Tara Sullivan, PT, DPT, PRPC, WCS, IF is on faculty with Herman & Wallace. She created Sexual Medicine in Pelvic Rehab and co-created Pain Science for the Chronic Pelvic Pain Population which she instructs alongside co-creator Alyson N Lowrey, PT, DPT, OCS. Tara started in the healthcare field as a massage therapist, practicing over ten years including three years of teaching massage and anatomy and physiology. Tara has specialized exclusively in Pelvic Floor Dysfunction treating bowel, bladder, sexual dysfunctions, and pelvic pain since 2012. She is adjunct faculty speaking at the annual conference for the International Society for the Study of Women’s Sexual Health (ISSWSH) and teaches an elective course at Northern Arizona University (NAU) and Franklin Pierce University on Pelvic Health. Tara is very passionate about creating awareness on Pelvic Floor Dysfunction and recently launched her website pelvicfloorspecialist.com to continue educating the public and other healthcare professionals.
You may have heard of Jessica Pin. She’s been making headlines lately with the unconventional ways she is going about changing what medical texts and schools teach about the clitoris…..which is currently very little. According to Pin, who has a bachelor’s degree in biomedical engineering, the average textbook has over 50 pages more dedicated to the penis than compared to the clitoris. Jessica Pin started her journey to create awareness of clitoral anatomy because at 17 years old she had a labiaplasty leaving her with sensory loss. Jessica’s activism has so far changed 8 medical texts to include detailed anatomy of the clitoris in hopes knowledge of this anatomy is understood well, as it is critical prior to performing surgery near the clitoris.
Loss of clitoral function can also occur after labiaplasty, biopsies, cosmetic surgeries, and repair. As pelvic rehab providers, there is a level of responsibility we have to help shift the narrative. How often have we seen or heard similar stories of young patients undergoing cosmetic surgeries to try to ‘look normal’ or apologize for the way they look? We have such a unique position to spend time educating our patients and treating sexual dysfunctions across the spectrum.
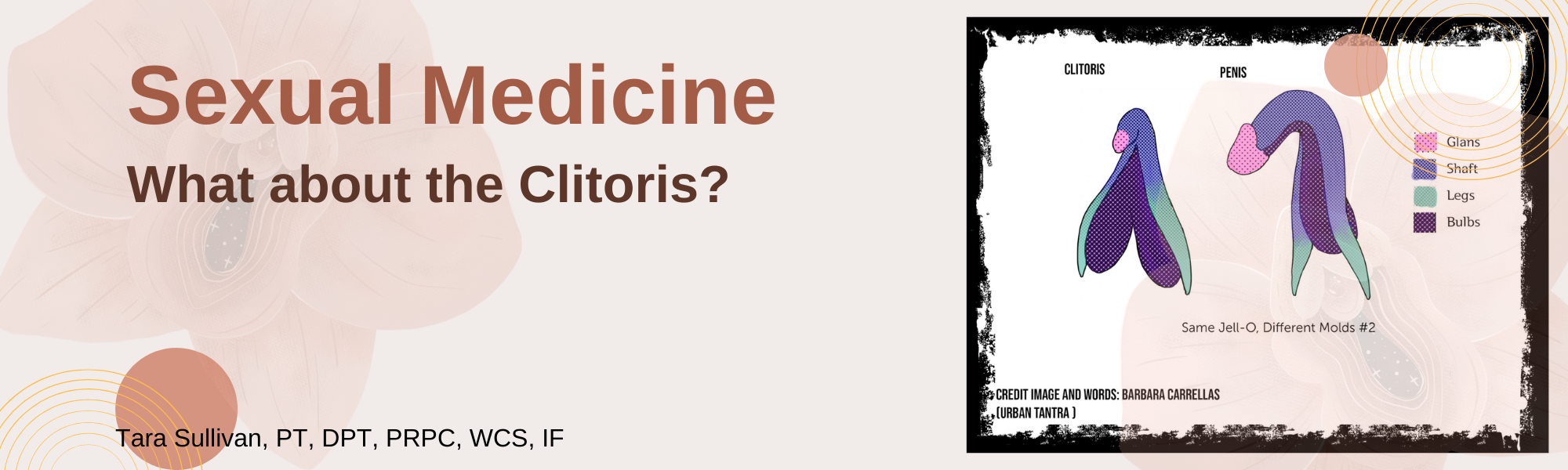
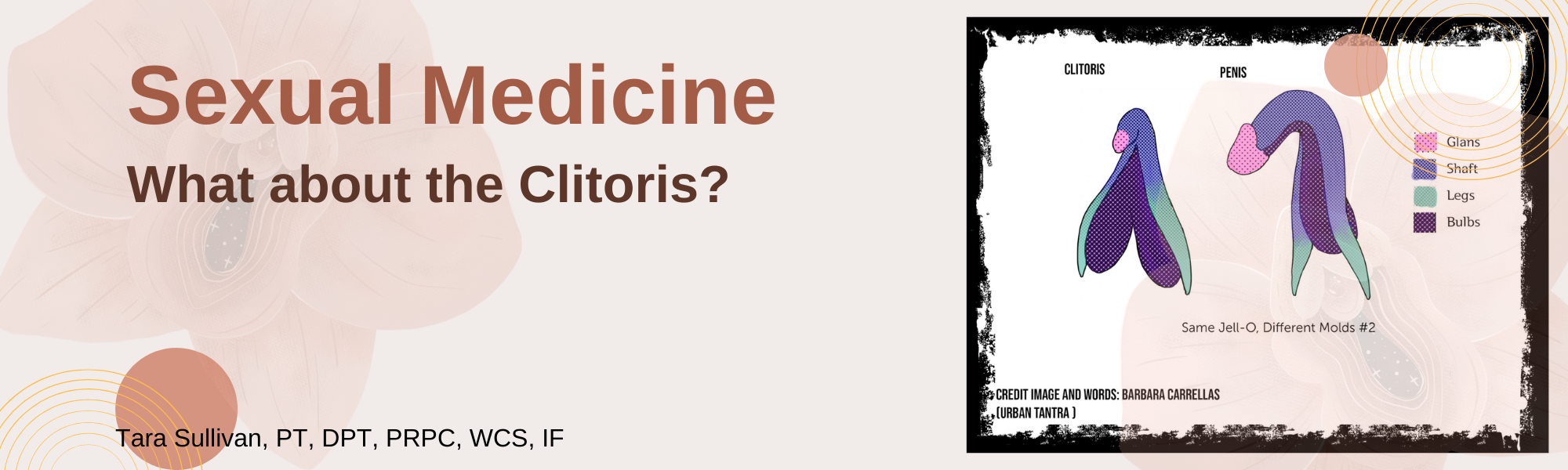
The clitoris is analogous to the penis so what is the cause of this disparity? It could be that, traditionally, the focus has been on penetrative intercourse which largely overlooks that the clitoris is the primary sexual organ of the female sexual response and that 81.6% of women don’t orgasm from intercourse alone (without additional clitoral stimulation). Only 18.4% of women report that intercourse alone is sufficient to orgasm (Herbenick, et al. 2018).
The clitoris has historically been omitted from anatomical textbooks and then ‘rediscovered’ throughout medical history (O’connell, 1998). If you look at the 1948 Grey’s Anatomy textbook you will see that the clitoris was left out. Anatomical information centralized around the medical field has been historically male-dominated, affecting how the world discusses and understands anatomy and their bodies even in the current day. In 2005 Wade, Kremer and Brown ran a study on college students and found that 29% of women and 25% of men could not identify the clitoris on a diagram of the vulva. We need to revolutionize female sexuality in general, change the focus from the linear model where penetrative sex and orgasm are the focus as it’s been traditionally taught.
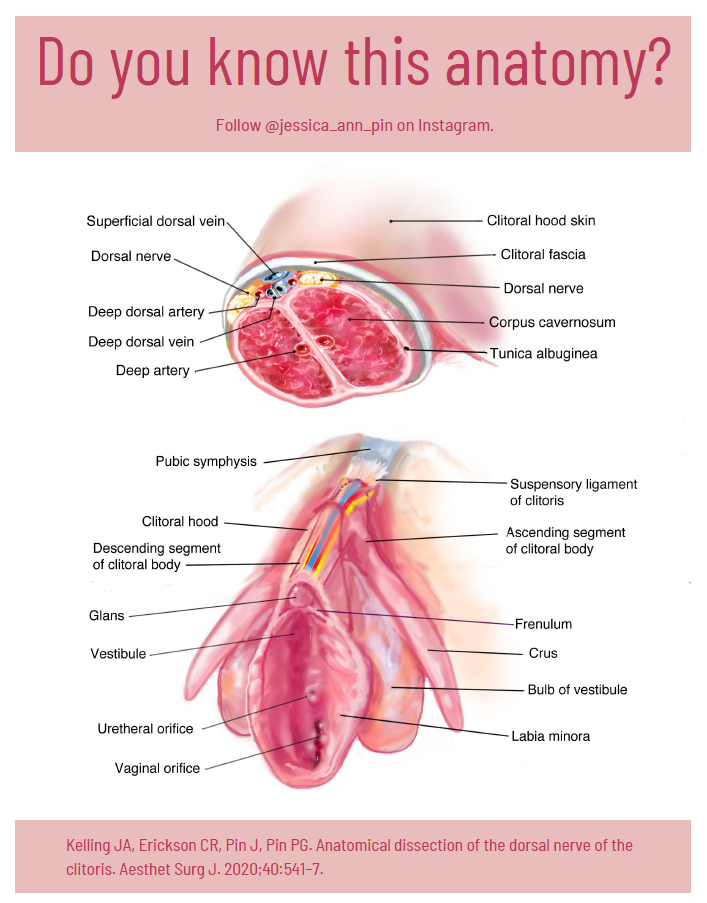
The full clitoris goes far beyond the crown which is the external tip. The clitoris actually extends several inches into the body where it branches into a shape similar to a wishbone. A description that I love is from Latham Thomas, “It’s all this amazing erectile tissue that wraps around, and it all engorges when it’s stimulated. Pound for pound, if you have a vulva, you actually have the same amount of erectile tissue that people with penises have, but it’s just internal.” These clitoral legs are responsible for the sensations where the front wall of the vagina connects to the paraurethral glands (the G-spot) and for female ejaculation.
I authored the Herman & Wallace Sexual Medicine in Pelvic Rehab course for practitioners to have a platform to learn proper anatomy, identify misconceptions, and understand that sexuality is circular with satisfaction as the focus. With the understanding of ‘normal’ anatomy and function, we can help our patients with sexual dysfunctions return to a healthy sexual lifestyle.
To sign the petition to get the nerves of the clitoris into the American College of OB/GYN curriculum go to:
Sexual Medicine in Pelvic Rehab is a two-day, remote continuing education course designed for pelvic rehab specialists who want to expand their knowledge, experience and treatment in sexual health and dysfunction. This course provides a thorough introduction to pelvic floor sexual function, dysfunction, and treatment interventions for the gender and sexual spectrum, as well as an evidence-based perspective on the value of physical therapy interventions for patients with chronic pelvic pain related to sexual conditions, disorders, and multiple approaches for the treatment of sexual dysfunction including understanding medical diagnosis and management.
Lecture topics include hymen myths, female squirting, G-spot, prostate gland, female and male sexual response cycles, hormone influence on sexual function, anatomy and physiology of pelvic floor muscles in sexual arousal, orgasm. As well as the function and specific dysfunction treated by physical therapy in detail including vaginismus, dyspareunia, erectile dysfunction, hard flaccid, prostatitis, post-prostatectomy; as well as recognizing medical conditions such as persistent genital arousal disorder (PGAD), hypoactive sexual desire disorder (HSDD) and dermatological conditions such as lichen sclerosis and lichen planus. Upon completion of the course, participants will be able to confidently treat sexual dysfunction related to the pelvic floor as well as refer to medical providers as needed and instruct patients in the proper application of self-treatment and diet/lifestyle modifications.
Course dates in 2022 include:
Top Homogenous Image: Internal genitalia depicting homology (Carrellas, B. and Sprinkle, A., 2017).
Bottom Clitoral Anatomy Image: Jessica Pin, https://drive.google.com/file/d/1fS1HfBWYqXAEBu_jnAPuiulTE3nqIYYQ/view
O'Connell, H.E., Hutson, J.M., Anderson, C.R. and Plenter, R.J., 1998. Anatomical relationship between urethra and clitoris. The Journal of Urology, 159(6), pp.1892–1897.
Herbenick, D., Tsung, Chieh F., Arter, J. Women's Experiences With Genital Touching, Sexual Pleasure, and Orgasm: Results From a U.S. Probability Sample of Women Ages 18 to 94. https://www.tandfonline.com/doi/abs/10.1080/0092623X.2017.1346530
Wade, L.D., Kremer, E.C. and Brown, J., 2005. The incidental orgasm: The presence of clitoral knowledge and the absence of orgasm for women. Women & Health, 42(1), pp.117–138.