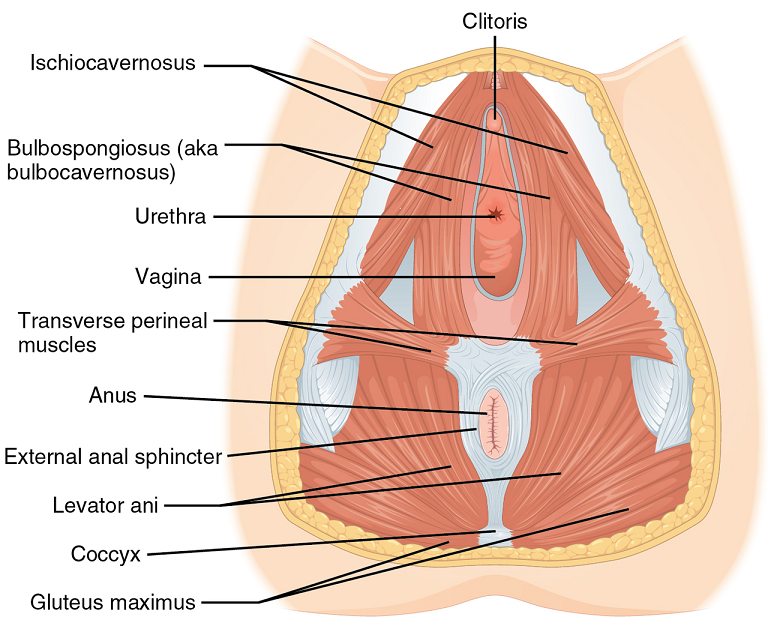
Perineal massage involves pelvic floor muscle stretching by application of an external pressure to muscle and connective tissue in the perineal region. It is performed 4 to 6 weeks before childbirth to help the soft tissue in that region to withstand stretching during labor. This helps to prevent perineum during birth by decreasing the need for an episiotomy or an instrument-assisted delivery. Lengthening of skeletal muscles is known to modify the viscoelastic properties of the muscle-tendon unit, which decreases the tension peak of the musculature and therefore, chances of injury.
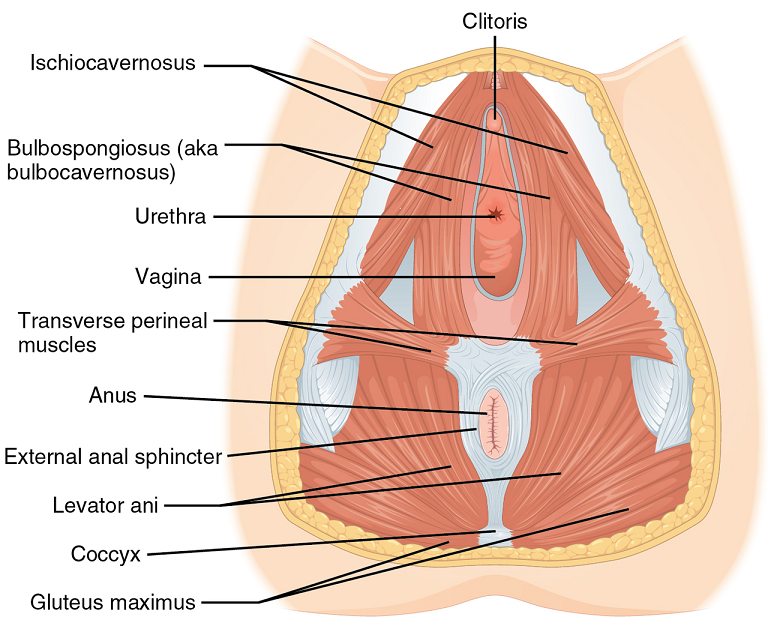 Pelvic floor muscle stretching is performed via widening of the hiatus in the axial plane. Perineal massage is a simple technique has been found to be associated with a decrease in the incidence of perineal tears requiring suture or an episiotomy. It has also been reported to reduce postpartum pain.
Pelvic floor muscle stretching is performed via widening of the hiatus in the axial plane. Perineal massage is a simple technique has been found to be associated with a decrease in the incidence of perineal tears requiring suture or an episiotomy. It has also been reported to reduce postpartum pain.
Instrument-assisted stretching is performed with the help of an inflatable silicon balloon that can be pumped to gradually stretch the vagina and perineum. However, the evidence to support its benefit is lacking. In fact, there is some concern that pelvic floor muscle stretching may cause a decrease in muscle strength. Some have argued that such exercise neither improve or worsen pelvic function (Labrecque M, et al., Medi-dan, et al.). While a meta-analysis by Aquino, et al. concluded that perineal massage during labor significantly lowered risk of severe perineal trauma, such as third and fourth degree lacerations (Aquino, et al.).
A recent major study done by deFreitas, et al., perineal massage and instrument-assisted stretching were found to improve perineal muscle extensibility when performed in multiple sessions on primiparous women beginning at 34th week of gestation, which is very helpful in preventing child trauma in labor; however, there was no increase in muscle strength.
The technique of performing the manual perineal massage (as exemplified in the aforementioned study) may involve two sessions per week for a month by an OBGYN-focused physiotherapist. The patients are rested in dorsal decubitus position with the inferior limbs semi-flexed and the lower limbs and feet supported on the examination table. Coconut oil can be used for the perineal massage - which starts off with circular movements in the external area of the vulva, around the vagina and in the central tendon of the perineum, followed by the index and middle fingers inserted approximately 4 cm in the vaginal introitus for an internal massage of the lateral walls of the vagina ending toward the anus, repeated four times on each side, with the whole process lasting approximately 10 minutes.
Instrument-assisted procedure may include inserting the instrument (Epi-No) covered with a condom and lubricated with a water-based gel, inflated at the vaginal introitus so that 2 cm of the balloon is visible, making sure the patient can tolerate the stretching, and are advised to keep the pelvic floor relaxed as the instrument is slowly expelled during expiration. Physiotherapist supervision is necessary in order to maintain the correct positioning of the balloon as it lengthens the muscles. He/she will also ensure proper expulsion of the equipment during expiration.
Overall, perineal massage techniques (with or without instrumentation) are beneficial in terms of preventing trauma during labor. There are many studies that support the efficacy of these techniques in doing so (Leon-Larios, et al.). But it is also important to appreciate the limitations and use it judiciously.
Randomized trial of perineal massage during pregnancy: perineal symptoms three months after delivery. Labrecque M, et al. Am J Obstet Gynecol. 2000.
Perineal massage during pregnancy: a prospective controlled trial. Mei-dan E, et al. Isr Med Assoc J. 2008.
Perineal massage during labor: a systematic review and meta-analysis of randomized controlled trials. Aquino CI, et al. J Matern Fetal Neonatal Med. 2018.
Effects of perineal preparation techniques on tissue extensibility and muscle strength: a pilot study. de Freitas SS, et al. Int Urogynecol J. 2018.
Influence of a pelvic floor training programme to prevent perineal trauma: A quasi-randomised controlled trial. Leon-Larios F, et al. Midwifery. 2017.
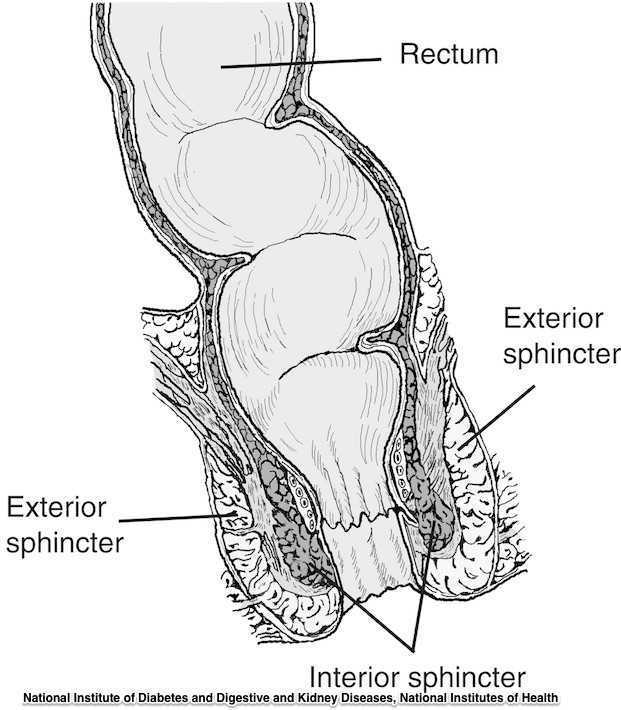
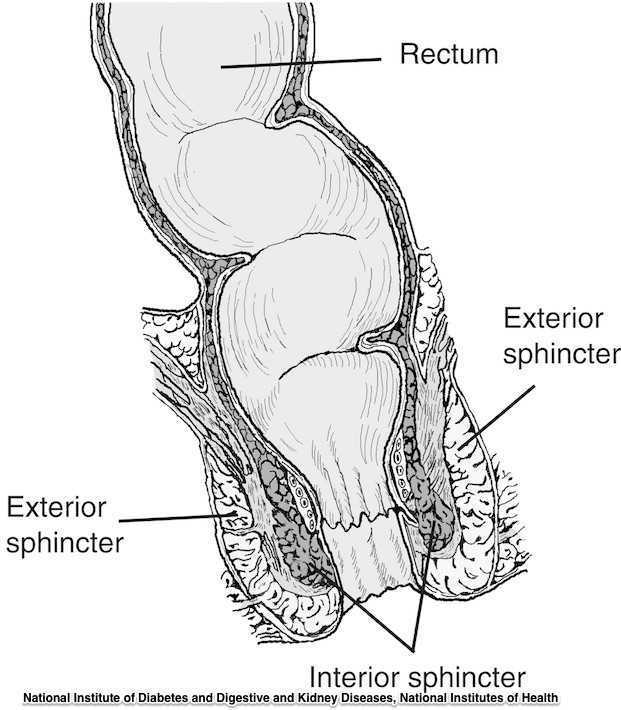
Guidelines for the management of 3rd and 4th degree tears were updated and published last month by The Royal College of Obstetricians & Gynaecologists. The purpose of the guidelines are to provide evidence-based guidelines on diagnosis, management and treatment of 3rd and 4th degree perineal tears. These types of tears are also referred to as obstetric anal sphincter injuries, or OASIS. The authors acknowledge an increased rate of reported anal sphincter injuries in England that may in part be due to increased awareness and detection of the issue. In terms of classification of anal sphincter injuries, the following is recommended (note the different levels at grade 3:
- 1st degree tear: injury to the perineal skin and/or the vaginal mucosa
- 2nd degree tear: injury to the perineum involving the perineal muscles but not involving the anal sphincter.
- 3rd degree tear: injury to the perineum involving the the anal sphincter complex
- Grade 3a tear: Less than 50% of the external anal sphincter (EAS) thickness is torn.
- Grade 3b tear: More than 50% of the EAS thickness is torn.
- Grade 3c tear: Both the EAS and the internal anal sphincter (OAS) are torn.
- 4th degree tear: Injury to the perineum involving the anal sphincter complex (EAS and IAS) and the anorectal mucosa.
Risk factors for anal injury are also outlined in the guidelines, although the authors point out that accurate prediction based on the risk factors is not reliable. The noted risk factors are as below:
- Asian ethnicity
- Nulliparity
- Birthweight greater than 4 kg (8.8 lb)
- Shoulder distocia
- Occipito-posterior position
- Prolonged 2nd stage labor
- Instrumented delivery
Recommendations worth noting include Level A evidence that warm compression during the 2nd stage of labor reduces the risk of OASIS. A noted best practice recommendation is that “Women should be advised that physiotherapy following repair of OASIS could be beneficial.” Guidelines such as these from The Royal College of Obstetricians & Gynaecologists can help in creating common language and in making recommendations that improve communication and expectations between patients and providers.
If you are interested in learning more about anal tears, Herman & Wallace offers several courses which cover the topic. For postpartum care specifically, check out Care of the Postpartum Patient.