Putting on My Neuro “Brain”
Erica Vitek, MOT, OTR, BCB-PMD, PRPC is the author and instructor of Neurologic Conditions and Pelvic Floor Rehab, a new course coming to Grand Rapids, MI and Philadelphia, PA. This post is the next in her series on creating a course about neurologic conditions and pelvic rehabilititation.
Being a clinician, as we evaluate and treat people with pelvic health conditions, we typically take all systems of the body into account. We take the problem presented to us by the client and we examine, from all angles, how we might go about advice and treatment to best achieve their goals in alleviating the problem. We do a full review of medical history and pharmacology. We examine our client in-depth from a musculoskeletal perspective. We look at psychological contributions to the problem they are facing. We can look at their lifestyle and have them make a detailed diary to help us analyze their bladder, bowel, fluid intake and dietary habits. Do we also always include a look at the neurological components? Do we know what we are looking for? What are the best tools we can have in our toolbox as clinicians to look at our client’s problem through a “neuro brain”?
 In writing each lecture of this course, I have had to step back each time I am developing a new concept and look at it with in-depth thought and contemplation about how I will use this in the clinic to assess my client’s concerns using a neuro-based approach. Taking the concepts and facts about the musculoskeletal system that we know well and then taking a look at the neurological systems contributions and relationship to that dysfunction can be challenging. The main reason for this challenge is that neuro system dysfunction is many times hard explain, presents with inconsistent or changing symptoms, may have motor or sensory deficits together or by themselves, may radiate to different locations than where the true dysfunction is located, and may have developed into central sensitization causing a hypervigilance to typically non-painful stimuli.
In writing each lecture of this course, I have had to step back each time I am developing a new concept and look at it with in-depth thought and contemplation about how I will use this in the clinic to assess my client’s concerns using a neuro-based approach. Taking the concepts and facts about the musculoskeletal system that we know well and then taking a look at the neurological systems contributions and relationship to that dysfunction can be challenging. The main reason for this challenge is that neuro system dysfunction is many times hard explain, presents with inconsistent or changing symptoms, may have motor or sensory deficits together or by themselves, may radiate to different locations than where the true dysfunction is located, and may have developed into central sensitization causing a hypervigilance to typically non-painful stimuli.
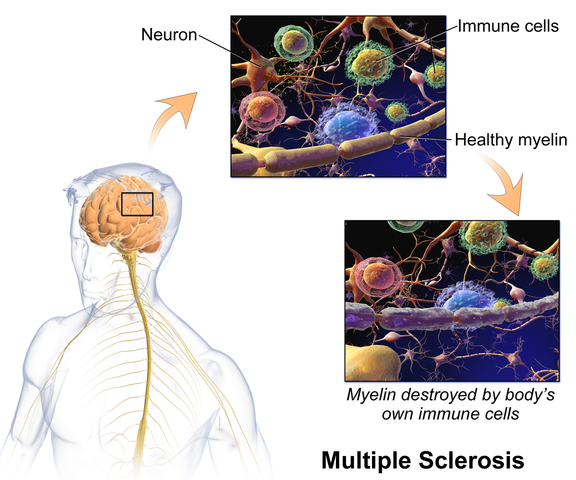
In brain storming our ideas for course creation, much was said about thinking back to college or other continuing education courses and “learning a little about a lot of things neuro” but not the in-depth knowledge one might want to have when focusing their attention on specific neurodegenerative conditions such as Parkinson disease, demyelinating diseases such as Multiple Sclerosis, injury to the brain due to cerebral vascular accident or incomplete or complete spinal cord injury.
As I progress deep into the development of this course, I have my “neuro brain” on and a persistent focus set on providing clinicians with as much in-depth information on neurological contributions to pelvic floor function and dysfunction. I want clinicians to walk away from this course feeling confident that through evaluation of a client that has been diagnosed with Parkinson disease, Multiple Sclerosis or suffered a spinal cord injury, they would have the tools to develop an in-depth treatment plan that would provide these clients with the best results possible to improve their quality of life. I also want clinicians to have the confidence to market themselves to their local neurologists. This is an entirely new avenue for developing a referral base in pelvic health work. Many times for clients who have chronic neurological conditions, the problem list is long and bladder, bowel and sexual health concerns might not even be broached within the very short physician appointment times. We can give our neurologists new treatments to be confident in and excited about to improve their patient’s quality of life!
By accepting you will be accessing a service provided by a third-party external to https://hermanwallace.com/






































