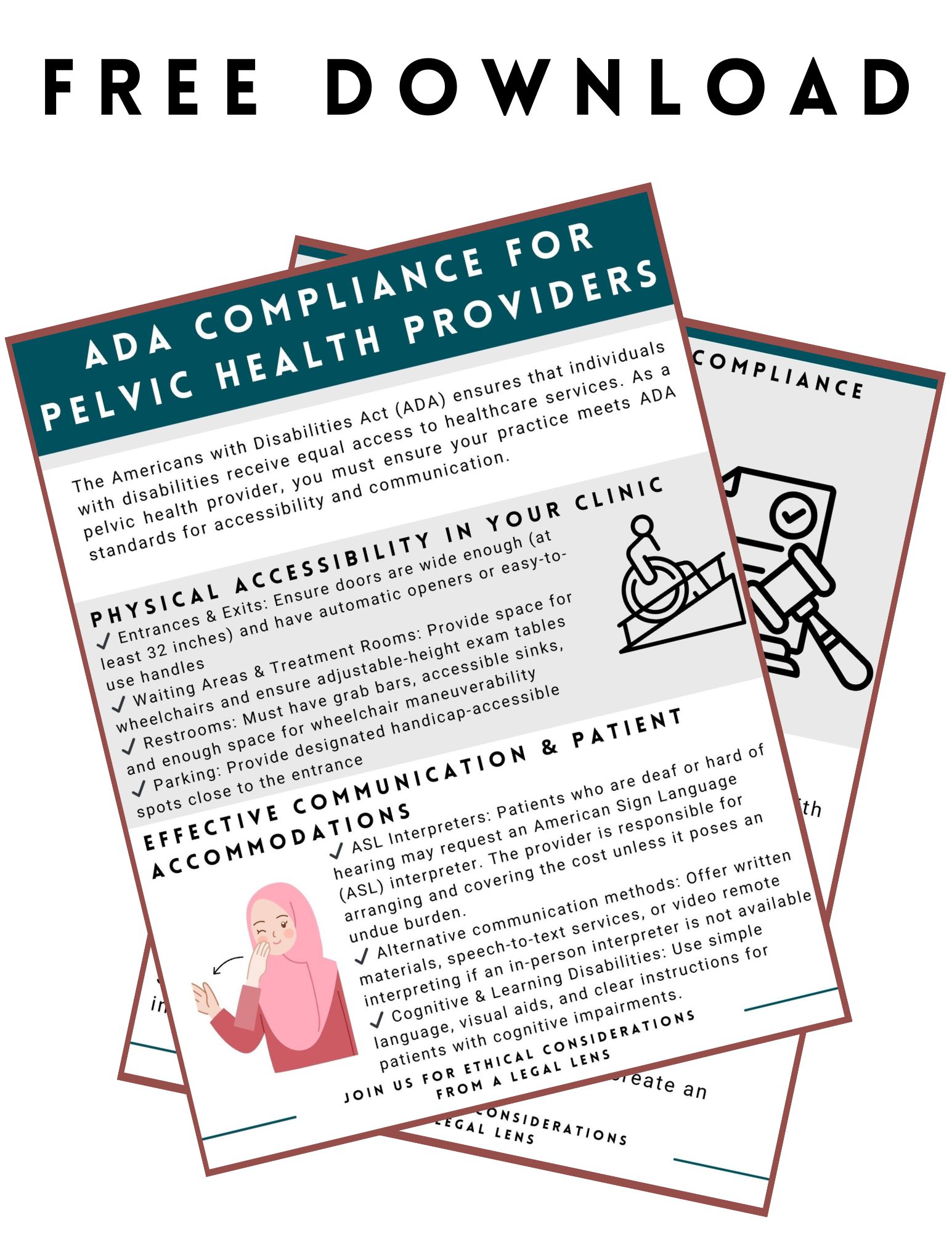

What do you know about the Americans with Disabilities Act (ADA)? You may be thinking that you are a pelvic health provider, so you don’t need to worry about laws, rules, and regulations. You may need to know more about the ADA than you thought.
Scenario: Your patient calls and requests an American Sign Language interpreter during their pelvic health evaluation. You don’t know much about this. You start to research online, and here is what you find…
Google search answer: “Yes, under the Americans with Disabilities Act (ADA), if your practice is a place of public accommodation (e.g., a healthcare provider), you are generally required to provide effective communication, which may include an ASL interpreter when necessary. However, the law considers "undue burden," meaning if the cost is too high relative to your resources, alternative accommodations (like written communication or remote video interpreting) may be acceptable. You cannot charge the patient for the interpreter.”

As I cruise through online Facebook Pelvic Health Mentorship Groups - a weird bedtime passtime that brings me more satisfaction than doom scrolling on TikTok - I hear many providers worried about getting in trouble for patient abandonment. As rehab providers, we have worked hard to get our education, licensure, jobs, and clients that trust us, so it makes sense there would be a fear of losing any of all of those things.
When this concern comes up, I just want to reassure providers and also let them know that there are three continuing education classes in the Herman & Wallace curriculum tailor-made to address other ethical questions and concerns pelvic rehabilitation providers may have:
- Ethical Considerations from a Legal Lens - Scheduled for April 12th
- Ethical Considerations for Pediatric Pelvic Health - Scheduled for July 27th
- Ethical Concerns for Pelvic Health Professionals - Next date TBD
What is patient abandonment? Patient abandonment is a failure of the provider to fulfill their duty of care, leaving a patient without necessary medical support at a critical time. Unlike a patient voluntarily discontinuing care or being referred to another provider, abandonment involves a lack of appropriate communication or planning.

I’ve been “on the record saying” I used to be a modalities skeptic. I didn’t think I used them a ton in my practice and when I switched from a big hospital system to my own private practice, I didn’t have access to the larger equipment machines like the big ultrasound or biofeedback devices.
I have, however, always been a fan of gadgets and tools as a pelvic health provider. For anyone who has ever been to a class where I was a teaching assistant, you’ve likely seen me literally roll in with a giant suitcase full of example things - models, pelvic trainers, examples of belts, braces, dilators, wands, weights, lube samples, pelvic organ stuffies etc. I always called it my toolkit and so many of my peers had this as well. When the Content & Curriculum team asked me to be on the team for writing for this project, I was initially unsure. I didn’t think I used modalities enough or valued them enough to create a two-day course on the topic.
Long story short…I was wrong. What I have learned is I was very wrong, and I use them constantly.

One of the things you'll learn when working with the pediatric population is that they're a different species than adults. Some of the common diagnoses may overlap, such as chronic constipation, fecal smearing, or nocturia. The way they present may be similar and the treatment ideas and philosophy may also overlap. However, how these treatments are implemented may vary when treating a child versus an adult. When I think of treating the pediatric population, I like to divide my thought process and approach into five different groups.
To me, pediatrics can be babies/infants, toddlers, preschool-aged children, elementary school-aged children, and then tweens/teens. It may feel excessive to divide this population into so many subgroups, but each of those groups has its own treatment considerations based on the child's development at that time in their lives. An infant may be working on regulating their GI system as they transition from being in-utero to being born. Toddlers and school-aged children are working through various internal and social benchmarks to help them continue to grow and develop. Likewise, a tween or teen may be managing the changes to their genitourinary system as they work through puberty towards adulthood or grappling with their sexuality and sexual identity as they mature.
Regardless of what stage they are in life, patients will potentially present differently and also need a customized treatment plan to meet them where they are at. When I have colleagues jumping into pediatric pelvic health, I rarely worry they have the clinical skills to help with the physical and physiological challenges a child may face. The place I see many clinicians struggle is how to apply the skills they know to these tiny humans in front of them. Treating reflux in an eighty-year-old versus an 8-week old person is very different.
Rehabilitation providers experience ethical conflicts every day, whether they realize it or not. Just today, I was cruising through social media on my lunch break and saw a post (edited for autonomy) that posed an ethical concern, potentially without its author even knowing. We’ll refer back to this post throughout the blog so please read:
“We have a patient at my clinic whose partner called and scheduled the appointment for the patient. My colleague did the evaluation this morning and said the partner answered all questions for the patient. The partner was inquiring about decreasing posterior pelvic floor tension for anal sex. The therapist found it strange that the partner was answering all the questions for the patient. At this time, I'm really wondering if the partner is forcing the patient to come to pelvic floor therapy and participate. How would you all handle this situation?”
You know this stopped my scroll immediately. Yes, it is a patient care question. However, this situation also brings up so many other intricacies that we encounter as pelvic health providers. I gave my reply and then read others, and this experience made me glad that Herman and Wallace offered three ethics classes talking about ethics for pelvic floor therapists to attend and be able to collaborate on issues just like the one above.


































