Nerve Entrapments and Pelvic Pain
This post was written by Elizabeth Hampton PT, WCS, BCIA-PMB, who teaches the course Finding the Driver in Pelvic Pain: Musculoskeletal Factors in Pelvic Floor Dysfunction. You can catch Elizabeth teaching this course in April in Milwaukee.
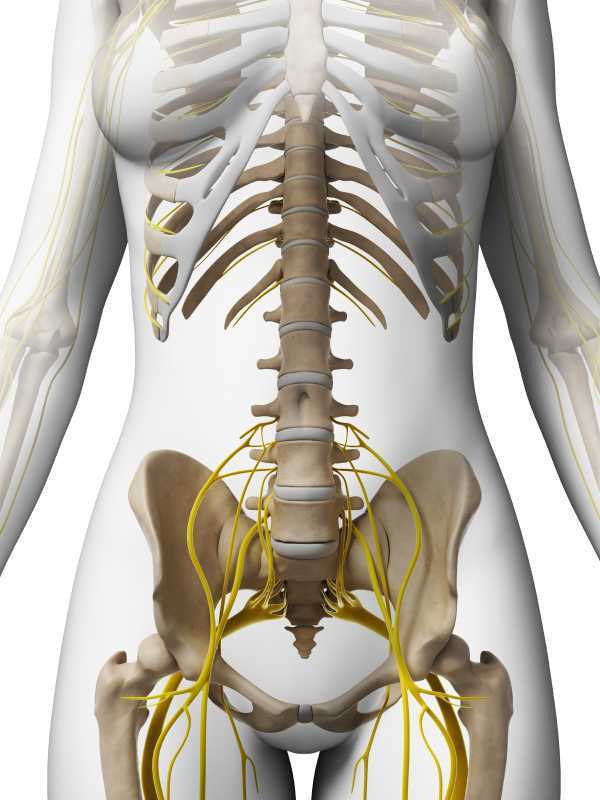
Chronic pelvic pain has multifactorial etiology, which may include urogynecologic, colorectal, gastrointestinal, sexual, neuropsychiatric, neurological and musculoskeletal disorders. (Biasi et al 2014) Herman and Wallace faculty member, Elizabeth Hampton PT, WCS, BCB-PMD has developed an evidence based systematic screen for pelvic pain that she presents in her course “Finding the Driver in Pelvic Pain”. One possible origin of pelvic pain as well as chronic psoas pain and hypertonus may arise from genitofemoral, ilioinguinal or iliohypogastric neuralgia, the screening of which is addressed in the “Finding the Driver” extrapelvic exam.
The iliohypogastric nerve arises from the anterior ramus of the L1 spinal nerve and is contributed to by the subcostal nerve arising from T12. This sensory nerve travels laterally through the psoas major and quadratus lumborum deep to the kidneys, piercing the transverse abdominis and dividing into the lateral and anterior cutaneous branches between the TVA and internal oblique. The anterior cutaneous branch provides suprapubic sensation and the lateral cutaneous branch provides sensation to the superiolateral gluteal area, lateral to the area innervated by the superior cluneal nerve. (10)
The ilioinguinal nerve arises from the L1 spinal levels, passes through the psoas major inferior to the iliohypogastric nerve, across the quadratus lumborum and iliacus and lastly through the transversus abdominis along with the iliohypogastric nerve between the transverse abdominis and the internal oblique muscle. (7) The ilioinguinal nerve supplies the skin of the medial thigh, upper part of the scrotum/labia as well as penile root (5).
The genitofemoral nerve arises from the L1 and L2 spinal levels and splits into the genital and femoral branches after passing through the psoas muscle. (1). The genital branch (motor and sensory) passes through the inguinal canal and innervates the upper area of the scrotum of men. In women it runs alongside the round ligament and innervates the area of the skin of the mons pubis and labia majora. The motor function of the genital branch is associated with the cremasteric reflex. The femoral (sensory) branch runs alongside the external iliac artery, through the inguinal canal and innervates the skin of the upper anterior thigh. (8)
Differential diagnosis of entrapment of one of the three nerves can be challenging due to their overlapping sensory innervations and anatomic variability. Rab et al found up to 4 different patterns of anatomical variability in these nerve pathways. (9)
Transient or lasting genitofemoral, ilioinguinal and iliohypogastric neuralgia results from compression or irritation of these nerves anywhere along their pathway: from their spinal origin to distal pathways. Cesmebasi at al report that “neuropathy can result in paresthesias, burning pain, and hypoalgesia associated with the nerve distributions. “ (11) These entrapments may be associated with surgery, T12-L2 segmental dysfunction or HNP, constipation and is commonly observed clinically alongside psoas overactivity and pain. Lichtenstein found that up groin pain after hernia surgery ranged from 6-29% with Bischoff et al (2012) (6) denoting the post-operative neuralgia ranging from 5-10%.
Differential diagnosis of nerve entrapments are key skills in the screening of musculoskeletal contributing factors to pelvic pain and physical therapists are uniquely skilled to put all of the puzzle pieces together in these complex clients. Finding the Driver is being offered twice in 2015: April 23-25, 2015 at Marquette University and again in the fall. Check Herman & Wallace's webite for further details.
http://www.gotpaindocs.com/gentfmrl_nurlga.htm
Tubbs et al.Journal of Neurosurgery: Spine. March 2005 / Vol. 2 / No. 3 / Pages 335-338. Anatomical landmarks for the lumbar plexus on the posterior abdominal wall. http://thejns.org/doi/abs/10.3171/spi.2005.2.3.0335
Phillips EH. Surgical Endoscopy. January 1995, Volume 9, Issue 1, pp 16-21. Incidence of complications following laparoscopic hernioplasty
http://link.springer.com/article/10.1007/s00268-012-1657-2
Tsu W et al. World Journal of Surgery. October 2012, Volume 36, Issue 10, pp 2311-2319. Preservation Versus Division of Ilioinguinal Nerve on Open Mesh Repair of Inguinal Hernia: A Meta-analysis of Randomized Controlled Trials
Bischoff JM. Hernia. October 2012, Volume 16, Issue 5, pp 573-577. Does nerve identification during open inguinal herniorrhaphy reduce the risk of nerve damage and persistent pain?
http://en.wikipedia.org/wiki/Ilioinguinal_nerve
http://en.wikipedia.org/wiki/Genitofemoral_nerve
Rab M, Ebmer And J, Dellon AL.. Anatomic variability of the ilioinguinal and genitofemoral nerve: implications for the treatment of groin pain.
Plastic and Reconstructive Surgery [2001, 108(6):1618-1623].
http://en.wikipedia.org/wiki/Cutaneous_innervation_of_the_lower_limbs
Cesmebasi et al (2014) Genitofemoral neuralgia: A review. Clinical Anatomy. Volume 28, Issue 1, pages 128–135, January 2015. http://onlinelibrary.wiley.com/doi/10.1002/ca.22481/abstract
By accepting you will be accessing a service provided by a third-party external to https://hermanwallace.com/




































