This is Part 2 of Tuesday's, April 27, 2021, blog Misbehaving Bladders and Cluster Drinking - A Novel Approach, Part 1.
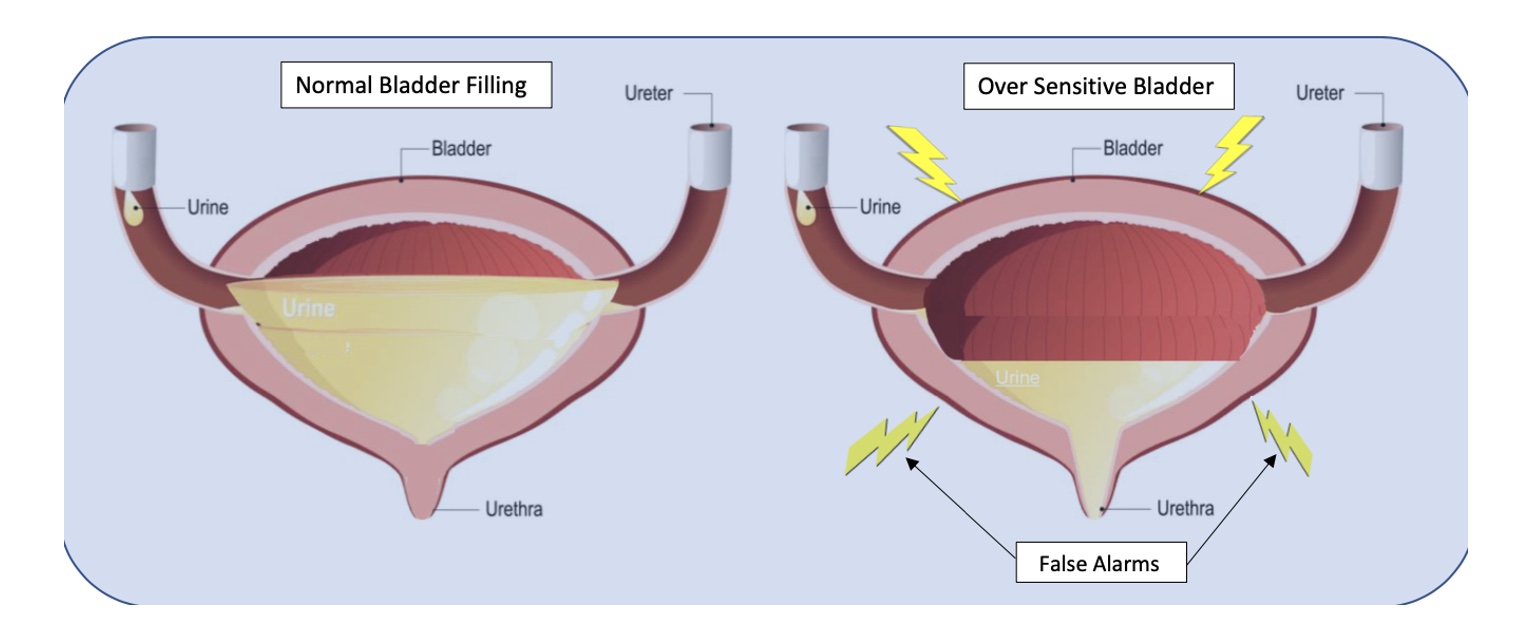
Bladder capacity ranges from around 400-500ml (13-16 oz). The use of a measuring cup or water bottle can be very helpful to teach this concept. We certainly don’t have to strive for a full bladder volume, but it is important to illustrate that 2-3 ounces are in fact “just in case” voids. I explain to patients that in situations of overactive or irritated bladders, the receptors in their bladder walls are hypersensitive and sending “false alarm” messages when only a small amount of urine is present. The kidneys are always active and refilling the bladder, so it will never be totally empty per se, therefore it must be desensitized and retrained to be a viable, reliable, and reasonably comfortable storage vessel.
There have been many constructive blogs about managing symptoms of overactive and misbehaving bladders, but I want to share an approach I have been using successfully for many years. Not only does this approach work for the majority of my patients in terms of addressing urgency, frequency, and urine leakage, but results are often quite rapid. After treating patients with modest success for many years with the traditional treatment approaches and noting that too often patients would plateau or results were just not effective or fast enough, I created my own approach to help these patients. I call it Cluster Drinking Approach and explain to my patients that cluster drinking begets cluster voiding.
When folks sip fluid, even water, all day long, it is hard for them to know when their bladder is full enough to warrant a trip to the bathroom. In patients with oversensitive or irritated bladders, the sensory receptors in the bladder wall are agitated and so often send false, unreliable signals,
when there is not much urine present. So they continue to struggle with urges and frequency and sometimes urine leakage. However, when they divide their fluid intake into 3-4, or sometimes even 5 or more, “clusters” then their bladders fill more predictably. They can sense it, and based on timing and amount of intake, they can reliably determine when the urges are accurate.
This requires a mindful and analytical approach to help retrain their bladders. The amount of intake and number of clusters are selected based on the level of bladder irritability, the patient’s schedule, as well as their weight, age, and level of anxiety. The variables can be modified according to their daily schedules, and their progress. Coupled with my mantra, “The bladder is a storage vessel, it is meant to hold urine!” this approach has been life-changing for many patients, and often in just a few visits!
Here is an example to illustrate what this might look like based on 60 fluid oz of daily intake. And important to share this pearl...In case you did not know...the adage of 8 glasses of 8 ounces of water was not based on research. So this will be quite individualized.
INTAKE
Cluster 1: 7:00 am-7:30am Consume 20 oz of fluid
Cluster 2: 11:30-12:00 Consume next 15 oz
Cluster 3: 4:30-5:00 Consume 15 more oz
Cluster 4: 7:00-7:30 Consume final 10 oz
Total Intake: 60 oz, plus sips for bedtime pills
OUTPUT
Void: Reliable urge 60-90 mins later
Possibly a 2nd void within the next 60 mins
Void: 1-2 times in next 60-120 minutes
Void: next 60-120 minutes
Void :next 60-120 mins
Final void: Bedtime
Total voids: generally 5-8, depending on actual intake
Kathy E. Golic, PT is a physical therapist at Overlake Hospital Medical Center in North Bend, Washington.
This post is a follow-up to the February 20th post written by Nancy Cullinane, "Pelvic Floor One is Heading to Kenya"
By the time folks are reading this, Nancy Cullinane, PT, MHS, WCS, Terri Lannigan, PT, DPT, OCS, and I will likely be in a warm, crowded classroom in Nairobi, Kenya helping 30+ “physios” navigate the world of misbehaving bladders, detailed anatomy description, and their first internal lab experiences. No doubt it will be both challenging and extremely rewarding. We are so grateful to the Herman & Wallace Pelvic Rehab Institute for sharing their curriculum in partnership with the Jackson Clinics Foundation to allow us to offer their valuable curriculum in order to affect positive health care changes.
I personally am humbled and honored to get to play a small but key role in the development of foundational knowledge and skills for these women PT’s who will no doubt change the lives of countless Kenyan women, and, consequently, their families.








































