In the United States, estimated direct medical costs for outpatient visits for chronic pelvic pain (CPP) is more than $2.8 billion per year.1 In a 2017 study in the Clinical Journal of Pain by Sanses et al, a detailed musculoskeletal exam of clients with CPP can assist both physicians as well as physical therapists in differential diagnosis and appropriate referrals for this population.
Evaluating a client with pelvic pain requires a skill set that includes direct pelvic floor as well as musculoskeletal test item clusters. The prioritization of which depends upon many factors including clinician discipline, experience, specialty vs. general setting, as well as client history, presentation and goals. In addition to the direct pelvic floor assessment, there are additional key musculoskeletal screening tests that are an essential part of a pelvic pain assessment. New this year, my course Finding the Driver in Pelvic Pain will incorporate the use of Real Time Ultrasound in neuromuscular assessment and re-education of the pelvic floor and abdominal wall during the Sunday morning lab session.
Peery et al (2012) noted that abdominal pain was one of the most common presenting reasons for an outpatient physician visit in the United States. Abdominal pain is one of the many complaints that our clients may report requiring differential diagnosis including urogynecologic, colorectal, musculoskeletal, visceral or neurogenic causes. Lower abdominal quadrant pain may denote serious emergent pathology. Clinical findings, physical exam and client symptoms in addition to smart differential diagnosis must be used to determine if the abdominal pain is musculoskeletal in nature. Direct access requires physical therapists to perform a skilled initial screening for abdominal pain in order to determine if it is abdominal wall versus a visceral origin. Physicians are fluent in ruling out emergent pathology but may not be familiar with musculoskeletal tests for non-emergent pathology. Assessment of bowel and bladder function and habits are essential to perform. This blog specifically addresses three physical exam tests that can be performed as part of abdominal wall pain screening. According to Cartwright et al, the location of the abdominal pain should drive the evaluation.
I’m Elizabeth Hampton PT, DPT, WCS, BCB-PMD and I teach “Finding the Driver in Pelvic Pain”, which offers practitioners a systematic screening approach to rule in or rule out contributing factors to pelvic pain. This course helps clinicians to understand and screen for the common co-morbidities associated with pelvic floor dysfunction, like labral tears, discogenic low back pain, nerve entrapments, coccygeal dysfunction, and more. Importantly, it also coaches clinicians to organize information in a way that enables them to prioritize interventions in complex cases. I've noticed that there are some questions that course participants frequently have as they talk through common themes in their care challenges and wrote this blog to share some clinical pearls you may find to be helpful for your own practice or as an explanation to your clients.
Here are some of the most common questions that I get when teaching Finding the Driver in Pelvic Pain:
1) Question: How do I even start to organize information when a client has a complex history and I am feeling overwhelmed?
I write down a road map with key categories: Bowel and bladder; Spine; Sacroiliac Joint/Pubic Symphysis; Hip; Pelvic floor muscles; biomechanics; respiration; neural upregulation; whatever details can be fit into ‘big buckets’ of information. I use it to both organize my thoughts for my notes, as well as educate the client as to what my findings are and the design of their treatment program.
2) Question: How do you get your clients to do a bowel and bladder diary?
I am proud to say that I can talk anyone into a 7 day bowel and bladder diary because I tell them how incredibly helpful it is to understand the way their body responds to what they eat, drink, and daily habits. It’s my secret weapon to snag clients to start connecting with their body and listening to their details, educate about defecation ergonomics and what happens in multiple systems when there is pelvic floor overactivity. It’s a great teaching tool that facilitates self-reflection and how their self-care choices impact their body’s behavior.
3) Question: How do you educate clients about pelvic floor function so they don’t focus so much on Kegels?
Pelvic floor muscles do three things:
They contract gently, or powerfully, with no discomfort, and totally normal breathing; PFMs should have the same kind of nuanced control like your voice does: they should be able to do a gentle contraction, like a “whisper” or a powerful contraction, like a “shout”, depending on the task position and intent.
Influencing pelvic floor EMG activity through hip joint mobilization and positioning
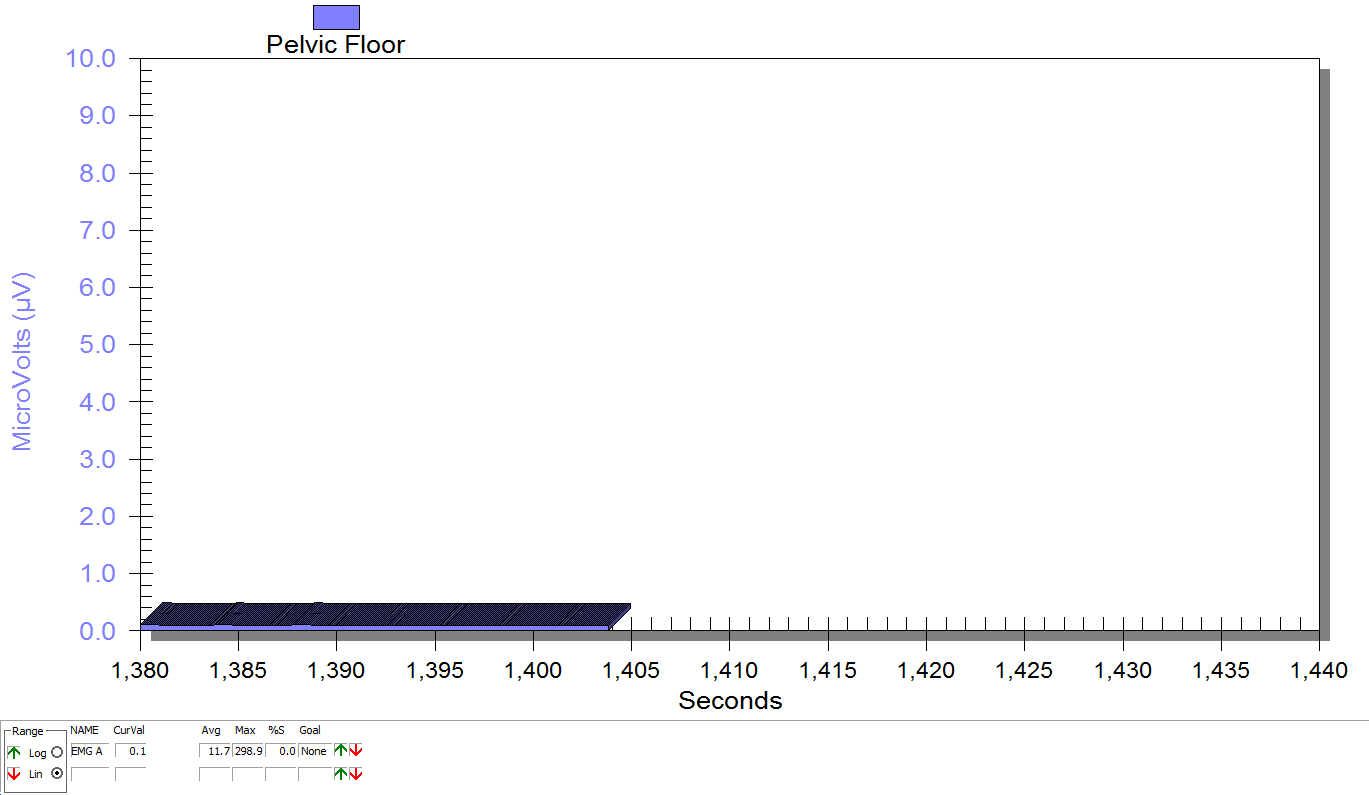
EMG is a helpful tool to observe pelvic floor muscle activity and how it is influenced by everything from regional musculoskeletal factors and mucosal health, to client motor control, awareness, and comfort.
In this post I will discuss the case of one client who was referred for dyspareunia treatment, and whose SEMG findings are outlined in Figures 1-3. She had validated test item clusters for right hip labral tear as well as femoral acetabular impingement, in addition to right sided pelvic floor muscle overactivity and sensitivity with less than 3 ounces of palpation pressure.
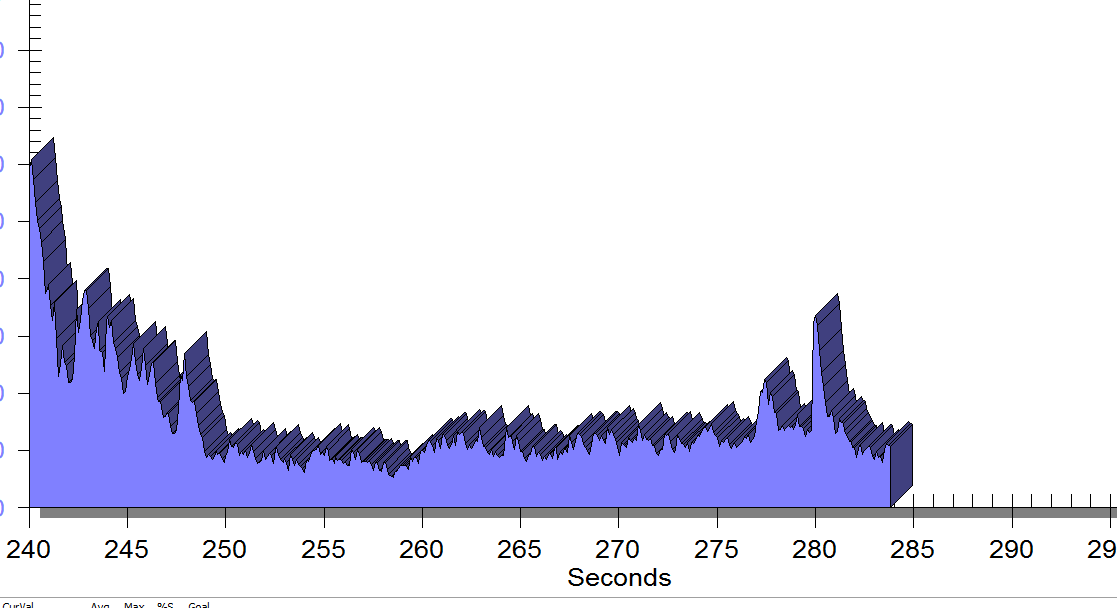
The figures below demonstrate peri-anal SEMG response of pelvic floor muscles within a single treatment session, which included sacral unloading in supine as well as hip joint mobilization to demonstrate the relationship between her pelvic floor and her hips. Our focus for this SEMG downtraining treatment was to enable her to understand the connection between her pelvic floor muscle holding patterns and her body’s preferences to remain out of ranges of motion that impinged and irritated her hip.
You went through Herman and Wallace’s Pelvic Floor 1 course and were ready to treat your clients with incontinence and prolapse……….then you started getting referrals for clients with pelvic pain.
You have 45-60 minutes (or longer if you are lucky) to create a safe and comfortable environment, skillfully establish trust and rapport and gather objective and subjective data to get to the bottom of their pain. You want to give them the summary of your findings, their rehab road map and something to work on at home. By the end of the visit, you need to have completed their problem list and plan of care. Where do you start?
No pressure, right?
Today we get the opportunity to hear from Herman & Wallace faculty member Elizabeth Hampton PT, WCS, BCIA-PMB! Elizabeth has been kind enough to offer her insights about the diagnosis of pelvic rehabilitation patients. Join Elizabeth at Finding the Driver in Pelvic Pain this November in Houston, TX in order to learn evaluation tools for complex pelvic pain clients!
Having taught for Herman and Wallace since 2006, I have a few observations that have been consistent over the years. Clinicians want their clients to get better, so much so that they are ready to jump in to treatment before having a solid problem list and validated findings. I can understand this: after a 3 day course we have clients Monday morning at 8 a.m. who have been waiting for us to take this course so we can get them better! We had better be smart ASAP! But what do we do when we are treating symptoms rather than understanding the primary, secondary and tertiary factors in their condition?
Finding the Driver in Pelvic Pain is a course that is a foundational first step in screening the pelvic pain client. It is a great place to start. I developed the course because there was no evidence based comprehensive factors that had been established as fundamentals for screening a pelvic pain client.
This post was written by Elizabeth Hampton PT, WCS, BCIA-PMB, who teaches the course Finding the Driver in Pelvic Pain: Musculoskeletal Factors in Pelvic Floor Dysfunction. You can catch Elizabeth teaching this course in April in Milwaukee.
Chronic pelvic pain has multifactorial etiology, which may include urogynecologic, colorectal, gastrointestinal, sexual, neuropsychiatric, neurological and musculoskeletal disorders. (Biasi et al 2014) Herman and Wallace faculty member, Elizabeth Hampton PT, WCS, BCB-PMD has developed an evidence based systematic screen for pelvic pain that she presents in her course “Finding the Driver in Pelvic Pain”. One possible origin of pelvic pain as well as chronic psoas pain and hypertonus may arise from genitofemoral, ilioinguinal or iliohypogastric neuralgia, the screening of which is addressed in the “Finding the Driver” extrapelvic exam.
The iliohypogastric nerve arises from the anterior ramus of the L1 spinal nerve and is contributed to by the subcostal nerve arising from T12. This sensory nerve travels laterally through the psoas major and quadratus lumborum deep to the kidneys, piercing the transverse abdominis and dividing into the lateral and anterior cutaneous branches between the TVA and internal oblique. The anterior cutaneous branch provides suprapubic sensation and the lateral cutaneous branch provides sensation to the superiolateral gluteal area, lateral to the area innervated by the superior cluneal nerve. (10)
This post was written by H&W instructor Elizabeth Hampton. Elizabeth will be presenting her Finding the Driver course in Milwaukee in April!
One of the most consistent questions that we hear at the Pelvic Floor 2B course is, “How do you choose between a pelvic floor and a musculoskeletal exam during your first visit with a pelvic pain client?” The answer depends on a number of factors, which include your clinical reasoning, toolbox, the client’s presentation, the clinical specialty, and expectations of the referring provider as well as the expectations of the client. It can be stressful to imagine gathering a detailed history, testing, client education and a home program within the first visit! Now that we have less time and total visits to evaluate and treat these complex issues, it can be overwhelming to know where to start.
Chronic pelvic pain has multifactorial etiology, which may include urogynecologic, colorectal, gastrointestinal, sexual, neuropsychiatric, neurological and musculoskeletal disorders. (Biasi et al 2014) Herman and Wallace faculty member, Elizabeth Hampton PT, WCS, BCB-PMD has developed an evidence based systematic screen for pelvic pain that she presents in her course “Finding the Driver in Pelvic Pain”. “There are a number of extraordinary models that exist for treatment of pelvic pain including Diane Lee’s Integrated System of Function, Postural Restoration Institute, Institute of Physical Art and more,” states Hampton. “However, regardless of the treatment style and expertise of the clinician, each clinician should be able to perform fundamental tissue specific screening. If a client has L45 discogenic LBP with segmental hypermobility into extension, femoral acetabular impingement, urinary frequency > 12/day as well as constipation contributed to by puborectalis functional and structural shortness, all clinicians should be able to arrive at the same fundamental findings during their screening exam. The driver of the PFM overactivity(3) needs to be explored further as local treatment alone (biofeedback and downtraining) will not resolve until the condition causing the hypertonus is found and treated.” Finding the Driver in Pelvic Pain is a course that models a comprehensive intrapelvic and extrapelvic screening exam with evidence based validated testing to rule out red flags, understand key factors in the client’s case as well as develop clinical reasoning for prioritizing treatment and plan of care. The screening exam complements any treatment model as it identifies tissue specific pain generators and structural condition, which will lead the clinician to follow their clinical reasoning and treatment model. Once the fundamentals are established, the clinician can move beyond screening and drill down into treatment of key factors which may include specific muscle gripping patterns, arthokinematic assessment and respiratory evaluation and retraining, among others.



































