Earlier this year, 3 prominent societies representing pelvic health met to discuss and update terminology for vulvar pain. The result is the “2015 Consensus Terminology and Classification of Persistent Vulvar Pain.” A complete list of the updated terminology can be accessed on the website of the International Pelvic Pain Society. The updated document takes into account the additions of the terms Primary versus Secondary Vulvodynia, intermittent versus persistent pain, and considers research-based interventions for the suspected etiologies of pain. Some of the other updates are highlighted below.
- Replace the term “unprovoked” with “spontaneous”
- Use the term “vulvar” rather than “vulvodynia” in the title of the terminology
- Vulvar pain definition removes the word “burning” from description
Vulvar pain can have a known cause, and the categories within vulvar pain caused by a specific disorder are: infectious, inflammatory, neoplastic, neurologic, trauma, iatrogenic, and hormonal deficiencies. Vulvodynia, defined as vulvar pain at least 3 months in duration, and without a clear identifiable cause, is described as having “potential associated factors.” There are also descriptor terms such as localized, provoked, or mixed, and terms such as intermittent, persistent, constant, immediate or delayed.
The terminology document recognizes that a patient may have a specific condition or diagnosis, and also be diagnosed with vulvodynia. As this consensus document is designed to replace the ISSVD terminology from the 2003 publication, becoming familiar with the updates is valuable for pelvic rehabilitation providers. The evaluation and treatment of vulvar pain is introduced in the Insitute’s Pelvic Floor Level 1 continuing education course, and further developed in the Level 2B course. For an immersion in the topic of vulvar pain, check out the Institute’s course on Vulvodynia: Assessment and Treatment instructed by Dee Hartmann. Your next opportunity to take the course is this March in Houston.
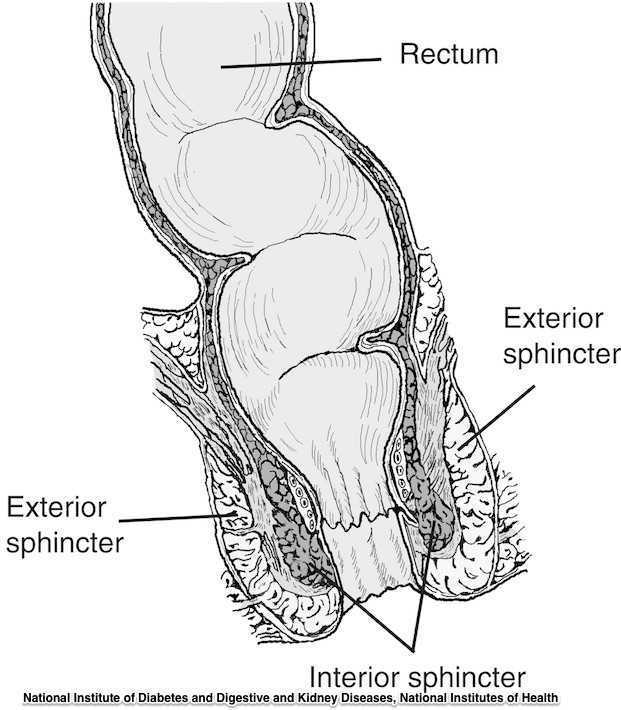
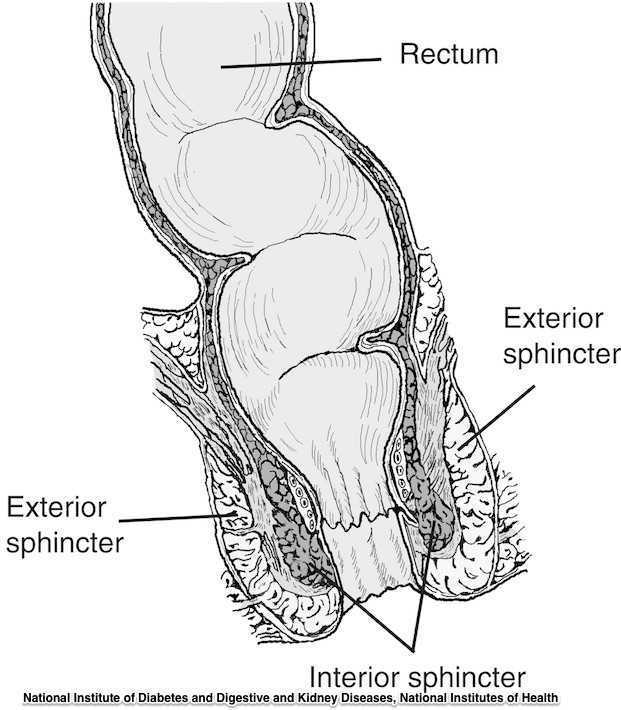
Guidelines for the management of 3rd and 4th degree tears were updated and published last month by The Royal College of Obstetricians & Gynaecologists. The purpose of the guidelines are to provide evidence-based guidelines on diagnosis, management and treatment of 3rd and 4th degree perineal tears. These types of tears are also referred to as obstetric anal sphincter injuries, or OASIS. The authors acknowledge an increased rate of reported anal sphincter injuries in England that may in part be due to increased awareness and detection of the issue. In terms of classification of anal sphincter injuries, the following is recommended (note the different levels at grade 3:
- 1st degree tear: injury to the perineal skin and/or the vaginal mucosa
- 2nd degree tear: injury to the perineum involving the perineal muscles but not involving the anal sphincter.
- 3rd degree tear: injury to the perineum involving the the anal sphincter complex
- Grade 3a tear: Less than 50% of the external anal sphincter (EAS) thickness is torn.
- Grade 3b tear: More than 50% of the EAS thickness is torn.
- Grade 3c tear: Both the EAS and the internal anal sphincter (OAS) are torn.
- 4th degree tear: Injury to the perineum involving the anal sphincter complex (EAS and IAS) and the anorectal mucosa.
Risk factors for anal injury are also outlined in the guidelines, although the authors point out that accurate prediction based on the risk factors is not reliable. The noted risk factors are as below:
- Asian ethnicity
- Nulliparity
- Birthweight greater than 4 kg (8.8 lb)
- Shoulder distocia
- Occipito-posterior position
- Prolonged 2nd stage labor
- Instrumented delivery
Recommendations worth noting include Level A evidence that warm compression during the 2nd stage of labor reduces the risk of OASIS. A noted best practice recommendation is that “Women should be advised that physiotherapy following repair of OASIS could be beneficial.” Guidelines such as these from The Royal College of Obstetricians & Gynaecologists can help in creating common language and in making recommendations that improve communication and expectations between patients and providers.
If you are interested in learning more about anal tears, Herman & Wallace offers several courses which cover the topic. For postpartum care specifically, check out Care of the Postpartum Patient.