Few patients discuss polycystic ovary syndrome (PCOS) in orthopedic manual therapy, but one lady left a lasting impression. She was adopted and did not know her family’s medical history or her genetics. At 18, she had a baby as a result of rape. At 34, she was married and diagnosed with POCS. She struggled with infertility, anxiety, obesity, and hypertension. Although I saw her for cervicalgia, the exercise aspect of her therapy had potential to impact her overall well-being and possibly improve her PCOS symptoms.
 Pericleous & Stephanides (2018) reviewed 10 studies that considered the effects of resistance training on PCOS symptoms. Some of these symptoms include the absence of or a significant decrease in ovulation and menstruation, which can lead to infertility; obesity, which in turn can affect cardiovascular health and increase the risk of diabetes, insulin resistance, and metabolic syndrome; and, mental health problems. Research has shown resistance training benefits include lowering body fat, improving insulin resistance and glucose metabolism, and increasing insulin sensitivity in type II diabetes. Although it has been documented that obesity and insulin resistance can exacerbate PCOS symptoms, resistance training is not a common recommendation in healthcare settings for patients with PCOS . Studies have shown diet and exercise are essential to improve cardiac and respiratory health and body makeup in patients with PCOS, as the combination improves the Follicle-stimulating hormone (FSH), sex hormone-binding globulin (SHBG), ovulation, testosterone levels, and weight loss. One systematic review found that weight loss can improve PCOS symptoms without consideration of diet; however, most other studies find intake of various macronutrients (protein, fat, carbohydrates) may lead to different results, and the effects of resistance training can only be optimized with appropriate dietary changes. These authors concluded caloric consumption and macronutrient habits must be considered in conjunction with resistance training to determine the greatest impact on improving PCOS symptoms.
Pericleous & Stephanides (2018) reviewed 10 studies that considered the effects of resistance training on PCOS symptoms. Some of these symptoms include the absence of or a significant decrease in ovulation and menstruation, which can lead to infertility; obesity, which in turn can affect cardiovascular health and increase the risk of diabetes, insulin resistance, and metabolic syndrome; and, mental health problems. Research has shown resistance training benefits include lowering body fat, improving insulin resistance and glucose metabolism, and increasing insulin sensitivity in type II diabetes. Although it has been documented that obesity and insulin resistance can exacerbate PCOS symptoms, resistance training is not a common recommendation in healthcare settings for patients with PCOS . Studies have shown diet and exercise are essential to improve cardiac and respiratory health and body makeup in patients with PCOS, as the combination improves the Follicle-stimulating hormone (FSH), sex hormone-binding globulin (SHBG), ovulation, testosterone levels, and weight loss. One systematic review found that weight loss can improve PCOS symptoms without consideration of diet; however, most other studies find intake of various macronutrients (protein, fat, carbohydrates) may lead to different results, and the effects of resistance training can only be optimized with appropriate dietary changes. These authors concluded caloric consumption and macronutrient habits must be considered in conjunction with resistance training to determine the greatest impact on improving PCOS symptoms.
Benham et al., (2018) also performed a recent systematic review to assess the role exercise can have on PCOS. Fourteen trials involving 617 females of reproductive age with PCOS evaluated the effect of exercise training on reproductive outcomes. The data published did not allow the authors to quantitatively assess the impact of exercise of reproductive in PCOS patients; however, their semi-quantitative analysis allowed them to propose exercise may improve regularity of menstruation, the rate of ovulation, and pregnancy rates in these women. Via meta-analysis, secondary outcomes of body measurement and metabolic parameters significantly improved after women with PCOS underwent exercise training; however, symptoms such as acne and hirsutism (excessive, abnormal body hair growth) were not changed with exercise. The authors concluded exercise does improve the metabolic health (ie, insulin resistance) in women with PCOS, but evidence is insufficient to measure the exact impact on the function of the reproductive system.
Increasing our knowledge about comorbidities such as PCOS, regardless of our practice setting, can help us provide better education to the patients we treat. Perhaps exercise compliance can increase when patients are told multiple long-term benefits, not just immediate symptom relief. More often than not, a patient’s 4-6 week interaction with us could motivate and promote healthy lifestyle changes.
Pericleous, P., & Stephanides, S. (2018). Can resistance training improve the symptoms of polycystic ovary syndrome? BMJ Open Sport — Exercise Medicine, 4(1), e000372. http://doi.org/10.1136/bmjsem-2018-000372
Benham, J. L., Yamamoto, J. M., Friedenreich, C. M., Rabi, D. M. and Sigal, R. J. (2018), Role of exercise training in polycystic ovary syndrome: a systematic review and meta‐analysis. Clin Obes, 8: 275-284. doi:10.1111/cob.12258
Suggested newly published resource for readers…
Teede, H. J., Misso, M. L., Costello, M. F., Dokras, A., Laven, J., Moran, L., … Yildiz, B. O. (2018). Recommendations from the international evidence-based guideline for the assessment and management of polycystic ovary syndrome. Human Reproduction (Oxford, England), 33(9), 1602–1618. http://doi.org/10.1093/humrep/dey256
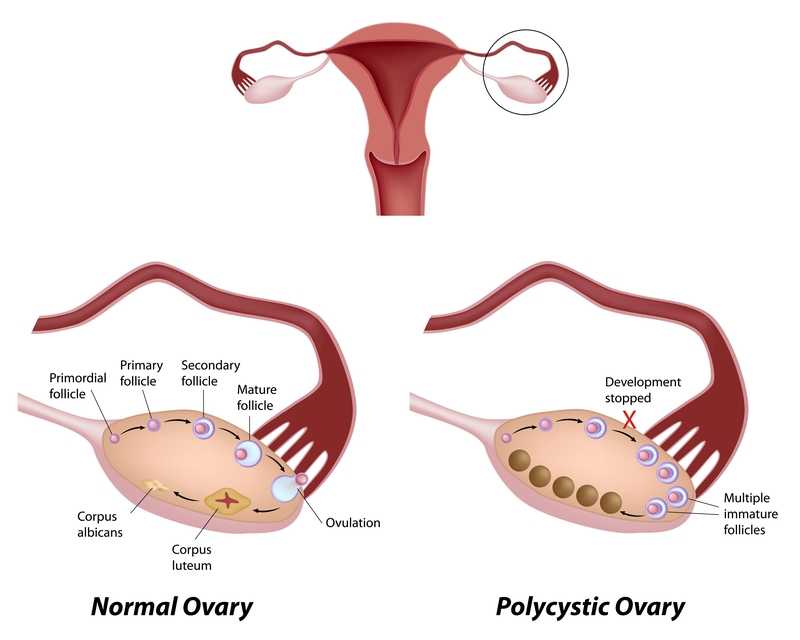
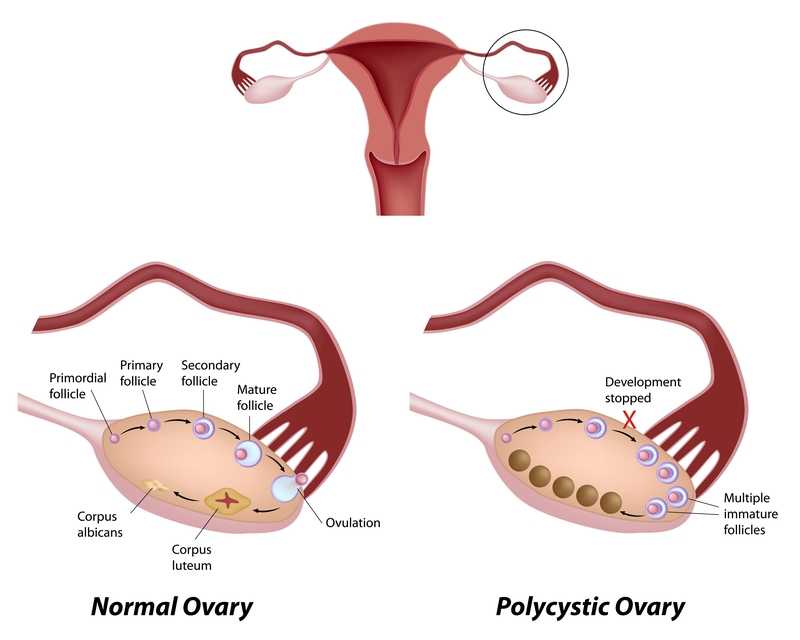
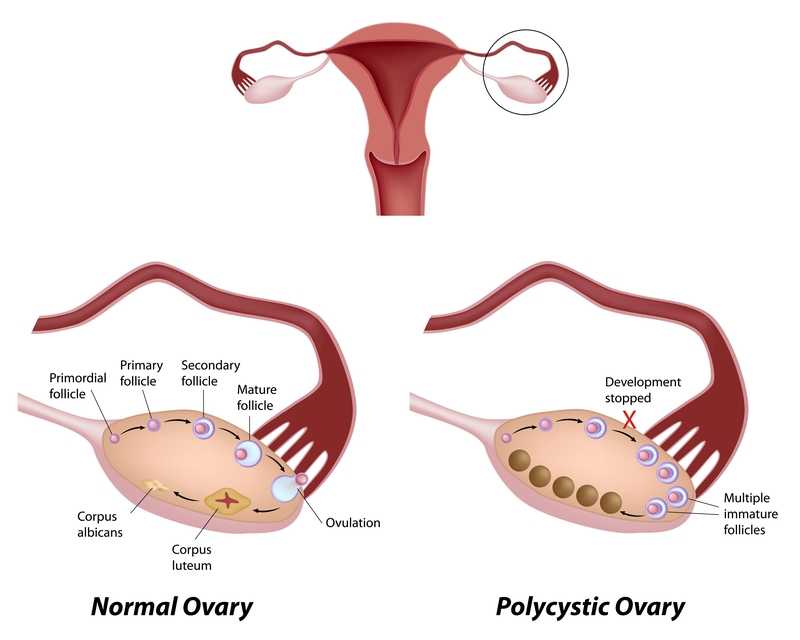
Polycystic ovarian disease (PCOS), also known as Stein-Leventhal syndrome, is an endocrine system disorder that affects women of reproductive age. The disease is associated with some major adverse health issues including infertility, diabetes, metabolic syndrome (a cluster of conditions that increase risk for heart disease, stroke and diabetes), cardiovascular issues and endometrial carcinoma. Because, according to Okamura et al., those with PCOS share risk factors for endometrial cancer and atypical endometrial hyperplasia, early detection and treatment are critical for optimal health outcomes. Some of the primary shared risk factors include obesity, not bearing any children (nulliparity), infertility, hypertension, diabetes, chronic anovulation, and unopposed estrogen supplementation.
One study (Malcolm2017) that addressed reproductive health comparisons among young women with and without PCOS found that although women diagnosed with PCOS had significant concerns about their reproductive health, they were found to be as sexually active as young women without PCOS. Unfortunately, women with PCOS were more likely to have pelvic inflammatory disease (PID), which could increase the risk of infertility. In this study, the importance of counseling in safe sex practices such as condom use and sexually transmitted infection screening was highlighted.
As weight loss in women diagnosed with PCOS has been shown to improve blood sugar levels, exercise and healthy weight management strategies can also be keystones of care. Vasheghani-Farahani et al report on a home-based exercise program with positive outcomes in health for women with PCOS. The women in this study were ages 15-40, with 16 patients in the exercise group and 14 in the control group. Blood pressure, waist to hip ratio, BMI, blood tests for insulin factors, sex hormones, and markers of inflammation made up outcomes measures at baseline and again at 12 weeks following intervention. The active group completed aerobic and strengthening exercises and were found to have an improved waist to hip ratio as well as reductions in cardiovascular risk profiles.
The exercise instructed as home program is as follows: 30 minute walk at least 5 days per week at medium intensity (64%-76% max heart rate), strengthening exercises of biceps curl, wall push up, chair push up, single arm row, seated lower leg lift, seated straight leg lift, stair step and chair squat 10 times each. The participants were instructed to increase the exercise bouts per day from 1 to 3 by the end of the study. Participants were guided through the exercises at the beginning of the study, and exercise logs as well as phone calls were used to track progress, answer questions.
This study is an encouraging example of simple yet effective strategies to guide women diagnosed with PCOS. Although there are other equally valuable aspects of care that a pelvic health therapist can be involved in for women managing this challenging disease, the research presented reminds us that basic information on healthy sexual practices and provider follow-up, strengthening and aerobic exercise can have meaningful impact on quality of life. If you are interested in learning more about PCOS and other endocrine conditions, and ways to help manage pelvic pain, adhesions, and other symptoms, join us in Pelvic Floor Series Capstone: Advanced Topics in Pelvic Rehab, available twice more in 2017.
Malcolm, S., Tuchman, L., Cheng, Y. I., Wang, J., & Gomez-Lobo, V. (2017). Differences in Reproductive Health Issues in Adolescent Females With Polycystic Ovarian Syndrome Compared to Controls. Journal of Pediatric and Adolescent Gynecology, 30(2), 330-331.
Okamura, Y., Saito, F., Takaishi, K., Motohara, T., Honda, R., Ohba, T., & Katabuchi, H. (2017). Polycystic ovary syndrome: early diagnosis and intervention are necessary for fertility preservation in young women with endometrial cancer under 35 years of age. Reproductive Medicine and Biology, 16(1), 67-71.
Vasheghani-Farahani, F., Khosravi, S., Yekta, A. H. A., Rostami, M., & Mansournia, M. A. (2017). The Effect of Home based Exercise on Treatment of Women with Poly Cystic Ovary Syndrome; a single-Blind Randomized Controlled Trial. Novelty in Biomedicine, 5(1), 8-15.