The following is our interview with Jose Antonio (Tony) Rodriguez Jr, COTA. Tony practices in Laredo, TX where he is also studying Athletic Training at the Texas A & M University. He recently attended Pelvic Floor Level 1 and plans to continue pursuing pelvic rehabilitation with Herman & Wallace. He was kind enoguh to share some thoughts about his experiences with us. Thank you, Tony!
Tell us a bit about yourself!
I am a COTA in Laredo where I was born and raised. My goal is to provide pelvic floor therapy to my community. I have been in school for quite some time. I have associate's degrees as a paramedic and occupational therapy assistant. I studied nursing briefly (finished my junior year). My bachelors is in psychology. I’m currently studying athletic training in Texas A & M International University in Laredo. My ultimate academic goal is acquiring my doctorate in physical therapy.



This post was written by the teaching team of Nancy Cullinane, PT, MSH, Kathy Golic, PT, and Terri Lannigan DPT, who took their talents to Nairobi, Kenya to teach a modified version of Herman & Wallace's Pelvic Floor Level 1 course.
At the end of week 1 of Kenyan Pelvic Floor Level 1, we are pleased to report that 35 physiotherapists are embracing pelvic health physical therapy. Our students are primarily from the Nairobi area, however a handful have traveled from rural areas. The majority of them have some aspect of women's health in their job duties, however, only two have previously performed internal pelvic floor muscle techniques. On the first day of class, we spent significant introductory time discussing course objectives, students' clinical experience, Kenyan healthcare delivery, and what they hoped to gain from us. One student described teaching herself skills she is using in her clinical practice from watching YouTube videos. Another student commented, "the only tool I have to treat my patients is the kegel exercise and it isn't working for many of my patients. I know I'm missing something and I hope to find it here." The concept of internal pelvic floor muscle evaluation and treatment is new in Kenya and this is the first presentation of this coursework. There was significant anxiety surrounding internal pelvic muscle examination lab in the course. Several participants were not aware what "internal examination" meant in the course description when they registered. One student did not return on day two because of it. Nonetheless, as soon as the first internal assessment lab was completed, the pace picked up considerably.
These pioneering physiotherapists have developed new skills this past week for treating overactive bladder, mixed urinary incontinence, overactive pelvic floor muscles, prolapse, and diastasis recti. We have delved into discussion regarding sexual trauma and how cultural differences here in Kenya will impact the students' potential strategies in initiating conversations with their patients. Nine of our students are employed at Kenyatta National Hospital, the largest public hospital in Nairobi. Several are employed in private hospitals, who serve those citizens who pay to receive care in their respective systems. Many of our students are under-employed and some see patients privately in their homes, often for cash.
Andrea Wood, PT, DPT, WCS, PRPC is a pelvic health specialist at the University of Miami downtown location. She is a board certified women’s health clinical specialist (WCS) and a certified pelvic rehabilitation practitioner (PRPC). She is passionate about orthopedics and pelvic health. In her spare time, you can find her enjoying the south Florida outdoors.
Inflammatory bowel disease (IBD) includes the two diagnosis of Crohn’s Disease and Ulcerative Colitis. While both can cause similar health effects, the differences of the disease pathologies are listed below:1
| Ulcerative Colitis | Crohn’s Disease | |
| Affected Area |
|
|
| Pattern of Damage |
|
|
Common complications experienced by patients with IBD include fecal incontinence, fecal urgency, night time soiling, urinary incontinence, abdominal pain, hip and core weakness, pelvic pain, fatigue, osteoporosis, and sarcopenia. In a sample of 1,092 patients with Crohn’s Disease, Ulcerative Colitis, or unclassified IBD, 57% reported fecal incontinence. Fecal incontinence was reported not only during periods of flare ups, but also during remission periods.2 One common factor affecting fecal incontinence is external anal sphincter fatigue. External anal sphincter fatigue has also been shown to be present in IBD patients who are not experiencing fecal incontinence or fecal urgency. IBD patients have been shown in studies to have similar baseline pressures versus healthy matched controls, thus indicating the possibility that deficits in endurance versus strength can play a larger role in fecal incontinence.3 Other factors contributing to fecal incontinence include post inflammatory changes that may alter anorectal sensitivity, anorectal compliance, neuromuscular coordination, and cause visceral hypersensitivity. Visceral hypersensitivity may be caused by continuous release of inflammatory mediators found in patients with IBD. It is also important to screen properly for incomplete bowel emptying and stool consistency to rule out overflow diarrhea or fecal impaction. Reports of need to splint digitally for full evacuation may indicate incomplete bowel emptying and defaectory disorders such as paradoxical contraction of the puborectalis muscle or rectocele. Anorectal manometry testing may be highly useful in identifying patients likely to improve from biofeedback therapy.4
Today's guest post comes from Kelsea Cannon, PT, DPT, a pelvic health practitioner in Seattle, WA. Kelsea graduated from Des Moines University in 2010 and practices at Elizabeth Rogers Pilates and Physical Therapy.
Many studies done on pelvic floor muscle training largely have subjects who are Caucasian, moderately well educated, and receive one-on-one individualized care with consistent interventions. This led a group of researchers to investigate the occurrence of pelvic floor dysfunction, specifically pelvic organ prolapse (POP), in parous Nepali women. These women are known to have high incidences of POP and associated symptomology. Another impetus to perform this research: the discovery that there was a major lack of proper pelvic floor education for postpartum women. These women were commonly encouraged to engage their pelvic floor muscles via performing supine double leg lifts, sucking in their tummies/holding their breath/counting to ten, and squeezing their glutes. These exercises would be on a list of no-no’s here in the United States. In 2017, Delena Caagbay and her team of researchers discovered that in Nepal, no one really knew the correct way to teach proper pelvic floor muscle contractions, preventing the opportunity for women to better understand their pelvic floors. The team then set out to investigate the needs of this population, with the eventual goal of providing effective pelvic floor education for Nepali women.
Caagbay and her team first wanted to know what baseline muscle activity the Nepali women had in their pelvic girdle. Physical examinations and internal pelvic floor muscle strength assessments revealed that surprisingly there was a low prevalence of pelvic floor muscle defects, such as levator avulsions and anal sphincter trauma. Uterine prolapses were most common while rectoceles were comparatively less common. Their muscles were also strong and well-functioning, often averaging a 3/5 on the Modified Oxford Scale. It was hypothesized that these women had low prevalence of muscle injury because instruments were not commonly used during childbirth, they had lower birth weight babies, and the women were typically younger when giving birth (closer to 20-21 years old). But they had a high prevalence of POP even with good muscle tone? Researchers suggested that their incidence of POP is likely stemming from their sociocultural lifestyle requirements, as women are left to do most of the daily household chores and caregiving tasks while men often travelled away from the home to perform paid labor. Physical responsibilities for these women commonly begin at younger ages and while it helps promote good muscle tone, the heavier loading places pressure on the connective tissue and fascia that support the pelvic organs. Because of the demands of their lifestyles, Nepali women are often forced to return to their physically active state within a couple weeks after giving birth.
Going to the Combined Sections Meeting of the American Physical Therapy Association (CSM2019)? Look for Herman & Wallace instructor Carolyn McManus, MPT, MA at the educational session titled “Pain Talks: Conversations with Pain Science Leaders on the Future of the Field”. Carolyn will be a panelist along with Kathleen Sluka, PT, PhD, Steve George, PT, PhD, Carol Courtney, PT, PhD and Adriaan Louw, PT, PhD. The panel will be moderated by Derrick Sueki, DPT, PhD and Mark Shepherd, DPT, OCS.
These influential leaders will share how they personally became interested in the field of pain and discuss innovative pain treatment, as well as leading edge pain research and its translation into clinical practice. Initiatives to standardize entry-level curriculum, develop pathways to pain specialization and create post-professional opportunities such as pain-specific residencies and fellowships will be explored. The session will conclude with the leaders discussing their views on the future of pain and the role of physical therapy in its management. The audience will be able to submit questions via text or email to the moderator for individual or panel discussion.
We are thrilled to have Carolyn on our faculty and excited that she has been offered this honor to contribute insights from her over 30-year career experience in the field of pain with her colleagues at CSM2019. Carolyn will offer her popular courses, Mindfulness for Rehabilitation Professionals at University Hospitals in Cleveland, OH on April 6 and 7, and Mindfulness-Based Pain Treatment in Portland, OR May 18 and 19, and Houston TX, October 26 and 27. We recommend these unique opportunities to train with a nationally recognized leader who pioneered the successful applications of mindfulness to the field of physical therapy. Hope to see you there!
"Over the next 30 years, growth in demand for services to care for female pelvic floor disorders will increase at twice the rate of growth of the same population. Demand for care for pelvic floor disorders comes from a wide age range of women… These findings have broad implications for those responsible for administering programs to care for women, allocating research funds in women’s health and geriatrics, and training physicians to meet this rapidly escalating demand"
- Karl M. Luber, MD, Sally Boero, MD, Jennifer Y. Choe, MD. The demographics of pelvic floor disorders: Current observations and future projections. Presented at the Sixty-seventh Annual Meeting of the Pacific Coast Obstetrical and Gynecological Society, Kamuela, Hawaii, November 14-19, 2000.
Patients with pelvic floor dysfunction have suffered for many years without knowing the names of their ailments. Chronic pain, constipation, incontinence, sexual dysfunction, and other pelvic conditions have a long history of being under-reported, misdiagnosed, and untreated. Shelby Hadden recounts in her animated documentary "Tightly Wound" being told by her doctor to treat vaginismus with a glass of wine before intimacy. She is not the only woman to be given such advice. It is going to take many voices to break through the years of misinformation and stigma that has impeded patients' ability to get treatment.
Thankfully the healthcare landscape has begun to shift. We seem to be on the cusp of a renaissance in pelvic care as patients become more aware of their treatment options. It is the mission of Herman & Wallace to help patients access a higher quality of care, through our courses and through our practitioner directory at https://pelvicrehab.com/. Patient education resources and practitioner directories are a big step in bringing about this awakening, and we believe that the more information the public has access to, the better. Ours is just one of several websites where patients can find learn about their conditions and find qualified clinicians to evaluate them and craft treatment regimens.
We hope that patients find pelvicrehab.com useful, and also encourage them to check out some other great resources. The Section on Women's Health operates a PT Locator available at https://ptl.womenshealthapta.org, and Pelvic Guru has been doing incredible work (see their robust patient portal at https://pelvicguru.com/for-patients/). Patients can also find helpful information via the International Pelvic Pain Society (IPPS) website at https://pelvicpain.org.
Authors: Tamara Rial, PhD, CSPS, Kathleen Doyle-Elmer, PT, DPT and Rebecca Keller, PT, MSPT, PRPC
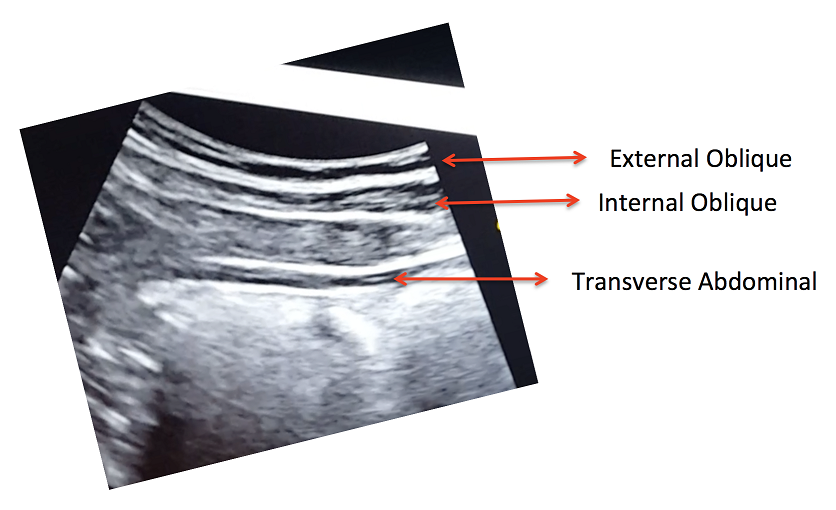
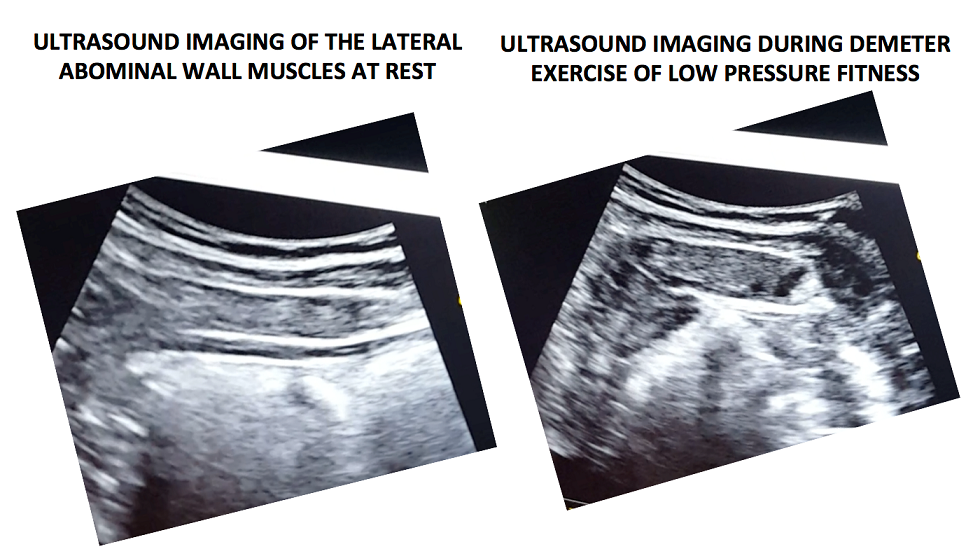
Tamara Rial, PhD, CSPS, co-founder and developer of Low Pressure Fitness will be presenting the first edition of Low Pressure Fitness and Abdominal Massage for Pelvic Floor Care Level 2 and 3 in Princeton, New Jersey in September, 2019. Rebecca Keller and Kathleen Doyle-Elmer are certified Low-Pressure Fitness specialists with training in rehabilitative ultrasound imaging. In this article, the authors discuss and explore the use of transabdominal ultrasound during Low Pressure Fitness on the abdominal and pelvic floor structures.
Real-time ultrasound imaging is a reliable and valid method to evaluate muscle structure, activity and mobility. Over the past few years, there has been increasing interest in the use of transabdominal ultrasound in the field of rehabilitation. The additional value of ultrasound imaging is that it allows for real-time analysis and visual feedback during the performance of pelvic floor and abdominal exercises (Hides et al., 1998). In the field of pelvic health, this is of notable importance when assessing proper movement of the deep abdominal and pelvic muscles during voluntary muscle actions. Transabdominal ultrasound has been found to be a safe, noninvasive, and accurate method to assess and observe muscular and fascial activity (Khorasani et al., 2012). When therapists learn how to properly use and apply ultrasound imaging, this technique can be a comprehensive tool for the clinician and a comfortable procedure for the patient. Moreover, it may be the method of choice for some patients who don’t want to have an internal pelvic examination (Van Delft, Thakar & Sultan, 2015). In this regard, a cross-sectional study found a moderate-to-strong correlation between ultrasound measurements and both digital examination and perineometry for the assessment of pelvic floor muscle actions (Volløyhaug et al., 2016).
Adina Leifer, PT, DPT, PRPC recently passed the Pelvic Rehabilitation Practitioner Certification exam and was kind enough to discuss her career with us. Adina Leifer, PT, DPT, PRPC practices at ABLe Pelvic Physical Therapy in Atlanta, GA. Thank you for the interview, Dr. Leifer, and congratulations on earning your certification!
How did you get involved in the pelvic rehabilitation field?
After graduating from Touro College, and receiving my Doctorate of Physical Therapy. I began to work in an outpatient sports rehab setting. While looking for continuing education courses, I happened upon Herman and Wallace through the Touro College website. They were hosting PF1 at their New York City campus. I knew nothing about pelvic health and rehabilitation at that time. Holly Herman and Tracy Sher taught that first class, after 3 days of class, I was hooked. I knew that pelvic health and wellness was my calling. It has been 9 years since I took that first course and I could not be happier.
What patient population do you find most rewarding in treating and why?
Not sure I can pick one diagnosis or patient population as my favorite. I feel that with each patient that comes to see me, they have either lost ability or do not have normal function of their bladder, bowel or sexual functioning. When I can treat them successfully and educate patients in proper strength and mobility of their pelvic muscles. When I can provide them with the tools so that they can function in their lives, there is nothing more rewarding then that.
Faculty member Nari Clemons, PT, PRPC recently created a two-course series on the manual assessment and treatment of nerves. The two courses, Lumbar Nerve Manual Assessment and Treatment and Sacral Nerve Manual Assessment and Treatment, are a comprehensive look at the nervous system and the various nerve dysfunctions that can impact pelvic health. The Pelvic Rehab Report caught up with Nari to discuss these new courses and how they will benefit pelvic rehab practitioners.
What is "new" in our understanding of nerves? Are there any recent exciting studies that will be incorporated into this course?
The course is loaded with a potpourri of research regarding nerves and histological and morphological studies. There are some fascinating correlations we see with nerve restrictions, wherever they are in the body. Frequently the nerves are compressed in fascial tunnels or areas of muscular overlap, then the nerve, wherever the location, frequently has local vascular axonal change, which increases the diameter of the nerve and prohibits gliding without pain. This causes local guarding and protective mechanisms. Changing pressure on the nerve can change that axonal swelling and allow gliding without pain.
Tamara Rial, PhD, CSPS, co-founder and developer of Low Pressure Fitness will be presenting the first edition of “Low Pressure Fitness and abdominal massage for pelvic care” in Princeton, New Jersey in July, 2018. Tamara is internationally recognized for her work with hypopressive exercise and Low Pressure Fitness. In this article she presents the novel topic of hypopressives as a complementary pelvic floor muscle training tool for incontinence after prostate cancer surgery.
Urinary Incontinence is the most common side effect men suffer after prostate cancer surgery along with erectile dysfunction. Although it is not life threatening, urinary incontinence definitely has a negative impact on the patient’s quality of life Sountoulides et al., 2013. Beyond the frustration and embarrassment associated with pelvic floor dysfunction, many patients describe it as depressing, disheartening and devastating.
The first line of conservative treatment - and most often recommended - is pelvic floor muscle training Andersen et al., 2015. Over the past few years, some researchers have also recommended alternative exercise programs with a holistic approach such as Pilates and hypopressives to improve the patient’s quality of life and urinary incontinence symptoms (Santa Mina et al., 2015). These alternative pelvic floor muscle training programs draw upon the connection between the pelvic floor, it’s synergistic muscles (abdominal, pelvic, lumbar) and their interrelated role in posture and breathing Hodges, 2007; Sapsford, 2004; Madill and McLean, 2008; Talasz et al., 2010. Among these complementary exercise programs, hypopressives have gained increasing attention for the recovery of post-prostatectomy urinary incontinence Santa Mina et al., 2015; Mallol-Badellino, et al. 2015.





































