Misbehaving Bladder - A Novel Approach, Part 2
This is Part 2 of Tuesday's, April 27, 2021, blog Misbehaving Bladders and Cluster Drinking - A Novel Approach, Part 1.
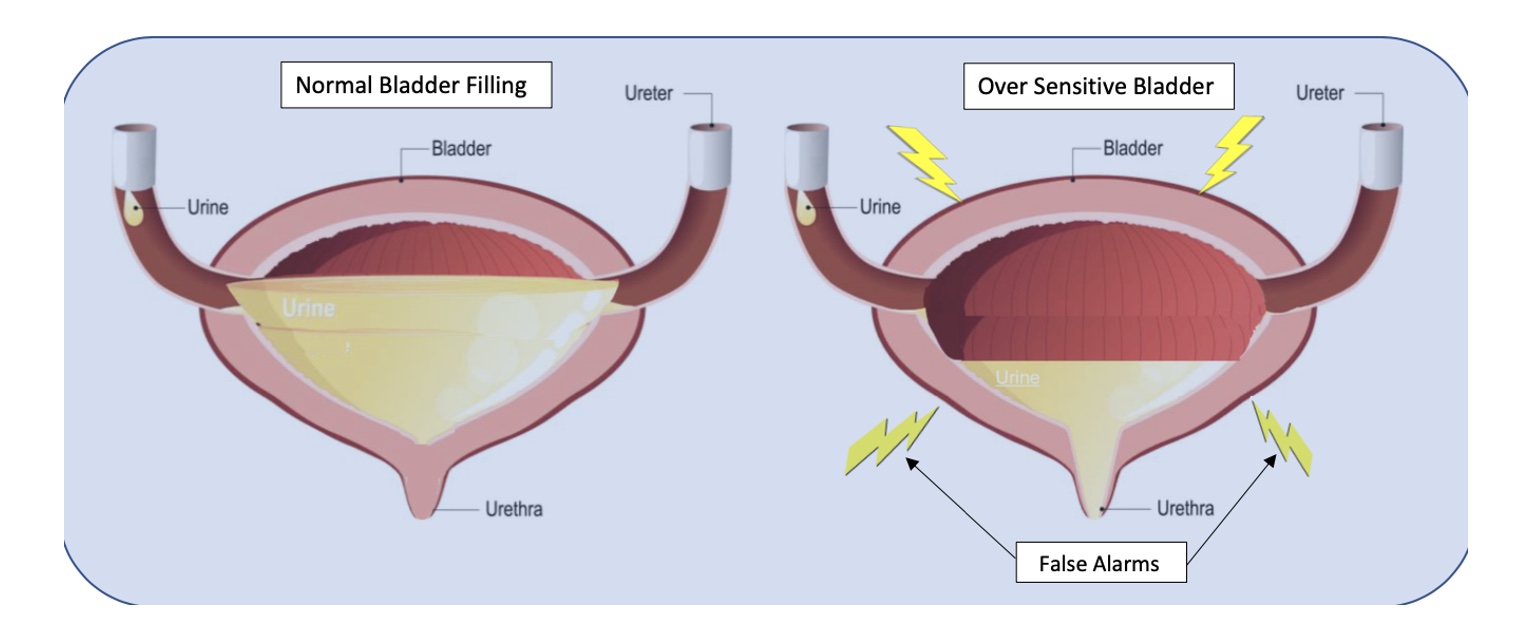
Bladder capacity ranges from around 400-500ml (13-16 oz). The use of a measuring cup or water bottle can be very helpful to teach this concept. We certainly don’t have to strive for a full bladder volume, but it is important to illustrate that 2-3 ounces are in fact “just in case” voids. I explain to patients that in situations of overactive or irritated bladders, the receptors in their bladder walls are hypersensitive and sending “false alarm” messages when only a small amount of urine is present. The kidneys are always active and refilling the bladder, so it will never be totally empty per se, therefore it must be desensitized and retrained to be a viable, reliable, and reasonably comfortable storage vessel.
With the Cluster Drinking Approach, it is important to try and drink the fluid in a short enough period of time to ensure an increased rate of bladder filling for this to be effective, but you must be careful to monitor the bladder irritability with the training. A fuller bladder will experience more pressure, but this also helps with urine flow during voids. We then embark on this process of retraining and using their bladder diaries to help us with detective work to determine optimal amounts of fluid intake in each cluster and the optimal timing of fluid intake, number of clusters, etc. for their daily schedules. It may take some time to get used to the new habits. It can be hard for some patients who are used to sipping on their water bottle all day long, and they can feel dehydrated. This is a habit and learned response and can be retrained with some gradual investment in the process. Once patients experience the rewarding outcomes, they are usually willing to make the changes.
Based on diary findings, we modify types of fluids as necessary, my motto being: minimal disruption to achieve desired results. Why give up coffee and all favorite beverages if not necessary? Sometimes making modifications on timing and amount of intake works just fine, other times we tweak the beverage types. I also teach and integrate urge suppression strategies (USS) as well, to help with the process of retraining; and of course, address breathing, pelvic floor dysfunctions, connective tissue restrictions, and chronic constipation, but the variable which sets this approach apart is the cluster drinking.
According to Washington state urogynecologist Elizabeth A. Miller, MD FPMRS, a practitioner at Overlake and Swedish Medical Centers, the Cluster Drinking Approach works similarly to some OAB medications in training your bladder to hold more urine. She endorses the Cluster Drinking Approach as a viable first-line treatment option since it works naturally without harmful side effects. Results are often profound and rapid even for folks who have been struggling with these bladder issues for years. Likewise, leaking issues tend to diminish as the bladder training is mastered. Patients can structure riskier activities around this cluster program, i.e. plan their Zumba after cluster intake and output. The same goes for major outings where one will not be near a bathroom. Even my constipation patients have benefitted due to a more reliable intake of adequate fluid.
Nocturia is a bit of a different situation because of the role of kidney hormones, but I have found this approach to be quite effective for many patients whose lives and sleep are impacted by this problem. The Cluster Drinking Approach helps these patients to structure their fluid intake during daytime hours, and I teach them to heed the 1st overnight urge if it is within 2-3 hours after going to sleep. Then if they awaken again, I coach them to use the mantra “the bladder is a storage vessel”, analyze their last intake and output, and permit themselves to use the Urge Suppression Strategies, and go back to sleep without worrying that their bladder will explode. The other good news is after their bladders (and brains) are “retrained”, and you have done your PT magic, they can often return to more natural drinking patterns without negative consequences.
Fun Fact: Even Did you know that under anesthesia the amazing expandable bladder can hold over 1 liter?!
Kathy E. Golic, PT is a physical therapist at Overlake Hospital Medical Center in Bellevue, Washington.
By accepting you will be accessing a service provided by a third-party external to https://hermanwallace.com/







































