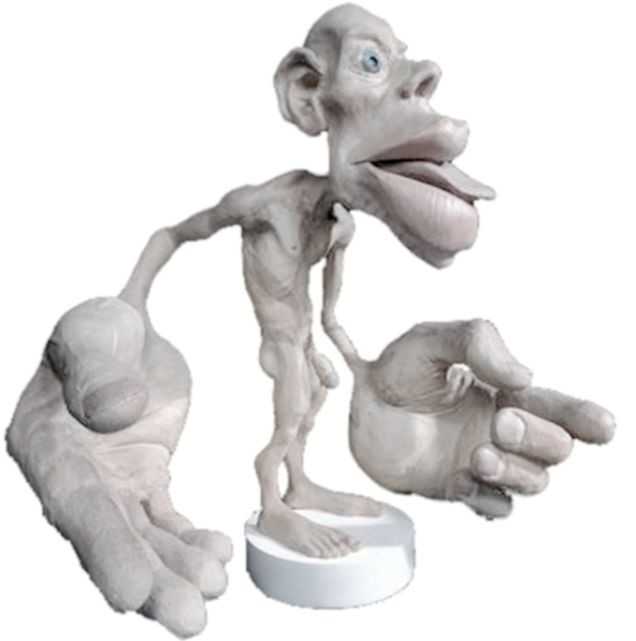
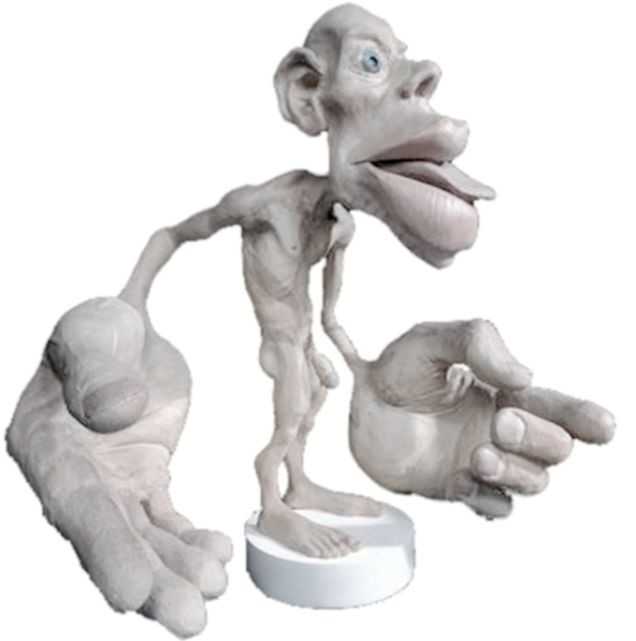
In the 16th century, a theory called Preformationism claimed that sperm contained a preformed, exceedingly minute body referred to as a homunculus, which eventually became a person. This idea of a tiny man had staying power, as today the homunculus is a “body map” based on how much of the cerebral cortex is devoted to sensing each part of the body. Although the idea of a 16th alchemist placing little bodies into a flask conjures a variety of tantalizing images, our program focuses on the mundane, contemporary version of the homunculus. So…what does this have to do with a course that addresses pelvic floor dysfunction? Everything.
 Emerging evidence indicates that therapies that include work to enhance body awareness/kinesthetic sense are potent and effective. Our professional training unfortunately, tends to over-emphasize a structural approach. The good news is that manual therapy, to some degree, enhances a client’s body awareness; but when we have more “tools” to capitalize on this synergy between manual therapy and improved body awareness, we have a potent “elixir” to promote change. To quote Deane Juhan, “touching hands are not like pharmaceuticals or scalpels…they are like flashlights in a darkened room.” By using the “flashlight”, we not only contribute to structural change, but neurological change – meaning the more we pay attention to a particular part of our body, the more “real estate” the brain devotes to that part of the body. Increasing the pelvic floor’s “footprint” on the brain can enhance function of the pelvic floor dramatically and quickly. Therefore, rehabilitation to address pelvic floor dysfunction benefits from weaving orthopedic, neurologic and mindfulness practices together.
Emerging evidence indicates that therapies that include work to enhance body awareness/kinesthetic sense are potent and effective. Our professional training unfortunately, tends to over-emphasize a structural approach. The good news is that manual therapy, to some degree, enhances a client’s body awareness; but when we have more “tools” to capitalize on this synergy between manual therapy and improved body awareness, we have a potent “elixir” to promote change. To quote Deane Juhan, “touching hands are not like pharmaceuticals or scalpels…they are like flashlights in a darkened room.” By using the “flashlight”, we not only contribute to structural change, but neurological change – meaning the more we pay attention to a particular part of our body, the more “real estate” the brain devotes to that part of the body. Increasing the pelvic floor’s “footprint” on the brain can enhance function of the pelvic floor dramatically and quickly. Therefore, rehabilitation to address pelvic floor dysfunction benefits from weaving orthopedic, neurologic and mindfulness practices together.
This program is designed to add a new dimension for the skilled pelvic floor practitioner and to also serve practitioners new to this area of practice. There is no internal manual work; rather we draw from our deep knowledge of Yoga, Tai Chi, along with other Chinese internal martial arts (that put lots of emphasis on the pelvic floor for performance) and Feldenkrais to address pelvic floor dysfunction. Some lessons focus directly on the pelvic region and others on integrating the pelvic floor with full body movement. Ultimately, our goal is to help you connect the dots between structural, functional movement and mindfulness practices, as this powerful triad offers practitioners a comprehensive, approach for treating pelvic floor dysfunction.
We hope you’ll come join in New York City on September 18th & 19th. If you do, wear comfortable clothes as the workshop is designed to provide participants opportunities to embody the work…emphasis is placed on labs more than lecture.
Don’t hesitate to contact us if you have any questions.
This email address is being protected from spambots. You need JavaScript enabled to view it.
This email address is being protected from spambots. You need JavaScript enabled to view it.
In manual therapy training, we do not learn just one position to mobilize a joint, so why should pelvic floor muscle training be limited by the standard training methods? There is almost always at least one patient in the clinic that fails to respond to the “normal” treatment and requires a twist on conventional therapy to get over a dysfunction. Thankfully, classes like “Integrative Techniques for Pelvic Floor and Core Function” provide clinicians with the extra tools that might help even just one patient with lingering symptoms.
 In 2014, Tenfelde and Janusek considered yoga as a treatment for urge urinary incontinence in women, referring to it as a “biobehavioral approach.” The article reviews the benefits of yoga as it relates to improving the quality of life of women with urge urinary incontinence. Yoga may improve sympatho-vagal balance, which would lower inflammation and possibly psychological stress; therefore, the authors suggested yoga can reduce the severity and distress of urge UI symptoms and their effect on daily living. Since patho-physiologic inflammation within the bladder is commonly found, being able to minimize that inflammation through yoga techniques that activate the efferent vagus nerve (which releases acetylcholine) could help decrease urge UI symptoms. The breathing aspect of yoga can reduce UI symptoms as it modulates neuro-endocrine stress response symptoms, thus reducing activation of psychological and physiologic stress and inflammation associated with stress. The authors concluded the mind-body approach of yoga still requires systematic evaluation regarding its effect on pelvic floor dysfunction but offers a promising method for affecting inflammatory pathways.
In 2014, Tenfelde and Janusek considered yoga as a treatment for urge urinary incontinence in women, referring to it as a “biobehavioral approach.” The article reviews the benefits of yoga as it relates to improving the quality of life of women with urge urinary incontinence. Yoga may improve sympatho-vagal balance, which would lower inflammation and possibly psychological stress; therefore, the authors suggested yoga can reduce the severity and distress of urge UI symptoms and their effect on daily living. Since patho-physiologic inflammation within the bladder is commonly found, being able to minimize that inflammation through yoga techniques that activate the efferent vagus nerve (which releases acetylcholine) could help decrease urge UI symptoms. The breathing aspect of yoga can reduce UI symptoms as it modulates neuro-endocrine stress response symptoms, thus reducing activation of psychological and physiologic stress and inflammation associated with stress. The authors concluded the mind-body approach of yoga still requires systematic evaluation regarding its effect on pelvic floor dysfunction but offers a promising method for affecting inflammatory pathways.
Pang and Ali (2015) focused on complementary and alternative medicine (CAM) treatments for interstitial cystitis (IC) and bladder pain syndrome (BPS). Since conventional therapy has not been definitely determined for the IC/BPS population, CAM has been increasingly used as an optional treatment. Two of the treatments under the CAM umbrella include yoga (mind-body therapy) and Qigong (an energy therapy). Yoga can contribute to IC/BPS symptom relief via mechanisms that relax the pelvic floor muscle. Actual yoga poses of benefit include frog pose, fish pose, half-shoulder stand and alternate nostril breathing. According to a systematic review, Qigong and Tai Chi can improve function, immunity, stress, and quality of life. Qigong has been effective in managing chronic pain, although not specifically evidenced with IC/BPS groups. Qigong has also been shown to reduce stress and anxiety and activate the brain region that suppresses pain. The CAM gives a multimodal approach for treating IC/BPS, and this has been recommended by the International Consultation on Incontinence Research Society.
Evidence is emerging in every area of treatment these days, so it is only a matter of time before randomized controlled trials regarding alternative treatment methods for the pelvic floor begin to fill pages of our professional journals. Yoga, Qigong, Tai Chi, biologically based therapies, manipulative and body-based approaches, and whole medical systems all offer safe, effective treatment options for the IC/BPS and urinary incontinence patient populations. The more we use these extra treatment tools and document the results, the more likely we will see clinical trials proving their efficacy.
Tenfelde, S and Janusek, L. (2014). Yoga: A Biobehavioral Approach to Reduce Symptom Distress in Women with Urge Urinary Incontinence. THE JOURNAL OF ALTERNATIVE AND COMPLEMENTARY MEDICINE. 20 (10), 737–742. http://doi.org/10.1089/acm.2013.0308
Pang, R., & Ali, A. (2015). The Chinese approach to complementary and alternative medicine treatment for interstitial cystitis/bladder pain syndrome.Translational Andrology and Urology, 4(6), 653–661. http://doi.org/10.3978/j.issn.2223-4683.2015.08.10