The diagnosis of chronic constipation may seem like a simple concept; however, bowel patients can be a challenging group within our pelvic health population. The interesting part about treating these patients is that constipation can result in a variety of complaints. Diaz et al confirmed this in their 2023 research. Their article shared that “Constipation encompasses several subtypes, each with its unique characteristics and underlying factors.”(1) Common complaints can include frequency, size, length, and consistency which can become overwhelming for the practitioner to decide which clinical complaints seem the most important to focus on.
Knowing how to effectively treat these patients and ask the right questions is valuable in the scheme of pelvic floor rehab, secondary to overlapping symptoms and etiology of chronic constipation. Consideration needs to be taken into account for any outside factors that can also contribute to patient complaints. For example, taking different prescription medications, supplements, and eating different foods can all influence the patient's stool frequency and formation (2). Realizing where this issue stems from is the deep-dive question to get a handle on their complaints.
Bowel frequency can be one of the biggest clinical challenges for clinicians to educate patients to master – consistency is key! Understanding what their normal frequency should be, or what it should be now, is part of the clinical judgment skill when setting goals. If your patient is only getting a natural bowel movement urge every 10 days, their goal of daily BMs, at first, should be emotionally readjusted so that they don’t feel like they have failed their rehabilitation goals.
Learning colon physiology helps to understand normal vs abnormal motility and can be helpful in treating your patient’s constipation. In my course, Bowel Pathology and Physiology we discuss the physiological reflex that controls the lower motility of the GI tract following a meal (3). When patients present with chronic constipation, they may be experiencing a profound loss of the gastrocolic reflex. The course is filled with clinical pearls and research tidbits that help to improve or slow down colonic motility. Join me in the next course offering on September 14-15, 2024 to learn more.
Resources:
- Diaz S, Bittar K, Hashmi MF, et al. [Updated 2023 Nov 12]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan. Available from: https://www.ncbi.nlm.nih.gov/books/NBK513291/
- Araújo MM, Botelho PB. Probiotics, prebiotics, and synbiotics in chronic constipation: Outstanding aspects to be considered for the current evidence. Front Nutr. 2022 Dec 8;9:935830. doi: 10.3389/fnut.2022.935830. PMID: 36570175; PMCID: PMC9773270.
- Mawer S, Alhawaj AF. Physiology, Defecation. 2023 Nov 13. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan–. PMID: 30969554.
AUTHOR BIO
Lila Abbate, PT, DPT, MS, OCS, WCS, PRPC
 Lila Abbate is the Director/Owner of New Dimensions Physical Therapy. She graduated from Touro College in Dix Hills, NY with a Bachelor of Science (BS) in Health Sciences and a Master of Arts (MA) in Physical Therapy in 1997. She completed her Advanced Masters in Manual Orthopedic Physical Therapy (MS) at Touro College, Bayshore, NY in 2003 and continued to pursue her Doctor of Physical Therapy (DPT) at Touro in 2005. Dr. Abbate is a Board-Certified Specialist by the American Physical Therapy Association in Orthopedics (OCS) 2004 and Women’s Health (WCS) 2011. She obtained the Certified Pelvic Rehabilitation Practitioner (PRPC) from the Herman & Wallace Institute in 2014. She is a Diane Lee/LJ Lee, Integrated Systems Model (ISM) graduate and completed the New York series in 2012.
Lila Abbate is the Director/Owner of New Dimensions Physical Therapy. She graduated from Touro College in Dix Hills, NY with a Bachelor of Science (BS) in Health Sciences and a Master of Arts (MA) in Physical Therapy in 1997. She completed her Advanced Masters in Manual Orthopedic Physical Therapy (MS) at Touro College, Bayshore, NY in 2003 and continued to pursue her Doctor of Physical Therapy (DPT) at Touro in 2005. Dr. Abbate is a Board-Certified Specialist by the American Physical Therapy Association in Orthopedics (OCS) 2004 and Women’s Health (WCS) 2011. She obtained the Certified Pelvic Rehabilitation Practitioner (PRPC) from the Herman & Wallace Institute in 2014. She is a Diane Lee/LJ Lee, Integrated Systems Model (ISM) graduate and completed the New York series in 2012.
Dr. Abbate has been an educator for most of her physical therapy career. She has experience as a full-time faculty at Touro College, Manhattan Campus from 2002 to 2006 teaching the biomechanical approach to orthopedic dysfunction and therapeutic exercise as well as massage/soft tissue work that highlighted trigger point work, scar management, and myofascial release. She is currently on faculty as a Lecturer at Columbia University teaching the private practice section Business & Management course (since 2016) along with the Pelvic Health elective (since 2012). She teaches nationally and internationally with the Herman & Wallace Pelvic Rehabilitation Institute teaching advanced courses of her own intellectual property: Orthopedic Assessment for the Pelvic Health Therapist, Bowel Pathology Function, Dysfunction and the Pelvic Floor, Coccydynia & Painful Sitting: Orthopedic Implications. She was a co-writer for the Pudendal Neuralgia course and teaches the Pelvic Function Series, and Pregnancy/Postpartum Series. She has written two book chapters in 2016: Pelvic Pain Management by Valvoska and Healing in Urology: Clinical Guidebook to Herbal and Alternative Therapies by Chughtai.
Lila is a member of the American Physical Therapy Association, the National Vulvodynia Association, the American Urogynecology Association, the International Pelvic Pain Society, and is also a Senior Physical Therapy consultant for SI Bone, a sacroiliac joint instrumentation company.

Congratulations on completing Pelvic Function Level 1 (PF1) and entering the world of pelvic rehabilitation. Are you ready for your next course but not quite sure which one to take? Well, you’re not alone. Everyone’s pelvic health educational journey is different based on their interests and patient demographics and there are a lot of course options available.
I’m going to zero in on the intermediate-level courses in the Pelvic Function Series for you as HW does recommend that practitioners take at least one or two of these. If you’ve looked at the course page you’ve noticed that there are three courses with a Level 2 designation – as well as a lab course. What does this mean? These courses are designed to be a progression of knowledge and skills learned in the foundational course Pelvic Function Level 1.
Here are the intermediate courses:
- Pelvic Function Level 2A (PF2A) - Colorectal Pelvic Health, Pudendal Neuralgia, and Coccyx Pain
- Labs provide an introduction to internal anorectal examination for all genders.
- Pelvic Function Level 2B (PF2B) Urogynecologic Examination and Treatment Interventions
- Labs provide external abdominal and pelvic and internal vaginal approaches.
- Pelvic Function Level 2C (PF2C) Men’s Pelvic Health and Rehabilitation
- Labs provide external abdominal, gluteal, perineal, and internal anorectal approaches.
- Modalities and Pelvic Function (PFMOD) The Pelvic Health Toolkit
- Labs provide supervised instruction to practice modalities.
Ready for a more in-depth look at the courses? Here is a more detailed breakdown:
Pelvic Function Level 2A (PF2A) Colorectal Pelvic Health, Pudendal Neuralgia, and Coccyx Pain
This course is intended for the pelvic health clinician who treats patients with common functional gastrointestinal (GI) dysfunctions and is interested in learning internal anorectal examination and the use of balloon re-training.
In this course, you will learn about common functional gastrointestinal (GI) dysfunctions including irritable bowel syndrome, fecal incontinence, and constipation. Course topics provide an introduction to nutrition for bowel health, colorectal conditions, and oncology. Participants will be educated on how diagnoses such as hemorrhoids, fistulas, fissures, and anorectal pain including pudendal neuralgia and coccygodynia may be improved with pelvic rehabilitation.
Practical, trauma-aware, hands-on labs provide supervised instruction of pelvic function evaluation with external observation, palpation, and internal anorectal examination of pelvic skeletal and soft tissues. These labs include an external perineal and internal anorectal approach as well as education in the use of balloon re-training.
Pelvic Function Level 2B (PF2B) Urogynecologic Examination and Treatment Interventions
This course is intended for the pelvic health clinician who treats patients with conditions including urinary incontinence, chronic pelvic pain (CPP), and pelvic organ prolapse.
In this course, you will learn, with increased specificity, evaluation for urogynecologic conditions as well as an overview of medical management, and multi-disciplinary pelvic healthcare. Course topics provide a more in-depth understanding of urinary incontinence, chronic pelvic pain (CPP), and pelvic organ prolapse. Participants will be educated on how diagnoses such as interstitial cystitis/painful bladder syndrome (IC/PBS), urinary tract infections, vaginismus, vulvar pain, dyspareunia, polycystic ovarian syndrome (PCOS), and endometriosis may be improved with pelvic rehabilitation.
Practical, trauma-aware, hands-on labs provide supervised instruction of pelvic structures in relationship to the vaginal canal and surrounding structures such as the lumbopelvic nerves, the uterus, urethra, bladder, and rectum. Interventions instructed will include patient management of trunk and pelvic pressure, relaxation training, breathing, and manual therapies for a variety of pelvic dysfunctions. These labs include an external abdominal and pelvic and internal vaginal approach.
Pelvic Function Level 2C (PF2C) Men’s Pelvic Health and Rehabilitation
This course is intended for pelvic health clinicians who are interested in treating male pelvic health conditions.
In this course, you will learn critical detailed information about men’s pelvic health conditions including post-prostatectomy urinary incontinence, erectile dysfunction, and chronic pelvic pain (CPP). Participants will be educated on how diagnoses such as hard/flaccid, urgency/frequency, scrotal, testicular, and penile pain may be improved with pelvic rehabilitation.
Practical, trauma-aware, hands-on labs provide supervised instruction of pelvic health evaluation with external observation, palpation, and internal anorectal examination of pelvic structures and soft tissues. These labs include an external abdominal, gluteal, perineal, and internal anorectal approach.
Modalities and Pelvic Function (PFMOD) The Pelvic Health Toolkit
This course is for the pelvic health clinician who has the opportunity to use modalities as an adjunct to their patient's care and goes beyond the "Big 3" (E-Stim, Biofeedback, and Ultrasound).
In this course, you will learn about and practice a variety of modalities. Modalities in PFMOD include biofeedback, cold laser/light therapy, electrotherapy, real-time ultrasound imaging, belts, braces, supports, lubricants, myofascial tools/techniques, and “special topics” that can be used to assist in relaxation, bowel and bladder health, and sexual function. Specialized knowledge from experts in different subjects will be shared throughout the course.
Certain modalities that are impractical to practice live will be shared and demonstrated via video. These Interventions include shockwave, rehabilitative ultrasound imaging, dry needling, and light therapy.
Practical, trauma-aware, hands-on labs provide supervised instruction to practice utilizing biofeedback and other modalities to allow kinesthetic learning before prescribing and recommending them to patients.
Previous course sponsors who have provided samples and products have included:
- Nix
- Flyte
- OhNut
- Replens
- RockTape
- Bellies Inc.
- Ice Soothers
- BabyBellyBand
- Intimate Rose
- The Pro Group
- Good Clean Love
- Cushion Your Assets
If you are interested in taking an intermediate-level Pelvic Function Course but still have questions, then please contact us.
Did you know that the Pelvic Rehabilitation Practitioner Certification (PRPC) is celebrating its 10th anniversary? That's right, the first PRPC examination was administered in 2014 and since then, over 700 practitioners from all over the world have earned their certification.
Are you ready to join the ranks of these proficient professionals? Becoming PRPC certified allows you to proudly display the designation "PRPC" after your name, establishing you as an expert in pelvic rehabilitation.
Not sure if you qualify to sit for the PRPC examination? Don't worry, here are some frequently asked questions that may help clarify your eligibility.
What is the PRPC?
The certification available through the Institute is called the Pelvic Rehabilitation Practitioner Certification (PRPC). Earning the PRPC Certification is a professional achievement that demonstrates your dedication and expertise in the field. Through a specialized exam, you'll validate your knowledge and join an exclusive community of respected practitioners.
The PRPC was the first-ever certification exam for therapists seeking distinction for treating pelvic dysfunction in all genders throughout the life cycle.
Who can sit for the exam? Do I have to be a physical therapist?
While a license to practice skills in pelvic rehabilitation is required for the PRPC exam, you don't have to be a physical therapist to apply. In fact, HW welcomes a diverse group of professionals including Physical Therapists (PTs), Physical Therapist Assistants (PTAs), Physicians (MDs), Registered Nurses (RNs), Occupational Therapists (OTs), Occupational Therapist Assistants (OTAs), Doctors of Osteopathic Medicine (DOs), Doctors of Chiropractic Medicine (DCs), Advanced Registered Nurse Practitioners (ARNPs), Nurse Midwives (CNMs), Doctors of Naturopathic Medicine (NDs), and Physician Assistants (PA-Cs) with an active state-board license.
Do I have to take certain Herman & Wallace courses?
There are no course prerequisites for taking the PRPC exam. A valid certification exam tests demonstrable knowledge and skills, which can be gained from a combination of coursework, clinical experience, professional mentorship, etc.
Therapists considering applying should have a comprehensive skill set, which is often gained through several beginner, intermediate, and advanced courses in pelvic function and dysfunction. These can include the Pelvic Function Series, from Level 1 to Capstone, as well as specialized courses for bowel, bladder, sexual, and pelvic pain dysfunctions, depending on your interests and patient demographics.
Pricing for PRPC is discounted for those who have completed at least one course through Herman & Wallace.
How much pelvic rehabilitation experience do I need?
To be eligible to sit for the exam, all applicants must have completed a minimum of 2000 hours of direct pelvic patient care within the past 8 years, with at least 500 of those hours completed in the last 2 years. It's important to note that these patient care hours must come from a licensed clinician and cannot include any hours spent before becoming licensed.
A general guideline for what qualifies as direct pelvic patient care is any time spent directly impacting the care of a specific patient. These activities include (but are not limited to) examination, evaluation, diagnoses, treatment plans, and intervention for conditions related in whole or in part, to the health and function of pelvic structures and the pelvic floor. This includes seeing patients for pelvic pain, pelvic girdle dysfunction, and conditions of bowel, bladder, and sexual dysfunction and includes the care for pediatric, adolescent, adult, and aged patients of any gender.
Where can I find more information?
All the details of the PRPC can be found on our website through the Certification Tab. You can find sample questions, pricing information, and even some study resources!
Are you ready to take your clinical practice to the next level?
Don’t miss this opportunity to become PRPC Certified! Remember - this is the only certification that encompasses pelvic rehabilitation for ALL people across the lifespan. The next testing administration is November 1-15, 2024. The registration cut-off date is October 1st, and the sooner you get your application approved, the faster you can be connected to like-minded practitioners who want to study with you for the exam!
While the exam itself may not be "fun" (let's be honest), the studying process is where you truly elevate your expertise. Immerse yourself in a wealth of knowledge, expand your skills, and refine your techniques - all while preparing for the exam. Good luck on your journey to becoming a certified expert in pelvic rehabilitation!
A testimonial from Erika Darbro, PT, DPT, PRPC
"As a perpetual learner, I recognize the importance of staying up to date with the latest advancements in the field. Each year, I actively participate in numerous continuing education courses, a practice that reflects my dedication to providing the highest quality of care. It was a natural next step to take my commitment a step further by pursuing the Pelvic Rehabilitation Practitioner Certification (PRPC) in 2020.
"Choosing to become certified was not a decision made lightly. The PRPC certification stood out as the perfect fit for my clinical ethos – to treat all genders. Unlike some certifications that focus solely on women's health, the PRPC encompasses pelvic health topics for all populations. This alignment with my values was a driving force behind my choice, emphasizing my dedication to being an inclusive pelvic health practitioner.
"Obtaining the PRPC certification was not just about acquiring a credential; it was a statement of my commitment to being an expert in the pelvic health field. It serves as a recognition of my passion for treating the pelvic health population and reinforces the idea that I don't merely dabble in pelvic health.
"The pursuit of certification was also a personal challenge. It pushed me to elevate my skills, deepen my knowledge, and continually evolve as a practitioner. By challenging myself, I hope to inspire other healthcare professionals to embrace continuous learning and strive for excellence in their field."
II. Labor and Delivery
The Baby Always Has a Different Plan
Towards the end of my pregnancy, my doctor ordered an ultrasound to make sure the baby was growing appropriately. This was precautionary as the baby had measured small the last couple appointments. The ultrasound gave us some important information. Baby K was growing appropriately, however, she was breech. At this point, she should have already flipped into the cephalic (head down) position, and it was unlikely that she would turn further along in my pregnancy. I knew what this meant… “C-section” (cesarean). Like so many women before me, this was not what I wanted for my birth plan. Having a planned cesarean had not really crossed my mind. I figured it would only be some kind of emergency that would result in this outcome. Instantly I thought of all the patients I have treated over the years who had cesarean delivery. I thought of abdominal adhesions and scar tissue mobility work that would need to be done postpartum. Naturally, as a physical therapist, I also thought of all the mobility challenges this would bring after baby. Having a cesarean would change my post-partum recovery; I would need more help with lifting, carrying, and we have so many stairs in our house! I know this may sound crazy… but what saddened me the most about cesarean delivery was that I was not going to experience what labor felt like. I felt cheated, in a weird way, I was looking forward to it, almost like a rite of passage. I wanted to analyze labor and delivery from a patient’s standpoint, not just as a therapist. I thought it would help me relate to patients and friends who have experienced labor. All that being said, a scheduled C-section was happening unless that baby miraculously flipped.
 My doctor suggested a version, which is a procedure where your doctor tries to manually turn your baby using an external technique. I had heard it is painful, but I pride myself on being a pretty tough woman who has dealt with some pain, I can do this! Needless to say, the version was painful… Very painful! As a matter of fact, the most painful procedure I have ever encountered. After trying about four times to turn the baby, my doctor asked me if we should try one more time. Although I was miserable, I asked if they thought the baby was close to being in the right position. The looks on my husband’s and doctor’s faces told me that she hadn’t moved at all. We gave it one more try, but that stubborn baby really liked the spot she was in. The plan was to proceed with the scheduled C-section at 39 weeks, unless I went into labor first, then it would be an emergency cesarean delivery.
My doctor suggested a version, which is a procedure where your doctor tries to manually turn your baby using an external technique. I had heard it is painful, but I pride myself on being a pretty tough woman who has dealt with some pain, I can do this! Needless to say, the version was painful… Very painful! As a matter of fact, the most painful procedure I have ever encountered. After trying about four times to turn the baby, my doctor asked me if we should try one more time. Although I was miserable, I asked if they thought the baby was close to being in the right position. The looks on my husband’s and doctor’s faces told me that she hadn’t moved at all. We gave it one more try, but that stubborn baby really liked the spot she was in. The plan was to proceed with the scheduled C-section at 39 weeks, unless I went into labor first, then it would be an emergency cesarean delivery.
At 39 weeks, I woke up the morning of the planned cesarean and thought, “it’s a good day to have a baby”. I was excited to finally meet this little princess, but a little nervous about the cesarean delivery. I was trying not to think about what was going to happen to my abdomen and uterus. I was hoping Baby K would handle all of this safely, and she would be well. My plan for the procedure was distraction, not to think about what was happening, as I knew too much. Sometimes ignorance is bliss. I did not want to think of every unfortunate story I had heard about “spinals”, and “cesareans gone wrong”, so I kept telling myself to trust my doctors and relax. After all, this is what they do every day, and they are good at it. I wasn’t the biggest fan of the numbness and tingling I felt in my legs, as well as the lack of motor control in the lower half of my body once they administered the spinal, but it did the trick.
All I felt during the caesarean was just some tugging on my abdomen as the doctor worked to get baby out and complete the procedure. Luckily, it was all happening behind a partition while my husband held my hand and we told jokes to relieve our nerves. All of a sudden, there was a loud cry, and I felt instant relief. It was my baby, and she had healthy lungs! My doctor popped around the screen and showed me my beautiful brown-haired baby. Next, my husband and the nurses cut the cord and took care of baby. Once she was cleared and safe, they plopped her on my chest. Like a moth to a flame, that baby wriggled herself right onto my breast. It was the purest form of instinct I have ever witnessed. How did that little baby that just entered this world have the innate knowledge to nourish, and the strength to find her food source. It was amazing! Overall, no matter how much you research and plan for labor and delivery, it likely won’t turn out how you plan it. The positive is that our bodies have been delivering babies forever, so trust in your body, and trust in those around you helping with the delivery. The labor and delivery experience is innate.
In case you’ve been under a rock (or maybe studying for the Pelvic Rehabilitation Provider Certification (PRPC) exam, the latest Netflix series starring Maria Bamford is out, and it is, as the kids say, amazeballs. We have Maria Bamford and team, and Lady Dynamite, to thank for getting the term vaginismus out in the public as the title of Season 1, Episode 8. The episode is named “A Vaginismus Miracle.” In this episode Maria is answering the question of when she last had sex. She answers that is was a year ago, which reminds her that the annual date of "Vaginismus" must be coming up. Maria further explains that she must have sex once per year because then everything is good "under the hood", and if she doesn't have sex once a year, her "vagina could close up." It's a nail biter of an episode as Maria's assistant has messed up the schedule, and Maria finds out that "Vaginismus" is that very night, and she must find a partner before midnight.
As a pelvic health provider, I knew that neither myself nor my colleagues would be able to sit back and worry about Maria suffering through another year with “Vaginismus” on her calendar, a looming deadline when we all know that with a little bit of rehabilitation, the issue could be much, much better, or maybe resolved altogether. The episode inspired me to write an open letter to Maria. Feel free to share and tag your friends who you think would love to watch a smart, funny show that puts real life issues including mental health in the spotlight.
![]()
Dear Lady Dynamite,
I recently saw your Netflix show and I have to say that it is brilliant. I love how you weave humor, the messiness of life, and important topics into an unpredictable series of events. You are clearly one smart cookie, but I’m not convinced that your new agent, Karen Grisham, is such a great influence on you (or anyone for that matter).
I wanted to reach out and let you know that, as a pelvic rehabilitation therapist and faculty member at the Herman & Wallace Pelvic Rehabilitation Institute, I really appreciate that you brought the term vaginismus into the big time. So many women suffer needlessly because there is so much that pelvic rehab can do for women like you! It does seem that you have figured out a system that works for you, but what if things hadn’t worked out with Scott that night? Hanging out in a bar hoping that you can find someone to hook up with is just so 80’s. Your condition of vaginismus, a tightening of the muscles around your Lady Dynamite parts, does often cause pain with sex, and that’s called dyspareunia. This is a condition that we pelvic rehab specialists treat every day with a heck of a lot of success. Your new boyfriend Scott (he is still your boyfriend after Thanksgiving and all, right?) could even help you overcome some tenderness and tightness by learning to help you release your vaginal muscle tension. Now if that doesn’t sound like great fodder for some stand-up I don’t know what does!
It’s hard to know sometimes why vaginismus starts, maybe it was the years of freezing temperatures in Duluth that led to your tight muscles, or sliding down Chester Bowl on the ice. Maybe it was spending too much time sitting in a wheelchair while medicated, or caused by medication itself (that happens too- even birth control pills can cause pelvic pain!) My point is, there’s no need to put so much pressure on yourself and have this horrible deadline of “vaginismus” hanging over your head when you can see a kind, smart health care provider about the issue. If you, dear Lady Dynamite, need a referral for a great pelvic rehab therapist in your neighborhood, let us know! We train hundreds of therapists every year, and can help you find the perfect fit (pun intended!) Ha! (We know you can handle a little “adult humor.”) Wishing you all the best, and thanks again for talking about your vagina!
Yours in Pelvic Health,
Holly Tanner
P.S. Good luck with the Pussy Noodles representation!
P.P.S Go ‘Toppers!
P.P.P.S Can’t wait for Season 2!
P.P.P.P.S And if you see Mark McGrath around, say “hi” for me!
![]()
So, dear readers, if you would like to enjoy a smart and really funny show, check out Lady Dynamite. And if you want to learn more about vaginismus, Herman & Wallace offers several courses which would be up your alley. Consider joining faculty member Dee Hartmann, PT, DPT at Vulvodynia: Assessment and Treatment - Denver, CO this October 15-16.
Brady, P. & Hurwitz, M. (Creators). (2016). Lady Dynamite: Season 1, Episode 8. Retrieved from http://netflix.com
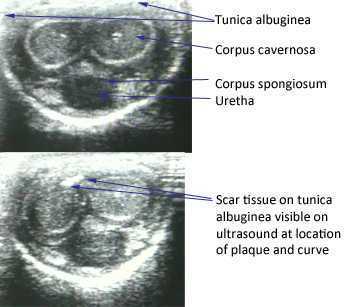
The American Urological Association issued new guidelines in May of this year for the diagnosis and treatment of Peyronie's. The disorder, which you can read more about at this link, often leads to a curvature in the penis that can be painful, or that can lead to impaired sexual or urinary function. While the exact mechanism leading to Peyronie's is still being researched, what is known is that plaques (sometimes calcified) may form in a deep layer of thick connective tissue called the tunica albuginea that surrounds the penis.
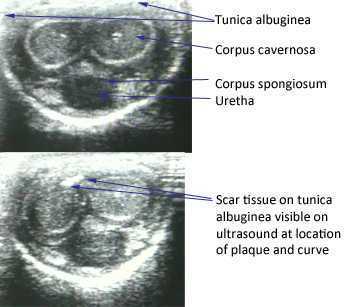
In the clinical guidelines, the authors state that a diagnostic process should include documentation of the signs and symptoms of Peyronie's disease. This can include a careful history (assessing any penile deformity, limitations in sexual function, penile pain, and level of distress). In the medical office, an intracavernosal injection (check here for a Medscape article describing an algorithm) can be completed. The authors also state, in line with expert opinion, that a provider should only evaluate a patient's Peyronie's disease when possessing "…the experience and diagnostic tools to appropriately evaluate, counsel, and treat the condition." In regards to pelvic rehabilitation, understanding the condition and encouraging the patient to visit a medical provider who is appropriately trained to manage Peyronie's is valuable. Establishing a baseline for the amount of dysfunction and curvature aids the patient and physician in determining current and future care planning.
Available treatments include education about possible treatments as well as adverse reactions to medical treatment. Interventions might include oral NSAIDs, intralesional injections (to reduce the amount of scar/thickened tissue or pain), and surgeries. Surgical options include procedures to remove the plaque or scar tissue, remodel the penile tissues after plaque removal, and for more severe cases, to implant a penile prosthesis. (Recommendations for treatments to avoid due to potential for harm or for lack of evidence are also listed in the article.)
The role of pelvic rehabilitation is emerging for men who present with genital pain, deformity, or pelvic dysfunction. There are certainly comorbid dysfunctions that we can address, such as pelvic muscle dysfunction, bowel and bladder issues if present, and we can provide a significant amount of education about pelvic health. Therapists are also teaching patients to perform connective tissue mobilization on the penile tissues, and some therapists are directing manual therapy, dry needling, and other modalities to the tissues. Rehabilitation lacks, at this time, compelling evidence to support direct treatment to the tissues, and hopefully that research will be seen in the near future. The authors of the new guidelines conclude that "…The most effective approach for a particular patient is best determined by the individual clinician and patient in the context of that patient’s history, values, and goals for treatment." This sounds to me like an effective approach for every patient who struggles with a condition that lacks a clear understanding of etiology and best treatments. These guidelines are a step forward in management of patients who deal with the frustrating condition, and the guidelines will be updated, according to the article, as the science advances.
If you would like to learn more about the rehabilitation implications of Peyronie's, and the potential and current roles of therapists in male pelvic health, you have two opportunities this year to attend the Male Pelvic Floor course , August in Denver, and November in Seattle. We expect the Seattle to course to sell out, and it's filling up fast, so check your calendar and come join us at the Male course.
A few weeks ago, a pelvic course participant shared some sensitive and intimate thoughts about being at a course and being "the biggest girl in class." This week, we will address specific strategies for communicating with your patients and for adapting your exam techniques when appropriate. The following quote is from an educational book for Nurse Practitioners, and echoes a very healthy and realistic sentiment about our role when working with patients in pelvic rehabilitation.
"If the exam is limited by obesity, the patient should be told in a clear, non-judgmental manner. Patients have a right and responsibility to understand the findings of the health care visit."

Unfortunately, according to the authors, women who are obese are less likely to receive routine gynecologic care due to bias and fear of judgement, or even practical issues like exam tables, gowns, and equipment not being adequate. Another issue is that of mobility: is the exam table too narrow for safety and comfortable positioning? In my own clinical practice, I have had patients ask me: "Is that massage table going to hold me?" In order to answer that question, you need to know what the safe weight limits are for your chairs, walkers, exam tables, and any other equipment your patients may use. You might imagine that if a patient is concerned about falling off of a table, completing an appropriate exam could be difficult due to muscle guarding. Other techniques recommended include the following:
- ask an assistant to gently hold back skin folds if vagina or vulva is obscured
- ask the patient to flex her hips upward if able
- ask patient to help hold back excess skin in lower abdomen if helpful
- ultrasound may be used rather than palpation as needed (this is in reference to a medical gynecologic exam, but how might rehab US contribute to our toolkit?)
- document any difficulty with the examination - placing a small towel or pillow under the patient's hips may also help in viewing the cervix
This "Bias Tool Kit" offers further suggestions to avoid causing harm when evaluating a woman who is obese:
- if you would like to weigh the patient, ask for consent first, using sensitive language, i.e. "would you like to be weighed today?" and maintain privacy
- in addition to considering equipment like tables, think about having a stepstool with a handle, properly sized blood pressure cuffs, sturdy, armless chairs, and a long exam speculum
- use words that patients find more acceptable, such as excess weight or BMI
Advice to the nurse practitioners include the following to counter the fact that obese women are often discriminated against:
"If the exam is limited by obesity, the patient should be told in a clear, non-judgmental manner. Patients have a right and responsibility to understand the findings of the health care visit." For example, for a medical exam: "Due to the shape and size of your body, I wasn't able to feel your uterus and ovaries." Any similarly needed communications can be shared in a professional and warm tone.
While sensitive topics can require patience, practice, and an abundance of professionalism, everyone wins when difficult subjects are approached with honesty. Thanks again to Erin B. for shining her light on this sensitive and valuable topic.
Pain associated with menstruation is known as dysmenorrhea, and more than half of women have pain related to their period for 1-2 days per month, according to The American College of Obstetricians and Gynecologists. Primary dysmenorrhea is related to menstruation, and often begins within a short period of time once menses occurs, whereas secondary dysmenorrhea is often related to a condition within the reproductive tract such as endometriosis or fibroids. In the medical office, a medical history, a pelvic exam, and possibly an ultrasound or laparoscopy will be completed. Treatment may include medications such as NSAIDs which target the prostaglandins that often lead to symptoms of dysmenorrhea, birth control pills, or surgeries.

A recent literature review asked if physiotherapy can help with symptoms of primary dysmenorrhea. Of the articles reviewed, 186 were chosen, and included a range of articles from descriptive, experimental studies to prospective, randomized controlled studies. A variety of interventions and approaches were included in the review, such as TENS, abdominal massage, acupuncture, cryotherapy and thermotherapy, connective tissue, Pilates, and belly dance. All of the approaches demonstrated some therapeutic benefit, either in response to the immediate application of the intervention, or up to a few months after the intervention was applied or instructed.
This literature review echoes a prior systematic review that evaluated the effectiveness and safety of acupressure, acupuncture, aspirin, behavioral interventions, oral contraceptives, and other supplements, procedures, and complementary and alternative medical interventions. Click here to view the full-text article. In that particular review, the authors reported the following:
- high-frequency TENS reduces pain (but less so than ibuprofen)
- acupressure may be as effective as ibuprofen
- topical heat may be as effective as ibuprofen and more effective than paracetamol
The bottom line from this research should be that we as pelvic rehabilitation providers need to help patients address pain and symptoms from dysmenorrhea. Clearly, there are many pathways to achieve symptom reduction, and some, such as TENS or topical heat, are easily carried out on an independent basis. How are you reaching adolescent girls who may develop primary dysmenorrhea? In clinical practice, talking with their parents, or reaching out at the community level to schools, churches, camps, gyms, or coaches may provide an opportunity to provide education and help. If you would like to learn more about myofascial release techniques for the abdomen and pelvis, check out the Myofascial Release for Pelvic Dysfunction continuing education course taking place next month in Illinois!
This question is one that, a decade ago, may have made more sense to ask, as very few male therapists were engaged in the world of pelvic rehabilitation. Most pelvic rehabilitation practices still stem from programs developed in "Women's Health" so it's logical to see more female patients being treated, usually by female therapists. We are at an exciting time in the healing professions, and particularly in pelvic rehabilitation, when choice of provider may come to be based more on experience, personality and qualifications of the treating therapist than on the provider's or patient's gender. At the Institute's most recent entry-level Pelvic Floor 1 (PF1) courses, 2 male therapists were in attendance at 2 different PF1 courses on opposite sides of the nation. This shift (we tend to have an occasional male therapist within the pelvic floor series courses) has been noticed, and at the Institute, we have committed efforts at exploring if and how this shift affects our coursework. For example, are the instructors comfortable, are the female participants cool with it, and do the men feel welcomed? To find out a little more about the subject, I bring your attention to a few of the men who are currently representing the field of pelvic health.
Herman & Wallace Institute faculty member, Peter Philip, has treated both men and women in his practice for years. This treatment involves internal assessment and intervention when needed, and Peter approaches all of his patients with the same matter-of-fact, clearly defined consent. As a private practice owner, it makes sense that Peter is able to retain his patients regardless of the condition for which they are seeking care. Having to refer a patient to another therapist or clinic would negate the ability for a therapist to provide comprehensive care. On his website you will find a listing of women's health issues described next to sports, work, and other lifestyle injuries.
I posed the following question to Jake Bartholomy , physical therapist in Seattle, Washington: "Why is it so important for a male therapist to be involved in pelvic rehab, regardless if the goal is to focus on working with male or female or other gendered patients?" Jake's response reflects the value of offering choices to the patients he serves: "I believe it's important for people to have a choice in their therapist. Many people are shy and nervous to discuss their pelvic issues and if male or transgendered patients are more comfortable working with a male therapist, I'm proud to offer that service in the Seattle area."
I recall meeting Daniel Kirages, physical therapist and clinical instructor at the University of Southern California, at a male pelvic floor course years ago. When he introduced himself to the group, he joked that he was there as the token male "to break up the girl party." While this joke has stuck with me, it also drives home the point that it takes courage to show up at coursework which has previously been dominated by female therapists. Daniel has been involved in research, teaching in the classroom and online, and lecturing nationally about pelvic rehab.
In my experience as an instructor, the male therapists who attend pelvic rehab courses are exceptionally grounded, open-minded, and exude a quiet confidence that seems necessary for working with sensitive issues surrounding pelvic rehabilitation. Just for the record, we absolutely do believe that male therapists belong in pelvic rehabilitation coursework and practice, and we at the Institute are going to continue to explore how we can support all genders working in this much-needed, and good work. If you are interested in learning more about the course series or any specialty topics courses, check out our course listings here.

A recent study aimed to determine if an association is present between childhood functional constipation and parental child-rearing attitudes. Of the 133 studied children (ages 4-18), all were diagnosed with functional constipation and participated in a randomized, controlled trial evaluating the effectiveness of behavioral therapy compared with conventional treatment. Outcomes tools included the Amsterdam version of the Parental Attitude Research Assessment (A-PARI). The scale measures parental attitudes in the following domains: autocratic ("the child needs authority, strictness"), autonomy (encouraging independence), over-protection (prevent disappointments for the child), and self-pity (irritation with bringing up child.) (For more information about the methods, results, inclusion or exclusion criteria, you can download the linked article as full, free text.)
The study determined an association between defecation and fecal incontinence and parental child-rearing attitudes. For example, a highly overprotective or a high self-pity attitude both increased fecal incontinence, and that high autonomy and low autonomy attitudes were found to be detrimental to bowel health. The authors conclude that "…child-rearing attitudes are associated with functional constipation in children" and that parenting issues should be addressed when treating constipation in children. Specifically, if parenting issues are limiting the success of the pediatric patient or "when the parent-child relationship is at risk", referral to mental health services may be needed. The research study discusses concepts of education to "demystify" the dysfunction and positively affect parental attitudes.
We know that management of pediatric urinary dysfunction relies in large part on management of bowel dysfunction. In addition to needing to understand how we approach childhood constipation rehabilitation, we may be able to identify concerns in how a parent is dealing with a child's constipation. It is understandable that managing a child's bowel or bladder dysfunction can be frustrating for a patient, yet if the pelvic rehabilitation provider has concerns about a parent's participation in home program carryover, the parent may be appropriate for referral to a mental health provider, as this study suggests. If you would like to have more information about treating children with bowel and bladder dysfunction, you can sign up for Pediatric Incontinence and Pelvic Floor Dysfunction. You have two opportunities still this year to take this course that will prepare you for helping kids with pelvic dysfunction: Houston in July, and Boston in October