A Weekend of Transformation
Let me start this plog (picture/blog?) by saying it had been almost 2 years since Nari Clemons and I taught Boundaries, Self Care, and Meditation for the first time. Nari had some amazing ideas to change some of the course material to reflect more of our hearts’ intention for personal reflection and transformative change. We were excited and nervous to see how our second run of this material would be received. We were also profoundly aware of how the (at times painful) events in our lives that led up to the development of the course have molded and shaped us into much healthier versions of ourselves. We wanted to share a bit about what we have learned and how it has changed us.
We met up in beautiful San Diego on Thursday. Because this course was Saturday to Mononday we had an added bonus of extra time to spend together. We decided to spend our time practicing what we talk about in class.
1. Get out in nature:
Tory Pines State Park provided much needed rejuvination. Ahh sea air.
2. Self-care is mandatory:
We spent Friday relaxing at a beautiful resort in Del Mar. We are learning we don’t need to justify or feel bad about caring for ourselves. It’s necessary and important. We are responsible for meeting our own needs and for refueling ourselves when we provide care for others.
3. Get out of your comfort zone:
The robes we got from the resort were super cozy and it was chilly on the beach, so why not walk the beach in a robe? We laughed at ourselves and others laughed at us and with us. But we were comfy and warm.
4. Do the work when it is time to do the work:
Instead of thinking and talking about the course all day we committed ourselves to being in the moment. When it came time to discuss the details of the next three days, a plan came together with relative ease. This is us working at the resort.
5. Challenges can change your perspective. And a change in perspective can help you with challenges:
This is a (terrible, sorry) picture of us interrupting our morning run to climb a tree. It was a fun challenge and gave us an interesting perspective on our day.
A little more about the course. Woah. The people who showed up came with open minds and hearts, ready and ripe for change. We had powerful times of sharing, listening, learning, and supporting. Meditation and yoga and a healing, honest and real atmosphere brought about transformation in the most beautiful awe-inspiring way. We were profoundly moved. The changes Nari suggested were PERFECT and I was grateful for her innovations. We were all pretty much out of our comfort zones, but that is where change happens.
In the words of one student, “This course couldn’t have come at a more appropriate time because I was in major burnout. I was becoming an unhappy person both professionally and personally. I needed to make a change. Now I am leaving this course empowered to care for myself so I can help patients in a healthy way and enjoy my job again. I am walking away from this course with so many valuable strategies and also feel so much more relaxed and hopeful”
6. Be silly sometimes: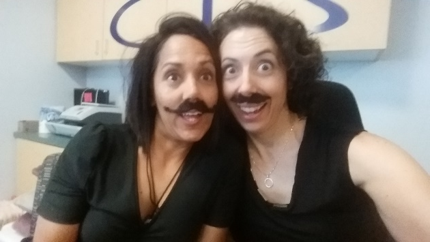
Laugh a lot. Especially at work. Play jokes, have fun. You know what they say about all work and no play. Play.
7. At the end of the day Shake it off (and use pain science as needed):
Our last day we took a run to the beach. When crossing a rail line I tripped and bashed the HECK out of my lower leg. Since I could still run I repeated the mantra “Hurt not harm!!” (which we discuss in class) with great vigor until the throbbing subsided, and we enjoyed a beautiful sunset and the conclusion of our time in San Diego.
Last words of Wisdom:
Gratitude can change us in powerful ways.
A huge and heart felt thank you to Herman & Wallace, our host site, and for each and every participant. We couldn’t do what we do without you and for this we are eternally grateful.
Thank you. Thank you. Thank you.

Herman & Wallace is excited to announce an upcoming course on pelvic rehab for the gender diverse patient, written and instructed by Dr. Laura Meihofer, DPT, ATC. As Dr. Meihofer indicated in a recent blog, "[t]he number of individuals who identify as transgender is growing each year. The Williams Institute estimated in 2016 that 0.6% of the U.S. population or roughly 1.4 million people identified as transgender (Flores, 2016)... With the rise of individuals who identify as transgender, gender non-binary and intersex, healthcare professionals have equally seen an influx of patients who require care throughout their discovery and transition."
The new course from Dr. Meihofer is called "Gender Diversity and Pelvic Health: Comprehensive Care for Transgender Men and Women", and it will be debuting on May 29-31, 2020 in Livingston, NJ.
Dr. Meihofer was kind enough to share some thoughts about the new course, her practice, and herself with The Pelvic Rehab Report. Thank you, Laura!
Tell us about yourself, Laura!
My name is Laura Meihofer and I’ve been a physical therapist for 7 years. I work at Mayo Clinic and I see patients throughout the gender spectrum who most commonly struggle with pelvic floor dysfunctions relating to overactive muscles such as: chronic and acute pelvic pain, urinary frequency/urgency/incontinence/hesitancy, constipation, pain with intercourse, low back and hip pain.
 What can you tell us about your new course, "Gender Diversity and Pelvic Health"?
What can you tell us about your new course, "Gender Diversity and Pelvic Health"?
Currently there are roughly 1.25 million transgender identified individuals in the United States and this number is growing. This course will help to dispel the idea of “other” when treating this demographic and demonstrate how much sameness there is when treating pelvic floor dysfunction.
These skills will greatly benefit any practice as this population is so underserved, they are looking for allies that are not just nice but competent. When you are able to successfully treat gender diverse patients, they spread the word about the great care they received and you now have a strong referral base. Taking this course opens up a whole new referral base of amazing people.
This course will not only feature videos from thought leaders in the field but will also highlight testimonials from patients and caregivers who have undergone their own gender transitions.
What essential skills does your course add to a practitioner’s toolkit?
I think the most important technique that attendees will learn will be how to assess a trans women and trans man after they have undergoing genital reconstruction surgery. Attendees will gain competence in the care of the gender diverse patient at any stage during their gender transition.
What was your inspiration to create this course for trans-identified patients?
Working at a major medical institution, I found that it was difficult finding providers in a patient’s area that were competent in care of a transgender patient. As I talked more and more with various physical therapists I realized they were thirsty for knowledge on how to serve these individuals. So I created the course!
What prepared you to create this course?
The most important thing I have done for this course is treat hundreds of patients who are trans identified throughout their gender journey. This allowed me to not only see all the medical interventions they went through but also to hear their personal journey of transition. These experiences expanded my empathy for what they go through and inspired me to search within myself on how I can be better for them. This desire to improve opened a creative well inside of me from which this course grew.
Discuss the effect conditions covered in your course have on a patient’s quality of life, your experience treating patients with this condition, and how their quality of life has increase after successful treatment.
Individuals who identify as transgender suffer from pelvic floor dysfunction just like our cis gender folks. There is no current data to capture the prevalence of pelvic floor issues in this specific population to date, however there is research to support the overall lack of care these individuals receive. Based on the results from the U.S. Transgender Survey which surveyed 28,000 respondents, the numbers in the health care field were staggering.
33% of respondents had at LEAST one negative experience with a health care provider in the last year due to being transgender. Negative experiences were qualified as verbal harassment, refusal of treatment or having to teach the health care provider about transgender people to receive appropriate care. 23% of respondents did not see a doctor when they needed to due to fear of being mistreated as a transgender person.
This course aims has two primary aims:
1) Educate providers on the unique concerns that transgender individuals experience related to hormone replacement and surgical techniques.
2) Equip attendees to provide competent care for this demographic
Join Dr. Meihofer for Gender Diversity and Pelvic Health this May 29-31, 2020 in Livingston, NJ!
Aparna Rajagopal, PT, MHS is the lead therapist at Henry Ford Macomb Hospital's pelvic dysfunction program, where she treats pelvic rehab patients and consults with the sports therapy team. Her interests in treating peripartum patients and athletes allowed her to recognize the role that breathing plays in pelvic dysfunction. She has just joined the Herman & Wallace faculty and co-authored the new course, "Breathing and the Diaphragm: Pelvic and Orthopedic Therapists", which helps clinicians understand breathing mechanics and their relationship to the pelvic floor.
Aparna was kind enough to introduce herself to us here on The Pelvic Rehab Report.
 Thank you for your time Aparna! To start, tell us a little bit about yourself.
Thank you for your time Aparna! To start, tell us a little bit about yourself.
My name is Aparna. I’ve been a physical therapist for 22 years. About 16 years ago I switched focus from orthopedics to treating pregnancy and postpartum patients and that’s where my initial interest in pelvic care started. In 2006 following my pregnancy and birth of my daughter, my interest in pelvic care grew with my special interest becoming pelvic pain.
I teach and mentor the pelvic health therapists within the fairly large hospital system that I work at and collaborate with our spine center team and our sports team.
What can you tell us about this new breathing course that is not mentioned in the “course description” and “objectives” that are posted online?
Physical therapy has evolved and continues to evolve as we speak. Regional inter dependence, wherein the different systems interplay, and one structure influences another, is fascinating. No longer is the body considered and treated as independent fragmented pieces. The ‘core’ with the contribution of the Diaphragm and the pelvic floor is so much more than just the Transverse Abdominis and the Multifidus working together. Fascial restrictions of the lower abdomen and the pelvis can influence how the low back feels, thoracic stiffness can influence the interplay between the various abdominal muscles by way on their insertion into the lower ribs, musculo- skeletal pain and postural deviations can stem from incorrect breathing patterns etc.
Normal breathing rate is about 10 times every minute. Breathing incorrectly reinforces wrong movement patterns tens of thousand times a day with negative consequences on the musculoskeletal system.
This course offers an in depth look at the diaphragm from the perspective of both orthopedic and pelvic therapists and attempts to tie in the diaphragm to the thoracic spine, the ribs, the pelvic floor, the core, posture and finally the athlete.
What essential skills does the breath course add to a practitioner’s toolkit?
The practitioner will walk away with the ability to view the patient as a “whole”. It offers a different perspective on neck and back pain, posture/ alignment along with the ability to assess for and connect breathing and the diaphragm to stability/ the core, continence issues and the Autonomic Nervous System.
As therapists we already do a great job of addressing strength issues, assessing and correcting posture, mobilizing etc. You can add to your treatment options by learning how the diaphragm works in concert with other muscles (especially the abdominals) and systems, identifying breathing pattern dysfunctions and postures, and movement patterns which may be linked to breathing pattern dysfunctions. This understanding is beneficial for both orthopedic and pelvic patients.
What inspired you to create this course? What void does this new offering fill?
I have used breathing and evaluation of the diaphragm as a part of pelvic care for several years now. As the mentor for the pelvic program at my hospital, and as a part of the spine team and sports team, I work with pelvic therapists, orthopedic therapists, manual certified therapists, and sports certified therapists. Through my interactions I have come to realize that although many of the therapists are aware that the Diaphragm and breathing are important, they are unsure of how to assess for dysfunctions and address those dysfunctions. I initially started conducting classes within the hospital system. At the same time Leeann who is a sports certified therapist and holds a manual therapy certificate and I started collaborating on our patients. Using a combination of her knowledge and effective manual techniques with my pelvic care and breathing techniques we realized that along with my pelvic patients; our back and neck patients, and her sports patients were all benefitting from this combined approach. We realized along the way that we had information worth sharing with our colleagues that would benefit them in treating their patients, and started classes within the hospital system and that is how this class was born!
What was your process like creating this course?
As a trained pelvic therapist, I have incorporated and used breath and the diaphragm in my treatment for over a decade. Leeann and I have created this course using a combination of our clinical experiences, our education in our respective chosen paths of patient care, and most importantly using recent and relevant research articles from journals to guide us extensively in creating this course.
Breathing and the Diaphragm: Pelvic and Orthopedic Therapists is a new course being offered next March 27-29, 2020 in Sterling Heights, MI, and again on December 11-13, 2020 in Princeton, NJ. It is created and taught by Aparna Rajagopal, PT, MHS and Leeann Taptich, PT, DPT. Come learn how the diaphragm and breathing can affect core and postural stability through intra-abdominal pressure changes. As an integrated approach, the course looks at structures from the glottis and the cervical region to the pelvic floor and helps in understanding a multi component system that works together.
Part 3: Carefully Choosing to Say Yes or No (or The Summer that Almost Wasn’t)
*Disclaimer: this essay is meant to be read in a voice of complete transparency and humility.
 Two summers ago I was anxiously anticipating a break. I was wrapping up home school for my girls and had scheduled some down time from writing my contribution to “Boundaries, Meditation and Self-Care” when I got the call…
Two summers ago I was anxiously anticipating a break. I was wrapping up home school for my girls and had scheduled some down time from writing my contribution to “Boundaries, Meditation and Self-Care” when I got the call…
Rewind a bit. Two years prior I also got a call. Would I be interested in writing a chapter in a Urology textbook on alternative care for pelvic pain conditions…edited by and partnering with a big name in pelvic floor rehab? Oh yes indeed I would! I have always dreamed of seeing my name in print. Was I scared out of my mind? Heck yes! I was working 20 hours a week, part time home schooling my girls and teaching for Herman & Wallace. I had one day a week to myself for cleaning, errands, the occasional book reading or interacting with friends. I decided I could spend my next year of Fridays researching, writing and editing said chapter. Oh, I also started therapy for the anxiety increase that came with the project. My therapist suggested I hire help with house cleaning, which I did. She also suggested meditation, mindfulness and using essential oils. I opted not to enact these suggestions. It was a crazy year, but I learned a ton and was proud of my contribution to the publication.
In the brief time that I caught my breath from the book chapter, I was invited to be part of the team writing the Pelvic Floor Capstone course. What an honor! I had always wanted to try writing a course and this would be a perfect opportunity to collaborate with others on such a big project. I committed, worsening my anxiety with heart palpitations which escalated to a level that required medication. My Fridays and evenings were again occupied for quite some time. Luckily, I still had the cleaning help and the therapist which were really just the skinniest strings that were maintaining my sanity.
While teaching our first Capstone class, although both of us were struggling with burnout, Nari Clemons and I had a moment of euphoria, seeing everything come together and watching students learn. We decided we would design and write another course and put together an outline and a plan for Boundaries, Self-Care and Meditation.
I think you might be getting a picture of my prior lifestyle. If there was time, I filled it. If there was an opportunity, I took it. If I did something once, I could do it again. But applying the concepts of our boundaries course to myself changed everything.
Nari and I knew we were burning out and needed change. I have always had anxiety, but it had escalated to the point of requiring both therapy and medication. I was giving my all, my best, to everyone else and my family got my scrappy leftovers, the worse of me. I had been functioning in these patterns my whole life and had no idea how to get off the hamster wheel.
As we developed Boundaries, Meditation and Self Care I became my own research study, incorporating the material we would be teaching into my own life. I finally started setting priorities and boundaries that helped put my family first and give them the best of me. I said no to a variety of opportunities that I then delegated to colleagues who were delighted to step up. I started meditating, practicing mindfulness and using essential oils as part of my self-care as my therapist suggested a year ago. I even enrolled my kids in full time school for the upcoming year. I was feeling so much better!
So when the next call came, I was prepared.
The editor and famous pelvic floor PT I had worked with on the book chapter was in need of an editor for an article that was going to be published in a medical journal. There was a lot of editing that needed to be done and time was of the essence. My contribution as editor would list me as a co-author. How many of you also dream of seeing your name attached to an article in a peer reviewed medical journal? Because of what I had learned through therapy and practiced with meditation I had the ability to pause, reflect, and make an informed choice that considered how this opportunity lined up with my priorities. I replied with much gratitude for the offer, but this time I said no. It was difficult to say no, and I had to work through some regret, but in the end I made the right choice and we had a great summer.
Life is funny sometimes and lessons in humility are plentiful. Back track again to when the urology text came out a few years ago. I excitedly ordered a print copy. When I opened to the chapter which I contributed, I discovered another person’s name had accidently been printed where mine should have been. The mistake was corrected for the ebooks but more paper copies were not printed. I may never see my name in print, but the Summer That Almost Wasn’t taught me that there are more important things in life.
If you find yourself struggling with boundaries, saying no, and prioritizing the things that are important to you personally and as a therapist, know that you are not alone, and you can get support. Consider talking with your supervisor, a counselor, reading a good book on the subject or taking Boundaries, Meditation and Self Care, a course offering through Herman and Wallace that was designed to help pelvic health professionals stay healthy and inspired while equipping therapists with new tools to share with their patients.
We hope you will join us for Boundaries, Meditation and Self Care this November 9-11, 2019 in San Diego, CA.
We are thrilled to announce that Herman and Wallace instructor, Carolyn McManus, MPT, will co-present an educational session with internationally recognized pain researcher Etienne Vachon-Pressseau, PhD at APTA’s NEXT meeting in Chicago on June 13. Dr. Vachon-Presseau is an assistant professor at the Alan Edwards Centre for Research on Pain at McGill University and has led pioneering research into stress-associated brain changes in patients with persistent pain.
 In a presentation entitled, When Stress Complicates Care for Your Patient in Pain: Evidence-Based Mechanisms and Treatment, Dr. Vachon-Presseau will discuss the latest research and theory illuminating the role of stress in the maladaptive neuroplastic brain changes observed in patients with chronic pain. Carolyn will discuss direct clinical applications of this marterial and highlight research on the role of mindfulness in the self-regulation of stress and pain. She will share a practical model for integrating mindfulness into physical therapy for the treatment of persistent pain conditions.
In a presentation entitled, When Stress Complicates Care for Your Patient in Pain: Evidence-Based Mechanisms and Treatment, Dr. Vachon-Presseau will discuss the latest research and theory illuminating the role of stress in the maladaptive neuroplastic brain changes observed in patients with chronic pain. Carolyn will discuss direct clinical applications of this marterial and highlight research on the role of mindfulness in the self-regulation of stress and pain. She will share a practical model for integrating mindfulness into physical therapy for the treatment of persistent pain conditions.
We are excited that Carolyn has been offered this honor to co-present at NEXT with a world renown researcher in the field of pain and contribute her insights from an over 30-year career specializing in mindfulness and pain. She will offer her popular course, Mindfulness-Based Pain Treatment, in Portland OR, July 27 and 28 and in Houston TX, October 26 and 27. We recommend these unique opportunities to train with Carolyn, a nationally recognized leader trailblazing the successful applications of mindfulness into the field of physical therapy. Hope to see you there!
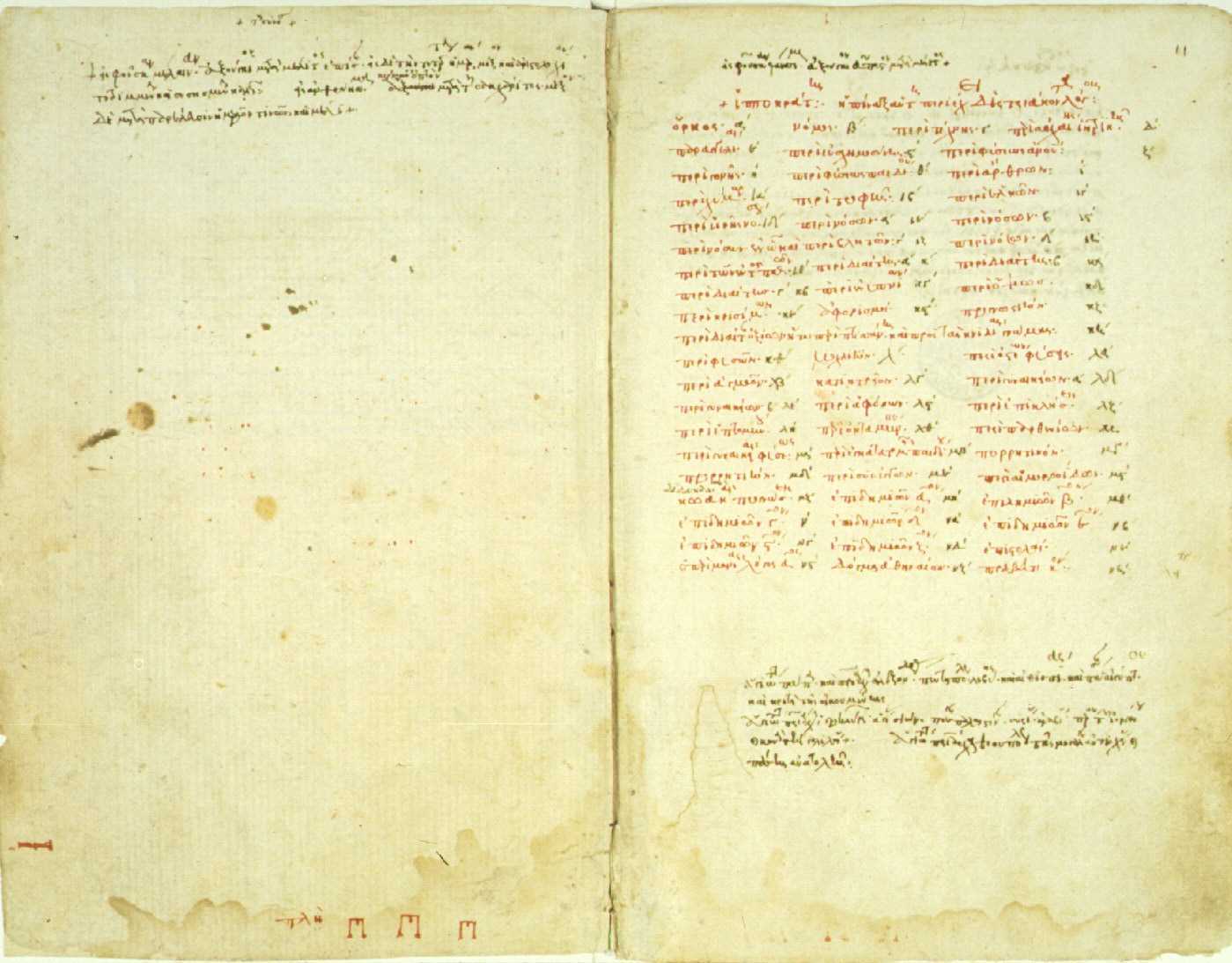
The need for artful incorporation of Hippocrates’ wisdom is great in today’s healthcare landscape. As conversation of nutrition broadens into multidisciplinary fields, his wisdom resonates: first, “we must make a habit of two things; to help; or at least to do no harm”. Second, we must modernize the ancient adage: “let food be thy medicine and let medicine be thy food”. And finally, health care providers will do well to be guided by his insight that “all disease starts in the gut”. Hippocrates’ keen observations during his era, modern science is confirming, hold keys to the plight of our times as we seek to find better ways to manage complex conditions commonly encountered in pelvic rehab practice settings and beyond.
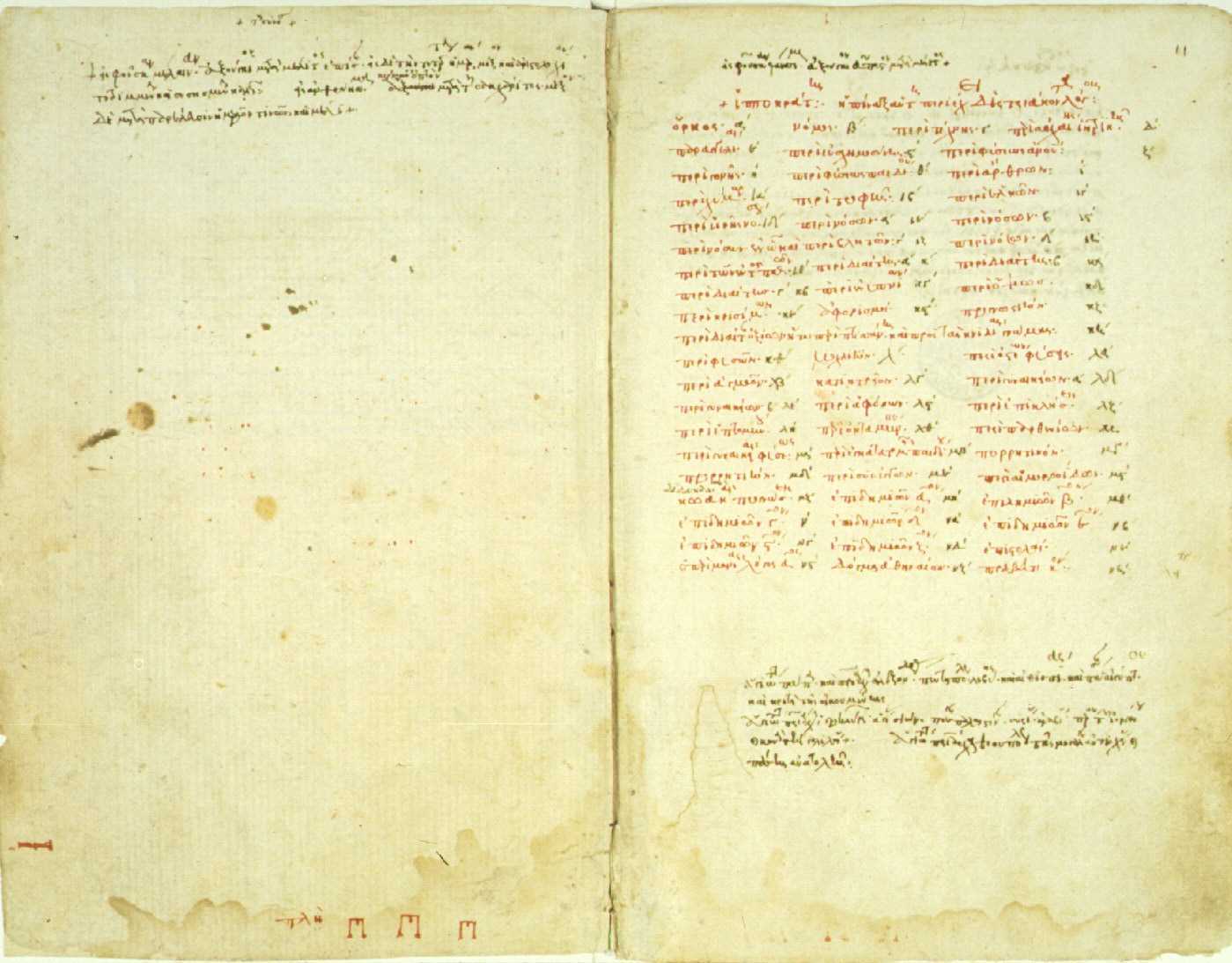 Considered some of the oldest writings on medicine, the “Hippocratic Corpus” is a collection of more than 60 medical books attributed directly and indirectly to Hippocrates himself who lived from approximately 460 to 377 BCE.2 According to the Corpus, Hippocratic approach recommends physical exercise and a “healthy diet” as a remedy for most ailments - with plants being prized for their healing properties. If -during illness states - employment of nourishment and movement strategies fail, then medicinal considerations could be made. This logos - the ancient Greek word for logic - is the art of reason whose relevance today is perhaps more poignant than in ancient times.
Considered some of the oldest writings on medicine, the “Hippocratic Corpus” is a collection of more than 60 medical books attributed directly and indirectly to Hippocrates himself who lived from approximately 460 to 377 BCE.2 According to the Corpus, Hippocratic approach recommends physical exercise and a “healthy diet” as a remedy for most ailments - with plants being prized for their healing properties. If -during illness states - employment of nourishment and movement strategies fail, then medicinal considerations could be made. This logos - the ancient Greek word for logic - is the art of reason whose relevance today is perhaps more poignant than in ancient times.
In this logos, by making a habit of helping, or at the very least, not harming, it becomes particularly important to identify the unique nutritional landscape that surrounds us. The Hippocratic Oath emanates reason. It is logical that we would seek to practice (healthcare) to the best of our ability, share knowledge with other providers, employ sympathy, compassion and understanding, and help in disease prevention whenever possible.2 One of the most helpful and powerful aspects of rehabilitation is the gift of time we have for meaningful and instructional conversation with our clients. Our interactions with clients can and should address the realm of nutrition as it relates to the health of the mind and body. Because, after all - to help - is why many become health care providers in the first place.
Detailing a “healthy diet” in Hippocratic times was certainly simpler, as the uncontrolled variable of processed foods- as we know them- did not exist. Therefore, we reflect upon the quote: “let food be thy medicine and let medicine be thy food” and acknowledge that this modern food landscape is vastly different 1 than in ancient times. Compounding the issue, our standard logic for helping has gotten somewhat out of order. And both medicine and food carry meanings today reflective of modern times. The issues of poly-pharmacy and the tragedy of medically prescribed unintentional overdoses (or intolerances) remind us of our ‘medicine first’ mentality and the unfortunate reality that medicine is not the cure-all we so wish it could be. Further, not all ‘food’ today is food. Real food sustains and nourishes us. Real food can also heal. We need to celebrate real food for being real food, and champion it’s miraculous ability to support, heal, and transform the human condition.
Finally, health care providers will do well to be guided by Hippocratic insight that “all disease starts in the gut” and to logically extrapolate the opposite: much healing can begin in the gut. It is through this ancient concept that we can organize our modern science and begin to concretely and intentionally help heal ourselves and others from the inside out. Once we understand the key role of digestion and our gut on our health and well-being, the rest is pure logic. We simply need a map for navigation of these universal concepts to go along with our renewed appreciation for the art of reason.
Let Nutrition Perspectives for the Pelvic Rehab Therapist help provide this map. Evolve your nutritional logos into a beautiful and nourishing framework by joining the hundreds of pelvic rehab therapists and other health care providers who have attended Nutrition Perspectives in Pelvic Rehab. Be inspired and empowered on your integrative journey. Live courses will be offered at three sites in 2019: March 1-3 in Arlington, VA, June 7-9 in Houston, TX, and October 11-13 in Tampa, FL!
Fardet, A., Rock, E., Bassama, J., Bohuon, P., Prabhasankar, P., Monteiro, C., . . . Achir, N. (2015). Current food classifications in epidemiological studies do not enable solid nutritional recommendations for preventing diet-related chronic diseases: the impact of food processing. Adv Nutr, 6(6), 629-638. doi:10.3945/an.115.008789
Biography.com https://www.biography.com/people/hippocrates-082216. Accessed January 11, 2019.
Faculty member Nari Clemons, PT, PRPC recently created a two-course series on the manual assessment and treatment of nerves. The two courses, Lumbar Nerve Manual Assessment and Treatment and Sacral Nerve Manual Assessment and Treatment, are a comprehensive look at the nervous system and the various nerve dysfunctions that can impact pelvic health. The Pelvic Rehab Report caught up with Nari to discuss these new courses and how they will benefit pelvic rehab practitioners.

What is "new" in our understanding of nerves? Are there any recent exciting studies that will be incorporated into this course?
The course is loaded with a potpourri of research regarding nerves and histological and morphological studies. There are some fascinating correlations we see with nerve restrictions, wherever they are in the body. Frequently the nerves are compressed in fascial tunnels or areas of muscular overlap, then the nerve, wherever the location, frequently has local vascular axonal change, which increases the diameter of the nerve and prohibits gliding without pain. This causes local guarding and protective mechanisms. Changing pressure on the nerve can change that axonal swelling and allow gliding without pain.
New pain theory also supports that much of pain perception is the body perceiving danger or injury to a nerve. By clearing up the path of the nerve and mobilizing it, we can decrease the body's perception of nerve entrapment and thus create change in pain levels.
What do you hope practitioners will get out of this series that they can't find anywhere else?
I hope they will leave the course able to treat the nerves of the region, which is essentially the transmission pathway for most pelvic pain. I don't know of other courses that have this emphasis.
You've recently split your nerve course in two. Why the split?
I didn't want this class to be a bunch of nerve theory without the manual intervention to make change. After running the labs in local study groups, we found it took more time for people's hands to learn the language, art, and techniques of nerve work. To truly do the work justice and for participants to have a firm grasp of the manual techniques without being rushed, we found it takes time, and I wanted to honor that, as well as treating enough of the related factors and anatomy to make real and lasting change for patients.
How did you decide to divide up content?
Basically, we divided them up by anatomical origin:
The lumbar course covers the nerves of the lumbar plexus, the abdominal wall when treating diastasis, and treatment of the inguinal canal (obturator nerve, femoral nerve, iliohypogastric, ilioinguinal, genitofemoral nerves). Also, the lumbar nerves have more effect in the anterior hip, anterior pelvis, and abdominal wall.
The sacral nerve course covers all the nerves of the sacral plexus (pudendal, sciatic, gluteal/cluneal, posterior femoral cutaneous, sciatic, and coccygeal nerves), as well as subtle issues in the sacral base and subtle coccyx derangement work as well as the relationship with the uterus and sacrum, to take pressure off the sacral plexus. The sacral nerves have more effect in the posterior and inferior pelvis and into the posterior leg and gluteals.
What are the main stories that either course tells?
Both courses tell the story of getting closer to the root of the pain to make more change in less time. Muscles generally just respond to the message the nerve is sending. Yet, by treating the nerve compression directly, we are getting much closer to the root of the issue and have more lasting results by changing the source of abnormal muscle tone. Rather than an intellectual exercise of discourse on nerves, we devote ourselves to the art of manual therapy to change the restrictions on the pathway of the nerve and in the nerve itself.
If someone went to the old nerve course, what's the next best step for them?
The first course was initially all the lumbar nerves with a dip into the pudendal nerve. They would want to take the sacral nerve course, as those nerves were not covered in the first round.
Anything else you would like to share about these courses?
Sure. Essentially, we will take each nerve and do the following:
- Thoroughly learn the path of the nerve
- Fascially clear the path of the nerve
- Manually lengthen supportive structures and tunnels that surround the nerve.
- Directly mobilize the nerve
- Glide the nerve
- Learn manual local regional integration techniques for the nerve after treatment
- Receive handouts for and practice home program for strengthening and increasing mobility in the path of the nerve
Join Nari at one of the following events to learn valuable evaluation and treatment techniques for sacral and lumbar nerves
Upcoming sacral nerve courses:
Sacral Nerve Manual Assessment and Treatment - Winfield, IL
Oct 11, 2019 - Oct 13, 2019
Sacral Nerve Manual Assessment and Treatment - Tampa, FL
Dec 6, 2019 - Dec 8, 2019
Upcoming lumbar nerve courses:
Lumbar Nerve Manual Assessment and Treatment - Phoenix, AZ
Jan 11, 2019 - Jan 13, 2019
Lumbar Nerve Manual Assessment and Treatment - San Diego, CA
May 3, 2019 - May 5, 2019
My name is Tina Allen. I teach a course called Manual Therapy Techniques for the Pelvic Rehab Therapist. I developed this course in 2016 out of desire to help clinicians feel comfortable in their palpation and hands on skills.
 My journey as a pelvic rehab therapist started with a patient whispering to me in the middle of a busy sports/ortho clinic gym; “is it normal to leak when you laugh”. I was treating her after her total hip replacement and my first question was “where are you leaking”? I was concerned that her incision was leaking, that she had an infection and it was beyond me to understand why it would happen when she laughed! I was 24 years old and 2 years out of PT school. Little did I know, that one whispered question would lead me to where I am today. I am in my 25th year as a PT and 20th year specializing in pelvic rehabilitation.
My journey as a pelvic rehab therapist started with a patient whispering to me in the middle of a busy sports/ortho clinic gym; “is it normal to leak when you laugh”. I was treating her after her total hip replacement and my first question was “where are you leaking”? I was concerned that her incision was leaking, that she had an infection and it was beyond me to understand why it would happen when she laughed! I was 24 years old and 2 years out of PT school. Little did I know, that one whispered question would lead me to where I am today. I am in my 25th year as a PT and 20th year specializing in pelvic rehabilitation.
When I started out there just were not many classes. I spent time learning from physicians, reading anything I could find and applying ‘general ‘orthopedic principles to the pelvis. I traveled to clinics and learned from other clinicians. I soaked up anything I could and brought it back to my clinical practice. When Holly Herman and Kathe Wallace asked me to teach with them I was humbled, honored and terribly nervous. Holly and Kathe where two of my greatest resources and to be able to teach along side them to help others along was humbling. As I prepared to teach I realized the breadth of what we do as pelvic rehab clinicians has grown exponentially since I started out.
Over the past 10 years of teaching the pelvic series with H&W; I noticed that for some of the participants there was a gap in confidence in palpation skills and in treatment techniques applied to the pelvic floor region. For most, it’s confidence in what they are feeling and where they are. This course came out of wanting to fill that gap. I wanted to allow a space that clinicians could come and spend two days learning, affirming and building confidence in their hands. They could then take those skills and confidence back to their clinics and help more patients.
The thought of writing this course was daunting. First off, written words are not my thing. Don’t get me wrong I love to read but me coming up with what to put on paper, much less a power point slide, frightened me. With much encouragement and support from colleagues and H&W, I got to work. The first thing was to think about what techniques to include. At some point after 20 years in the field, your hands just do the work and you don’t think about how you do something. My colleague and dear friend Katy Rice allowed me to sit down with her, practice a technique and then write down each specific step to do the skill. She would read them over and then attempt to do the technique by following only the written instructions. I also had patients who were instrumental in helping me choose what techniques to include. They would say to me “that is what made all the difference for me; it has to be included in what you teach others. “
I would think about who taught me each technique, whether it was a course, another clinician or a patient. I know that I did not make any of these up myself; while I may have modified a technique to work with my hands I did not originate them. Holly Tanner was so kind to brain storm with me and lead me to references for some of the techniques that we as clinicians use every day and that I was planning to include.
What happened next was months of me sitting at the kitchen table combing through books, articles, course manuals and online videos looking for origins of the techniques I use every day in my clinical practice. I wanted to be sure to give credit to sources. It was tedious but also inspiring to realize that some of these techniques have been around and documented since 1956 (Dicke, E., & Bischof-Seeberger, I.) and also that the same techniques are sited by multiple different sources. After about 6 months of our kitchen table not being suitable for dinner it was time to see what I had gathered and how it would all fit together. The result was this 2 day course: Manual Therapy Techniques for the Pelvic Rehab Therapist which has seven labs including internal, external and combination techniques, home program/self care ideas and time for brainstorming treatment progressions. Join me in Philadelphia, PA this October 20 - 21 to learn these essential skills.
This post is part two of Nari Clemon's series on practitioner burnout, compassion fatigue, and the story of a pelvic rehab therapist who struggled to care for herself while caring for patients. Read part one here.
There is a point where caring so much and wanting to help becomes counter-productive to us, until we burn out. We can develop true compassion fatigue. Compassion fatigue makes us feel apathetic, spent, and sometimes even jaded or cranky. But, how do we turn that caring off in time? Our compassion is what led us to this field in the first place.
 That day, I talked to my colleague and close friend, whom I was teaching with, Jen VandeVegte. Jen and I both felt that conversation was a wake-up call. We talked about seeing this same scenario at our courses: so many amazing therapists getting spent, and our best therapists getting burnt out. People were coming back with enhanced skills course after course, but many of them were looking weary and tired...
That day, I talked to my colleague and close friend, whom I was teaching with, Jen VandeVegte. Jen and I both felt that conversation was a wake-up call. We talked about seeing this same scenario at our courses: so many amazing therapists getting spent, and our best therapists getting burnt out. People were coming back with enhanced skills course after course, but many of them were looking weary and tired...
In the prior years, Jen and I were both trying to be mindful and intentional. But, it hadn’t been enough in our own lives. I remember thinking, “I’m mindful I’m getting drained and there is a creeping sensation of fatigue as I am working with this patient. Now what?” There seemed to be some pitfalls many of us were getting trapped in. We noticed there were certain patients who drained us more: when the role was therapist as hero and patient as victim. There were themes of not being able to leave the patient stories at work, finding ourselves laughing less, being less adventurous. There also seemed to be a link with empathy. Those of us who were more empathic carried burdens differently than our more concrete minded peers.
For myself, I had to hit bottom to learn how to climb back out. It got to the point where I didn’t honestly want to go to my thriving private practice and treat patients. I was treating more and more complex patients and leaving work drained, despite having a repertoire of advanced skills. I remember consulting with many people trying to understand how to stop this process of my patients’ illnesses and moods bleeding into my space and my body. People told me all kinds of things: “Imagine wearing gloves that are impenetrable”, “Picture a plexiglass box around yourself”, or “Just decide it is a one way flow.” None if it worked for me. I studied Reiki and worked with therapists. Still, I was so spent after treating patients. When I moved from Indiana to Portland, I took a whole year off of work with a singular mission: get healthy and figure out how to stay that way in my work. There was no book on this. There were some crazy stories and consults that made me realize I was heading in the wrong direction, and I finally learned the key concepts that changed my life.
And oddly enough, my great friend, Jen, also had to transform. We talked honestly and shared our failures, fears and successes as we learned. We committed to being real and honest about what parts of us were stuck in old, unhelpful paradigms. Some of these were playing the hero, feeling like there should not be limits on our compassion, not holding boundaries with what was ours to own, facing difficult things within ourselves, learning how to deeply own the space in our own bodies, and accepting that as intuitive, empathic women, we can’t expect ourselves to reproduce a very masculine, directive method of treating that denies so much of who we actually are. We also changed how we dialogued with patients from the outset. We read and researched and learned how to apply a shared responsibility model from the first contact with our patients and how to hold that model during the course of care. We then applied more pain theory and how to educate patients on those aspects of their own recovery to encourage a model of mind-body wellness and responsibility for their own reframing with our guidance. I created a mediation for pelvic health CD, so patients had a clear way to practice these home programs.
Jen and I both found that as we healed and re-framed there was a great freedom and honesty that emerged in our lives and our practices. We would get together to teach Capstone and were filled with gratitude for how much had shifted and that work no longer felt like a burden. Our lives were more balanced and we were physically, mentally and emotionally stronger. We felt like we had found the holy grail of balanced practices.
But, there we stood, teaching so many of our peers who were clearly in the same quicksand that had been plaguing us in the past. Where could our colleagues who were at our series courses go to learn how to do this job and navigate their days differently? How could they feel as good at the end of the day as they did before they saw patients? This was the training many pelvic therapists needed to thrive in this field AND their life, but it had taken us so many years. This was our call to action.
We all take courses on how to help our patients and how to reach those few difficult patients and help them. Yet, as medical professionals, we do not have enough training in how to care for ourselves. At some point, we all need to realize that our care is as important as our patients. Our wellness, physical, mental, and emotional also matter and may actually be necessary to keep helping patients. Enjoying our lives is no less important. It is an investment in your family, your future patients, and yourself to take a few days to peel back and deeply examine the root of why work is so taxing and come up with a clear, individualized plan to take your life, joy and passion back…without leaving pelvic rehab.
We need all of you in this field. We want to help you stay in this field and stay in it well! Please come join us in Boundaries, Self-Care and Meditation for a retreat-like weekend to change the framework of your practice and commit to your own wellness as a provider. Come learn how to shift dynamics from your first interaction with patients and how to hold that space. You are worth it!
Last year, I was teaching our Pelvic Floor Series Capstone course. It was the end of day three of the course. Most, students were thanking us for a course that filled in so many gaps in their practice and taught them a whole new way to use their hands. They were feeling energized and excited to bring all the new information back to their patients who had plateaued, so this was a surprising and atypical comment. To those of you who are unfamiliar with Capstone, it is a course for experienced pelvic therapist who have already taken three of the series courses, and it was written to address truly challenging patients, to learn to problem solve with manual therapies, to address all the things that my co-authors and I wished we had known five years into our field. It teaches complex problem solving and more receptive and dynamic use of their hands. So, usually, by this course, therapists are fully committed to this field and geeked-out to get so many more pearls. They are usually on board and looking for more sophisticated tools.
 As one student, Soniya (name changed) was walking out, she said, “I took this course to figure out if I want to treat pelvic patients, and I definitely don’t. It confirmed what I already knew about pelvic rehab being wrong for me.” I was so confused at that point. All I could say in that moment was, “Can you please tell me more about that? I’m interested.”
As one student, Soniya (name changed) was walking out, she said, “I took this course to figure out if I want to treat pelvic patients, and I definitely don’t. It confirmed what I already knew about pelvic rehab being wrong for me.” I was so confused at that point. All I could say in that moment was, “Can you please tell me more about that? I’m interested.”
Soniya went on to explain that she used to be a pelvic therapist. She said she loved it at first. But, she got so enmeshed with her patients and found she stopped having energy for the rest of her life: her kids, her health, her own enjoyment. She said she would go into her “dark cave” treatment room with her patients, isolated with them one at a time, and come out spent and depleted at the end of the day. She clarified that it was rewarding helping people so profoundly, but there came a point when she had to choose between helping others and saving herself. She changed back to outpatient ortho, choosing to treat in the gym, dynamically interacting with other PT’s all day and not being one-on-one in a room with patients and her problems. She also changed to part time, stating she just couldn’t be around patients five days a week anymore.
I understood. I totally got it. I hear this all the time at courses from other pelvic PT’s: that they love what they are doing, and they feel called to this line of help, but ultimately, they are depleted. I have been there. Pelvic rehab can get to be a little confusing with all the blurred lines. There are so many boundaries that are different. We ask our patients questions normal PT’s don’t. We do treatments in areas that other therapists don’t normally touch or see. We are one on one in a private room with our clients. We know more private details about our patients than most of their friends and family. And…we care deeply and listen intently….sometimes many hours a day to stories of other people’s pain, fears, and stress. Often, we are a lone pelvic practitioner in a practice with other kinds of PT’s. Let’s face it, our colleagues who don’t do pelvic rehab think we are a little weird! With HIPPAA, we can’t talk to our coworkers about our heart wrenching stories. We are also not trained psychologists, and our training in PT school really didn’t address how to deal with all we face in a day, especially the psychological aspects.
A recent study found nursing students show compassion fatigue before they even graduate and that “Therefore, knowledge of compassion fatigue and burnout and the coping strategies should be part of nursing training”. Yet, as pelvic therapists we are taught to recognize signs of trauma in our patients, but we are not yet taught how to stop ourselves from being traumatized.
I asked “Soniya” if it had worked for her: changing back to outpatient ortho and going part time. She said it had for the most part. She felt she had her life and energy back for the most part.
So, I asked “Soniya” how she landed at Capstone? What brought her here? It turns out her boss had asked her to come to Capstone and consider going back to pelvic rehab. So, she came and heard about all kinds of problem solving and new research with very complex patients at Capstone: cancer, multiple surgeries, systemic inflammation, endometriosis, and even gender affirming/change surgeries. She learned about complex hormonal issues, pharmacology and anatomy she hadn’t ever considered as an experienced pelvic therapist. She spent around 10 hours that weekend in lab, learning new ways to use her hands to make change. At the end, she said the thought of going “back in the cave” with such complex patients and having her hands on them all day long was draining to her. She just couldn’t go back.
There is a point where caring so much and wanting to help becomes counter-productive to us, until we burn out. We can develop true compassion fatigue. Compassion fatigue makes us feel apathetic, spent, and sometimes even jaded or cranky. But, how do we turn that caring off in time? Our compassion is what led us to this field in the first place.
This post is a two-part series on practitioner burnout and compassion fatigue from faculty member Nari Clemons, PT, PRPC. Nari helped to create the advanced Pelvic Floor Series Capstone course, which is available several times each year. Nari is also the author and instructor for Boundaries, Self-Care, and Meditation, Lumbar Nerve Manual Assessment and Treatment, and Sacral Nerve Manual Assessment and Treatment. Stay tuned for part two in an upcoming post on The Pelvic Rehab Report!
Mathias CT, Wentzel DL. Descriptive study of burnout, compassion fatigue and compassionsatisfaction in undergraduate nursing students at a tertiary education institution in KwaZulu-Natal. Curationis. 2017 Sep 22;40(1):e1-e6. doi: 10.4102/curationis.v40i1.1784. PMID: 2904178