Who are you? Describe your clinical practice.
Hi! I’m Molly O’Brien-Horn. I’m a Pelvic Health Physical Therapist practicing in an outpatient hospital-based clinic in California. I work with patients of a variety of ages, gender identities, and body variations.
What has your educational journey as a pelvic rehab therapist looked like and how did you get involved in the pelvic rehabilitation field?
I started my career in pediatrics and outpatient orthopedics. I began to notice that those patient populations also had pelvic floor dysfunction, in addition to the diagnoses I was seeing them for. I was fortunate enough to shadow a colleague at the time who did pelvic health. That colleague recommended I take Pelvic Function Level 1 with Herman & Wallace, which I did, and I loved it. During the course, I decided that Pelvic Health was what I wanted to do with my life and the rest is history.
What patient population do you find most rewarding to treat and why?
I know it may sound cliché, but variety is the spice of life, right? I like having the ability to treat a variety of diagnoses within the pelvic health field and be able to help as many different people from as many different walks of life as possible. Being able to treat people of all gender identities, sexual orientations, ability levels, body variations, ages, etc. within the pelvic health field is what’s the most rewarding to me.
What lesson have you learned in a course, from an instructor, or from a colleague or mentor that has stayed with you?
Learning how to practice from a trauma-informed lens has really stayed with me. I’ve been fortunate enough to take multiple courses over the years that centered around trauma-informed care. Trying to practice from a trauma-informed lens, especially when working with patient populations who may have experienced trauma or abuse in their lifetime has been so helpful for my practice and growth as a healthcare provider and as a person.
Now that we know a little bit about you, can you tell us about your new course Intersex Patients: Rehab and Inclusive Care?
What made you want to create this course?
I’ve been to plenty of courses about LGBTQIA+ healthcare and Gender-Affirming Care for LGBTQIA+ folx, but I started to notice that Intersex folx were only briefly mentioned if they were mentioned at all. Healthcare providers need to be better educated on how to provide Intersex-Affirming Healthcare and to learn how to be better allies in healthcare to Intersex folx. They also need to be educated on the healthcare needs that are unique and specific to Intersex patient populations, as those needs may be different than non-Intersex LGBTQIA+ folx, and I wanted to make a course to address that.
What need does your course fill in the field of pelvic rehabilitation?
My course fills a gap in healthcare education about how to provide Intersex-Affirming Healthcare and hopefully helps healthcare workers learn how to be better allies to Intersex folx. Many courses don’t address Intersex-specific needs and wishes in healthcare, and I my course can address that. In the course, I’ve included resources, interviews, and quotes from multiple Intersex folx, activists, and advocacy organizations, as well as research from international human rights groups. I wanted this course to include a variety of Intersex voices from different people across different walks of life so that Intersex folx could discuss their specific wishes, asks, and needs from healthcare providers who are working with Intersex folx.
Who, what demographic, would benefit from your course?
Any healthcare provider can benefit from my course, especially pelvic health providers. I wanted as much of my course to be applicable to as many healthcare providers in different fields and different countries as possible. However, some of the treatments may be geared more towards pelvic health providers since I’m a pelvic health PT in the U.S. and that’s the lens I work through.
What message do you want to send to practitioners who take your course?
I want practitioners to know that I hope they enjoy the course, learn something new, and that they walk away from the course as a better ally in healthcare and as a better Intersex-affirming healthcare provider.
Anything else you want to tell us?
I’m just very grateful for this opportunity to teach with Herman & Wallace and debut this course. I really hope that everyone learns and enjoys the course. And I can’t wait to see everyone for the course's inaugural date on May 4th!
Nicholas Gaffga, MD, MPH, FAAFP sat down with The Pelvic Rehab Report this week to discuss himself and how he came to TA (and teach) for Herman & Wallace. Niko is scheduled to TA next in Birmingham, AL for Pelvic Floor Level 1 scheduled March 4-5 2023, and will be instructing Menstruation and Pelvic Health on February 25-26 2023.
Who are you?
Describe your clinical practice. My name is Niko Gaffga, and I am a family medicine physician seeing patients in Atlanta, GA. Over the 20 years I have been practicing medicine, I have worked in a number of settings: pediatrics, gerontology, emergency room, ICU, HIV prevention in Africa for 4 years, occupational medicine, travel medicine, and obstetrics and gynecology. As I look back over these memories, the area of work where I most feel connected with my patients is women’s health and outpatient gynecology.
How did you get involved in the pelvic rehabilitation field?
My journey in pelvic health physical therapy has been one of the most exciting and rewarding of my career. One day in my clinic I saw a patient who had pelvic pain. When I walked into the room she was crying. Over the next few months, we were able to reduce her IC symptoms considerably with medications and diet modification. And one time when I went into the room to see her, she stood up and smiled and hugged me. This reminded me why I wanted to be a doctor. Along this journey, I realized there were aspects of her experience that I could not address using my training as a physician, so I began investigating other ways to provide more holistic care to my patients. That was when I discovered the world of pelvic floor physical therapy. To understand more, I signed up for PF1. During that 3-day weekend, I saw the power of powerful pelvic floor physical therapy to help patients feel better. Since that time, I have taken all the courses in the Pelvic Floor series, as well as Male Pelvic Floor and three other specialty courses offered at Herman & Wallace. I even overcame my fear and anxiety and signed up to be a teaching assistant. I thought I could never be a TA…but since that time I have been TA 13 times and each time I am grateful for the opportunity to make a difference in other people’s lives. My experience working with pelvic floor practitioners has shown me the power of collaborating among health care professionals with different skills and treatment modalities to offer our patients the most holistic and effective care they can get.
What patient population do you find most rewarding in treating and why?
The most interesting and rewarding aspect of my work is helping patients improve their Menstrual Experience. Menstrual Forums can be difficult to find, but they create opportunities to share knowledge and understanding of the Menstrual Experience to increase Menstrual Optimism, Menstrual Confidence, and ultimately, Menstrual Pride. I have been working for 7 years to create a course that empowers pelvic health practitioners to open a Menstrual Forum with patients to help them better understand and improve their Menstrual Experience. It is a humbling, fascinating, and rewarding experience to walk with someone on a Menstrual Journey.
If you could get a message out to physical therapists about pelvic rehab what would it be?
If there are issues that as a rehab practitioner you are having trouble helping your patients with, explore referring them to a pelvic floor therapist who can help the patient in a whole different way.
What lesson have you learned in a course, from an instructor, or from a colleague or mentor that has stayed with you?
There is a simple scenario that profoundly changed how I see my patients. Physicians carrying out gynecological procedures are trained to sit at the foot of the bed to get the best field of view and to be able to carry out procedures on the patient. However, pelvic floor physical therapists usually sit next to the patient for ergonomics and also to be able to detect pain or anxiety on the face of the patient with each procedure that is carried out. This simple change in perspective invited me to be more aware of the effect that the visit is having on the patient and be more mindful of how they experience the encounter.
What do you find is the most useful resource for your practice?
My most useful resource is the ability to communicate with a variety of health professionals who have
What is in store for you in the future as a clinician?
My dream is to work in outpatient gynecology in close collaboration with a pelvic floor physical therapist to provide holistic health care for our patients.
What books or articles have impacted you as a clinician?
The Female Pelvis (Bandine Calais-Germain) for its beautiful informative illustrations that make pelvic anatomy and physiology come to life; In the Flo (Alisa Vitti) and The Rumi Collection (Kabir Helminski) for their new perspective on life; Period Repair Manual (Lara Briden); and The Fifth Vital Sign (Lisa Hendrickson-Jack) for their informative and proactive approach to understanding and improving the Menstrual Experience.
What has been your favorite Herman & Wallace Course and why?
Pelvic Floor Level 1 was life-changing for me because it introduced me to a whole new field of care and a whole different way of seeing patients. Herman & Wallace has been welcoming to me, as a physician and as a male, into a world where I could have potentially felt like an outsider. Thank you.
What lesson have you learned from a Herman & Wallace instructor that has stayed with you?
In the past 3 years, I have worked with 14 different Herman & Wallace instructors as a participant and as TA. I have learned many lessons, but the one that has helped me the most is the encouragement to follow my dreams and to be the best I can be, even if the road seems difficult or unorthodox. There is a world out there waiting to be created.
What do you love about assisting at courses?
Being a TA at Herman & Wallace courses is the highlight of my month. I literally look at my calendar each day to see how soon it will be until the class starts. I love being a part of other people’s journey to learn more about pelvic floor physical therapy, I love helping people find their way in their careers, I love sharing the things that I am passionate about, I love sharing a physician’s perspective, and most of all I love seeing the light bulb turn on in someone’s eyes when they have visualized something in a new and exciting way.
What is your message to course participants who are just starting their journey?
If pelvic floor therapy is a field that you are curious about or find interesting and you feel a calling for, I encourage you to invest time and energy to learn more about it. Your professional options and your ability to help people will only be limited by what you can imagine.
Ziya Altug, PT, DPT, MS, OCS is a board-certified doctor of physical therapy with 32 years of clinical experience treating musculoskeletal injuries. Z currently provides outpatient physical therapy in the home setting in Los Angeles, California, and serves as a continuing education instructor. He received his Bachelor of Science in Physical Therapy at the University of Pittsburgh in 1989, a Master of Science in Sport and Exercise Studies in 1985, a Bachelor of Science in Physical Education in 1983 from West Virginia University, and a Doctor of Physical Therapy from the College of St. Scholastica in 2015. Z is a long-standing member of the American Physical Therapy Association and a member of the American College of Lifestyle Medicine. He has attended workshops in yoga, tai chi, qigong, Pilates, Feldenkrais Method, and the Alexander Technique.
Dr. Altug is the author of the books Integrative Healing: Developing Wellness in the Mind and Body (2018), The Anti-Aging Fitness Prescription (2006), and Manual of Clinical Exercise Testing, Prescription, and Rehabilitation (1993). In 2020, he published the chapter Exercise, Dance, Tai Chi, Pilates, and Alexander Technique in The Handbook of Wellness Medicine. In 2021, he published the article Lifestyle Medicine for Chronic Lower Back Pain: An Evidence-Based Approach in the American Journal of Lifestyle Medicine. Z joins the H&W faculty and is presenting his personally curated course Integrative and Lifestyle Medicine Toolbox for Rehab and Pain Management. This week he sat down with The Pelvic Rehab Report to discuss his course.
What made you want to create this course?
My father was a physician specializing in internal medicine. He specialized in treating conditions such as tuberculosis, chronic obstructive pulmonary disease (COPD), and asthma. Starting in elementary school, I remember discussing with my Dad the importance of nutrition, sleep, stress control, and sustainable activity in healing. Of course, as a ten-year-old, I played with his stethoscope and reflex hammer for hours! My father used “lifestyle medicine” principles to help his patients recover. My Mom introduced me to the benefits of aromatherapy for relaxation. She used to wash our clothes with lavender-scented soaps, and there was lavender-scented potpourri throughout our house. My mother used to say the lavender was to “keep the wolves away so the sheep can sleep.” She also taught me how to prepare and cook healthful meals in high school. Now, I have a fascination with culinary medicine. I am very grateful for all of these childhood experiences.
Before entering PT school, I majored in physical education and exercise science. After I graduated from PT school, I wanted to use my interest in wellness, health, fitness, and self-care strategies to help patients heal and recover. Recently, I have followed the American College of Lifestyle Medicine research and webinars to gain additional knowledge. Currently, I treat patients in their homes and teach continuing education courses in integrative and lifestyle medicine.
What need does your course fill in the field of pelvic rehabilitation?
This course provides practical tools to help clinicians manage pain. For example, my course will cover research, resources, and labs to create clinically relevant pain, anxiety, depression, and stress management strategies using lifestyle medicine, integrative medicine, and expressive and art-based therapies. Participants will be able to practice Tai Chi/Qigong, expressive and art-based therapies including Music, Dance, and Drama Therapy, nature and aromatic therapies, self-hypnosis, and self-massage. All of these strategies may be helpful for clinicians specializing in pelvic rehabilitation.
Who, what demographic, would benefit from your course?
Rehabilitation providers of any experience level would benefit from taking this course.
What patient population do you find most rewarding in treating and why?
I currently focus on orthopedics and geriatrics. I especially enjoy working with older patients in their homes and designing creative home exercise programs they can use to stay healthy.
What do you find is the most useful resource for your practice?
I enjoy using resources from the following organizations:
- American College of Lifestyle Medicine
- American College of Sports Medicine
- International Association for the Study of Pain
What books or articles have impacted you as a clinician?
I enjoyed reading the following three books to expand my knowledge of lifestyle medicine and integrative medicine:
- Lifestyle Medicine by James Rippe
- Lifestyle Medicine Handbook by Beth Frates and colleagues
- Lifestyle Medicine by Garry Egger and colleagues
What is your message to course participants who are just starting their journey?
I recommend all clinicians collaborate with professionals outside their own profession. For example, I recommend physical therapists work with the following:
- Acupuncturists, massage therapists, registered dietitians
- Practitioners in yoga, Pilates, qigong, tai chi, Alexander Technique, Feldenkrais Method
- Specialists in expressive therapies such as dance, music, art, drama, poetry, and play.
Integrative and Lifestyle Medicine Toolbox for Rehab and Pain Management

Course Dates:
January 21, 2023
Price: $125
Experience Level: Beginner
Contact Hours: 4.5
Description: This course was written and developed by Ziya “Z” Altug, PT, DPT, MS, OCS, a board-certified doctor of physical therapy with 32 years of experience in treating musculoskeletal conditions, Brief lectures on the research and resources and labs will cover a toolbox approach for creating clinically relevant pain, anxiety, depression, and stress management strategies using lifestyle medicine, integrative medicine, expressive and art-based therapies, and the impact of nature on health. Participants will be able to practice Tai Chi/Qigong, expressive and art-based therapies including Music, Dance, and Drama Therapy, nature and aromatic therapies, self-hypnosis, and self-massage.
Tara Sullivan, PT, DPT, PRPC, WCS, IF sat down with Holly Tanner and The Pelvic Rehab Report to discuss her course, Sexual Medicine in Pelvic Rehab. Tara started in the healthcare field as a massage therapist, practicing for over ten years including three years of teaching massage and anatomy, and physiology. Tara has specialized exclusively in Pelvic Floor Dysfunction treating bowel, bladder, sexual dysfunctions, and pelvic pain since 2012.
Hi Tara, can you introduce yourself and tell us a little bit about your background?
Sure! So I’m Tara. I’ve been a pelvic health rehab therapist for about 10 years now. I started right out of PT school and I got a job at a local hospital where they were looking to grow and build the pelvic rehab program. So of course, I found Herman & Wallace and started taking all of the classes there that I could and just kept learning over the years. Now the program is expanded across the valley, we have nine different locations, and it’s been very successful and fulfilling. It’s my passion.
Recently, I would say the past four to five years of my career, I’ve started getting more into sexual dysfunctions. I was always into pelvic floor dysfunction in general - bowel, bladder, sexual dysfunction, and chronic pelvic pain, but I didn’t get specifically into the sexual medicine side of it until recently. I did the fellowship with ISSWSH that really pulled all of that information together with what I’ve learned through the years.
Can you explain what ISSWSH is and how that combined with the knowledge base that you already had?
I feel like ISSWSH for me, where I came full circle. I finally was like “I get it.” ISSWSH is the International Society for the Study of Women’s Sexual Health and it’s all the gurus like Dr. Goldstein, Rachel Rubin, and Susan Kellogg that have been around forever doing the research on sexual medicine. I started attending their conferences, became a faculty member, and presented at their annual fall meeting here in Scottsdale. Then I ended up doing their fellowship. Every year I would attend the conference, but it took a couple of years for all of that knowledge to soak in and for me to be able to really apply it. For example, that patient with that sticky discharge, maybe that is lichen planus – that’s the kind of medical side that you don’t necessarily learn in physical therapy school.
That for me just really helped my differential diagnosis which means that you can get the patient’s care faster. Get them to that resolution faster because you are working with a team of people and we all have our roles. As PTs and rehab practitioners, we have the time to sit with our patients. We are so blessed to have an hour, and the medical doctors don’t, for us to really take that time to figure out the patient’s history and what they’ve been through, and what could be the cause of it. We have the time to be the detective and help them get the care they need. Whether it’s with us, or in conjunction with something else. My goal is to never tell someone that I can’t help them because it’s not muscular.
How has this knowledge helped you in your collaboration with other practitioners in your practice?
I feel like this knowledge was the missing link for me. It brings it all together for the patient. So the patients come here and the urologist says “that’s not my area,” and then the gynecologist says “that’s not my area.” Then they come to you and you’re like “it’s kind of my area, but I can’t prescribe the medication that you need.”
My practice got so much better, just in the sense of the overall quality of care, when I was able to develop those relationships with the doctors. I could pick up the phone and say “Hey, that patient that you sent me – I think they have vestibulodynia, and I think it’s from their long-term use of oral contraceptive pills. I think that they might benefit from some local estrogen testosterone cream.” They would say, I don’t know about that, and I’d respond “let me send you some articles. Let me tell you what I’ve learned.”
Now I can just pick up the phone or send them a text asking them to prescribe so and so. It really helped bridge that gap. The doctors now will say “Ok. I know something’s going on, but I don’t know if it’s muscular or tissue. I don’t have that training, what do you think?” So it’s just been such a collaboration, it’s been so great. Then I’ll go the reverse of that and watch them do a surgery, watch them do a procedure.
For our patients, we need to take that time and work with the physicians and develop that relationship with them, because it’s easy to pass it off as “that’s not my job.” Especially the vestibule! The gynecologist goes right through it and looks into the vaginal canal and then the urologist is like I’m going to look at the urethra but I’m not looking around it, let me just stick that scope in. This knowledge and ability to use differential diagnosis, for me just brings it all together.
Does your course have an online, pre-recorded portion as well as a live component?
Yes. There are about nine lab videos on manual techniques because everyone wants to know what to do. For me, it’s more about what you know. What can you identify and differentiate with the differential diagnosis. Then we have about two hours of just the basic lectures on general pain and overactivity of the pelvic floor so that we can spend our time in the live lecture getting into the very specific conditions that we as PTs are, not necessarily diagnosing, but recognizing and sending for further care. That’s really where I wanted this class to fill the gap between the urologist, the gynecologist, and the PT.
Is your course primarily vulvo-vaginal conditions or are there some penile, scrotal, or other conditions?
It is both male and female dysfunctions, and I have a few transgender cases. I don’t personally treat the transgender population very often so I only have a couple of examples of that. I have a lot of examples where I’m trying to get practitioners to recognize the problem by what the patient is saying and their history, and how to funnel this into their differential diagnosis. Case studies include different types of vestibulodynia and causes, all the different skin conditions…and it’s not necessarily something that they didn’t learn in one of the Pelvic Floor Series courses, but I wanted one class where they could just talk about all the sexual dysfunctions and get into some of the ones that we don’t see as often but are present.
We also talk about PGAD (persistent genital arousal disorder), and with male dysfunctions, we talk about spontaneous ejaculation and urethral discharge, post finasteride syndrome. All of these things that you might not see every day, but when you see them you’ll recognize them so that you can help patients talk to the doctor and get the proper care. There are a lot of random, not as obvious, conditions that are not as prevalent. Then there are the common conditions that we see every single day like lichens.
What is the biggest takeaway that practitioners have who come into your class?
It is really being able to access and effectively use differential diagnosis. A lot of practitioners in the course are like “I always wondered what that was.” I have a ton of pictures that I share, and I’m like, I know have seen this before. I think a lot of it is the differential diagnosis. The feedback that I get from every class is “I feel like I can go to the clinic on Monday and apply what I learned.” “I’m going to go buy a q-tip and start doing a q-tip test because now I know what to do with that information.” They feel that confidence of really being able to apply it, talk to the patient, talk to the doctors, and figure out that meaningfulness.

Sexual Medicine in Pelvic Rehab
Course Dates:
January 14-15, 2023
May 13-14, 2023
September 23-24, 2023
Price: $450
Experience Level: Beginner
Contact Hours: 15
Description: This two-day course provides a thorough introduction to pelvic floor sexual function, dysfunction, and treatment interventions, as well as an evidence-based perspective on the value of physical therapy interventions for patients with chronic pelvic pain related to sexual conditions, disorders, and multiple approaches for the treatment of sexual dysfunction including understanding medical diagnosis and management.
Lecture topics include hymen myths, squirting, G-spot, prostate gland, sexual response cycles, hormone influence on sexual function; the anatomy and physiology of pelvic floor muscles in sexual arousal, orgasm, and function, and specific dysfunction treated by physical therapy in detail. Including vaginismus, dyspareunia, erectile dysfunction, hard flaccid, prostatitis, and post-prostatectomy, as well as recognizing medical conditions such as persistent genital arousal disorder (PGAD), hypoactive sexual desire disorder (HSDD), and dermatological conditions such as lichen sclerosis and lichen planus. Upon completion of the course, participants will be able to confidently treat sexual dysfunction related to the pelvic floor as well as refer to medical providers as needed and instruct patients in the proper application of self-treatment and diet/lifestyle modifications.
Course Reviews:
- The instructor offered excellent examples of what can be seen in the patient population and advised good treatment plans to help. She was very thorough in answering questions and very well-informed on all topics presented in this class. I was so thankful to learn more about the hormone component of pelvic floor rehab, as I feel that this is greatly lacking in the Midwest -- we still live on the idea that hormones and HRT are BAD! Looks like I will be doing some heavy marketing soon with research articles! Thank you so much for all of this information!
- Various topics only glossed over in other courses were covered in detail to meet the various levels of knowledge of all students in the class. On top of this, new and useful material was also introduced and explained very well.
- Tara gave practical tips for us to start using in clinical practice and her notes to her lecture were KEY!
Rachna Mehta, PT, DPT, CIMT, OCS, PRPC is the author and instructor of the Acupressure for Optimal Pelvic Health course. Rachna brings a wealth of experience to her physical therapy practice and has a personal interest in various eastern holistic healing traditions.
One of the main reasons I got into Acupressure was because of my complex orthopedic patients. People who were struggling with chronic pelvic pain, and a lot of my patients were doing complementary and alternative medicine ( CAM ) modalities like Acupuncture and Yoga. That got me interested, because as they were going along with those programs in addition to therapy, the question they always asked was what could they do themselves.
I started looking into Acupressure and found that there was such a big knowledge base, but the information was very scattered. If I found a study that talked about Acupressure points, I wouldn’t know where they were located, what they were good for, where I could use them, or how I could integrate them into my practice. I started to piece the information together and that was the conception of this course Acupressure for Optimal Pelvic Health.
Acupressure for Optimal Pelvic Health is a two-day course with about an hour and a half of pre-recorded lectures that go over the history of Acupuncture (because Acupressure draws from that), Traditional Chinese Medicine (TCM) concepts, getting our basics down, and terminology. We talk about the meridian channels, Ying and Yang, and where the meridians and Acupoints are located on the body. Next we delve into the scientific and evidence-based perspectives by taking a look at all of the evidence for Acupuncture and Acupressure.
From there we go into how to read the chart and what are the abbreviations. We have 12 main meridians that we look at and out of those there are 4 that we focus more on for pelvic health. Those are the Bladder, the Kidney, the Stomach, and the Spleen meridians - those have the most points that we focus on. There are also other important points all over the body that help and stimulate the nervous system and tap into the peripheral nervous system, the Qi, and improve the physiological functioning of the organs.
Lectures also talk about the fascial and connective tissue networks, and how Acupoints are located along fascial planes. We discuss the connections of the fascia with the peripheral nervous system and how Acupoints have high electrical conductivity on the surface of the skin (there are instruments that can measure this). Next, we tackle the question of how Acupoints tap into the central nervous system and how there are internal connections to the different organs that can help to heal and promote physiological wellbeing. Acupressure can treat conditions like anxiety, incontinence, constipation, dysmenorrhea and a host of pelvic health conditions. Acupressure is good for so many different things.
On day two of class, we dive into Yin yoga. Yin yoga is a very beautiful form of yoga. It’s a quiet, meditative form of yoga, and it connects the Acupressure points by putting the body in specific poses that stress those tension lines along the meridians. It is a mindful way of putting the body in specific positions and supporting the body with props. It is also a meditative state in which we stay in each pose for about 3 to 5 minutes, and we become still. The main principles of Yin Yoga are that we arrive in a pose, become still and stay for time. We get into a pose and basically, we are meeting our body where it is. It’s also a lot of acceptance and mindfulness. Stillness is something that a lot of people have a hard time doing, be it physical or stillness of the mind.
The beauty of us using Acupressure is that we are musculoskeletal specialists and we are so hands on with all of our patients. If we know exactly where the points are, we can work on those points as we are working on other things such as stretching a muscle, doing range of motion, or just working on fascia. There are a lot of things that we can do for our pelvic health patients in particular, but this is applicable to even our orthopedic patients.
Acupressure is truly a mind-body practice that can be taught to patients in their journey towards self-care, holistic healing and wellness.
Acupressure for Optimal Pelvic Health
Course Dates:
October 15-16, 2022
February 4-5, 2023
June 3-4, 2023
October 14-15, 2023
Price: $450
Experience Level: Beginner
Contact Hours: 12.5
Description: This is a two-day course that offers an evidence-based perspective on the application of Acupressure for evaluating and treating a host of pelvic health conditions including bowel, bladder, and pelvic pain issues. The course explores a brief history of Acupressure, its roots in Acupuncture and Traditional Chinese Medicine (TCM), and presents current evidence that supports the use of complementary and alternative medicine as an adjunct to western medicine. TCM concepts of Meridian theory and energy channels are presented with scientific evidence of Acupoints transmitting energy through interstitial connective tissue with potentially powerful integrative applications through multiple systems.
Lectures will present evidence on the use of potent Acupressure points and combinations of points for treating a variety of pelvic health conditions including chronic pelvic pain, dysmenorrhea, constipation, digestive disturbances, and urinary dysfunctions to name a few. Key acupoints for decreasing anxiety, and stress and bringing the body back to a state of physiological balance are integrated throughout the course. Participants will be instructed through live lectures and demonstrations on the anatomic location and mapping of acupressure points along five major meridians including the spleen, stomach, kidney, urinary bladder, and gall bladder meridians. Key associated points in the pericardium, large intestine, small intestine, lung and liver meridians as well as the governing and conception vessels will also be introduced. The course offers a brief introduction to Yin yoga and explores Yin poses within each meridian to channelize energy through neurodynamic pathways to promote healing across multiple systems. Participants will learn how to create home programs and exercise sequences and will be able to integrate acupressure and Yin yoga into their orthopedic and pelvic health interventions.
This week The Pelvic Rehab Report sat down with faculty member Ken McGee, PT, DPT. Ken (they/he) is a queer transmasculine pelvic health physical therapist based in Seattle whose mission is to bring greater awareness to the pelvic health needs of the LGBTQIA2S community. Their practice, B3 Physical Therapy, centers on transgender and perinatal rehabilitation. Ken also provides peer bodyfeeding support and doula care, and can be found on Instagram at @b3ptcob3ptco.
You can join Ken in their remote course, Perinatal Mental Health: The Role of the Pelvic Rehab Therapist, scheduled for October 22, 2022.
Who are you? Describe your clinical practice.
Experiencing inadequate care for my own pelvic health conditions as a teenager motivated me to become a pelvic health physical therapist. Being a member of the queer community further drove me to offer trauma-informed care and develop better access to care through home visits. Currently, I split my time between providing gender-affirming physical therapy and serving as a birth doula.
What lesson have you learned (in a course, from an instructor, or from a colleague or mentor) that has stayed with you?
Very few clients will remember detailed biomechanical explanations or every exercise you teach them. However, each client will remember how you treated them and how you made them feel. Asking clients about their preferences for care and following up go a long way in establishing rapport.
What do you find is the most useful resource for your practice?
One of my favorite resources is Decolonizing Fitness. It is an educational platform by Ilya Parker, PTA, (he/they). It provides a catalog of exercises and trainings for people looking to improve their care of gender-diverse people and People of Global Majority.
What books or articles have impacted you as a clinician?
The healthcare field regularly puts people in boxes to determine care. For example, many providers might determine care based on whether someone is a transgender woman or man. However, gender is actually someone’s individual experience rather than a category. Kate Bornstein’s My New Gender Workbook is a good starting point for understanding gender as uniquely one’s own, rather than part of a treatment algorithm.
What made you want to create this course, Perinatal Mental Health?
I wanted to create this course because, as a parent and physical therapist, I see both the challenges that the perinatal period presents, as well as the ways that rehabilitation providers can support mental health. In developing the content, I drew upon my background as a volunteer for a perinatal mental health warm line.
What need does your course fill in the field of pelvic rehabilitation?
Pelvic rehabilitation providers regularly interact with people who have mental health challenges. However, there are very few courses that specifically address the needs of the pelvic health providers serving folks in the perinatal period. This course looks at perinatal mental health from the perspective of pelvic rehabilitation providers, while offering specific actions providers can take to support their clients.
Who, what demographic, would benefit from your course?
Rehabilitation providers of any experience level would benefit from taking this course. Providers who are new parents or considering becoming pregnant may also find the content personally enriching. While the research discussed in this course focused on the perinatal period, much of it can be extrapolated to other populations.
What is your message to course participants who are just starting their journey?
For people just starting in pelvic rehabilitation, I would recommend focusing on patient education. For me, I find that the greatest amount of client improvement comes through reviewing the basics. It’s okay to still be developing skills in manual therapy.

Perinatal Mental Health: The Role of the Pelvic Rehab Therapist
Price: $150
Contact Hours: 5.75
Course Date: October 22, 2022
Description: This one-day remote course covers mental health considerations in pregnancy and postpartum and is targeted to the pelvic rehab clinician treating patients in the peripartum period. Topics include common mental health concerns in the postpartum period including depression, anxiety, OCD, and PTSD, as well as the connectedness between mental health and physical dysfunction. The course will introduce useful screening tools and how to connect patients to resources and diagnosing professionals. Labs will include partnered breakout sessions to practice listening and dialogue skills. The course also includes a review of coping techniques to support mental health and physical symptoms.
This week for the Pelvic Rehab Report, Holly Tanner sat down to interview faculty member Erica Vitek, MOT, OTR, BCB-PMD, PRPC on her specialty course Parkinson Disease and Pelvic Rehabilitation. If you would like to learn more about working with this patient population join Erica on June 24th-25th for the next course date!
This is Holly Tanner with the Herman and Wallace Pelvic Rehab Institute and I'm here with Erica Vitek who's going to tell us about of course that she has created for Herman and Wallace. Erica, will you tell us a little bit about your background?
Yes. Absolutely. Thanks for chatting with me today about my course! So my course is Parkinson Disease and Pelvic Rehabilitation. I'm just so excited to be part of the team and to be sharing all this great information. How I got the idea for the course is that there was a need for more neuro-type topics related to pelvic health, and individuals were reaching out to me because my specialty is in both Parkinson disease, rehabilitation, as well as pelvic health, and I always talked about the connections and wanting to bring that information to more people. So I wanted to plate all that information together in this great course.
I got started specializing in Parkinson's back in the early 2000s. I was hired at a hospital as an occupational therapist working with people with Parkinson disease. But when I was in college my real interest was pelvic health. So I kind of got thrown into learning a whole lot about Parkinson disease at that time and I got really interested in how it all related to what I really wanted to do, which was pelvic health. I was able to connect that all, really right from the beginning of my career. Even though I started more on the physical rehabilitation side of Parkinson disease, which I continue to this day. I am able to combine those two passions of mine.
I also am an instructor with LSVT Global(1)and so we do LSVT BIG®(2) course training and certification workshops and I work with them a lot. I also have still a physical rehab background, as well as my connection to the public health background, and I bring that all together in my course Parkinson Disease and Pelvic Rehabilitation. We have two packed-full days of information and I think really it does translate well to the virtual environment.
What are the connections between neuro and pelvic health? Can you talk about what some of the big cornerstone pieces are that you get to dive into with your class?
The beginning of the course on the first day is going back to the basics of neuro in general. Really getting our neuro brains on and thinking about terminology, topics related to neurotransmitters and the autonomic nervous system. Individuals with Parkinson’s specifically, their motor system is affected but also their non-motor systems. This includes autonomic function, the limbic system, and all of the different motor functions that also affect the pelvic floor in addition to all of the other muscles in the body.
We have all of this interplay of things going on that affect the bladder, bowel, and sexual health systems in individuals with Parkinson's that is a little bit different than your general population. There are a multitude of bladder issues that are very specific to the PD population, for example, overactive bladder.
This is just one example of the depths we go into right in the beginning on day one where we get into the neuroanatomy and neurophysiology of why that is actually happening. This then helps us go into day two where we talk about the practicality of what you do in the clinic about the things that are happening neurologically which is causing all of these bladder, bowel, and sexual health issues.
What kind of tools do you give to people to help practitioners understand and implement a treatment program?
People with PD are on very complex medication regimens and many of them are elderly, so the medication complexity is much more challenging in this population. At the end of day one, the last lecture, we go through the pharmacology very specifically for people with Parkinson’s in order to have a base of understanding of how that is interplaying with the pelvic health conditions.
We set the baseline of getting that information from your patient off the bat, then discuss what you want to be looking for when you start off with that patient and the importance of finding out what kind of bladder and bowel medications they have taken thus far and how that can potentially interplay with their Parkinson’s. Individuals with PD can have potentially worse side effects from some of those medications that are used for bladder issues specifically. We dig into what to look for, we talk a lot about practical behavioral modifications using bladder and bowel diaries and things like that to weed out some things in addition to using our other skills as pelvic health practitioners.
How can people prepare themselves to come to Parkinson Disease and Pelvic Rehabilitation, are there required readings or things that would be helpful for people to catch up a little bit on the pelvic health or neuro side?
I feel like, and I hope, that I did a really good job at the basic review right at the beginning so we can talk through these topics together. I prefer to take a course and not have to spend a lot of extra time on the pre-recordings because sometimes that can be overwhelming with busy lifestyles. When I put together this course I really wanted us to focus together as a group as we start the class to dig into those basics at the beginning and not have a lot of required things to do prior.
So what I did at the beginning of the course is to make a lot of tables, a lot of charts, and a lot of drawings, that we can reference (we don’t have to memorize it) and look at as needed. We can look at a chart and a drawing right next to it in the manual. I spent a lot of time just putting it all down in words, what I’m saying, so you don’t have to take a lot of notes. I think this has really helped practitioners as we get into the course and learn about the details of Parkinson’s and pelvic health.
What is it that makes you so passionate about working with these patients and continuing to learn and share your knowledge?
It is so heartwarming and feels so good to help these individuals. The motor symptoms of PD are really the ones recognized by physicians or even outwardly noticed even by other individuals. These private conditions of pelvic health that we are helping with are things that they might not even mention to their physician. Maybe we find out when we are doing other physical rehab or when colleagues refer them to us because they know what we do, and to help them with something of this magnitude that affects their everyday life - when they have trouble just walking, or moving or transferring.
Their caregiver burden for these individuals is so high because their loved one - now turned caregiver - is helping them do everything. We can make such an impact on these individuals. I mean, we do on other people too, but when you have a progressive neurologic condition and we can make an effect on shaping techniques they can use to improve their day-to-day. It’s just so great to be able to help them.
Sometimes these patients with PD can have cognitive impairments, they can have difficulties learning, and that can be helpful for the care partner. It can be a significant reduction in their burdon. I do talk a lot in the course about cognitive impairment and I give a lot of tips about how we can train and some ideas. People with Parkinson’s muscles and minds are a little different so there are some great tips that I can provide and lots of clinical experience.
I’ve been an occupational therapist for over 20 years, so I have a ton of clinical experience with this population. It’s been the population I’ve worked with my entire career. I hope I can provide the passion that I have for working with these individuals as well as the individuals who take my class.
I’m sure you would agree that we need more folks knowledgeable about Parkinson’s and combine that with pelvic health knowledge as well.
There are over a million people in the United States alone that have Parkinson disease. It’s the second most common neuro-degenerative disorder just behind Alzheimer’s disease. So there are so many individuals dealing with this and I think we can really expand our practices. I don’t think a lot of individuals that work in pelvic health market themselves to neurologists. There is an opening there for additional referrals and more people that we can help.

References:
- SVT Global is an organization that develops innovative treatments that improve the speech and movement of people with Parkinson’s disease and other neurological conditions. They train speech, physical and occupational therapists around the world in these treatments so that they can positively impact the lives of their patients.
- LSVT BIG®: Physical Therapy for Parkinson’s Disease and Similar Conditions. LSVT BIG trains people with Parkinson disease to use their body more normally.

The following is an excerpt from the short interview between Holly Tanner and Tara Sullivan discussing her course Sexual Medicine in Pelvic Rehab. Watch the full video on the Herman & Wallace YouTube Channel.
Hi Tara, can you introduce yourself and tell us a little bit about your background?
Sure! So I’m Tara. I’ve been a pelvic health rehab therapist for about 10 years now. I started right out of PT school and I got a job at a local hospital where they were looking to grow and build the pelvic rehab program. So of course, I found Herman & Wallace and started taking all of the classes there that I could and just kept learning over the years. Now the program is expanded across the valley, we have nine different locations, and it’s been very successful and fulfilling. It’s my passion.
Recently, I would say the past four to five years of my career, I’ve started getting more into sexual dysfunctions. I was always into pelvic floor dysfunction in general - bowel, bladder, sexual dysfunction, and chronic pelvic pain, but I didn’t get specifically into the sexual medicine side of it until recently. I did the fellowship with ISSWSH that really pulled all of that information together with what I’ve learned through the years.
Can you explain what ISSWSH is and how that combined with the knowledge base that you already had?
I feel like ISSWSH for me, where I came full circle. I finally was like “I get it.” ISSWSH is the International Society for the Study of Women’s Sexual Health and it’s all the gurus like Dr. Goldstein, Rachel Rubin, and Susan Kellogg that have been around forever doing the research on sexual medicine. I started attending their conferences, became a faculty member, and presented at their annual fall meeting here in Scottsdale. Then I ended up doing their fellowship. Every year I would attend the conference, but it took a couple of years for all of that knowledge to soak in and for me to be able to really apply it. For example, that patient with that sticky discharge, maybe that is lichen planus – that’s the kind of medical side that you don’t necessarily learn in physical therapy school.
That for me just really helped my differential diagnosis which means that you can get the patient’s care faster. Get them to that resolution faster because you are working with a team of people and we all have our roles. As PTs and rehab practitioners, we have the time to sit with our patients. We are so blessed to have an hour, and the medical doctors don’t, for us to really take that time to figure out the patient’s history and what they’ve been through, and what could be the cause of it. We have the time to be the detective and help them get the care they need. Whether it’s with us, or in conjunction with something else. My goal is to never tell someone that I can’t help them because it’s not muscular.
How has this knowledge helped you in your collaboration with other practitioners in your practice?
I feel like this knowledge was the missing link for me. It brings it all together for the patient. So the patients come here and the urologist says “that’s not my area,” and then the gynecologist says “that’s not my area.” Then they come to you and you’re like “it’s kind of my area, but I can’t prescribe the medication that you need.”
My practice got so much better, just in the sense of the overall quality of care, when I was able to develop those relationships with the doctors. I could pick up the phone and say “Hey, that patient that you sent me – I think they have vestibulodynia, and I think it’s from their long-term use of oral contraceptive pills. I think that they might benefit from some local estrogen testosterone cream.” They would say, I don’t know about that, and I’d respond “let me send you some articles. Let me tell you what I’ve learned.”
Now I can just pick up the phone or send them a text asking them to prescribe so and so. It really helped bridge that gap. The doctors now will say “Ok. I know something’s going on, but I don’t know if it’s muscular or tissue. I don’t have that training, what do you think?” So it’s just been such a collaboration, it’s been so great. Then I’ll go the reverse of that and watch them do a surgery, watch them do a procedure.
For our patients, we need to take that time and work with the physicians and develop that relationship with them, because it’s easy to pass it off as “that’s not my job.” Especially the vestibule! The gynecologist goes right through it and looks into the vaginal canal and then the urologist is like I’m going to look at the urethra but I’m not looking around it, let me just stick that scope in. This knowledge and ability to use differential diagnosis, for me just brings it all together.
Does your course have an online, pre-recorded portion as well as a live component?
Yes. There are about nine lab videos on manual techniques because everyone wants to know what to do. For me, it’s more about what you know. What can you identify and differentiate with the differential diagnosis. Then we have about two hours of just the basic lectures on general pain and overactivity of the pelvic floor so that we can spend our time in the live lecture getting into the very specific conditions that we as PTs are, not necessarily diagnosing, but recognizing and sending for further care. That’s really where I wanted this class to fill the gap between the urologist, the gynecologist, and the PT.
Is your course primarily vulvo-vaginal conditions or are there some penile, scrotal, or other conditions?
It is both male and female dysfunctions, and I have a few transgender cases. I don’t personally treat the transgender population very often so I only have a couple of examples of that. I have a lot of examples where I’m trying to get practitioners to recognize the problem by what the patient is saying and their history, and how to funnel this into their differential diagnosis. Case studies include different types of vestibulodynia and causes, all the different skin conditions…and it’s not necessarily something that they didn’t learn in one of the Pelvic Floor Series courses, but I wanted one class where they could just talk about all the sexual dysfunctions and get into some of the ones that we don’t see as often but are present.
We also talk about PGAD (persistent genital arousal disorder), and with male dysfunctions, we talk about spontaneous ejaculation and urethral discharge, post vasectomy syndrome. All of these things that you might not see every day, but when you see them you’ll recognize them so that you can help patients talk to the doctor and get the proper care. There are a lot of random, not as obvious, conditions that are not as prevalent. Then there are the common conditions that we see every single day like lichens.
What is the biggest takeaway that practitioners have who come into your class?
It is really being able to access and effectively use differential diagnosis. A lot of practitioners in the course are like “I always wondered what that was.” I have a ton of pictures that I share, and I’m like, I know you guys have seen this before. I think a lot of it is the differential diagnosis. The feedback that I get from every class is “I feel like I can go to the clinic on Monday and apply what I learned.” “I’m going to go buy a q-tip and start doing a q-tip test because now I know what to do with that information.” They feel that confidence of really being able to apply it, talk to the patient, talk to the doctors, and figure out that meaningfulness.

2022 Course Dates:
July 16-17 2022 and October 15-16 2022
Sexual Medicine in Pelvic Rehab is designed for pelvic rehab specialists who want to expand their knowledge, experience, and treatment in sexual health and dysfunction. This course provides a thorough introduction to pelvic floor sexual function, dysfunction, and treatment interventions for all people and sexual orientations, as well as an evidence-based perspective on the value of physical therapy interventions for patients with chronic pelvic pain related to sexual conditions, disorders, as well as multiple approaches for the treatment of sexual dysfunction including understanding medical diagnosis and management.
Lecture topics include hymen myths, female squirting, G-spot, prostate gland, female and male sexual response cycles, hormone influence on sexual function, anatomy and physiology of pelvic floor muscles in sexual arousal, orgasm, and function and specific dysfunction treated by physical therapy in detail including vaginismus, dyspareunia, erectile dysfunction, hard flaccid, prostatitis, post-prostatectomy, as well as recognizing medical conditions such as persistent genital arousal disorder (PGAD), hypoactive sexual desire disorder (HSDD) and dermatological conditions such as lichen sclerosis and lichen planus. Upon completion of the course, participants will be able to confidently treat sexual dysfunction related to the pelvic floor as well as refer to medical providers as needed and instruct patients in the proper application of self-treatment and diet/lifestyle modifications.
Audience:
This continuing education course is appropriate for physical therapists, occupational therapists, physical therapist assistants, occupational therapist assistants, registered nurses, nurse midwives, and other rehabilitation professionals of all levels and experience. Content is not intended for use outside the scope of the learner's license or regulation. Physical therapy continuing education courses should not be taken by individuals who are not licensed or otherwise regulated, except, as they are involved in a specific plan of care.
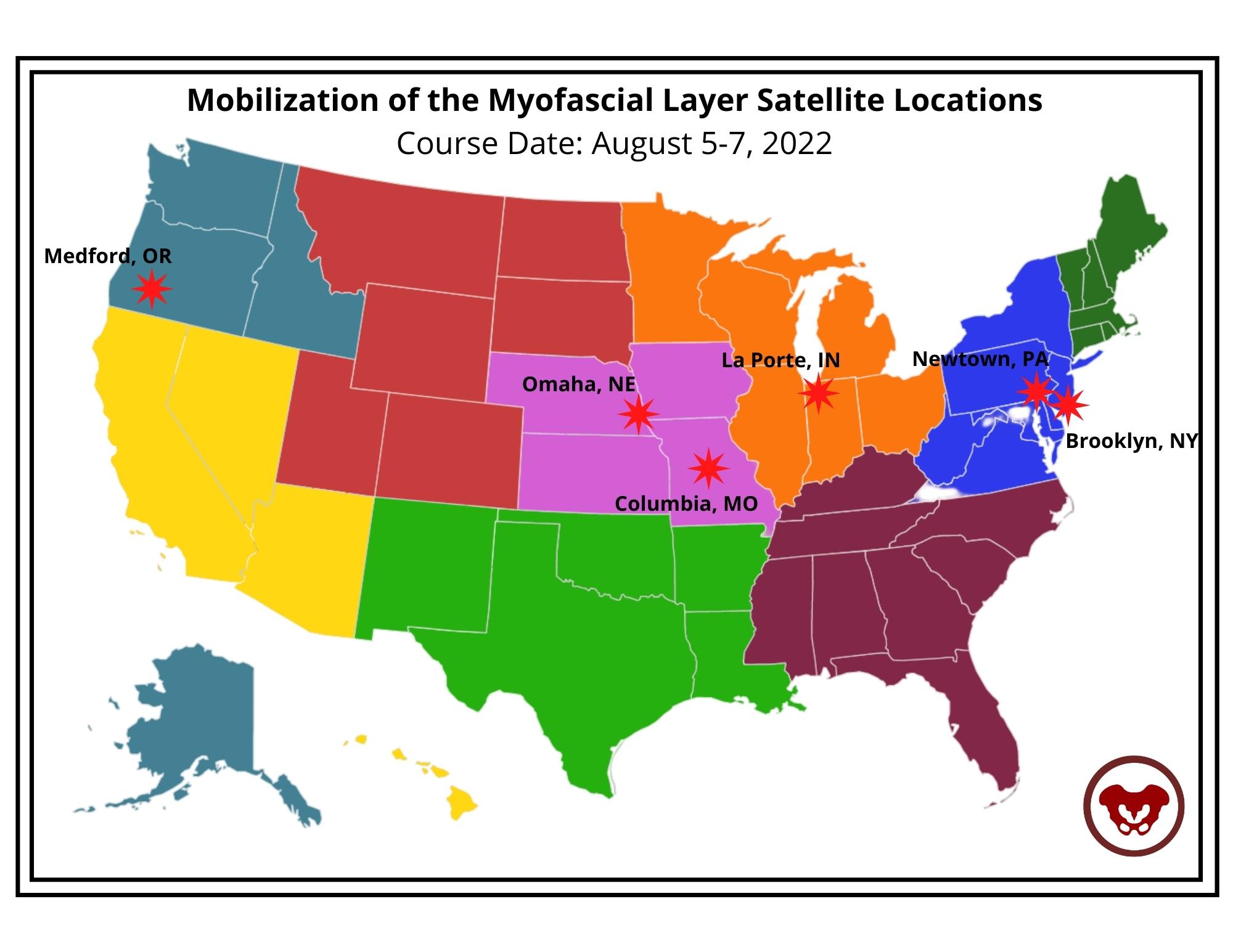
This week Ramona Horton sat down with Holly Tanner to discuss manual therapy and her course Mobilization of the Myofascial Layer: Pelvis and Lower Extremity. The following is an excerpt from her interview.
What do we really know about manual therapy? We have decent evidence that shows that asymmetry matters. The tenet of the myofascial course is an osteopathic tenet called ARTS:
- Asymmetry
- Restriction of Mobility
- Tissue Texture Changes
- Sensitivity
The whole myofascial course is designed around looking for ARTS. When you find the asymmetry within the myofascial system then that’s where you direct your efforts and energy.
Often patients have already tried breathing, yoga, medication, etcetera – and it’s the manual therapy piece that they often have not had. It’s not that uncommon for me to be someone’s second or third therapist. Some patients may have tried some type of manual therapy but it was more things like ischemic compression where the problem was that the manual therapy was triggering nociception.
So in the myofascial course, we start with ARTS but we also have an idea where we flip ARTS on its head and we go to STAR. In STAR, you take sensitivity and put it at the top of your list. That becomes the highest portion in your paradigm. Then we use simple techniques that are not non-nociceptive. Indirect technique versus direct technique, such as something as simple as positional inhibition.
The whole idea of the myofascial course is to teach people to think and problem solve. Then have a very broad spectrum way of you find an inner articular issue where this joint is moving and this one is not. Learn to not chase the booboo. Just because it hurts on the right doesn’t mean that you’re going to treat the right. It might hurt on the right because there is a hypo-mobility on the left. Let’s treat where the brain is protecting the tissue, and holding, and guarding the tissue. Trust in the belief that the body is a self-righting mechanism. The body will then normalize itself.
In manual therapy, our job is to get the body moving like it's supposed to. It’s not to fix the ‘booboo.’ The issue is not in the tissue. If the tissue is tight, it’s tight because the brain is keeping it that way. The way I teach manual therapy is the fascial system gives us access to the nervous system. By utilizing the fascial system in a non-nociceptive manner, what we’re really doing is just having a conversation with the brain. We’re not fixing the tissue. That’s the whole premise of the course - to get people to understand and change their thinking and their paradigm to ask what the brain is protecting and utilizing the fascial system.
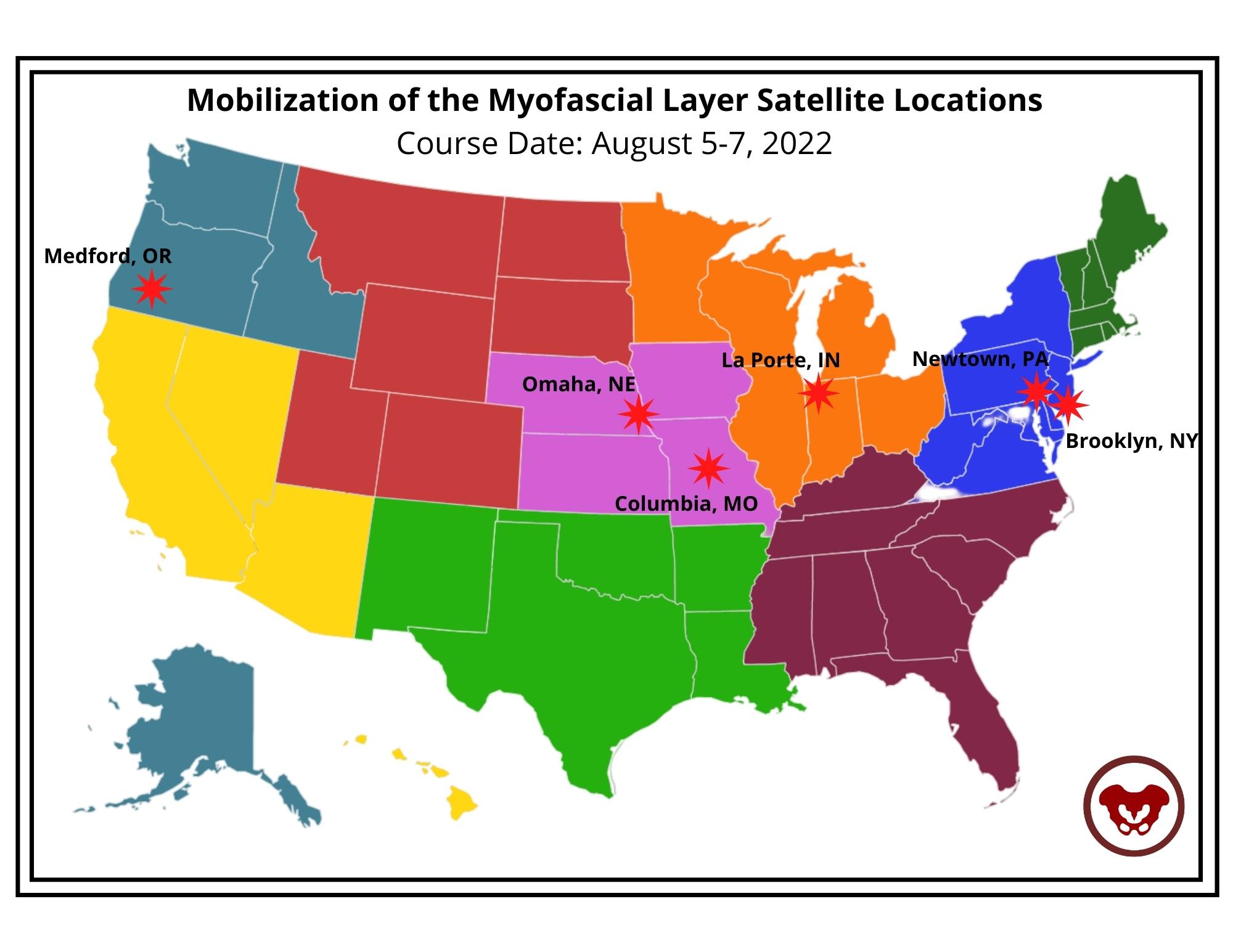
Course Date: August 5-7, 2022
- Self-Hosted - for groups of at least 2 qualified practitioners.
Congratulations to Dr. Mia Fine (they/she) for achieving their Ph.D. in Clinical Sexology and on their book titled 'From Unwanted Pain to Sexual Pleasure: Clinical Strategies for Inclusive Care for Patients with Pelvic Floor Pain' for their dissertation doctoral project.
Dr. Fine was gracious enough to share a draft of their dissertation with Herman & Wallace and to answer a couple of questions about how this impacts their practice and what they hope other practitioners will take away from their book and course Sexual Interviewing for Pelvic Health Therapists.
Mia's course is for the pelvic rehab therapist and others in the medical profession who work with patients experiencing pelvic pain, pelvic floor hypertonicity, and other pelvic floor concerns and would like to learn applicable skills from the sex therapist's clinical toolkit. The next course date for Sexual Interviewing for Pelvic Health Therapists is August 13-14,

How does Trauma-Informed Care apply to the skills that you teach in your Sexual Interviewing course?
When I utilize the term ‘trauma-informed’ I am referring to therapeutic work that communicates expectations clearly (including prioritizing people’s access needs with this communication), invites clients awareness of their own agency, and is upfront about my scope of practice and my therapeutic approach, offers mutuality in inviting of questions and ongoing conversation about our work together, awareness that an individual can end therapy at any time, and share information at any time in our therapeutic space.
The modalities I utilize when working with clients who have experienced trauma include Eye Movement Desensitization and Reprocessing (EMDR), Polyvagal Theory, Somatics, and Developmental Theory. While I integrate various theories and modalities into my work with clients, the methods above are empirical in their data to support healing from trauma wounds.
Trauma-informed means humility regarding cultural, racial, gender, sexual, and other minority experiences. I will not know all of the things but I will do my best to self-educate and not leave that responsibility to my clients. When I make a mistake I will appropriately, directly, and compassionately apologize for the harm I caused and invite opportunity for repair should the client be interested. Trauma-informed means collaboration in exploring therapy together, co-creating a space that feels safer to the client and checking in with them when I notice non-verbal cues that indicate activation, honoring a client’s pacing, and bringing awareness to the reality that as a therapist I hold power and while I don’t know a person’s full story there is always the potential for me to unintentionally activate a client so to share this possibility with clients and continuously check in about how our therapy is working for them. I keep my client’s well-being at the forefront of our work and I center their needs at all times while maintaining boundaries that keep everyone as safe and secure as possible.
It is up to us as trauma-informed and inclusive providers to explore a person’s experience of pain by asking questions about onset, process, location, and impact, in addition to offering psychoeducation about anatomy, physiology (arousal, interest, desire), and self-regulation. This must be done alongside commitment to our patient’s co-regulation, normalization, and informed consent concerning the therapeutic process—all of which are needed for comprehensive trauma-informed care.
Can you explain how expanding what 'normal' is to practitioners can impact the patients and clients that they work with?
Sex is not supposed to be painful. How many people have come to me having had painful sexual intercourse for years and reported “pushing through”? The first time having intercourse does not necessarily have to be painful, but when our cultural narratives tell us “the first time having sex is painful for everyone” we end up ignoring the signals our bodies are offering because we have convinced ourselves that the pain is both okay and normal. The “pushing through” is a reflection of misogyny: people assume the first experiences people have with penetration are supposed to be painful. How is this misogynistic? Well, who benefits from a person “pushing through” pain? The partner with the penis. Important to note here as well is that enthusiastic consent is ableist and ignores the mind-body connection because it does not take into account masking or fawning which are common experiences for many.
A quarter of people who experience sexual health concerns share this with their providers. Why such a small fraction? Fear. Fear of embarrassment and shame. Fear that there is something “abnormal” about them that mutates into the shame humans tend to experience in response. Fear that the concern won’t be held or taken seriously by their provider. Fear that, if it is addressed, will be at such a high financial cost that the treatment will be unaffordable. Fear that there’s not enough time or that they won’t be taken seriously. Fear of exclusivity, feeling othered, or misunderstood by their provider. Fear of the unknown because the reality is that people are afraid of what we don’t understand.
One of the major cultural issues we have in the US is the perpetuation of sexual stigma which is largely associated with a lack of comprehensive sex education. People don’t have access to basic information about their own bodies which influences our beliefs about sex, pleasure, agency, communication, and self-awareness. Sex education should be a birthright, and yet we are so far behind the curve that it sometimes feels impossible to break down the barriers.
When I first started in this career it would often take clients months of working with me to feel comfortable enough to talk about where they felt pain during sex, but in developing the tools to co-create safety in our therapeutic relationship and the skills to ask the important questions with compassion and patience, I learned how to better hold space for healing.
Patients don’t often know what information is important for them to share with us (which is why offering visuals of where the pain is located is important). How could they know what information is important to offer when mental and sexual health are so deeply stigmatized? The stress of shame and embarrassment that people feel about their bodies is emotional pain that further exacerbates the physical pain that they came to therapy to address in the first place. It’s a terrible and self-perpetuating cycle.
I teach people the difference between a vulva and a vagina one thousand times a year. If a client does not know the terminology for labia, vulva, vagina, and clitoris, how are they supposed to know when their sexual health is of concern? If a person enters sex therapy with “sexual pain” but is unable to distinguish the difference between their labia and vagina (that they are different body parts, where they are located, and what their functions are) we cannot expect them to accurately articulate the location of pain or comprehend potential solutions. “What is your hygiene process when cleaning your vulva?” may activate the fight or flight response in clients if they do not know what their vulva is or that there could be a good hygiene process, in addition to the shame of not knowing. How are they supposed to know where or to whom they may ask for help?
An online search for “anatomical vulva”, “pelvic floor pain”, “vaginismus treatment” and 99% of the images and figures you will see are those of hairless, slender bodies with white/light skin and small labia. Racism and white supremacy are present everywhere. The anatomical depictions of vulvas are of white bodies, the people modeling in vaginismus treatment advertisements are white, and the language is geared toward and written for white people. I was intentional about not featuring white vulvas in this book because white bodies should not be the default of what is mainstream. This lack of diversity in skin tone and variation of body type is another reflection of racism called “colorism”. White and light skin bodies are viewed as more ‘normal’ and when we continue to center white bodies in visuals “because that is what is available” we perpetuate white supremacy. One goal is to disrupt the idea and practice of whiteness as the default. This is what it means to practice anti-racism and attempt to divorce ourselves from white supremacy.
The impact of shame shows up in the pervasive erotophobia rampant in our society. Erotophobia can be broadly defined as a “fear of sex” or more specifically a “fear of intercourse”. When erotophobia is judgment as a result of societal shame and stigma, we can navigate it by deconstructing the etiology and impact of messages received; when it is a result of a mental health condition such as Obsessive Compulsive Disorder (OCD) or Post Traumatic Stress Disorder (PTSD), we do deep trauma and/or anxiety/exposure work. Because of the vast impact of shame, people fear sharing sensitive information about themselves with others, including therapists who are trained to help them. Often, therapists are untrained in sexual health which also can contribute to erotophobia and shame. When therapists have not done their own work on sexuality, and remain untrained in these areas, they may be afraid to discuss sex with their clients which reinforces the belief that topics regarding sex are shameful.
When people do not have the language to articulate what is happening in their body, as significant as the pain or discomfort might be, talking about sex with a provider is often the last item on a long list of concerns they bring to a medical appointment. Symptoms of sexual pain may be hidden by other “more pressing” concerns such as anxiety, depression, PTSD, or sleep issues. While these are of course vital for a medical provider to know, having 20 minute appointments with a physician who will prioritize the “presenting concern” that they came in to seek treatment for leaves very little time to discuss unwanted sexual pain. After 15-20 minutes of a medical appointment (if it goes well), a patient might feel comfortable enough to bring up their sexual concern, but this might leave 1 minute for it to be acknowledged and no time to conduct a comprehensive assessment or develop an intentional plan. We call these last-minute oh-by-the-way’s “door-knobbing” for a reason. This is a call for medical clinics to have training in sexual health so they can create intake documentation that explores clients’ sexual health and ask the questions that are vital to gather necessary information ahead of time.
In the same way that people lack language and anatomic understanding, people also lack awareness of the mind-body relationship. Due to the ableist sex-negative culture in which we live, people are often not taught to have knowledge of or listen to our own body. We’re not taught that pain is a signal from the body telling us that something’s wrong.