
A recent article published in the Evidence Based Women's Health Journal reports on the use of transcutaneous electric nerve stimulation (TENS) for labor pain. The study was carried out in a teaching hospital in Cairo, Egypt, and involved 100 subjects divided into a treatment group (TENS application) and a control group (intramuscular pethidine 50-100 mg.) Pain assessment was completed by a visual analog scale (VAS) and a postpartum satisfaction questionnaire 48 hours after birth. Outcomes included relief of labor pain, duration of first stage of labor, labor augmentation, mode of delivery, fetal outcome, and adverse event reports. Patients were excluded in the following cases: cephalopelvic disproportion, multiple gestations, presence of a cardiac pacemaker, known congenital abnormalities, in the presence of complications such as preeclampsia, antepartum hemorrhage, and fetal asphyxia.
TENS was applied in the paravertebral area, between T10-L1 and S2-S4 at the time in labor when the woman experienced regular, painful contractions. In the control group, a gluteal intramuscular injection of meperidine hydrochloride (opioid analgesic) was applied every 4 hours or more as needed. For more details about the methods and results you can see the full text article by clicking here.
This randomized, controlled trial had groups similar in maternal age, gestational age, and parity. Results included both groups having a significant decrease in pain scores. However, the satisfaction surveys demonstrated a dramatic difference with the TENS group at 83% satisfaction rate, and only 10% in the control group. Reasons cited for dissatisfaction with the medication used by the control group included side effects of drowsiness, nausea and vomiting. Other results included decrease augmentation of labor needed in TENS group, mode of delivery and length of first stage of labor was similar among groups. Very compelling is the fact that Apgar scores were significantly higher in the TENS group despite all infants being healthy.
While it is appropriate and necessary to use caution when applying modalities with patients who are pregnant, this study offers further support about the efficacy of TENS for pain control in labor, and furthermore, this research highlights the perceived value of TENS use via satisfaction reports. (For a fantastic site to find evidence-based, current information about modalities, go to Tim Watson's website at www.electrotherapy.org) A woman's right to have a birth that is safe for her and her baby, with the added element of pain relief options that a laboring woman can choose for herself is critical. Healthy pregnancy, labor and delivery is a mission that the Pelvic Rehabilitation Institute includes in our mission, and Institute co-founder Holly Herman has led the field in educating therapists about peripartum rehabilitation across the United States (and now the world!) for decades.
This year we unveiled the Peripartum course series, designed by Holly Herman and faculty members Jenni Gabelsberg, Michelle Lyons, and Holly Tanner. Come join us at one of the courses focusing on Pregnancy, Postpartum, or Special Topics. Your next opportunity for each can be found here. We still have a few seats in the Care of the Pregnant Patient course in April in Illinois, Care of the PostpartumPatient course in March in California, and the next chance to take Peripartum Special Topics is in Texas in October.

This June, H&W is thrilled to be partnering with our dear friend, Fatima Hakeem, PT to bring a new course, The Business of Pelvic Rehab, to Denver, CO! This two-day course is intended for the clinician establishing or currently operating a women's health practice who would like to learn concrete skills for running his/her practice, including how to create a Business Plan, marketing to the community as well as physicians and hospital administrators, and recruiting and managing staff.
We sat down with Fatima to hear more about this great, new course.
PRR: What inspired you to create this course?
FH: For several years, I have been receiving calls and emails from therapists regarding the administrative piece of running a women’s health practice: questions on marketing, billing, regulatory requirements and business planning as they relate to women’s health. In addition, instructors that teach clinical courses consistently share with me that questions about the “admin” piece come up in every course. This course is a way to meet with these therapists face to face and help them start up and grow their women’s health service lines.
What resources and research were used when writing this course?
There are several text books on employee satisfaction, marketing to women, business planning, from which I have taken information and made it relevant to women’s health. I have attended several seminars put on by the Private Practice Section and bought several of their publications. I also have completed Billing and Coding courses.
Most importantly, I have set up two women’s health practices from “scratch” and have many years of experience dealing with regulatory requirements, physicians and patients. I have to say the mistakes I have made setting up two practices “from scratch” have been on my list of things to share with participants.
What can you tell us about this course that isn't covered in the description and objectives?
The course is designed, above all, to be practical and problem solving. We will spend time doing “labs”, meaning participants will not only leave with didactic information but with outlines of Business Plans and Marketing Plans.
Why should a therapist take this course? How can these skill sets benefit his/ her practice?
To have an effective practice that is financially viable, the business goals/skills and the clinical services must move in parallel. This seminar will help the therapist PLAN and EXECUTE a clinical women’s health program. The clinical courses offered are fabulous and allow the therapists to leave the courses with ready- to- implement clinical skills. However, those therapists may then find themselves stuck on the administrative aspects related to billing, G Codes, how to convince physicians to refer patients, how to handle patient complaints, and how to meet the corporate goals of productivity and quality. The skills learned in this course are effective, easy to implement and will help minimize these mistakes that are so easy to make along the way.
Want to learn more from Fatima? Join us in Denver in June!
Pelvic rehabilitation providers typically evaluate basic nutritional influences on a patient's bowel and bladder function. Instructing in dietary irritants, adequate and appropriate fluid intake (more water, less soda, for example and in the importance of whole foods and fiber's effects on the bowels is commonly included in a rehabilitation program. Although most therapists are not nutritionists, this level of patient education frequently improves a patient's function significantly, and has little potential for harm in the absence of medical conditions that may require fluid restriction, or avoidance of particular foods.
What is known about the impact of diet on commonly treated conditions? Consider interstitial cystitis, also known as painful bladder syndrome, and the varied experiences our patients report: for some, diet limitations dramatically control a patient's flare-ups, for others, there appears to be no rhyme or reason to diet and dysfunction. For patients who have irritable bowel syndrome (IBS research has suggested that a diet low in FODMAPS (fermentable oligosaccharides, disaccharides, monosaccharides, and polyols) may reduce the pain, bloating, and gastrointestinal symptoms in general. Other research describes the positive effect of the oligo-antigenic, sometimes described as a "severe" elimination diet, on the healing of chronic anal fissures.
The impact of nutrition on health and healing extends far beyond bowel and bladder dysfunctions as described above, but what is fact and what is fiction? Does the basic sciences research support the claims about nutrition's affects on pain and pelvic health? When is a pelvic rehabilitation provider obligated to refer a patient to a nutritionist or other provider? What resources are available to the clinician and to the patient when additional supportive services are not available? The Pelvic Rehabilitation Institute is thrilled to offer answers to all of the above questions through a new continuing education course on Nutrition Perspectives for the Pelvic Rehab Therapist that was written by Megan Pribyl, a physical therapist who also holds a dual-degree in nutrition and exercise sciences. From basic sciences, gastrointestinal anatomy, high-level functional nutritional concepts, to practical applications for the pelvic rehabilitation therapist, this course can provide the clinician with updated knowledge about the relationships and influences of nutrition on healing.
This course will be offered in Seattle, WA at the end of August- the perfect time to plan one last trip before back-to-school!

In 2013, H&W debuted a brand new course on Rehabiltation for the Breast Oncology Patient. This coming year, we are thrilled to be offering this course on the West Coast, in San Diego in April. Pelvic Rehab Report talked to course author and instructor Susannah Haarmann, PT, CLT, WCS about what she learned from teaching this course for the first time and what she looks forward to sharing with participants this year.
PRR: You developed and started teaching this course for the first time in 2013. What did you learn from your first time teaching this course?
SH: I learned that the breadth of topics that ought to be covered in order to present a holistic approach to rehabilitation and breast oncology is gigantic! I was inspired to teach this course because, from my perspective, in most clinics and hospitals, the vast concerns of breast survivors regarding physical well-being and quality of life are not being addressed. I turned to mentors for guidance, but their knowledge had holes. I probed the research, but the information pertaining to rehabilitation seemed disjointed. I sought out continuing education, however, the topics covered were not as complete and detailed as I would have preferred.
In summary, I learned teaching in 2013 that I bit off a lot to chew! Feedback from the course was largely optimistic, however, I have made huge modifications. The course material has been reorganized from a 3-day to 2-day course. Although the course is still steeped in research, the content has been stream-lined. I have also included more labs with pertinent case scenarios for didactic learning and skills development.
Were there any surprises? How did feedback from participants inform the evolution of this course as you prepare to teach in 2014?
I was surprised by the variability in course participants! There were physical therapists and occupational therapists, women’s health practitioners, travelling physical therapists and certified lymphedema therapists, outpatient practitioners and acute care therapists…the perspectives that we had during the debut course was incredible! I treat breast cancer survivors on an outpatient basis, but feedback from the acute care therapists helped me address post-surgical and inpatient issues. Furthermore, I am a certified lymphedema therapist (CLT) trained by the Norton School of Lymphedema, however, there were also Leduc trained CLTs present as well. Interacting with these practitioners broadened my awareness of lymphedema treatment approaches.
Finally, the labs included in this course are broad in scope; they require us to pull from our basic knowledge of cardiopulmonary, integumentary and neuromuscular systems knowledge. Many participants were glad to sharpen their skills in orthopedic testing of the shoulder or vitals assessment and interpretation. In order to be experts, sometimes we have to perfect the basics- Be prepared to call on your generalist wisdom!
What were the most common questions asked by participants during the course? How does the course address frequent questions/misconceptions therapists might have about this topic?
I would say that many of the therapists were inspired by the idea of a health care team that became familiar with the client from the time of diagnosis through the ‘re-entry’ phase into long-term survivorship. Participants wanted to know how to facilitate the practice of the prospective surveillance model in their communities and develop relationships with physicians.
I think that a frequent misconception about breast oncology rehabilitation is that it just addresses lymphedema. In most cases, all bodily systems are affected by treatments related to breast cancer; some rear their heads during the acute phase, whereas other side effects become noticeable with the aging process. We as rehabilitation professionals are able to work with various body systems across the continuum of care. If you take this course be prepared to learn about treating post-surgical side effects such as lymphatic cording, muscle imbalances and post-mastectomy pain syndrome. Get ready to dig into treating side effects of chemotherapy such as peripheral neuropathy, fatigue, osteoporosis and dyspareunia. Learn about rehabilitation considerations pertaining to radiation such as integumentary and potential cardiopulmonary changes. But, we won’t stop there! Behind every ‘body’ is a person; you will also be exposed to what the research says about how medical interventions can affect the psyche and how methods such as mindfulness based stress reduction can not only improve personal well-being, but also affect cancer outcomes.
Want to learn more from Susannah? Check her out in San Diego, April 12-13!
A recently published review about peripartum management of gestational diabetes mellitus (GDM) confirms that use of recommended guidelines, testing, and follow-up "…seems suboptimal at best and arbitrary at worst." Despite the fact that during pregnancy, a mother and her fetus experience health risks related to gestational diabetes, screening remains low across countries and study settings. Once a woman is diagnosed with GDM, she is at risk for developing postpartum Type II diabetes. The necessary follow-up testing is also not consistently completed, and many new mothers are challenged by recommended lifestyle modifications.
Unfortunately, women who develop gestational diabetes may not have any symptoms. Medical providers typically screen for GDM with an oral glucose tolerance test between weeks 24-28, or earlier if risk factors are present. According to Medline Plus, excessive thirst or increased urination may be present as a symptom. Blurred vision, fatigue, weight loss despite increase in appetite, frequent infections, or nausea and vomiting may also occur. A common challenge of diagnosing women with disease conditions during the peripartum period is that symptoms such as fatigue, nausea, or changes in hunger and thirst may occur as a typical part of pregnancy or the postpartum period, so a woman may not report all symptoms to her provider. Risk factors for patients in developing gestational diabetes can include age over 25, having a family history of diabetes, giving birth to a child weighing greater than nine pounds, having high blood pressure, or a high body mass index (BMI) prior to pregnancy.
What is the potential impact for pelvic rehabilitation providers who work with women during the prenatal or postpartum period? Because women who develop GDM often have larger babies, there may be an increased risk of a cesarean section, or injury to the pelvis during childbirth. While pregnant, a woman with GDM may have elevated blood pressures. In the postpartum period, the risk for developing Type II diabetes increases, yet may not develop for 5-10 years. Medical providers and patients each experience barriers to screening and follow-up, as described in the open access article available here. Barriers for health care providers can include not seeing the patient during the screening period, not having appropriate resources available for testing, lack of coordination between different providers, and patient refusal of the test. Even if a woman is identified early as having gestational diabetes, and is informed about appropriate diet and exercise modifications that will reduce the risk of developing Type II diabetes in the postpartum period, poor self-efficacy and social support may limit a woman from achieving her desired goals.
As is often asked regarding review of articles in this blog, what is the role of the pelvic rehabilitation provider? If a rehab provider is aware of the risks for the condition, we can respectfully inquire if the patient has been screened, and encourage her to follow-up during the 24-28 week window as needed. If a woman complains of fatigue or blurred vision, or changes in her habits that "don't seem right" to the provider or the patient, a referral to the managing medical provider can be made. During the postpartum period, providing community education, health and wellness screening, or clinical screening can be completed. It is necessary for rehab therapists to assist in identifying barriers to exercise and proper nutrition, and coordinate with a patient's resources as able. Having a support team such as nutritionists, exercise therapists, and social services can have a positive impact, as many women are focused on the daily acts of raising a child and have too little focus on their own health.
If you are interested in learning more about the prenatal period, the postpartum recommendations for gestational diabetes, and exercise prescription, find out which of the Perinatal Series of continuing education courses fits into your schedule. (These courses do not need to be taken in any particular order. )Therapists will find a blend of evidence-based support related to peripartum issues as well as evaluation and intervention techniques to apply in the clinic. The next Care of the Pregnant Patient takes place in April in Maywood (near Chicago Care of the PostpartumPatient is in Oakland, CA, in March, and the next Peripartum Special Topics course happens in Texas in October.
Throughout the Guidelines on Chronic Pelvic Pain created by the European Association of Urology, the recognition of anxiety and depression as a concomitant symptom of chronic pelvic pain is made. Various types of pelvic dysfunctions have been demonstrated to have an association with anxiety and depression, including urethral pain, chronic pelvic pain, anorectal disorders, and sexual dysfunction. While a first line of medical treatment for patients who complain of neuropathic pain type, according to the Guidelines, is the prescribing of antidepressants, there are other interventions identified in the literature for alleviating anxiety and stress related to chronic pain. One of the studied interventions for pain, anxiety, and stress is yoga.
In a systematic review and meta-analysis for yoga and low back pain (which is also a common comorbidity of pelvic pain) yoga was found to have "…strong evidence for short-term effectiveness and moderate evidence for long-term effectiveness…" and the study concludes that yoga can be recommended for patients who have chronic low back pain. In this review of ten randomized controlled trials including 967 subjects with chronic low back pain, no serious adverse events were reported. A report in the journal Alternative Medicine Review states that yoga, which may be considered an adjunct therapy for stress and anxiety, is supported by good compliance among patient populations and a lack of drug interactions. The same study states that better research is needed before strongly recommending yoga for the specific purposes of reducing anxiety and stress. The current research is plagued with common statistical challenges: lack of a control group, variations in studied physiological markers, lack of validated scales, and heterogenous study populations.
For the pelvic rehabilitation provider, having a working knowledge of common yoga terminology and postures can assist in modification or adaptation of a patient's current routine. In addition, learning to apply yoga concepts and postures such as breathing, trunk and pelvic coordination, soft tissue lengthening within a patient's comfort can add to a pelvic rehab provider's toolbox. There is room for you to join Dustienne Miller, physical therapist and yoga instructor, in California at the Yoga for Pelvic Pain course. Contact the Pelvic Rehabilitation Institute if you have any questions about this continuing education course.
For patients who are diagnosed with constipation, functional anorectal testing is often completed prior to referral for physical therapy. A recent study concluded that clinical examination of pelvic floor muscle function is critical for identifying a rectocele or pelvic muscle overactivity, and that anorectal function tests should be reserved for selected cases. Pelvic rehabilitation therapists are able to perform tests of the pelvic muscles and function during a patient's attempts to contract, relax, and bear down through the pelvic floor. These tests are easy to repeat and a patient can be instructed in corrective muscle techniques to improve the ability to empty the bowels.
Consider the patient who presents to the clinic after experiencing a defecography. In this test, a patient undergoes an imaging study while sitting on an elevated toilet seat. The patient is asked to bear down to evacuate a bolus of material that is placed inside the rectum. It is easy to understand why a patient finds this test to be "embarrassing." Following this test, when a patient is diagnosed with dyssynergia (when the puborectalis muscle contracts rather than lengthening and relaxing during attempt to defecate) he or she is frequently referred to pelvic rehabilitation. A pelvic rehab therapist can observe and palpate the same phenomena in the clinic: when asked to bear down or drop the pelvic floor muscles, if a patient instead contracts or is unable to lengthen the muscles, re-training can be implemented.
I have often wondered why a patient would need to complete this type of testing for constipation-related pelvic muscle dysfunction if the same patient could reverse a dysfunctional muscle pattern with a brief bout of pelvic rehabilitation. The research by Lam and Felt-Bersma (full-free text article linked above) appears to confirm this thought, concluding that anorectal functional testing contributes little to information that can be gained in clinical examination in women who have idiopathic constipation.
The authors studied 100 women who were diagnosed with idiopathic constipation and who fit the Rome III criteria. A prospective evaluation included an extensive questionnaire regarding complaints, abdominal, rectal, and vaginal examination, and anorectal function tests such as anorectal manometry (ARM)and anal endosonograpy (AUS). Exclusion criteria included inflammatory bowel disease, fissures, or fistula, and endocrine disorders orcolonic obstruction were ruled out. Of these 100 women, 25% were found to have hypertonia and dyssynergia of the pelvic floor, and 15% presented with a rectocele. During anorectal manometry, the authors also noted that women had difficulty relaxing during straining. In the group studied, 37 women complained of impaired evacuation, and interestingly, 40% of these women had a rectocele, yet no rectoceles were identified in the women who did not complain of impaired evacuation.
While medical screening for patients who complain of constipation is important, this research identifies a group of patients (those diagnosed with idiopathic constipation) for whom ARM or AUS testing does not contribute significantly to the evaluative process. The study is very valuable reading for pelvic rehabilitation providers as the authors clearly understand the role of rehabilitation and articulate the value ofpelvic floor muscle function in meaningful ways throughout the report. If you are interested in learning how to evaluate and treat patients who have constipation, there are 3 seats remaining in the PF2A continuing education course at the end of this month in Fairfield, California (right next to Napa, in case that interests you!) The PF2A course covers bowel dysfunction such as constipation, fecal incontinence, and other colorectal conditions, and also offers on Day 3 an Introduction to Male Pelvic Floor function and dysfunction related to pelvic pain and urinary dysfunction. Following the West coast PF2A, there are East coast and Midwest dates, click here to find the course information. Sign up early as this course always sells out!
Treating patients who have chronic pelvic pain is challenging for many reasons. The nature of chronic pain in any body site often means that the patient has a multifactorial presentation that requires a team approach to interventions. And because the pelvis also contains the termination of several body systems such as the urologic, reproductive, and gastrointestinal, there exists potential for addressing a musculoskeletal issue that is masking a medical issue which requires intervention by a medical provider. The phrase "When you have a hammer, everything looks like a nail" can be applied to patient care for any discipline. When a patient presents with chronic pelvic pain, pelvic rehabilitation therapists can usually find tender pelvic muscles to treat. Is the pelvic muscle tenderness from guarding due to visceral pain or infection?
In a 2013 article in the journal General Practitioner, Dr Croton describes red flag symptoms in acute pelvic pain. These include pregnancy, pelvic or testicular masses, and vaginal bleeding and/or pain in postmenopausal women. During the history taking, patients can be asked about menstrual patterns, possibility of pregnancy, and sexual history. Further medical evaluation may include a pregnancy test, ultrasound, laparoscopy, and urine tests to rule out infection. While the above is not an exhaustive list, it reminds the pelvic rehabilitation provider to always keep in mind the potential for medical evaluation and intervention. Once a patient has been deemed to have "only chronic pelvic pain," a new, equally challenging list emerges: is the pain generated by an articular issue, myofascial dysfunction, neuropathy, psychological stress, or postural pattern? Is the pain local, such as in the pubis symphysis or in the sacroiliac joint ligaments, or are the symptoms referred from a nearby structure, such as the abdominal wall or the thoracolumbar junction? And what are the best methods to examine in a systematic way the various theories about the origins of a patient's pain?
Peter Philip has created a course to provide answers to the above questions. He combines skills in both orthopedics and manual therapy, and pulls from an extensive knowledge about pelvic pain and differential diagnosis which was the research topic of his Doctor of Science degree. Peter's course provides clearly instructed techniques in anatomical palpation, spinal and joint assessment, and he also instructs in how the nervous system and cognition can impact a patient's perception of pain. The course will be offered at the end of this month in Seattle- don't miss this chance to refine skills in differential diagnosis for chronic pelvic pain!
As I looked through this post by an accomplished yoga instructor on the "Top 10 Yoga Postures for Strength," I tried to look at the words and images through the eyes of our typical patients. The chosen postures made the list as they contained foundational "alignment and strength needed to master many more advanced postures." While this may be true for some, I can easily imagine the trouble that most of my patients would find by attempting to cruise through the demonstrated techniques. With jump backs, headstands, handstands, and one arm side planks, there is little caution made about hyper extensibility, about "gripping" postures as Diane Lee explains so well, or about compensatory patterns that can cause strain or injury.
The yoga instructor is not to be blamed- any magazine, blog post, or website that sells fitness or wellness attempts to package information to the public in attractive and efficient methods. An impressively toned, graceful, and high-level yoga practitioner is perfect for such a marketing goal. Unfortunately, any person reading an instructor's guide to finding your physical strength does not have said instructor giving the required feedback about joint position, compensations, and necessary modifications or starting postures.
Patients everywhere espouse the benefits of a yoga practice, and we all have likely met someone whose life was drastically changed for the better after finding yoga. Can yoga also be the cause of an injury? I recall entering a new yoga class at a gym (where the instructor had created a "guru" type following) and I was horrified at the instructor's lack of restraint in guiding a room of 70 or more students through very advanced poses that they were simply expected to push themselves through. The students wore their suffering like a badge, telling each other to "stick it out" as they would keep getting stronger. The instructor then approached me and, without knowing anything about me or my body, twisted me aggressively into a posture that I quickly unraveled as soon as she moved away. As if students cannot find enough ways to push the body outside of a comfort zone, having an instructor violate basic safety principles (was I returning to yoga after a spinal surgery?) adds to the potential for injury.
In a systematic review of adverse events associated with yoga, Cramer, Krucoff & Dobos describe musculoskeletal injuries such as fractures, ligament tears, joint injuries, disc annular tears, and several cases related to breathing techniques. Headstands were a common method for acquiring a yoga-related injury. The authors suggest that for patients who have physical or mental ailments, yoga can be adapted to a patient's "…needs and abilities and performed under the guidance of an experienced and medically trained yoga teacher."
While yoga does not need to be discouraged, we may need to consider the patient's abilities and challenges, and be familiar with our community resources prior to suggesting that a patient begin yoga. If you are more interested in advancing your own practice and in learning how to apply yoga principles and postures to your patient populations, the Institute has several means to accomplish this. For patients who have pelvic pain, Dustienne Miller will teach Yoga for Pelvic Pain in March, where you can learn how to tailor specific yoga techniques for specific patient presentations and conditions. You can also check out Ginger Garner's live and on-line yoga courses by clicking here (scroll down to Yoga as Medicine).
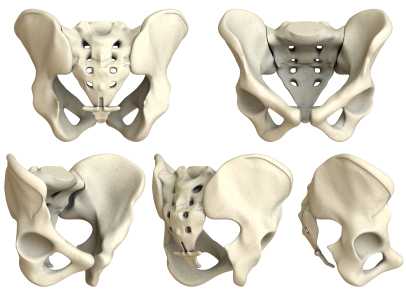
Are sacroiliac joint injections useful for our patient population? A 2013 review article, available here, concludes that current literature "…is unable to fully conclude the effectiveness of the modality and provide adequate comparison against surgical treatment." The above linked article provides a description of fluoroscopy-guided sacroiliac joint injections that can be used for both diagnostic and for therapeutic purposes.
According to the article, a guided injection may be indicated in a patient who has known sacroiliac joint pathology, a history of trauma, or referred symptoms into the buttock or lower extremity. Contraindications can include pathology of coagulation, pregnancy (due to radiation effects), systemic or local skin infection, or patient allergies to medication. During the procedure, a local anesthetic is utilized, and the patient is minimally sedated so that he or she is able to answer questions about pain. Both a pain-reducing medication and an anti-inflammatory are typically utilized; however, in patients who have received a maximum level of steroids, only an analgesic may be injected.
Results of an injection may include provocation of symptoms and/or immediate relief, which provides diagnostic value, i.e., that the structures injected may have, in fact, been causative to the patient's symptoms. For many patients, pain relief occurs within 24 hours. The long-term benefits of sacroiliac joint injections is not well-documented, so the ability to predict length of benefit is challenging.
In regards to rehabilitation of the patient who has undergone a sacroiliac joint injection, following a procedure, the patient is usually instructed to rest for 3-4 days and to follow-up with the referring medical provider within 2-3 weeks. The level at which a patient should resume physical activity, therapeutic exercises, and participation in physical therapy is determined by the medical provider. Level of activity in rehabilitation should therefore be coordinated with the patient's medical provider and potentially with the interventionist who performed the injection.
For more information about sacroiliac joint injections, check out this MedScape article about the topic, or clickhereto view a video of an SIJ injection. To learn clinical information about SIJ evaluation, mobilization, and stabilization activities, check out the next Sacroiliac Joint & Pelvic Ring Dysfunctioncontinuing education course taught by Pelvic Rehabilitation Institute faculty member Peter Philip. This course will be offered two times this year; coming up in early February on the West coast (Santa Barbara, CA) and in July on the East coast (Baltimore, MD.) Click here to learn more about the course objectives and schedule.
By accepting you will be accessing a service provided by a third-party external to https://hermanwallace.com/










































