 Several weeks ago, I evaluated a patient who was referred to me from a fellow physical therapist. The patient was suffering from sacroiliac joint and low back pain. The patient is a 34-year-old nulliparous woman who is physically fit and participates in several outdoor activities. The therapist had fully evaluated the patient and did not find any articular issues within her spine or pelvis. What she did find was weakness in her local stabilizing muscles and tightness in her global stabilizing muscles. The therapist has an ample amount of clinical experience at treating low back and pelvic pain issues. She is adept at using different verbal cues, positions, and tactile cueing in order to help encourage proper activation of the local core muscles. However, the therapist knew the patient was not getting her local core muscles to fire properly. She didn’t know what else to do with this patient in order to get her to properly activate these muscles. She had tried numerous positions, verbal and tactile cueing without success.
Several weeks ago, I evaluated a patient who was referred to me from a fellow physical therapist. The patient was suffering from sacroiliac joint and low back pain. The patient is a 34-year-old nulliparous woman who is physically fit and participates in several outdoor activities. The therapist had fully evaluated the patient and did not find any articular issues within her spine or pelvis. What she did find was weakness in her local stabilizing muscles and tightness in her global stabilizing muscles. The therapist has an ample amount of clinical experience at treating low back and pelvic pain issues. She is adept at using different verbal cues, positions, and tactile cueing in order to help encourage proper activation of the local core muscles. However, the therapist knew the patient was not getting her local core muscles to fire properly. She didn’t know what else to do with this patient in order to get her to properly activate these muscles. She had tried numerous positions, verbal and tactile cueing without success.
Do you ever have patients where you feel stuck, who are not progressing as you would like them to in treatment? We all do! It is frustrating, isn’t it? The physical therapist called me and asked me to evaluate the patient using real-time ultrasound imaging. The therapist said “If the patient can just see what she is doing, she will then be able to learn how to work the muscles correctly.” She referred the patient to me so I could use ultrasound imaging within the treatment to better assess her activation strategies and use the imaging for biofeedback for with the patient. The patient was amazed with the ability to see what the different layers of muscles were doing. We found she was contracting her TA but only on her left side, and her deep multifidus was not firing at all. Using the ultrasound images, the patient was able to learn the proper way to activate her muscles. She is now working on a strengthening program for her local core muscles including her TA, pelvic floor, and multifidus. Within two treatments, the patient was able to fire her muscles in a different way and reports her back has felt better than it has in years!

The Pathway Ultrasound Imaging System, available from The Prometheus Group, is a portable ultrasound solution for pelvic rehab
I cannot emphasize enough how using ultrasound might change your practice! It not only can help you when you are stuck with a patient’s progress, but it can attract more patients to your practice. There are a lot of visual learners out there and access to visual images in therapy can influence progress and the results that are achieved. You not only can use the ultrasound to retrain the local core muscles for back and pelvic instability patients, but you can use it for incontinence patients, prolapse patients, and post prostatectomy patients as well. You can strengthen the pelvic floor without having to disrobe the patient each visit. How many men and women would appreciate that?
If you are interested in learning more about how you can use ultrasound in your practice, join me in August in New Jersey, or in November in California for Rehabilitative Ultrasound Imaging - Women's Health and Orthopedic Topics! See you there!
In a previous post on The Pelvic Rehab Report Sagira Vora, PT, MPT, WCS, PRPC told us how "women with sexually adverse experiences tend to have impaired genital response when in consensual sexual situations, however, women who do not have sexual abuse histories and but have sexual pain tend to have appropriate genital response." Today Sagira helps us understand how the pelvic floor responds to consensual sexual activity in women with a history of sexual trauma.
Today we try to look for answers for questions that came up during the last blogs.
 How does the cohort that has had adverse sexual experiences present? How do women with history of sexual trauma process sexual experiences? How does the pelvic floor present or respond to consensual sexual situations when a woman has been abused in the past?
How does the cohort that has had adverse sexual experiences present? How do women with history of sexual trauma process sexual experiences? How does the pelvic floor present or respond to consensual sexual situations when a woman has been abused in the past?
To answer these questions, it’s important to understand two facts about the pelvic floor. 1) the pelvic floor plays a role in emotional processing1, and 2) muscle activity in all muscles, including the pelvic floor, increases with exposure to stress and during anxiety evoking experiences2.
We explored in the last blog that women with sexual abuse histories responded with increased pelvic floor overactivity when watching movie clips with sexually threatening and consensual sexual content. Apparently, for women with sexual abuse history even consensual sexual situations can be experienced as threatening1.
Lehrer et. al. found overactivity in the neuronal and hormonal circuits that increase sexual arousal and activity. These circuits are already overactive in individuals who have Post Traumatic Stress Disorder (PTSD), and increased activity can increase anxiety, fear and other symptoms of PTSD instead of normal sexual arousal and excitement during a sexual experience2. For the woman with PTSD this means that sexual arousal signals impending threat rather than pleasure1. And as we already learned in previous blogs and above that when humans feel threatened they respond by tightening muscles and most notably the pelvic floor muscle.
Significant co-relation is found between sexual abuse, subsequent PTSD and chronic pelvic pain3. Hooker et. al, found irritable bowel syndrome, pelvic pain, and physical and sexual abuse to be the most commonly diagnosed together4. More importantly, when patients were successfully treated for PTSD they continued to be 2.7 times more likely to have pelvic floor dysfunction and 2.4 times more likely to have sexual dysfunction. This builds the case for interventions that are multidisciplinary to help patients of abuse and sexual assault, with the pelvic floor therapist playing a significant role.
In the next blog, lets explore how the pelvic floor therapist can work with a counselor and a sex therapist to help the woman with sexual pain dysfunction.
Anna Padoa and Talli Rosenbaum. The overactive pelvic floor. Springer. 1st ed. 2016
Yehuda R, Lehrner A, Rosenbaum TY. PTSD and sexual dysfunction in men and women. J Sex Med. 2015:12(5):1107-19
Blok BF. Holstege G. The neuronal control of micturition and its relation to the emotional motor system. Prog Brain Res. 1996; 107:113-26
Para ML, Chen LP, Goranson EN, Sattler AL, Colbenson KM, Seime RJ, Et. al. Sexual abuse and lifetime diagnoses of somatic disorders. JAMA. 2013; 302:550-61
Hooker AB, van Moorst BR, van Haarst EP, Van Ootegehem NAM, van Dijken DKE, Heres MHB, Chronic pelvic pain: evaluation of the epidemiology, baseline characteristics, and clinical variables via a prospective and multidisciplinary approach. Clin Exp Obstet Gynecol. 2013; 40:492-8
In a previous post on The Pelvic Rehab Report Sagira Vora, PT, MPT, WCS, PRPC shared that "cognitive-behavioral therapy appears to play a significant role in improving sexual function in women". Today, in part three of her ongoing series on sex and pelvic health, Sagira explores how sexual pain affects sexual dysfunction in women.
 After having explored what allows for women to have pleasurable sexual experiences including pain-free sex and mind-blowing orgasms, we now turn towards our cohort that have pain with sex and intimacy. How does this group differ from women who do not have pain with sex? Are there some common factors with this group of women, and perhaps understanding these factors may help the pelvic floor therapist render more effective and successful treatment?
After having explored what allows for women to have pleasurable sexual experiences including pain-free sex and mind-blowing orgasms, we now turn towards our cohort that have pain with sex and intimacy. How does this group differ from women who do not have pain with sex? Are there some common factors with this group of women, and perhaps understanding these factors may help the pelvic floor therapist render more effective and successful treatment?
There are few studies exploring sexual arousal in women with sexual pain disorders. However, their findings are remarkable. Brauer and colleagues found that genital response, as measured by vaginal photoplethysmography and subjective reports, was found to be equal in women with sexual pain vs. women who did not have pain, when they were shown oral sex and intercourse movie clips. This and other studies have shown that genital response in women with dyspareunia is not impaired. Genital response in women with dyspareunia is however, effected by fear of pain. When Brauer and colleagues subjected women with dyspareunia to threat of electrical shock (not actual shock) while watching an erotic movie clip they found that women with dyspareunia had much diminished sexual response including diminished genital arousal. But Spano and Lamont found that genital response was diminished by fear of pain equally in women with sexual pain and women without sexual pain.
Fear of pain also resulted in increased muscle activity in the pelvic floor. However, this increase was noted in women with pain and women without sexual pain equally and was noted with exposure to sexually threatening film clips as well as threatening film clips without sexual content. The conclusion, then, from these results is that the pelvic floor plays a role in emotional processing and tightening, or overactivity is a protective response noted in all women regardless of sexual pain history.
The one difference that was noted was with women who had the experience of sexual abuse. For them, pelvic floor overactivity was noted when watching sexually threatening as well consensual sexual content. Women without sexual abuse history did not have increased pelvic floor activity when watching consensual sexual content.
In summary, evidence supports the hypothesis that women with sexually adverse experiences tend to have impaired genital response when in consensual sexual situations, however, women who do not have sexual abuse histories and but have sexual pain tend to have appropriate genital response. Both groups, however, have increased pelvic floor muscle activity in consensual sexual situations. This increase in pelvic floor muscle activity leads to muscle pain, reduced blood flow, reduced lubrication, increased friction between penis and vulvar skin and hence leads to pain.
This brings us to our next questions, how does the cohort that has had adverse sexual experiences present? How do women with history of sexual trauma process sexual experiences? How does the pelvic floor present or respond to consensual sexual situations when a woman has been abused in the past? Please tune in to the next blog for answers…
Blok BF, Holstege G. The neuronal control of micturition and its relation to the emotional motor system. Prog Brain Res. 1996; 107:113-26
Brauer M, Laan E, ter Kuile MM. Sexual arousal in women with superficial dyspareunia. Arch Sex Behav. 2006; 35:191-200
Brauer M, ter Kuile MM, Janssen S, Lann E. The effect of pain-related fear on sexual arousal in women with superficial dyspareunia. Eur J Pain: 2007; 11:788-98
Spano L, Lamont JA. Dyspareunia: a symptom of female sexual dysfunction. Can Nurse 1975;71:22-5
My name is Tina Allen. I teach a course called Manual Therapy Techniques for the Pelvic Rehab Therapist. I developed this course in 2016 out of desire to help clinicians feel comfortable in their palpation and hands on skills.
 My journey as a pelvic rehab therapist started with a patient whispering to me in the middle of a busy sports/ortho clinic gym; “is it normal to leak when you laugh”. I was treating her after her total hip replacement and my first question was “where are you leaking”? I was concerned that her incision was leaking, that she had an infection and it was beyond me to understand why it would happen when she laughed! I was 24 years old and 2 years out of PT school. Little did I know, that one whispered question would lead me to where I am today. I am in my 25th year as a PT and 20th year specializing in pelvic rehabilitation.
My journey as a pelvic rehab therapist started with a patient whispering to me in the middle of a busy sports/ortho clinic gym; “is it normal to leak when you laugh”. I was treating her after her total hip replacement and my first question was “where are you leaking”? I was concerned that her incision was leaking, that she had an infection and it was beyond me to understand why it would happen when she laughed! I was 24 years old and 2 years out of PT school. Little did I know, that one whispered question would lead me to where I am today. I am in my 25th year as a PT and 20th year specializing in pelvic rehabilitation.
When I started out there just were not many classes. I spent time learning from physicians, reading anything I could find and applying ‘general ‘orthopedic principles to the pelvis. I traveled to clinics and learned from other clinicians. I soaked up anything I could and brought it back to my clinical practice. When Holly Herman and Kathe Wallace asked me to teach with them I was humbled, honored and terribly nervous. Holly and Kathe where two of my greatest resources and to be able to teach along side them to help others along was humbling. As I prepared to teach I realized the breadth of what we do as pelvic rehab clinicians has grown exponentially since I started out.
Over the past 10 years of teaching the pelvic series with H&W; I noticed that for some of the participants there was a gap in confidence in palpation skills and in treatment techniques applied to the pelvic floor region. For most, it’s confidence in what they are feeling and where they are. This course came out of wanting to fill that gap. I wanted to allow a space that clinicians could come and spend two days learning, affirming and building confidence in their hands. They could then take those skills and confidence back to their clinics and help more patients.
The thought of writing this course was daunting. First off, written words are not my thing. Don’t get me wrong I love to read but me coming up with what to put on paper, much less a power point slide, frightened me. With much encouragement and support from colleagues and H&W, I got to work. The first thing was to think about what techniques to include. At some point after 20 years in the field, your hands just do the work and you don’t think about how you do something. My colleague and dear friend Katy Rice allowed me to sit down with her, practice a technique and then write down each specific step to do the skill. She would read them over and then attempt to do the technique by following only the written instructions. I also had patients who were instrumental in helping me choose what techniques to include. They would say to me “that is what made all the difference for me; it has to be included in what you teach others. “
I would think about who taught me each technique, whether it was a course, another clinician or a patient. I know that I did not make any of these up myself; while I may have modified a technique to work with my hands I did not originate them. Holly Tanner was so kind to brain storm with me and lead me to references for some of the techniques that we as clinicians use every day and that I was planning to include.
What happened next was months of me sitting at the kitchen table combing through books, articles, course manuals and online videos looking for origins of the techniques I use every day in my clinical practice. I wanted to be sure to give credit to sources. It was tedious but also inspiring to realize that some of these techniques have been around and documented since 1956 (Dicke, E., & Bischof-Seeberger, I.) and also that the same techniques are sited by multiple different sources. After about 6 months of our kitchen table not being suitable for dinner it was time to see what I had gathered and how it would all fit together. The result was this 2 day course: Manual Therapy Techniques for the Pelvic Rehab Therapist which has seven labs including internal, external and combination techniques, home program/self care ideas and time for brainstorming treatment progressions. Join me in Philadelphia, PA this October 20 - 21 to learn these essential skills.
Nutrition Perspectives for the Pelvic Rehab Therapist
There are moments when I pause and realize how far we’ve come in a short period of time, and then others when I’m acutely reminded how far we have yet to go. Our destination is an integrative health care system which addresses nourishment first and early versus last, not at all, or only when all else fails. My mission is to support the concept of nourishment first and early though sharing of “Nutrition Perspectives for the Pelvic Rehab Therapist” through the Herman & Wallace Pelvic Rehab Institute.
 After each weekend I teach Nutrition Perspectives for the Pelvic Rehab Therapist, I feel affirmed that this class, this information is vital and at times life-changing for practicing clinicians. And every time I teach, participants share that they take away much more than they expected. It’s a course that makes accessible complex concepts to entry level participants while offering timely and cutting edge integrative instruction to the advanced clinician eager to incorporate this knowledge into their practice. Supportive literature is woven throughout the tapestry of the course.
After each weekend I teach Nutrition Perspectives for the Pelvic Rehab Therapist, I feel affirmed that this class, this information is vital and at times life-changing for practicing clinicians. And every time I teach, participants share that they take away much more than they expected. It’s a course that makes accessible complex concepts to entry level participants while offering timely and cutting edge integrative instruction to the advanced clinician eager to incorporate this knowledge into their practice. Supportive literature is woven throughout the tapestry of the course.
After the most recent live course event, a participant shared with me a letter she received from a patient in 2016 who mentions the lack of nutritional attention during her cancer treatment. I want to share with you the essence of this letter:
“In October 2015, I was diagnosed with cancer. The following December I started treatments of radiation and chemotherapy. I really appreciate all the fine employees who helped me through care and treatments. Every clinician I came across, whether a doctor, nurse, phlebotomist, radiation and chemo teams, and my PT, were all exceptional in showing care, concern and knowledge.
However, one area I felt was lacking in was nutrition. I was frequently offered a standard hospital-issue protein drink. When offered, I explained that I would not take it due to it containing high fructose corn syrup (HFCS). I asked if they knew that HFCS was like putting and accelerant on a fire? I received a smile and a nod of head as to say they understood.
I was also offered soda pop to wash down bad tasting medicines/ liquids I was to take. I opted to just down the medication without chasing it as I didn’t want to exacerbate my condition. While taking chemotherapy, I was offered snacks containing HFCS and other non-nutritive so-called foods.
I was also offered limited entree choices, but there were plenty of pies, cakes, jellies, and other non-nutritive foods to choose from. All Items I would not consider for a cancer diet or even a healthy diet. I finally took a picture of the menu selection sheet as I thought no one would believe such a thing could happen.
I received excellent care throughout your system with the exception of nutrition . I would ask that you take a look at making menus with truly healthy options as well as giving patients options that do not contain ingredients that feed the cancer.”
While this letter addresses an inpatient issue at one regional health system, it correspondingly brings into focus the irony present in the vast majority of health care settings across the nation from inpatient to outpatient settings: there is a profound lack of clarity about what it means to be nourished, especially when we are at our most vulnerable.
I cannot claim “Nutrition Perspectives” will solve our nation-wide problem, however, I am certainly encouraging a movement towards a collective understanding of the imperative fact that food is medicine - powerful medicine - and we must as front-line practitioners harness what this understanding can offer. Pelvic rehab practitioners are uniquely positioned to process this information and begin immediately sharing it in clinical practice.
Like many providers, this same participant shared with me that upon receipt of this letter two years ago, she struggled to make progress with what and how to offer nutritional information - mainly because of the overwhelming nature of the subject, and also because of the conflicting and oftentimes confusing information traditionally shared with the public. After attending Nutrition Perspectives, she said “I cannot even begin to describe how much your course has met ALL my hopes for helping clients!….I had struggled to put something together and here it all is - so unbelievably grateful.”
And that’s what this course is all about - empowering you as you broaden your scope of knowledge in a way that teaches you not facts, but deep understanding. Once that foundational understanding is laid, this grass-roots effort will progress like putting an accelerant on the integrative movement. Soon we’ll see the inclusion of nourishment information as first-line practice, and the lives impacted in a positive way will continue to grow.
Please join me at the next opportunity to share in this live experience with other like-minded clinicians. Nutrition Perspectives for the Pelvic Rehab Therapist will be coming to Denver, CO September 15 & 16, 2018!
For many of our patients, chronic pain is a chronic stress. Unfortunately, the resulting ongoing physiological stress reaction can have neurotoxic influences in key brain regions, including the prefrontal cortex, amygdala and hippocampus, and drive maladaptive neuroplastic changes that may further fuel a chronic pain condition.1 For example, chronic stress generates extensive dendritic spine loss in the prefrontal cortex, hyperactivity in the amygdala, and neurogenesis suppression in the hippocampus.2,3,4 In parallel, patients with chronic pain have been shown to exhibit reduced gray matter in the prefrontal cortex, increased neuronal excitability in the amygdala and reduced hippocampal neurogenesis.5,6,7
These three brain areas have been identified to play an important role in fear learning and memory.8 Modulated by stress hormones and stress-induced neuroplastic changes, stress may:
(a) enhance the memory of the initial pain experience at pain onset
(b) promote the later persistence of the pain memory
(c) impair the memory extinction process and the ability to establish a new memory trace.9
 In other words, an ongoing stress reaction, triggered by distressing cognitions and emotions in response to pain or other life circumstances, could reinforce and strengthen the memory of pain. The experience of pain could be generated not by nociceptive activity, but by a well-established memory of pain and inability of the brain to create new associations. Leading researchers in the cortical dynamics of pain at Northwestern University suggest this learning process and persistence of pain memory could be a major influencing mechanism driving chronic pain.9,10
In other words, an ongoing stress reaction, triggered by distressing cognitions and emotions in response to pain or other life circumstances, could reinforce and strengthen the memory of pain. The experience of pain could be generated not by nociceptive activity, but by a well-established memory of pain and inability of the brain to create new associations. Leading researchers in the cortical dynamics of pain at Northwestern University suggest this learning process and persistence of pain memory could be a major influencing mechanism driving chronic pain.9,10
In addition, neurogenesis suppression in the hippocampus is associated with depression, while increased amygdala excitability is associated with anxiety, two mood disorders that frequently accompany and complicate chronic pain conditions.11,12
Why is this important? Appreciating the complex factors that contribute to chronic pain conditions can point to treatment strategies that address these factors.13 For example, strategies that help reduce a patient’s stress reaction, mitigate the experience of fear and anxiety, and/or promote relaxation, positive mood and self-efficacy could conceivably reduce the stress reaction and reverse maladaptive neuroplasticity. While chronic pain is a multifaceted and highly complex condition with no simple answers or one-size-fits-all successful treatment strategy, initial research suggests promise for this approach to modulate cortical structure. In a study of cognitive-behavioral therapy (CBT) in the treatment of chronic pain, an 11-week CBT treatment course increased gray matter in the prefrontal cortex and hippocampus.14
In addition, a systematic review of brain changes in adults who participated in Mindfulness-Based Stress Reduction identified increased activity, connectivity and volume in the prefrontal cortex and hippocampus in stressed, anxious and healthy adults.15 Also, the amygdala demonstrated decreased activity and improved functional connectivity with the prefrontal cortex. Although yet to be studied in patients with chronic pain, these neuroplastic changes could potentially promote improved cortical dynamics in our patients.
I am excited to share this model of chronic stress and chronic pain and evidence-based applications of mindfulness to pain treatment in my upcoming course Mindfulness-Based Pain Treatment in Arlington, VA August 4 and 5, 2018 and in Seattle, WA November 3 and 4, 2018. Course participants will learn about mindfulness and pain research, practice mindful breathing, body scan and movement and expand their pain treatment tool box with practical strategies to improve pain treatment outcomes. Research examining the application of mindfulness in the treatment of patients at risk of opioid misuse will be included. I hope you will join me!
Vachon-Presseau E. Effects of stress on the corticolimbic system: implications for chronic pain. Prog Neuropsychopharmacol Biol Psychiatry. 2017; Oct 25. pii: S0278-5846(17)30598-5.
Arnsten AF. Stress signaling pathways that impair prefrontal cortex structure and function. Nat Rev Neurosci 2009:10(6):410-422.
Zhang X, Tong G, Guanghao Y, et al. Stress-induced functional alterations in amygdala: implications for neuropsychiatric diseases. Front Neurosci. 2018 May 29;12:367.
Kim EJ, Pellman B, Kim JJ. Stress effects on the hippocampus: a critical review. Learn Mem. 2015;22(9):411-6.
Fritz HC, McAuley JH, Whittfeld K, et al. Chronic back pain is associated with decreased prefrontal and anterior insular gray matter: results from a population-based cohort study. J Pain. 2016;17(1):111-8.
Veinante P, Yalcin I, Barrot M. The amygdala between sensation and affect: a role in pain. J Mol Psychiatry. 2013;1(1):9.
Vachon-Presseau E. Roy M, Martel MO, et al. The stress model of chronic pain: evidence from basal cortisol and hippocampal structure and function. Brain. 2013;136(Pt 3):815-27.
Greco JA, Liberzon I. Neuroimaging of fear-associated learning. Neuropsychopharmacology. 2016;41(1):320-334.
Mansour AR, Farmer MA, Baliki. Chronic pain: role of learning and brain plasticity. Restor Neurol Neurosci. 2014;32(1):129.
Baliki MN, Apkarian AV. Nociception, pain, negative moods and behavior. Neuron. 2015;87(3):474-491.
Schmaal L, Veltman DJ, van Erp TG, et al. Subcortical brain alterations in major depressive disorder: findings from ENIGMA major depressive disorder working group. Mol Psychiatry. 2016;21(6):806-12.
Shin LM, Liberzon I. The neurocircuitry of fear, stress and anxiety disorders. Neuropsychopharmacology. 2010;35(1):169-91.
Greenwald J, Shafritz KM. An integrative neuroscience framework for the treatment of chronic pain: from cellular alterations to behavior. Front Int Neurosci. 2018 May 23;12:18.
Seminowicz DA, Shpaner M, Keaser ML, et al. Cognitive-behavioral therapy increases prefrontal cortex gray matter in patients with chronic pain. J Pain. 2013;14(2):1573-84.
Gotink RA, Meijboom R, Vernooij, et al. 8-week Mindfulness Based Stress Reduction induces brain changes similar to traditional long-term meditation practice – A systematic review. Brain Cogn. 2016;108:32-41.
The British author, John Donne, wrote, “No man is an island, entire of itself; every man is a piece of the continent.” In a similar idea, no neurological symptom is independent and isolated; every system has potential to impact the whole body. Neurogenic bladder should cue a clinician to check for neurogenic bowel and to assess the pelvic floor in order to get a complete map of what to address in treatment.
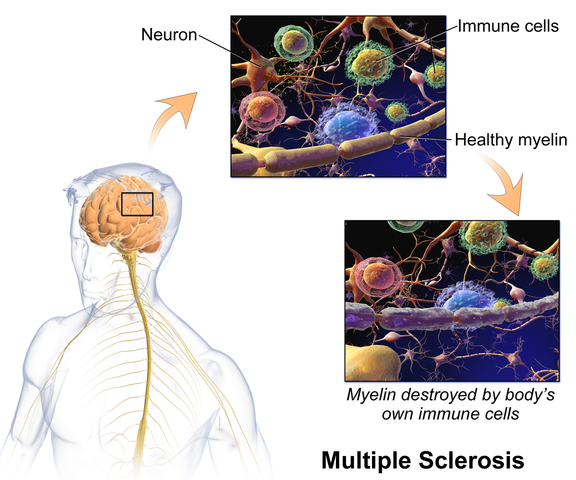 Martinez, Neshatian, & Khavari (2016) reviewed literature on neurogenic bowel dysfunction (NBD) and neurogenic bladder in patients with neurological conditions such as multiple sclerosis (MS). Constipation and fecal incontinence can coexist with NBD, and a multifactorial bowel regimen is vital to conservative management in patients with neurological disorders. Nonpharmacological, pharmacological, and surgical approaches were reviewed in the article. Specific results for MS were reported only for transanal irrigation (TAI) and biofeedback. In TAI, fluid is used to stimulate the bowel and clean out stool from the rectum. A study showed 53% of the 30 patients with MS demonstrated a 50% or better improvement in bowel symptoms with TAI. In anorectal biofeedback, operant conditioning retrains motor and sensory responses via exercises guided by manometry. With biofeedback, a study showed 38% of patients had a beneficial impact with the intervention. The list of treatment approaches not specifically researched for MS patients in this review includes: dietary modifications, perianal/anorectal stimulation, abdominal massage, suppositories, oral medications such as stool softeners or prokinetic agents, sacral neuromodulation, antegrade continence enema, and colostomy.
Martinez, Neshatian, & Khavari (2016) reviewed literature on neurogenic bowel dysfunction (NBD) and neurogenic bladder in patients with neurological conditions such as multiple sclerosis (MS). Constipation and fecal incontinence can coexist with NBD, and a multifactorial bowel regimen is vital to conservative management in patients with neurological disorders. Nonpharmacological, pharmacological, and surgical approaches were reviewed in the article. Specific results for MS were reported only for transanal irrigation (TAI) and biofeedback. In TAI, fluid is used to stimulate the bowel and clean out stool from the rectum. A study showed 53% of the 30 patients with MS demonstrated a 50% or better improvement in bowel symptoms with TAI. In anorectal biofeedback, operant conditioning retrains motor and sensory responses via exercises guided by manometry. With biofeedback, a study showed 38% of patients had a beneficial impact with the intervention. The list of treatment approaches not specifically researched for MS patients in this review includes: dietary modifications, perianal/anorectal stimulation, abdominal massage, suppositories, oral medications such as stool softeners or prokinetic agents, sacral neuromodulation, antegrade continence enema, and colostomy.
Miletta, Bogliatto, & Bacchio (2017) presented a case study about management of sexual dysfunction, perineal pain, and elimination dysfunction in a 40 year old female with multiple sclerosis. She had been experiencing perineal pain for 5 months and had chronic MS symptoms of lower anourogenital dysfunction, including bladder retention and obstructed defecation syndrome. Physical therapy treatment included pelvic floor muscle training (primarily decreasing overactivity of pelvic muscles in this case), perineal massage, biofeedback, postural correction, global relaxation techniques, and a home self-training program. After 5 months of physical therapy, the woman had improved pelvic floor muscle contraction strength, resolution of pelvic floor muscle overactivity, increased sexual satisfaction (according to the Female Sexual Function Index score), a visual analog scale improvement of vulvar and perineal pain by 4 points, normalization of obstructed defecation syndrome, and decreased bladder retention symptoms. The authors concluded the variety of symptoms in MS require a multimodal approach for treatment, considering all the motor, autonomic, and cognitive impairments as well as side effects of medications that try to improve those symptoms. The quality of life of women with MS has potential to be improved significantly if pelvic floor disorders related to MS are addressed appropriately.
Ultimately, treating urinary dysfunction but avoiding bowel dysfunction does neurological patients a disservice. Systems are intertwined in a series of cause and effects throughout the body. The “Neurologic Conditions and the Pelvic Floor” course can expand your knowledge and understanding of how the symptoms of conditions such as multiple sclerosis can impact pelvic health and how we can better address the whole patient for optimal outcomes.
Martinez, L., Neshatian, L., & Khavari, R. (2016). Neurogenic Bowel Dysfunction in Patients with Neurogenic Bladder. Current Bladder Dysfunction Reports, 11(4), 334–340. http://doi.org/10.1007/s11884-016-0390-3
Miletta, M., Bogliatto, F., & Bacchio, L. (2017). Multidisciplinary Management of Sexual Dysfunction, Perineal Pain, and Elimination Dysfunction in a Woman with Multiple Sclerosis. International Journal of MS Care, 19(1), 25–28. http://doi.org/10.7224/1537-2073.2015-082
This post is part two of Nari Clemon's series on practitioner burnout, compassion fatigue, and the story of a pelvic rehab therapist who struggled to care for herself while caring for patients. Read part one here.
There is a point where caring so much and wanting to help becomes counter-productive to us, until we burn out. We can develop true compassion fatigue. Compassion fatigue makes us feel apathetic, spent, and sometimes even jaded or cranky. But, how do we turn that caring off in time? Our compassion is what led us to this field in the first place.
 That day, I talked to my colleague and close friend, whom I was teaching with, Jen VandeVegte. Jen and I both felt that conversation was a wake-up call. We talked about seeing this same scenario at our courses: so many amazing therapists getting spent, and our best therapists getting burnt out. People were coming back with enhanced skills course after course, but many of them were looking weary and tired...
That day, I talked to my colleague and close friend, whom I was teaching with, Jen VandeVegte. Jen and I both felt that conversation was a wake-up call. We talked about seeing this same scenario at our courses: so many amazing therapists getting spent, and our best therapists getting burnt out. People were coming back with enhanced skills course after course, but many of them were looking weary and tired...
In the prior years, Jen and I were both trying to be mindful and intentional. But, it hadn’t been enough in our own lives. I remember thinking, “I’m mindful I’m getting drained and there is a creeping sensation of fatigue as I am working with this patient. Now what?” There seemed to be some pitfalls many of us were getting trapped in. We noticed there were certain patients who drained us more: when the role was therapist as hero and patient as victim. There were themes of not being able to leave the patient stories at work, finding ourselves laughing less, being less adventurous. There also seemed to be a link with empathy. Those of us who were more empathic carried burdens differently than our more concrete minded peers.
For myself, I had to hit bottom to learn how to climb back out. It got to the point where I didn’t honestly want to go to my thriving private practice and treat patients. I was treating more and more complex patients and leaving work drained, despite having a repertoire of advanced skills. I remember consulting with many people trying to understand how to stop this process of my patients’ illnesses and moods bleeding into my space and my body. People told me all kinds of things: “Imagine wearing gloves that are impenetrable”, “Picture a plexiglass box around yourself”, or “Just decide it is a one way flow.” None if it worked for me. I studied Reiki and worked with therapists. Still, I was so spent after treating patients. When I moved from Indiana to Portland, I took a whole year off of work with a singular mission: get healthy and figure out how to stay that way in my work. There was no book on this. There were some crazy stories and consults that made me realize I was heading in the wrong direction, and I finally learned the key concepts that changed my life.
And oddly enough, my great friend, Jen, also had to transform. We talked honestly and shared our failures, fears and successes as we learned. We committed to being real and honest about what parts of us were stuck in old, unhelpful paradigms. Some of these were playing the hero, feeling like there should not be limits on our compassion, not holding boundaries with what was ours to own, facing difficult things within ourselves, learning how to deeply own the space in our own bodies, and accepting that as intuitive, empathic women, we can’t expect ourselves to reproduce a very masculine, directive method of treating that denies so much of who we actually are. We also changed how we dialogued with patients from the outset. We read and researched and learned how to apply a shared responsibility model from the first contact with our patients and how to hold that model during the course of care. We then applied more pain theory and how to educate patients on those aspects of their own recovery to encourage a model of mind-body wellness and responsibility for their own reframing with our guidance. I created a mediation for pelvic health CD, so patients had a clear way to practice these home programs.
Jen and I both found that as we healed and re-framed there was a great freedom and honesty that emerged in our lives and our practices. We would get together to teach Capstone and were filled with gratitude for how much had shifted and that work no longer felt like a burden. Our lives were more balanced and we were physically, mentally and emotionally stronger. We felt like we had found the holy grail of balanced practices.
But, there we stood, teaching so many of our peers who were clearly in the same quicksand that had been plaguing us in the past. Where could our colleagues who were at our series courses go to learn how to do this job and navigate their days differently? How could they feel as good at the end of the day as they did before they saw patients? This was the training many pelvic therapists needed to thrive in this field AND their life, but it had taken us so many years. This was our call to action.
We all take courses on how to help our patients and how to reach those few difficult patients and help them. Yet, as medical professionals, we do not have enough training in how to care for ourselves. At some point, we all need to realize that our care is as important as our patients. Our wellness, physical, mental, and emotional also matter and may actually be necessary to keep helping patients. Enjoying our lives is no less important. It is an investment in your family, your future patients, and yourself to take a few days to peel back and deeply examine the root of why work is so taxing and come up with a clear, individualized plan to take your life, joy and passion back…without leaving pelvic rehab.
We need all of you in this field. We want to help you stay in this field and stay in it well! Please come join us in Boundaries, Self-Care and Meditation for a retreat-like weekend to change the framework of your practice and commit to your own wellness as a provider. Come learn how to shift dynamics from your first interaction with patients and how to hold that space. You are worth it!
Tamara Rial, PhD, CSPS, co-founder and developer of Low Pressure Fitness will be presenting the first edition of “Low Pressure Fitness and abdominal massage for pelvic care” in Princeton, New Jersey in July, 2018. Tamara is internationally recognized for her work with hypopressive exercise and Low Pressure Fitness. In this article she presents the novel topic of hypopressives as a complementary pelvic floor muscle training tool for incontinence after prostate cancer surgery.
Urinary Incontinence is the most common side effect men suffer after prostate cancer surgery along with erectile dysfunction. Although it is not life threatening, urinary incontinence definitely has a negative impact on the patient’s quality of life Sountoulides et al., 2013. Beyond the frustration and embarrassment associated with pelvic floor dysfunction, many patients describe it as depressing, disheartening and devastating.
The first line of conservative treatment - and most often recommended - is pelvic floor muscle training Andersen et al., 2015. Over the past few years, some researchers have also recommended alternative exercise programs with a holistic approach such as Pilates and hypopressives to improve the patient’s quality of life and urinary incontinence symptoms (Santa Mina et al., 2015). These alternative pelvic floor muscle training programs draw upon the connection between the pelvic floor, it’s synergistic muscles (abdominal, pelvic, lumbar) and their interrelated role in posture and breathing Hodges, 2007; Sapsford, 2004; Madill and McLean, 2008; Talasz et al., 2010. Among these complementary exercise programs, hypopressives have gained increasing attention for the recovery of post-prostatectomy urinary incontinence Santa Mina et al., 2015; Mallol-Badellino, et al. 2015.
What is known about hypopressives for post-prostatectomy incontinence?
Although hypopressive exercise has become popular for women, some researchers, clinicians and practitioners have begun to apply these exercises for specific male issues such as urinary incontinence following a prostatectomy. Recently, a case-study I co-authored about an adapted program of hypopressive exercise for urinary incontinence following a radical prostatectomy surgery was published in the Journal of the Spanish physiotherapy association Chulvi-Medrano & Rial, 2018. We describe the case of a 46-year-old male with severe stress urinary incontinence six months after surgery. We used a pelvic floor exercise program consisting of hypopressive exercises as described in the Low Pressure Fitness level 1 practical manual Rial & Pinsach, 2017 combined with contraction of the pelvic floor muscles. Satisfactory results were obtained after the rehabilitation protocol as evidenced by a reduction from 3 daily pads to none. Of note, clinical trails have demonstrated the benefits of initiating a rehabilitation program to strengthen the pelvic floor as soon as possible after prostatectomy. Previously, I’ve studied hypopressive exercise for female urinary incontinence Rial et al., 2015 and for the improvement of female athletes pelvic floor function Álvarez et al., 2016. However, this was the first time we’ve studied hypopressives in the context of male urinary leakage.
In the same light, other researchers have also included hypopressives in their pelvic floor training protocol for post-prostatectomy urinary incontinence. For example, Serda et al (2010) and Mallol-Badellino (2015) used protocols that combined pelvic floor contractions with postural re-education and hypopressives. Both studies found improvements in the severity of involuntary leakages and improvements in the patients’ quality of life. Similar results are also described in the clinical case by Scarpelini et al. (2014) who used hypopressives and psoas stretching exercises to reduce urinary incontinence after prostatectomy.
But how do hypopressives work?
The hypothesis underlying the use of hypopressives as a complementary pelvic floor and core exercise program is that it retrains the core system with specific postural and breathing strategies while reducing pressure on the pelvic organs and structures. The most striking part of hypopressives breathing technique is the abdominal vacuum. This breathing maneuver involves a low pulmonary volume exhale-hold technique followed by a rib-cage expansion involving the activation of the inspiratory muscles. The rib-cage expansion during the breath-holding phase leads to a noticeable draw-in of the abdominal wall and simultaneously to the rise of the thoracic diaphragm. Recent observational studies have shown how the hypopressive technique was able to elevate the pelvic viscera and to activate the pelvic floor and deep core muscles in women trained with hypopressives Navarro et al., 2017. From an historical point of view, this characteristic breathing maneuver was first described and practiced as a yoga pranayama called Uddiyanha Bandha Omkar & Vishwas, 2009.
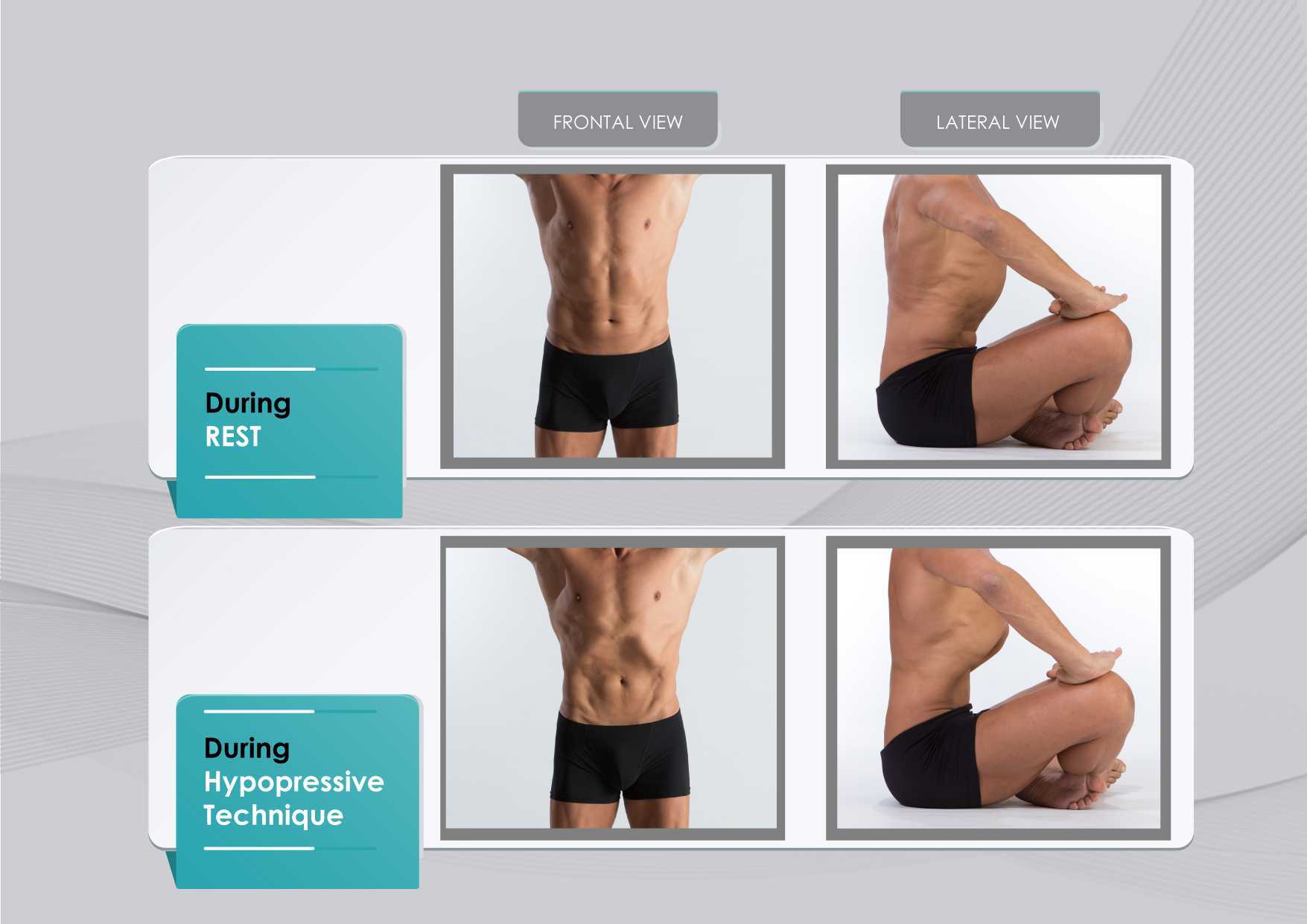
Figure 1 shows the anatomical behavior of the rib cage and the abdominal wall when performing the hypopressive breathing maneuver, which should not be confused with an abdominal hollowing, or a bracing maneuver. Anatomical observation of the thoracic and abdominal behavior during the breathing maneuver of the hypopressive exercise. Figure elaborated by the author.
In addition to breath control, the hypopressive technique involves a series of static and dynamic poses which operate on the hypothesis of training the stabilizing muscles of the spine, such as the core and pelvic muscles. In this sense, hypopressives are not exclusively a breathing technique, but rather they are an integrated whole-body technique. The practice of hypopressives involves body control, body awareness, postural correction and mindfulness throughout its different poses and postural techniques. The introduction of holistic exercise programs to train the synergist pelvic floor muscles and breathing patterns can be viewed as complementary tools for the restoration of a patient’s body awareness and functionality.
Another hypothesis of the effects of the hypopressive-breathing in the pelvic floor is the ability to move the pelvic viscera cranially as a consequence of the ribcage opening up after the breath-hold. This vacuum lifts the diaphragm and consequently creates an upward tension on the transversalis fascia, the peritoneum and other related fascial structures. In addition to the diaphragmatic suction effect, a correct alignment of the rib cage and pelvis during the exercise contributes to an improved suspension and position of the viscera in the pelvis. The mobility achieved with the breathing and its body sensations may be one of the reasons why hypopressives have also been recommended as a proprioceptive facilitator for those with low ability to “find their pelvic floor” Latorre et al., 2011.
It’s crucial to highlight that a complete surgical resection of the prostate will cause - in most of the cases - post-operative fibrosis and neurovascular damage Hoy-Land et al., 2014. Both, the neurovascular and musculoskeletal injuries are contributing factors for urinary incontinence post-prostatectomy. Subsequently, exercises focusing on increasing local vascular irrigation and re-activating the damaged musculature have been highlighted as the main goals to help patients recover continence. In this sense, breathing movements, fascia manipulation and decreased pelvic pressure can result in increased vascular supply. A previous study has shown an improvement in venous return of the femoral artery during the hypopressive-breathing maneuver Thyl et al., 2009. Collectively, all these factors may favor microcirculation in the pelvic area. Finally, the muscle activation of the pelvic floor and core muscles observed during the practice of hypopressives (Ithamar et al., 2017) and the changes of puborectalis and iliococcygeus muscles after an intensive pelvic floor muscle training (Dierick et al., 2018) are other factors that could have impact on urge incontinence, stress incontinence and overflow incontinence symptoms common after prostatectomy surgeries.
To date, the results from these investigations and clinical reports open new complementary pelvic floor training strategies for the treatment of post-prostatectomy incontinence. Hypopressives and pelvic floor muscle exercises are non-invasive, don’t require expensive material, and provide an exercise-based approach as part of a healthy lifestyle. However, qualified instruction, technique-driven progression and adherence to the intervention are critical components of any pelvic floor and hypopressive training protocol.
Álvarez M, Rial T, Chulvi-Medrano I, García-Soidán JL, Cortell JM. 2016. Can an eight-week program based on the hypopressive technique produce changes in pelvic floor function and body composition in female rugby players? Retos nuevas Tendencias en Educación Física, Deporte y Recreación, 30(2): 26-29.
Anderson CA, Omar MI, Campbell SE, Hunter KF, Cody JD, Glazener CM. 2015. Conservative management for postprostatectomy urinary incontinence. Cochrane Database Syst Rev, 1:CD001843.
Chulvi-Medrano I, Rial T. 2018. A case study of hypopressive exercise adapted for urinary incontinence following radical prostactetomy surgery. Fisioterapia, 40, 101-4. Doi: DOI: 10.1016/j.ft.2018.01.004
Dierick F, Galrsova E, Laura C, Buisseret F, Bouché FB, Martin L. 2018. Clinical and MRI changes of puborectalis and iliococcygeus after a short period of intensive pelvic floor muscles training with or without instrumentation. European Journal of Applied Physiology, doi:10.1007/s00421-018-3899-7
Ithamar, L., de Moura Filho, A.G., Benedetti-Rodrigues, M.A., Duque-Cortez, K.C., Machado, V.G., de Paiva-Lima, C.R.O., et al. 2017. Abdominal and pelvic floor electromyographic analysis during abdominal hypopressive gymnastics. J. Bodywork. Mov. Ther. doi: 10.1016/j.jbmt.2017.06.011.
Latorre G, Seleme M, Resende AP, Stüpp L, Berghmans B. Hypopressive gymnastics: evidences for an alternative training for women with local proprioceptive deficit of the pelvic floor muscles. Fisioterapia Brasil 2011; 12(6): 463-6.
Hodges P. 2007. Postural and respiratory functions of the pelvic floor muscles. Neurourol Urodyn, 26(3): 362-371.
Hoyland K, Vasdev N, Abrof A, Boustead G. 2014. Post-radical prostatectomy incontinence: etiology and prevention. Rev Urol. 16(4), 181-8.
Madill, S., McLean, L. 2008. Quantification of abdominal and pelvic floor muscle synergies in response to voluntary pelvic floor muscle ontractions. J. Electromyogr. Kinesiol. 18, 955-64. doi: 10.1016/j.jelekin.2007.05.001.
Mallol-Badellino J., et al. 2015. Resultados en la calidad de vida y la severidad de la incontinencia urinaria en varones prostatectomizados por neoplasia de próstata. Rehabilitación, 49(4); 210-215.
Navarro, B., Torres, M., Arranz, B. Sánchez, O. 2017. Muscle response during a hypopressive exercise after pelvic floor physiotherapy: Assessment with transabdominal ultrasound. Fisioterapia. 39, 187-194. doi:10.1016/j.ft.2017.04.003.
Omkar, S., Vishwas, B. 2009. Yoga techniques as a means of core stability training. J. Bodywork Mov. Thep. 13, 98-103. doi: 10.1016/j.jbmt.2007.10.004.
Rial T, Chulvi-Medrano I, Cortell-Tormo JM, Álvarez M. 2015. Can an exercise program based on hypopressive technique improve the impact of urinary incontinence on women´s quality of life? Suelo Pélvico, 11:27-32.
Rial, T., Pinsach, P. 2017. Low Pressure Fitness practical manual level 1. International Hypopressive and Physical Therapy Institute, Vigo.
Santa Mina D, Au D, Alibhai S, Jamnicky L, Faghani N, Hilton W, Stefanky L, et al. 2015. A pilot randomized trial of conventional versus advanced pelvic floor exercises on treat urinary incontinence after radical prostatectomy: a study protocol. BMC Urology, 15. DOI 10.1186/s12894-015-0088-4
Sapsford R. 2004. Rehabilitation of pelvic floor muscles utilizing trunk stabilization. Man Ther, 9(1): 3-12.
Serdá B, Vesa, A. del Valle, y Monreal P. 2010. La incontinencia urinaria en el cáncer de próstata: diseño de un programa de rehabilitación. Actas Urológicas Españolas, 34(6): 522-30.
Scarpelini P, Andressa Oliveira F, Gabriela Cabrinha S, Cinira H. 2014. Protocolo de ginástica hipopressiva no tratamento da incontinência urinária pós-prostatectomia: relato de caso. UNILUS Ensino e Pesquisa, 11(23): 90-95
Talasz, H., Kofler, M., Kalchschmid, E., Pretterklieber, M., Lechleitner, M. 2010. Breathing with the pelvic floor? Correlation of pelvic floor muscle function and expiratory flows in healthy young nulliparous women. Int. Urogynecol. J. 21, 475-81. doi: 10.1007/s00192-009-1060-1.
Thyl S., Aude P, Caufriez M, Balestra C. 2009. Incidence de l'aspiration diaphragmatique associée à une apnée expiratoire sur la circulation de retour veineuse fémorale: étude par échographie-doppler. Kinésithérapie scientifique, 502; 27-30.
Exciting news! Carolyn McManus, Herman & Wallace instructor of Mindfulness-Based Pain Treatment, will be a presenter in programming at the International Association for the Study of Pain (IASP) World Congress on Pain in to be held in Boston, September 11 - 16. This conference brings together experts from around the globe practicing in multiple disciplines to share new developments in pain research, treatment and education. Participants from over 130 countries are expected to attend. The last time it was held in the U.S. was 2002, so it presents an especially exciting opportunity for those interested in pain to have this international program taking place in the U.S. Carolyn will present a workshop on mindfulness in a Satellite Symposia, Pain, Mind and Movement: Applying Science to the Clinic.
 Carolyn has been a leader in bringing mindfulness into healthcare throughout her over-30 year career. She recognized early on in her practice how stress amplified patients’ symptoms and, as she had seen the benefits of mindfulness in her own life, it was a natural progression to integrate mindful principles and practices into her patient care. An instructor for Herman and Wallace since 2014, she has developed two popular courses, Mindfulness-Based Pain Treatment and Mindfulness for Rehabilitation Professionals, enabling her to share her clinical and research experiences with her colleagues.
Carolyn has been a leader in bringing mindfulness into healthcare throughout her over-30 year career. She recognized early on in her practice how stress amplified patients’ symptoms and, as she had seen the benefits of mindfulness in her own life, it was a natural progression to integrate mindful principles and practices into her patient care. An instructor for Herman and Wallace since 2014, she has developed two popular courses, Mindfulness-Based Pain Treatment and Mindfulness for Rehabilitation Professionals, enabling her to share her clinical and research experiences with her colleagues.
For many patients, pain is not linearly related to tissue damage and interventions based on structural impairment alone are inadequate to provide full symptom relief. Mindfulness training can offer a key ingredient necessary for a patient to make additional progress in treatment. By learning therapeutic strategies to build body awareness and calm an over-active sympathetic nervous system, patients can mitigate or prevent stress-induced symptom escalation. They can learn to move with trust and confidence rather than fear and hesitation.
A growing body of research in mindfulness-based therapies demonstrates multiples benefits for patients suffering with pain conditions. Research suggests that mindfulness training can be helpful to women preparing for childbirth and patients suffering from fibromyalgia, pelvic pain, IBS and low back pain. In addition, for patients with anxiety, mindfulness training may contribute to reductions in anxiety and in adrenocorticopropic hormone and proinflammatory cytokine release in response to stress. Authors of this study conclude that these large reductions in stress biomarkers provide evidence that mindfulness training may enhance resilience to stress in patients with anxiety disorders.
In addition to her presentation at the IASP World Congress Satellite Symposia, Carolyn will be sharing a more in-depth examination and practice of mindfulness in her upcoming course Mindfulness-Based Pain Treatment, August 4 and 5 at Virginia Hospital Center, Arlington VA, and again November 3 and 4 at Pacific Medical Center in Seattle, WA. Please join an internationally-recognized expert for 2 days of innovative training in mindfulness that will both improve your patient outcomes and enhance your own well-being!
Duncan LG, Cohn MA, Chao MT, et al. Benefits of preparing for childbirth with mindfulness training: A randomized controlled trial. BMC Pregnancy Childbirth 2017 May 12;17(1):140.
Fox SD, Flynn E, Allen RH. Mindfulness meditation for women with chronic pelvic pain: a pilot study. J Reprod Med.2011;56(3-4):158-62.
Garland EL, Gaylord SA, Paisson O. Therapeutic mechanisms of a mindfulness-based treatment for IBS: effects on visceral sensitivity, catastrophizing and affective processing of pain sensations. J Behav Med. 2012;35(6):591-602.
Cherkin DC, Sherman KJ, Balderson BH, et al. Effect of mindfulness-based stress reduction vs cognitive behavioral therapy or usual care on back pain and functional limitations in adults with chronic low back pain: a randomized Clinical Trial. JAMA. 2016;315(12):1240-9.
Hoge EA, Bui E, Palitz SA, et al. The effect of mindfulness meditation training on biological acute stress responses in generalized anxiety disorder. Psychiatry Res. 2018;262:328-332.
By accepting you will be accessing a service provided by a third-party external to https://hermanwallace.com/








































