Treating patients who have chronic pelvic pain is challenging for many reasons. The nature of chronic pain in any body site often means that the patient has a multifactorial presentation that requires a team approach to interventions. And because the pelvis also contains the termination of several body systems such as the urologic, reproductive, and gastrointestinal, there exists potential for addressing a musculoskeletal issue that is masking a medical issue which requires intervention by a medical provider. The phrase "When you have a hammer, everything looks like a nail" can be applied to patient care for any discipline. When a patient presents with chronic pelvic pain, pelvic rehabilitation therapists can usually find tender pelvic muscles to treat. Is the pelvic muscle tenderness from guarding due to visceral pain or infection?
In a 2013 article in the journal General Practitioner, Dr Croton describes red flag symptoms in acute pelvic pain. These include pregnancy, pelvic or testicular masses, and vaginal bleeding and/or pain in postmenopausal women. During the history taking, patients can be asked about menstrual patterns, possibility of pregnancy, and sexual history. Further medical evaluation may include a pregnancy test, ultrasound, laparoscopy, and urine tests to rule out infection. While the above is not an exhaustive list, it reminds the pelvic rehabilitation provider to always keep in mind the potential for medical evaluation and intervention. Once a patient has been deemed to have "only chronic pelvic pain," a new, equally challenging list emerges: is the pain generated by an articular issue, myofascial dysfunction, neuropathy, psychological stress, or postural pattern? Is the pain local, such as in the pubis symphysis or in the sacroiliac joint ligaments, or are the symptoms referred from a nearby structure, such as the abdominal wall or the thoracolumbar junction? And what are the best methods to examine in a systematic way the various theories about the origins of a patient's pain?
Peter Philip has created a course to provide answers to the above questions. He combines skills in both orthopedics and manual therapy, and pulls from an extensive knowledge about pelvic pain and differential diagnosis which was the research topic of his Doctor of Science degree. Peter's course provides clearly instructed techniques in anatomical palpation, spinal and joint assessment, and he also instructs in how the nervous system and cognition can impact a patient's perception of pain. The course will be offered at the end of this month in Seattle- don't miss this chance to refine skills in differential diagnosis for chronic pelvic pain!
As I looked through this post by an accomplished yoga instructor on the "Top 10 Yoga Postures for Strength," I tried to look at the words and images through the eyes of our typical patients. The chosen postures made the list as they contained foundational "alignment and strength needed to master many more advanced postures." While this may be true for some, I can easily imagine the trouble that most of my patients would find by attempting to cruise through the demonstrated techniques. With jump backs, headstands, handstands, and one arm side planks, there is little caution made about hyper extensibility, about "gripping" postures as Diane Lee explains so well, or about compensatory patterns that can cause strain or injury.
The yoga instructor is not to be blamed- any magazine, blog post, or website that sells fitness or wellness attempts to package information to the public in attractive and efficient methods. An impressively toned, graceful, and high-level yoga practitioner is perfect for such a marketing goal. Unfortunately, any person reading an instructor's guide to finding your physical strength does not have said instructor giving the required feedback about joint position, compensations, and necessary modifications or starting postures.
Patients everywhere espouse the benefits of a yoga practice, and we all have likely met someone whose life was drastically changed for the better after finding yoga. Can yoga also be the cause of an injury? I recall entering a new yoga class at a gym (where the instructor had created a "guru" type following) and I was horrified at the instructor's lack of restraint in guiding a room of 70 or more students through very advanced poses that they were simply expected to push themselves through. The students wore their suffering like a badge, telling each other to "stick it out" as they would keep getting stronger. The instructor then approached me and, without knowing anything about me or my body, twisted me aggressively into a posture that I quickly unraveled as soon as she moved away. As if students cannot find enough ways to push the body outside of a comfort zone, having an instructor violate basic safety principles (was I returning to yoga after a spinal surgery?) adds to the potential for injury.
In a systematic review of adverse events associated with yoga, Cramer, Krucoff & Dobos describe musculoskeletal injuries such as fractures, ligament tears, joint injuries, disc annular tears, and several cases related to breathing techniques. Headstands were a common method for acquiring a yoga-related injury. The authors suggest that for patients who have physical or mental ailments, yoga can be adapted to a patient's "…needs and abilities and performed under the guidance of an experienced and medically trained yoga teacher."
While yoga does not need to be discouraged, we may need to consider the patient's abilities and challenges, and be familiar with our community resources prior to suggesting that a patient begin yoga. If you are more interested in advancing your own practice and in learning how to apply yoga principles and postures to your patient populations, the Institute has several means to accomplish this. For patients who have pelvic pain, Dustienne Miller will teach Yoga for Pelvic Pain in March, where you can learn how to tailor specific yoga techniques for specific patient presentations and conditions. You can also check out Ginger Garner's live and on-line yoga courses by clicking here (scroll down to Yoga as Medicine).
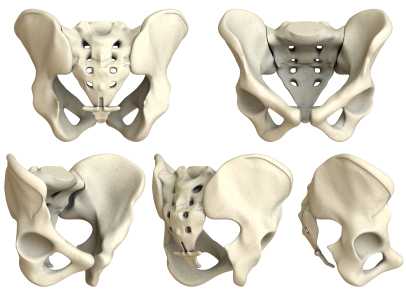
Are sacroiliac joint injections useful for our patient population? A 2013 review article, available here, concludes that current literature "…is unable to fully conclude the effectiveness of the modality and provide adequate comparison against surgical treatment." The above linked article provides a description of fluoroscopy-guided sacroiliac joint injections that can be used for both diagnostic and for therapeutic purposes.
According to the article, a guided injection may be indicated in a patient who has known sacroiliac joint pathology, a history of trauma, or referred symptoms into the buttock or lower extremity. Contraindications can include pathology of coagulation, pregnancy (due to radiation effects), systemic or local skin infection, or patient allergies to medication. During the procedure, a local anesthetic is utilized, and the patient is minimally sedated so that he or she is able to answer questions about pain. Both a pain-reducing medication and an anti-inflammatory are typically utilized; however, in patients who have received a maximum level of steroids, only an analgesic may be injected.
Results of an injection may include provocation of symptoms and/or immediate relief, which provides diagnostic value, i.e., that the structures injected may have, in fact, been causative to the patient's symptoms. For many patients, pain relief occurs within 24 hours. The long-term benefits of sacroiliac joint injections is not well-documented, so the ability to predict length of benefit is challenging.
In regards to rehabilitation of the patient who has undergone a sacroiliac joint injection, following a procedure, the patient is usually instructed to rest for 3-4 days and to follow-up with the referring medical provider within 2-3 weeks. The level at which a patient should resume physical activity, therapeutic exercises, and participation in physical therapy is determined by the medical provider. Level of activity in rehabilitation should therefore be coordinated with the patient's medical provider and potentially with the interventionist who performed the injection.
For more information about sacroiliac joint injections, check out this MedScape article about the topic, or clickhereto view a video of an SIJ injection. To learn clinical information about SIJ evaluation, mobilization, and stabilization activities, check out the next Sacroiliac Joint & Pelvic Ring Dysfunctioncontinuing education course taught by Pelvic Rehabilitation Institute faculty member Peter Philip. This course will be offered two times this year; coming up in early February on the West coast (Santa Barbara, CA) and in July on the East coast (Baltimore, MD.) Click here to learn more about the course objectives and schedule.
At the end of this month, Herman & Wallace instructor Michelle Lyons, BSc Physio, PT, MISCP will be teaching our Pelvic Floor Level One course at Coventry University in the United Kingdom.
H&W teamed up with Gerard Greene, MSc (Manip Physio), MMACP, MCSP, PG Cert HEd to put on this course. Below is a guest blog from our friend across the pond, Gerard, about his experience putting on an H&W PF1 event:
There has been a lot of buzz and excitement in UK Physiotherapy circles about the first Herman & Wallace PF1 course.
The majority of Physiotherapists attending this course will be from England, but we also have participants flying in from Northern Ireland, Portugal and Cypress. The participants have a range of clinical backgrounds, including working in the UK National Health Service (NHS), private hospitals and private practice. There will also be some University- based Physiotherapy lectures. What will really make the PF1 course unique will be the attendance of some Midwifery Lecturers. It is hoped that the Physiotherapy/ Midwifery synergy on the course will lead to some joint projects in 2014, which will only further improve patient care and outcomes.
Women’s Health in the UK has been getting increasing profile in both the media and the professional literature with two key publications recently on NICE guidelines for Stress Incontinence and a Cochrane review for management of Pregnancy related pelvic and LBP.
As the course organiser, I was able to generate a lot of energy and momentum around the course through the use of social media such as Twitter, Facebook and Linkedin. Although the Twitter community around pelvic rehab and women’s health physiotherapy is well established in the USA and Australia, it is in it’s infancy in the UK.
Patterson Medical, the biggest supplier of Physiotherapy and rehab equipment in the UK, will be supplying the EMG devices so that participants can learn to use this modality.
Michelle and I also share an Irish connection, as we both graduated from Physiotherapy School in Dublin, Ireland in 1994; Michelle from University College Dublin and me from Trinity College Dublin. Although both Universities were seen as traditional rivals, in the Physiotherapy world this common ground has been a real bonus in the development of our professional relationship. Michelle is a recognized expert in Women’s Health Physiotherapy and she and I have worked closely in organizing the UK course, as well as further plans for the development of Women’s Health Physiotherapy education and training in the UK in 2014. Working with instructor Michelle Lyons, and H&W team members Siv Prince and Derek Huff has been a very positive and energizing experience, and I’m already looking forward to the next joint event.

Gerard has a musculoskeletal physiotherapy background and has taught and delivered Physiotherapy courses in Ireland, N Ireland, England, Scotland, Wales, Turkey and Jordan. Gerard is looking forward to doing some further teaching in the Middle East and the USA next year. He also lectures on the MSc Manual Therapy Programme in Coventry University which has a national and international reputation for excellence. H&W is very much looking forward to working with him on this course and in the future!
A recent study asked if transcutaneous electrical nerve stimulation (TENS) can be a helpful treatment for men who have refractory chronic pelvic pain. 60 men completed pain diaries and the National Institutes of Health Chronic Prostatitis Symptom Index (NIH-CPSI) at baseline, after 12 weeks of TENS treatment, and at last known follow-up. The mean age of the subjects was 46.9 years. TENS was measured as an effective treatment in nearly half of the men, and the benefits of the treatment were sustained during a mean follow-up of 43.6 months in 21 of 29 patients. The primary measurement tool for pain, the Visual Analog Scale, or VAS, significantly decreased from 6.6 to 3.9. Quality of life measurement was also improved, with more men feeling mostly satisfied, pleased, or delighted versus dissatisfied, unhappy, or terrible.
What's the take home message? Regardless of the limitations of the study (non-randomized, non-placebo), TENS was found to be a safe and effective treatment without any adverse responses within this study. As a means of neuromodulation, which we know is critical in conditions of chronic pain, the application of electrotherapy is inexpensive, low-risk, and is a useful tool in the healing process. That healing process should include therapies that the patient can apply himself, so that he recognizes his own capacity and necessity for participating in recovery of function.
As there are few studies that address electrotherapy only for chronic pelvic pain, this research is useful in adding some weight to our clinical choices in modality use. Does a patient need to utilize TENS for 12 weeks to determine efficacy? Probably not, but this is an easy modality that can be trailed in the clinic, and utilized as a home program tool if recorded as beneficial for the patient.

Following H&W founder Holly Herman's amazing presentation at the North American Menopause Society's Annual Meeting, Holly sat down with Dr. Mache Seibel to talk pelvic rehab and the role of the PT in treating patients with bladder, bowel and sexual dysfunction.
You can watch the interview HERE
According to NAMS, the attendance at the annual meeting was over 70% physicians and 13% nurses. Physical therapists and "other professionals" made up only 8% of attendace, so kudos to Holly for spreading the gospel about the important role of the PT in women's health!
Want to catch more Holly? She'll be teaching Pelvic Floor Level One, Pelvic Floor Level Three, Care of the Pregnant Patient, Care of the Postpartum Patient, and Peripartum Special Topics in 2014!

This March, H&W is launching a brand new course on Oncology and the Male Pelvic Floor. This course was developed by H&W faculty member Michelle Lyons, PT, MISCP.
Pelvic Rehab Report sat down with Michelle to learn more about her course.
PRR: What inspired you to create this course?
ML: I am very passionate about oncology rehab and pelvic physical therapy. While it has been great to see the huge advancements being made in the provision and recognition of pelvic physical therapy, I often feel that cancer survivors don’t always get the treatment they deserve – they don’t fall exclusively into the domain of the pelvic therapist or the oncology therapist. Add to this the lack of awareness in the medical community about the benefits of physical therapy generally (and pelvic physical therapy especially) and it becomes obvious that a lot of pelvic oncology patients, both men and women, have many issues that we can help address. The first step is creating awareness, both with our medical colleagues and with cancer survivors, about the benefits of physical therapy
What resources and research were used when writing this course?
I like to use a wide range of resources when creating a course. My main priority was to determine if there was a need for this service – I visited cancer survivorship websites and forums and asked on various social media sites, as well as talking to medical and therapy colleagues, about their opinions on the topic. The answer was a resounding ‘We need this!’
I read hundreds of journal articles, interviewed healthcare professionals and patients as well as drawing on my own professional experience. I want this course to be based on the best evidence based medical practice out there, but more importantly, I want to make the information immediately clinically applicable, so there will be a generous allotment of time to discussing and practising manual therapy techniques and exploring different ideas for exercise prescription. I believe we are all students and we are all teachers; I know I learn something new every time I teach, so I am really hoping these classes will be a forum to get therapists brainstorming and planning how best to serve this community
Can you describe the clinical/treatment approach/techniques covered in this continuing education course?
We will be looking at how to apply the skills we have to help problem solve pelvic issues such as bladder, bowel and sexual dysfunction, but also thinking about the sequelae and complications of cancer treatments such as osteoporosis, fatigue and cognitive changes. I want to discuss the necessary precautions and contraindications we need to be aware of but also to look at how to develop the skillset we already have to really enhance cancer survivors’ quality of life
Why should a therapist take this course? How can these skill sets benefit his/ her practice?
Fortunately, we are seeing more people living longer lives as cancer survivors – there have been huge advances in the treatment of many pelvic cancers. But these treatments do have side effects that impact on the pelvic health of the many men and women who battle pelvic cancers. We are the experts in pelvic rehabilitation and I think we need to expand our skillsets to offer cancer survivors access to our expertise. The many exciting changes we are seeing in cancer care means that therapists need to be able to not only assess, treat and educate cancer survivors but also to be able to show that the work we do has a body of research to demonstrate the value of what we do. I think developing an expertise in pelvic oncology will be of huge value to a therapist’s repertoire of marketable skills, but I can also tell you that working with pelvic cancer survivors will be one of the most rewarding aspects of your career. You will literally be changing people’s lives.
The course will be offered January 25-26 in San Diego, CA. Don't miss this brand new offering - Register today!
The Pelvic Rehabilitation Practitioner Certification test, or PRPC, is a certification that was developed to recognize expertise in the field of male and female pelvic rehabilitation. Until now, there is no other test available for therapists who wish to establish to their patients and to the community such expertise. As the applications come in to the Institute for review, one common question we hear is "How should I study for the exam?" There is no right answer to this question, as each therapist will need to decide what content areas of knowledge and skills are fresh versus needing an update.
The PRPC examination contents are broken down into 8 different domains. The 150 items or questions on the test will be based on these domains in the ratios shown below.
|
Anatomy |
22-23 items |
(15%) |
|
Physiology |
30 items |
(20%) |
|
Pathophysiology |
30 items |
(20%) |
|
Pharmacology |
7-8 items |
(5%) |
|
Medical Intervention & Tests |
7-8 items |
(5%) |
|
Tests & Measures |
15 items |
(10%) |
|
Interventions |
30 items |
(20%) |
|
Professional & Legal |
7-8 items |
(5%) |
When you consider the above categories, think of how each applies to pelvic rehab. In other words, while it may be helpful for you to have an exceptional knowledge base about the elbow, unless we are relating elbow anatomy, pathophysiology, or interventions to pelvic rehab, you can rest assured that items are not built around knowledge of the elbow. On the other hand, if a medical intervention, such as a surgery or medication, has an implication for pelvic rehabilitation, the examination can include such content. Topics that will not be directly tested on the examination include documentation, billing, the mechanisms of diagnostic testing such as urodynamics, marketing, or techniques outside of our scope such as prostate examination.
In terms of preparing for the certification test, upon approval of the application, a therapist will be sent documents that include information upon which the examination is built. The Job Tasks Analysis and the test Blueprint will be sent to the applicant, and the Blueprint contains more detailed topics within each of the domains listed in the above chart. Keep in mind that all topics were chosen through a rigorous process to represent the body of work in pelvic rehabilitation. There is no particular coursework that is required for this certification. You can be included on a list of participants interested in sharing contact details for a study group- this request is a part of the application process. The Institute also recently developed a page on the website listing resources that the pelvic rehabilitation provider may find helpful in locating sources of information. Keep in mind that this page will be continually developed, so check back often for links to articles and abstracts. For other questions about the PRPC examination, or to download an application, click here to access the website page for PRPC. Please contact the Institute directly by phone or email for any other questions.
Lumbopelvic and pelvic girdle pain (PGP) in pregnancy is estimated to occur in 20-30% of women, with prevalence as high as 50%. (Elden et al., 2013; Gutke et al., 2006; Mens & Pool-Goudzwaard, 2012; Ostgaard, 1991; Vleeming et al., 2008) One in four women who develop PGP in pregnancy develop chronic postpartum pain. (Ostgaard, 1991) According to Albert et al., 2006, risk factors for developing pelvic girdle pain in pregnancy include history of prior low back pain, back or pelvic trauma, high levels of stress, multiparity, and low job satisfaction. Non-risk factors include contraceptive medications, time since past pregnancy, height, weight, and smoking. (Vleeming et al., 2008) Fortunately, there is a trend for PGP to decrease within the first 3 months of delivery. (Elden et al., 2008) For pain that does persist, guidelines for treating pelvic girdle pain include providing individualized exercise prescription. (Vleeming et al., 2008) What type of individualized exercise or other intervention is appropriate?
A recent study by Elden and colleagues (2013) assessed the effect of including craniosacral therapy to standard treatment for pregnant women with pelvic girdle pain. In the multicenter, randomized, single blind, controlled trial, 123 patients were treated, with 60 in the control group and 63 in the intervention group. Standard treatment included education about the condition and anatomy of the back and pelvis, instruction in concepts of load demand and rest, activities of daily living advice, instruction in use of pelvic support belt, and exercises to stretch and strengthen the trunk, hip and shoulder muscles. Women in the intervention group received, in addition to the above, craniosacral manual releases to the pelvis. To see the program utilized, access the full article here.
Outcome measures included frequency of sick leave, morning and evening pain on visual analog scale, the Oswestry Disability Index scale, Disability Rating Index, European Quality of Life measure, intensity of discomfort of PGP, and blinded examiner assessment of recovery. The authors conclude the following: "Between-group differences for morning pain, symptom-free women and function in the last treatment week were in favor of the intervention group…treatment effects were small and clinically questionable…"
While craniosacral therapy is not strongly suggested based on the outcomes of this study, the authors acknowledge that craniosacral therapy is demonstrated in this and in previous research to have pain-relieving effects and a potential to halt deterioration of function. This type of clinical research model may prove to be very helpful in development of additional studies that assess the effects of specific interventions.
In my clinical and teaching experiences, and in the experiences of my colleagues, many therapists have questions about how to treat pregnant and postpartum conditions. It is common to encounter fears about working with patients who are pregnant due to the importance of avoiding potentially harmful examination and intervention techniques. We have also found that many therapists who are interested in women's health seek more information about orthopedic skills and practical clinical considerations. For these reasons, the Peripartum course series was developed over the past couple of years. Many of you may have taken the "Highlights of Pregnancy and Postpartum" taught by Institute founder Holly Herman, and will enjoy expanding your knowledge with the added days of coursework that includes both lecture and lab activities. The Institute offers a course based on pregnancy, one on postpartum, and a course on special topics during the peripartum period. The next opportunity to take the Pregnancy course is in January in Oklahoma City- there are still a few openings for this site.Join us to discuss issues such as pelvic girdle pain, what the evidence tells us, and what we can do for our patients.
References
Albert, H. B., Godskesen, M., Korsholm, L., & Westergaard, J. G. (2006). Risk factors in developing pregnancy-related pelvic girdle pain. [Article]. Acta Obstetricia et Gynecologica Scandinavica, 85(5), 539-544. doi: 10.1080/00016340600578415
Elden, H., Hagberg, H., Fagevik Olsén, M., Ladfors, L., & Ostgaard, H. (2008). Regression of pelvic girdle pain after delivery: follow?up of a randomised single blind controlled trial with different treatment modalities. Acta Obstetricia et Gynecologica Scandinavica, 87(2), 201-208
Elden, H., Östgaard, H. C., Glantz, A., Marciniak, P., Linnér, A. C., & Olsén, M. F. (2013). Effects of craniosacral therapy as adjunct to standard treatment for pelvic girdle pain in pregnant women: a multicenter, single blind, randomized controlled trial. Acta Obstetricia et Gynecologica Scandinavica.
Gutke, A., Lundberg, M., Östgaard, H. C., & Öberg, B. (2011). Impact of postpartum lumbopelvic pain on disability, pain intensity, health-related quality of life, activity level, kinesiophobia, and depressive symptoms. European Spine Journal, 20(3), 440-448
Gutke, A., Östgaard, H. C., & Öberg, B. (2006). Pelvic girdle pain and lumbar pain in pregnancy: a cohort study of the consequences in terms of health and functioning. Spine, 31(5), E149-E155.
Ostgaard, H. C., Anderson, G. B. J., & Karlson, K. (1991). Prevalence of back pain in pregnancy: A review (Vol. 16, pp. 95-101)
Mens, J., & Pool-Goudzwaard, A. (2012). Severity of signs and symptoms in lumbopelvic pain during pregnancy. Manual Therapy
Vleeming, A., Albert, H. B., Östgaard, H. C., Sturesson, B., & Stuge, B. (2008). European guidelines for the diagnosis and treatment of pelvic girdle pain. European Spine Journal, 17(6), 794-819
Can patients successfully perform a pelvic muscle contraction following verbal instruction? This question was asked by Bump and colleagues in the often-cited research article published in 1991. Urethral pressure profiles were assessed in forty-seven women at rest and during a pelvic muscle contraction following brief, standardized verbal instruction. In the article, the authors found that nearly half of the women performed with "an ideal effort" leading to urethral closure without a Valsalva effort. 25% of the women, unfortunately, demonstrated an effort at muscular contraction that could promote incontinence. The authors' conclusion is that simple verbal or written instruction is not the best approach for a patient engaging in a pelvic floor muscle training program.
The limitations of the above study (small number of subjects, arbitrary definition of "effective Kegel," and inability to predict patient outcomes based on urethral profile) are made very clear throughout the article, yet how do we see this apply to our patient population? How often do we complete a perineal observation during an examination and identify that the patient is not generating any perineal movement, demonstrating a bearing down maneuver rather than a shortening, protective contraction, or creating such force through the abdomen that even a well-contracted pelvic floor would struggle against the strain from above? The value of the Bump study reminds us that not all patients respond positively to verbal or written instruction only.
What about men? A recent study aimed to assess the ability of 52 healthy men (mean age of 22.6 years with a standard deviation of 4.42 years) to complete a pelvic muscle contraction in standing or crook lying following brief, standardized instruction. Real-time transabdominal ultrasound was used to measure bladder base elevation. 6 participants were unable to contract the pelvic floor muscles in either position, 17 were unable to contract the muscles in crook lying, and 14 could not contract the muscles in standing. While many of the men we instruct in pelvic muscle rehabilitation strategies are significantly older than the men in this study, the major point matches that of the Bump article: it is not safe to assume that a patient (even a young, healthy patient) can contract the pelvic floor muscles following verbal instruction. The authors suggest that transabdominal ultrasound may be a useful clinical tool for measuring bladder base elevation and therefore pelvic muscle activity.
To be fair, more people in general need to be educated about the pelvic floor muscles;we can likely agree that the lack of awareness and discussion about the roles the PFM play in daily life leads to persisting dysfunction. There are people within the population who can activate the pelvic muscles appropriately with verbal instruction, and for this portion of the population, verbal or written instruction may be better than no instruction. Group education in community or institutional settings may benefit patients who are unwilling, unable or uninterested in acquiring a referral to a pelvic rehab provider. But for the group of patients who is either not contracting the muscles or bearing down rather than lifting, the consequences of doing pelvic muscle strengthening incorrectly may be significant. Do we need to change how we are instructing the patient verbally? Should we offer assessment of pelvic muscle contraction ability in varied positions? Must we include other functional applications of the coordinating muscles such as the respiratory diaphragm? At this time, there is not one answer. If we can ask the questions, read the research, and participate in our own way to the research, or at a minimum, apply these questions to clinical care, we may find the best answer for each individual patient.
By accepting you will be accessing a service provided by a third-party external to https://hermanwallace.com/





































