
“But nothing showed up on the MRI…”
If you’ve worked with people experiencing chronic pelvic pain, you’ve likely heard this line (or screamed it into the void yourself). Pelvic pain is complex. It’s layered. And when traditional diagnostic tools come up short, patients are left confused, discouraged, and often dismissed.
This is where pain science education becomes not just helpful—it becomes essential. Especially when we’re talking about central sensitization, a sneaky, brain-driven process that keeps the pain party going long after the tissue has healed.
Let’s dig into what this means for our pelvic pain population—and why it’s time every clinician added “pain science educator” to their superpower list.

As rehabilitation professionals, we must ask ourselves: Are we fully educating our patients on all available rehab techniques beyond just Kegels? Here’s an evidence-based overview of penile rehabilitation following radical prostatectomy, emphasizing the importance of a comprehensive approach to restore erectile function and maintain overall penile health.
Understanding Penile Rehabilitation
Penile rehabilitation focuses on enhancing blood flow to the penis after radical prostatectomy (removal of the prostate). Even with nerve-sparing techniques, the cavernous nerves—essential for erections—can sustain trauma. This injury, known as neuropraxia, may require up to two years to recover from, potentially leading to temporary or prolonged changes in erectile function.
Why Rehabilitation Is Critical

For decades, the G-spot has captivated attention, sparking debates in science and popular culture. Is it a distinct anatomical structure, a myth, or simply the same region as the 'female prostate'? While opinions differ, the heart of the discussion may be less about anatomy and more about semantics. Let’s explore the evidence and why this debate persists.
The Anatomy of the G-Spot and Female Prostate
The term 'G-spot' was introduced by German gynecologist Ernst Gräfenberg in 1950, describing a sensitive area on the anterior vaginal wall linked to the urethra and its surrounding tissues (near the bladder neck). In 1981, sexologists Beverly Whipple and John D. Perry popularized the term in their book, emphasizing that this area could enhance pleasure for some women. Notably, the G-spot was never claimed to be a single 'magic button' but rather a zone of heightened sensitivity.
Modern research has shifted focus to the female prostate, also known as Skene’s glands, which are located near the urethra. These glands share histological and functional similarities with the male prostate, contributing to urinary health, sexual arousal, and orgasm.
Evolving Perspectives on the Debate
Early Skepticism: In 2001, Terrence Hines dismissed the G-spot as a 'modern gynecologic myth,' citing inconsistent evidence and suggesting its existence was more cultural than anatomical.

Tara Sullivan instructs her course Sexual Medicine in Pelvic Rehab on October 19-20. Her course provides a thorough introduction to pelvic floor sexual function, dysfunction, and treatment interventions of all sexual orientations, as well as an evidence-based perspective on the value of physical therapy interventions for patients with chronic pelvic pain related to sexual conditions, disorders, and multiple approaches for the treatment of sexual dysfunction including understanding medical diagnosis and management.
Menopause is a natural phase in a woman's life, signaling the end of her reproductive years. While many are familiar with common symptoms such as hot flashes, night sweats, brain fog, and mood changes, there is another less-discussed condition that affects many women: Genitourinary Syndrome of Menopause (GSM). GSM encompasses a range of symptoms affecting the genital and urinary systems, profoundly impacting a woman’s quality of life. Understanding GSM is crucial for women entering menopause and healthcare providers, especially pelvic floor specialists.


Vestibulodynia is defined as pain at the vestibule, which is the area around the opening of the vagina (introitus). Being diagnosed with vestibulodynia can leave patients feeling frustrated because it doesn’t explain WHY they have pain at the vestibule. There are several types of vestibulodynia including infection, inflammation, neoplastic, neurologic, trauma, and hormonal deficiencies.
The most common type of vestibulodynia is caused by hormonal deficiencies known as Hormonally-Mediated Vestibulodynia. This type is caused by hormonal changes including taking birth control, breast feeding, postpartum, estrogen blockers, and peri or post menopause.
The most common cause of Hormonally-Mediated vestibulodynia in younger women (under the age of 25) is systemic birth control (i.e. oral contraceptive pills (OCPs), depo-shot, NuvaRing). Side effects of birth control (BC) such as breakthrough bleeding, nausea, headaches, increased risk of stroke, and abdominal cramping are more commonly discussed among doctors and patients.
Tara Sullivan, PT, DPT, PRPC, WCS, IF is on faculty with Herman & Wallace. She created Sexual Medicine in Pelvic Rehab and co-created Pain Science for the Chronic Pelvic Pain Population which she instructs alongside co-creator Alyson N Lowrey, PT, DPT, OCS. Tara started in the healthcare field as a massage therapist, practicing over ten years including three years of teaching massage and anatomy and physiology. Tara has specialized exclusively in Pelvic Floor Dysfunction treating bowel, bladder, sexual dysfunctions, and pelvic pain since 2012. She is adjunct faculty speaking at the annual conference for the International Society for the Study of Women’s Sexual Health (ISSWSH) and teaches an elective course at Northern Arizona University (NAU) and Franklin Pierce University on Pelvic Health. Tara is very passionate about creating awareness on Pelvic Floor Dysfunction and recently launched her website pelvicfloorspecialist.com to continue educating the public and other healthcare professionals.
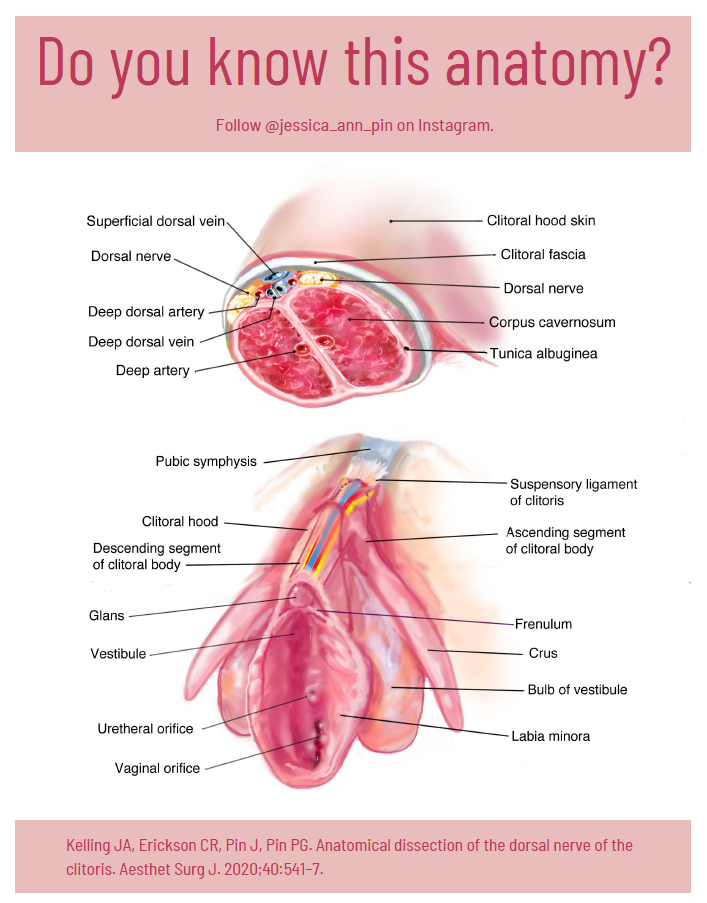
You may have heard of Jessica Pin. She’s been making headlines lately with the unconventional ways she is going about changing what medical texts and schools teach about the clitoris…..which is currently very little. According to Pin, who has a bachelor’s degree in biomedical engineering, the average textbook has over 50 pages more dedicated to the penis than compared to the clitoris. Jessica Pin started her journey to create awareness of clitoral anatomy because at 17 years old she had a labiaplasty leaving her with sensory loss. Jessica’s activism has so far changed 8 medical texts to include detailed anatomy of the clitoris in hopes knowledge of this anatomy is understood well, as it is critical prior to performing surgery near the clitoris.
Loss of clitoral function can also occur after labiaplasty, biopsies, cosmetic surgeries, and repair. As pelvic rehab providers, there is a level of responsibility we have to help shift the narrative. How often have we seen or heard similar stories of young patients undergoing cosmetic surgeries to try to ‘look normal’ or apologize for the way they look? We have such a unique position to spend time educating our patients and treating sexual dysfunctions across the spectrum.



































