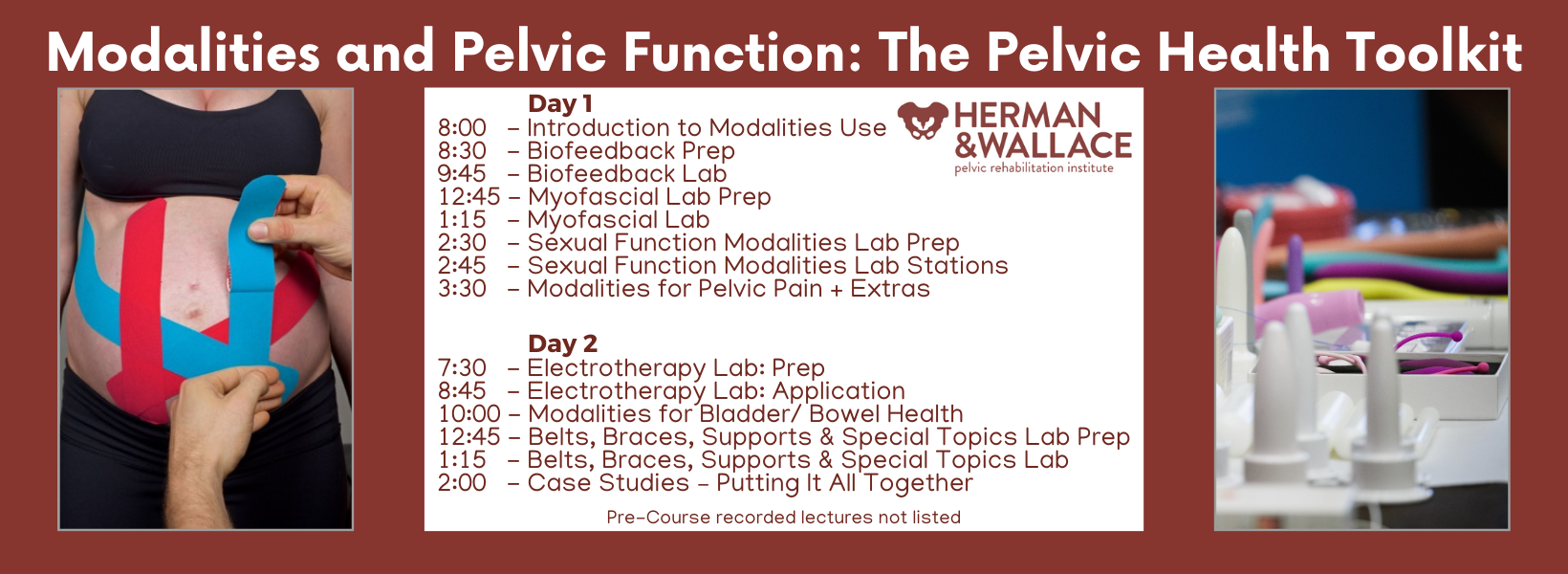
Since its launch in the beginning of 2024, Modalities for Pelvic Function has only continued to grow. The cool thing about this class is that although the curriculum content stays mostly the same, there are always amazing products for pelvic health being released and discovered by the curriculum team. Our next class offering is in July of 2025 and we’re adding at least 3 new products to the class. Enjoy our introduction to them in the order they will appear in our course work!
New to the Myofascial Techniques Lab - The BAligned Bowtie The BAlign® Bowtie by TheraTrain is a therapy tool designed by Dr. Jaime Loomis, a Doctor of Physical Therapy, to promote spinal alignment and alleviate musculoskeletal discomfort. The BAlign Bowtie is a compact, hard rubber device shaped like two connected ovals. Dr. Jamie gives tips on where to place it, usually the base of the spine or pelvis, and then the client lies on it for a few minutes to help realign the spine and relieve pain. This tool is particularly beneficial for individuals experiencing low back pain, hip tightness, or asymmetrical posture. It's also been reported to aid in conditions like scoliosis and improve mobility in activities such as golf and running.
The BAlign® Bowtie by TheraTrain is a therapy tool designed by Dr. Jaime Loomis, a Doctor of Physical Therapy, to promote spinal alignment and alleviate musculoskeletal discomfort. The BAlign Bowtie is a compact, hard rubber device shaped like two connected ovals. Dr. Jamie gives tips on where to place it, usually the base of the spine or pelvis, and then the client lies on it for a few minutes to help realign the spine and relieve pain. This tool is particularly beneficial for individuals experiencing low back pain, hip tightness, or asymmetrical posture. It's also been reported to aid in conditions like scoliosis and improve mobility in activities such as golf and running.
I had the privilege of meeting with Dr. Jamie to talk about her product, and she gave me the insider scoop on it. This product can be used for pelvic alignment, but can also be used higher up in the spine to help with asymmetry and pain. I personally love a multifaceted tool for investment and creative purposes! She created this tool to save time in therapy sessions. Dr. Jamie noticed that patients with pelvic and shoulder asymmetries would have improvement with their alignment and pain in therapy, but then be back to baseline by their next session. She’d have to spend time in their session repeating previous work to realign things again. She found that with this tool, her patients could have something actionable at home and their return sessions in alignment and were able to focus on other areas of therapy such as strength, function, and mobility.
If you want to check this product out before our next class offering Modalities for Pelvic Function , check out her website or snag it from Amazon! Dr. Jamie has some really helpful videos to train therapists and their patients. Think of this as another tool in a patient’s self-care toolbox for their home program!
To learn more: https://theratrain.org/balign
Modalities for Bladder/ Bowel Health - Alonea PelvicTool
 This product was introduced to me by a faculty member who tried it at the APTA Combined Sections Meeting and sent me an email immediately about how it NEEDED to be in the modalities course. In our Modalities for Bladder/Bowel Health, we have a 90-minute hands-on lecture about all the products we have collected that relate to pelvic floor therapy for bladder and bowel diagnoses. We review and trial a whole bunch of pelvic floor muscle trainers to help with coordination and relaxation, but the Alonea PelvicTool is a wonderful new addition.
This product was introduced to me by a faculty member who tried it at the APTA Combined Sections Meeting and sent me an email immediately about how it NEEDED to be in the modalities course. In our Modalities for Bladder/Bowel Health, we have a 90-minute hands-on lecture about all the products we have collected that relate to pelvic floor therapy for bladder and bowel diagnoses. We review and trial a whole bunch of pelvic floor muscle trainers to help with coordination and relaxation, but the Alonea PelvicTool is a wonderful new addition.
The Alonea PelvicTool is marketed as a non-invasive, app-supported pelvic floor training device designed for women, men, and children. It utilizes biofeedback technology to help users strengthen and improve control over their pelvic floor muscles. It features an ergonomic seat cushion with a soft pressure-sensitive sensor that connects via Bluetooth to the PelvicTool app, providing real-time biofeedback during muscle contractions. This visual guidance helps users correctly engage their pelvic floor muscles, making it ideal for home use, fitness centers, or therapy clinics. This device offers options for guided workouts, free training, and progress tracking. The device supports rehabilitation and prevention of issues like incontinence, back pain, pelvic instability, and erectile dysfunction without the need for internal devices or undressing.
Clinically, this device could be beneficial for anyone who does not want to have a pelvic floor muscle assessment for a variety of reasons, but feels comfortable sitting on the PelvicTool and monitoring their pelvic floor motion on an app. This device can provide reassurance to both the patient and clinician that IF pelvic floor muscle engagement or relaxation is indicated that it is happening correctly.
Alonea has kindly provided a 10% discount to Herman & Wallace course participants: h&walonea10%
To learn more: https://alonea.ch/en/pelvictool-alonea-pelvic-floor-trainer/
Belts, Braces, Supports & Special Topics - My Pelvic Bra
 Last but not least, this product was created by Jeanice Mitchell, PT, MPT, WCS, BCB- PMD, founder of myPFM. She describes imaging an external support after having her first baby but wanting something discreet that she could wear under her clothes. She had a hard time finding something that was supportive AND discreet at the same time. She was introduced to a friend of a friend who was a costume designer for Disney and myPelvicBra™ was born.
Last but not least, this product was created by Jeanice Mitchell, PT, MPT, WCS, BCB- PMD, founder of myPFM. She describes imaging an external support after having her first baby but wanting something discreet that she could wear under her clothes. She had a hard time finding something that was supportive AND discreet at the same time. She was introduced to a friend of a friend who was a costume designer for Disney and myPelvicBra™ was born.
The myPelvicBra™ is a discreet, wearable support garment designed by a pelvic floor physical therapist to provide gentle perineal compression and lift to the pelvic floor. It aims to alleviate symptoms associated with pelvic organ prolapse, urinary leaks, and pelvic pressure, especially during physical activities like walking, exercise, or prolonged standing. This product is constructed with a breathable, sweat-wicking liner and a reinforced hammock structure, it offers a second skin feel without visible panty lines. The adjustable waistband of the Classic allows users to customize the level of support needed throughout the day. Available in both Classic and Sports versions, the myPelvicBra™ caters to varying lifestyle needs, providing a non-invasive alternative to internal devices like pessaries. Its design focuses on comfort, discretion, and effectiveness, making it a valuable tool for individuals seeking external pelvic support.
I can tell you from personal experience, this product has been a life saver for my patients who need support for their symptoms. It's especially helpful as a quick intervention as patients are working on therapy goals of strength, coordination, and load transfer/pressure management. My patients who have significant prolapse with symptoms who are doing all of the therapy things and needing more support, but don’t want to go the route of pessary fitting or surgery also have really benefitted from this product.
To learn more: https://www.mypelvicbra.shop/
We’re excited to continue to add products to Modalities for Pelvic Function so that those taking the class can learn about, practice, and explore amazing products they may not have known existed to help support patients on their pelvic health journeys. Join an upcoming Modalities for Pelvic Function near you:
AUTHOR BIO
Mora Pluchino, PT, DPT, PRPC

Mora Pluchino, PT, DPT, PRPC (she/her) is a graduate of Stockton University with a BS in Biology (2007) and a Doctorate of Physical Therapy (2009). She has experience in a variety of areas and settings, working with children and adults, including orthopedics, bracing, neuromuscular issues, vestibular issues, and robotics training. She began treating Pelvic Health patients in 2016 and now has experience treating women, men, and children with a variety of Pelvic Health dysfunction. There is not much she has not treated since beginning this journey and she is always happy to further her education to better help her patients meet their goals.
She strives to help all of her patients return to a quality of life and activity that they are happy with for the best bladder, bowel, and sexual functioning they are capable of at the present time. In 2020, She opened her own practice called Practically Perfect Physical Therapy Consulting to help meet the needs of more clients. She has been a guest lecturer for Rutgers University Blackwood Campus and Stockton University for their Pediatric and Pelvic Floor modules since 2016. She has also been a TA with Herman & Wallace since 2020 and has over 150 hours of lab instruction experience. Mora has also authored and instructs several courses for the Institute.

As physical therapists who specialize in treating all genders and all conditions related to the niche practice of pelvic health, it has been a privilege for us to deliver whole-person care, emphasizing self-healing, nervous system regulation, and mind-body integration. We often see patients who are under high stress and anxiety, and even more so when they have no other options except surgical intervention.
 One such case was a 71-year-old patient who came in with a rectal prolapse. She had experienced a 10 cm rectal prolapse post-defecation, and it had taken prolonged bed rest for half a day for spontaneous reduction to occur. This happened after every bowel movement. She was told there were no other options except surgery. She was afraid to undergo rectal surgery and was willing to try anything to avoid it. Over the course of the first visit, I also learned that she had a family member who was very ill, and she rated her stress and anxiety levels beyond 10/10.
One such case was a 71-year-old patient who came in with a rectal prolapse. She had experienced a 10 cm rectal prolapse post-defecation, and it had taken prolonged bed rest for half a day for spontaneous reduction to occur. This happened after every bowel movement. She was told there were no other options except surgery. She was afraid to undergo rectal surgery and was willing to try anything to avoid it. Over the course of the first visit, I also learned that she had a family member who was very ill, and she rated her stress and anxiety levels beyond 10/10.
Rectal prolapse is full thickness protrusion of the rectum through the anal canal. It can occur in both sexes, but is 6 times more likely in women. Overall, about 13% of women will undergo surgery for some form of pelvic prolapse at some point in their lives. The incidence of pelvic prolapse also increases with age, peaking in those over 70 years1,2. Rectal prolapse can present in a variety of forms and is associated with a range of symptoms including pain, incomplete evacuation, mucous rectal discharge, and fecal incontinence or constipation2,3,4,5,6.
It is associated with lifestyle-limiting symptoms for the patient and frequently co-exists with other types of pelvic prolapse, making multidisciplinary management key, as it is primarily managed with surgical reconstruction2. Multiple surgical approaches exist within the two broad categories of perineal and abdominal. Perineal approaches are considered less physiologically taxing but are associated with higher recurrence rates. Anterior mesh rectopexy appears to balance the best functional outcomes with the lowest risk of recurrence2.
There is currently limited evidence to support non-surgical rehabilitation options for this condition. Complementary and Alternative Medicine (CAM) techniques, such as Acupressure, have shown promise in pelvic health, yet are largely underexplored in the context of rectal prolapse.
 Given this patient’s high anxiety and impaired bowel function that required prolonged bed rest post-defecation, I decided to use a novel multimodal rehabilitation approach. This approach integrated Acupressure, pelvic floor muscle training (PFMT), manual therapy, breathing and mindfulness techniques, and postural and functional retraining. The goal was to address her symptoms, improve activity tolerance and function, and improve her quality of life.
Given this patient’s high anxiety and impaired bowel function that required prolonged bed rest post-defecation, I decided to use a novel multimodal rehabilitation approach. This approach integrated Acupressure, pelvic floor muscle training (PFMT), manual therapy, breathing and mindfulness techniques, and postural and functional retraining. The goal was to address her symptoms, improve activity tolerance and function, and improve her quality of life.
Acupressure was introduced at the first visit. Over the course of 7 visits, this patient progressed through a gentle pelvic floor strengthening program and had a 90% improvement in her rectal prolapse symptoms. She was also trained to use pelvic floor Acupressure at the Governing Vessel 1 (GV 1) Acupoint to effectively and quickly reduce her rectal prolapse after every bowel movement.
 The patient was also taught an Acupressure nervous system self-regulation program that consisted of Acupressure points to help her improve mind-body awareness & connection to down-regulate her nervous system. Several Acupoints, such as Conception Vessel 17 (CV17), Governing Vessel 24.5 (Yintang point), Heart 7, and Pericardium 6, were used to help her manage and control her stress and anxiety. These points were reviewed and reinforced at each session. Her functional gains included restored ability to perform ADLs without post-bowel movement limitations. She also demonstrated improved pelvic floor muscle coordination, increased standing and walking tolerance, and was very pleased that she was able to avoid surgery. Her anxiety levels significantly improved with the daily self-regulation practice, and she felt she now had physical control over her symptoms.
The patient was also taught an Acupressure nervous system self-regulation program that consisted of Acupressure points to help her improve mind-body awareness & connection to down-regulate her nervous system. Several Acupoints, such as Conception Vessel 17 (CV17), Governing Vessel 24.5 (Yintang point), Heart 7, and Pericardium 6, were used to help her manage and control her stress and anxiety. These points were reviewed and reinforced at each session. Her functional gains included restored ability to perform ADLs without post-bowel movement limitations. She also demonstrated improved pelvic floor muscle coordination, increased standing and walking tolerance, and was very pleased that she was able to avoid surgery. Her anxiety levels significantly improved with the daily self-regulation practice, and she felt she now had physical control over her symptoms.
Acupressure is an evidence-based practice that is rooted in Acupuncture and Traditional Chinese Medicine. In Acupressure, we use gentle finger pressure instead of needles to stimulate specific points on the body known as Acupuncture points. These energy points are known to have high electrical conductivity at the surface of the skin and are embedded within the body’s vast fascial network. Because of this, they offer a unique gateway to access and influence the nervous system.
As a Holistic pelvic health practice, Acupressure can be used to:
- Reduce Pelvic Pain
Potent acupoints on the abdomen, pubic bone and sacrum can help to relax pelvic floor muscles, ease menstrual cramps and pelvic pain. The Bladder meridian points along the sacral spine (B27–B34) — are for back pain, pelvic tension, and reproductive organ support. - Enhance Blood Flow & Energy (Qi)
Certain acupoints stimulate blood and lymph circulation in the pelvic region, supporting physiological functioning of various sexual and reproductive organs. The Kidney 1 point, located on the sole of the foot — is for grounding, calming, and helps with anxiety and stress stored in the pelvic bowl. - Regulate Menstrual & Reproductive Health
Acupressure can help regulate cycles, reduce PMS symptoms, and support fertility by harmonizing hormonal pathways. The Spleen 6 – Sanyinjiao point, which is located on the inner leg, above the ankle — regulates menstrual cycles, supports fertility, and soothes menstrual cramps. - Promote Nervous System Regulation
Acupressure engages the parasympathetic nervous system and can help to calm the body, improve sleep, and promote relaxation. The pelvis is often a storehouse for unprocessed emotions, especially trauma. Acupressure combined with breathwork or somatic practices can help with these symptoms. - Support Bladder & Bowel Function
Pressing on meridian points associated with the bladder, kidneys, spleen, or large intestine can aid with incontinence, constipation, and other bowel & bladder symptoms. Acupressure can also help with symptoms of Rectal Prolapse as noted in this patient case.
This patient case explores a multimodal rehabilitation program integrating Acupressure with traditional pelvic floor therapy, which may serve as an effective non-surgical intervention for rectal prolapse. Improvements in symptom control, functional mobility, and self-management highlight the potential of Acupressure as a conservative approach for prolapse care.
I am so humbled to share that this patient’s Case study has been accepted at the International Urogynecological Association (IUGA) & European Urogynecological Association (EUGA) joint meeting that is being held in Barcelona, Spain in June this year. This is a great step forward to explore holistic options in pelvic health, and I am grateful to be part of this patient’s journey to wellness.
To learn more about Acupressure, please join the upcoming remote course Acupressure for Optimal Pelvic Health scheduled for June 7- 8th. The course will introduce participants to the basics of Traditional Chinese Medicine (TCM), Acupuncture & Acupressure. The course introduces the 12 major Meridians or energy channels, focusing on the Bladder, Kidney, Stomach, and Spleen meridians. The course is packed with key potent points that can help to self-regulate the nervous system and help with anxiety, insomnia, chronic pelvic pain, dysmenorrhea, infertility, constipation, urinary dysfunctions, digestive disturbances, cancer pain, and much more. The course also offers an introduction to Yin yoga and explores Yin poses within each meridian channel that can be integrated with Acupressure and mindfulness practices.
References
- Bordeianou L, Hicks CW, Kaiser AM, Alavi K, Sudan R, Wise PE. Rectal prolapse: an overview of clinical features, diagnosis, and patient-specific management strategies.J Gastrointest Surg. 2014;18(5):1059-1069. doi:10.1007/s11605-013-2427-7
- Romero-Morales C, Bravo-Aguilar M, Abuín-Porras V, et al. Current advances and novel research on minimal invasive techniques for musculoskeletal disorders. Dis Mon. 2021;67(10):101210. doi:10.1016/j.disamonth.2021.101210
- Yang J, Do A, Mallory MJ, Wahner-Roedler DL, Chon TY, Bauer BA. Acupressure: An Effective and Feasible Alternative Treatment for Anxiety During the COVID-19 Pandemic.& Glob Adv Health Med. 2021;10:21649561211058076. Published 2021 Dec 12. doi:10.1177/21649561211058076
- Wen J, Chen X, Yang Y, et al. Acupuncture Medical Therapy and Its Underlying Mechanisms: A Systematic Review. Am J Chin Med. 2021;49(1):1-23. doi:10.1142/S0192415X21500014
- Zhou YF, Zhang GL, Sun N, et al. Acupuncture for emotional disorders in patients with inflammatory bowel disease: a systematic review protocol. BMJ Open. 2022;12(9):e058568. Published 2022 Sep 27. doi:10.1136/bmjopen-2021-058568
- Gallo G, Martellucci J, Pellino G, et al. Consensus Statement of the Italian Society of Colorectal Surgery (SICCR): management and treatment of complete rectal prolapse. Tech Coloproctol. 2018;22(12):919-931. doi:10.1007/s10151-018-1908-9
AUTHOR BIO
Rachna Mehta PT, DPT, CIMT, OCS, PRPC, RYT 200
 Rachna Mehta PT, DPT, CIMT, OCS, PRPC, RYT 200 (she/her) graduated from Columbia University, New York with a Doctor of Physical Therapy degree. Rachna has since been working in outpatient hospital and private practice settings with a dual focus on Orthopedics and Pelvic Health. She was instrumental in starting one of the first Women’s Health Programs in an outpatient orthopedic clinic setting in Mercer county in New Jersey in 2009. She has authored articles on pelvic health for many publications. She is a Certified Integrated Manual Therapist through Great Lakes Seminars, is Board-certified in Orthopedics, is a certified Pelvic Rehab Practitioner and is also a registered yoga teacher through Yoga Alliance. Rachna has trained in both Hatha Yoga and Yin Yoga traditions and brings the essence of Yoga to her clinical practice.
Rachna Mehta PT, DPT, CIMT, OCS, PRPC, RYT 200 (she/her) graduated from Columbia University, New York with a Doctor of Physical Therapy degree. Rachna has since been working in outpatient hospital and private practice settings with a dual focus on Orthopedics and Pelvic Health. She was instrumental in starting one of the first Women’s Health Programs in an outpatient orthopedic clinic setting in Mercer county in New Jersey in 2009. She has authored articles on pelvic health for many publications. She is a Certified Integrated Manual Therapist through Great Lakes Seminars, is Board-certified in Orthopedics, is a certified Pelvic Rehab Practitioner and is also a registered yoga teacher through Yoga Alliance. Rachna has trained in both Hatha Yoga and Yin Yoga traditions and brings the essence of Yoga to her clinical practice.
Rachna currently practices in an outpatient setting. Her clinical practice has focused on an Integrative physical therapy approach blending traditional physical therapy methods with holistic practices that address the whole person - physically, mentally, emotionally, and spiritually. She specializes in working with pelvic health patients who have bowel & bladder issues with high pelvic pain which sparked her interest in Eastern holistic healing traditions and complementary medicine. She has spent many hours training in holistic healing workshops with teachers based worldwide. She is a member of the American Physical Therapy Association and a member of APTA’s Academy of Orthopaedic Physical Therapy and Academy of Pelvic Health Physical Therapy.
Rachna also owns TeachPhysio, a PT education and management consulting company. Her course Acupressure for Optimal Pelvic Health brings a unique evidence-based approach and explores complementary medicine as a powerful tool for holistic management of the individual as a whole focusing on the physical, emotional, and energy body.
I’ve been “on the record saying” I used to be a modalities skeptic. I didn’t think I used them a ton in my practice and when I switched from a big hospital system to my own private practice, I didn’t have access to the larger equipment machines like the big ultrasound or biofeedback devices.
I have, however, always been a fan of gadgets and tools as a pelvic health provider. For anyone who has ever been to a class where I was a teaching assistant, you’ve likely seen me literally roll in with a giant suitcase full of example things - models, pelvic trainers, examples of belts, braces, dilators, wands, weights, lube samples, pelvic organ stuffies etc. I always called it my toolkit and so many of my peers had this as well. When the Content & Curriculum team asked me to be on the team for writing for this project, I was initially unsure. I didn’t think I used modalities enough or valued them enough to create a two-day course on the topic.
Long story short…I was wrong. What I have learned is I was very wrong, and I use them constantly.
As we created the outline for Modalities and Pelvic Function, it became very clear that I had not really understood the definition of a modality. Spoiler alert, we spend the first lecture talking all about this. Once I understood that a modality is basically anything we use to create a change with a patient, I realized I LOVED them and used them all day, every day. I happily settled into writing with the team, reaching out to companies for samples, trial devices, and helped to make this AMAZING toolkit for a class that is like the biggest game of pelvic health show and tell.
I was lucky enough to be one of the instructors for the inaugural class and have been present at every class since. What I did not expect from this class was the “aha” moments and how well these helped students put it all together. Feedback-wise, our team always gets requests to “show more treatment” and “give skills to bring back to the clinic for treatment.” Welcome to two straight days of this for every pelvic topic we could think of in reference to bowel, bladder, and sexual dysfunction while also making room for oddball topics like patient education, models, and handouts.
If you have questions about this course, then look through the following FAQs. If you don’t see your question answered, then reach out to the Herman & Wallace team and they can answer it for you!
Will this class make me buy something?
Nope, no purchase is necessary, but we did work with a whole bunch of companies to get you some free samples or really good discounts if you want your own.
Does my pelvic floor have to be available for this class?
We do two labs with internal sensors so a provider can feel what biofeedback and e-stim feel like. You get to choose your sensor and preferred canal and apply your own device. For those who are a little shy about sharing their pelvis for the sake of science, I’ve been told this has been a really safe feeling option. If you’re not up for an insertable device, we offer external options as well.
What skills will I take home?
You’ll learn all the features of every modality that our writing team could think of all organized by topic and primary treatment usage (don’t worry, we’ll also share our pearls and hacks.) We’ll also talk about ways to teach your patients about these devices including why a device might be indicated, how it can be used, cleaned, etc.
Is this class for newbies or those who are seasoned?
Yes! We’ve had participants of all different experiences and skill levels find this class extremely useful and a great resource for their practice. If you work in pelvic health and are an expert in gadgets already, this may NOT be the course for you unless you’d like to be one of our awesome teaching assistants.
We’ve worked so hard to make Modalities and Pelvic Function a well-rounded learning experience. This class is ONLY in person and tends to be a very intimate group of providers, which was another request from our Herman & Wallace customers. We hope to see you at one of the five offerings of Modalities and Pelvic Function this year!
- Galloway, NJ - February 8-9
- Sacramento, CA - April 5-6
- Houston, TX - July 12-13
- Akron, OH - September 20-12
- Somerset, NJ - October 4-5
AUTHOR BIO
Mora Pluchino, PT, DPT, PRPC
 Mora Pluchino, PT, DPT, PRPC (she/her) is a graduate of Stockton University with a BS in Biology (2007) and a Doctorate of Physical Therapy (2009). She has experience in a variety of areas and settings, working with children and adults, including orthopedics, bracing, neuromuscular issues, vestibular issues, and robotics training. She began treating Pelvic Health patients in 2016 and now has experience treating women, men, and children with a variety of Pelvic Health dysfunction. There is not much she has not treated since beginning this journey and she is always happy to further her education to better help her patients meet their goals.
Mora Pluchino, PT, DPT, PRPC (she/her) is a graduate of Stockton University with a BS in Biology (2007) and a Doctorate of Physical Therapy (2009). She has experience in a variety of areas and settings, working with children and adults, including orthopedics, bracing, neuromuscular issues, vestibular issues, and robotics training. She began treating Pelvic Health patients in 2016 and now has experience treating women, men, and children with a variety of Pelvic Health dysfunction. There is not much she has not treated since beginning this journey and she is always happy to further her education to better help her patients meet their goals.
She strives to help all of her patients return to a quality of life and activity that they are happy with for the best bladder, bowel, and sexual functioning they are capable of at the present time. In 2020, She opened her own practice called Practically Perfect Physical Therapy Consulting to help meet the needs of more clients. She has been a guest lecturer for Rutgers University Blackwood Campus and Stockton University for their Pediatric and Pelvic Floor modules since 2016. She has also been a TA with Herman & Wallace since 2020 and has over 150 hours of lab instruction experience. Mora has also authored and instructs several courses for the Institute.
If you’ve spent any time on social media as a healthcare practitioner, you’ve probably encountered a flood of ads promoting shockwave therapy as a miracle solution for everything from orthopedic pain to urological and gynecological conditions. The marketing push for these devices has skyrocketed over the past five years, driven by claims of its ability to treat a wide range of diagnoses. Recent research, including a comprehensive review published in The Journal of Clinical Medicine, confirms that shockwave therapy is making significant waves in modern medicine. But with all the buzz surrounding this technology, the real question remains: is it truly a game changer for patients and clinics alike?
As a medical professional, my approach to any new treatment, procedure, or modality begins with skepticism. I believe it is my responsibility to ensure that the interventions I offer in my clinic are grounded in solid research, and proven efficacy. When I first encountered shockwave therapy in early 2020, I was highly skeptical. The companies I spoke with made sweeping claims, portraying shockwave therapy as a universal solution for virtually every condition. Despite their promises, I remained cautious. However, after hearing positive feedback from a few trusted colleagues and witnessing a session that yielded seemingly impressive results, I decided to delve deeper into the research.
I found that while there is a substantial amount of literature available, much of it is confusing and, it lacks clarity — especially in the area of pelvic health. The majority of the research outside of orthopedics focuses on conditions such as erectile dysfunction, with little attention given to men’s pelvic health concerns and even less given to women’s pelvic health issues.
Recent advances in shockwave therapy have highlighted its growing potential in the field of men's and women’s sexual and pelvic health. The latest research trends are clear. As a non-invasive treatment, shockwave is no longer considered solely beneficial for orthopedics and sports medicine. Its applications are expanding rapidly in gynecology, urology, and pelvic floor disorders. This shift is driven by the therapy’s ability to enhance blood flow immediately and provide significant pain relief faster than traditional methods, making it an innovative option for conditions such as chronic pelvic pain, dyspareunia, and vaginal atrophy.
However beneficial, the fact remains that confusion abounds when, as a clinician, you are deciding which device would be best for your patients. At the forefront of the confusion when you delve into the research are:
- protocols vary substantially between devices
- energy levels and units of measure aren’t consistent among devices,
- There are popular devices in the research labeled shockwave, when in fact, they do not produce shockwaves and create different outcomes.
If you would like to learn more about incorporating shockwave therapy into your daily practice, register for my one-day remote course Shockwave Treatment: Therapeutic Interventions in Pelvic Health & Demystifying the Research scheduled for October 22, 2024. This course provides an introduction to using this cutting-edge technology in the clinic for improved patient outcomes and an understanding of how shockwave can enhance manual therapy treatment skills. Course lectures cover what is shockwave, how it decreases pain and potentially accelerates healing, the research behind it, the different types of shockwave devices, and the best indications of use for each of them as well as case studies discussing patient protocols and outcomes.
AUTHOR BIO
Stacey Roberts, PT, RN, MSN

Stacey Roberts, PT, RN, MSN (she/her), has been a physical therapist specializing in outpatient orthopedics and sports medicine, since 1990. After completing a sports medicine fellowship and working at several hospitals and outpatient clinics, in 2000 Stacey had an opportunity to move overseas, where she became adept with complementary medicine approaches, becoming a master in herbalism in 2003. From 2004 to 2017, Ms. Roberts owned and operated a cash-based health and wellness clinic on the Gold Coast of Australia specializing in women’s health and hormones and couples' fertility, where she began seeing patients via Telehealth in 2006.
Combining her knowledge of functional medicine, conventional medicine, and complementary medicine, Stacey emphasizes lifestyle changes, and her treatment programs are based on cutting-edge evidence-based research. Currently, she is a co-principle investigator for an IRB-approved study related to shockwave and Dyspareunia.
She has written 3 hard-copy books and 7 ebooks on women’s health and couples' fertility. Her new book, The Pain-Free Formula: A Holistic Approach to Finally Getting Rid of Pain Without Surgery, Drugs, Or Injections, is coming out in 2025. Ms. Roberts has mentored over 100 medical professionals in her women’s health and couples fertility training program. After returning to the United States, Stacey was hired by a national physical therapy company, Aegis Therapies, from 2018 to 2020 to assist in the growth and development of their orthopedic outpatient practice in Wisconsin. She set records for the company related to bringing clinics to profitability faster than any of their other outpatient clinics in the country at that time.
From 2016- to 2020 Stacey was an associate clinical professor at the University of Wisconsin Milwaukee’s Physical Therapy doctoral program until opening New You Health and Wellness, a cash-based clinic, where she brings her knowledge of wellness, hormone health, fat loss, and musculoskeletal health to treating patients with issues related to musculoskeletal injuries, sexual health, and pelvic health. Since 2020 she has been analyzing Shockwave research extensively to develop clear and concise therapeutic applications and protocols for pelvic health, sexual health, and muscular-skeletal patients. She is finding extraordinary results with her patients using this modality in her cash-based practice.
Stacey completed her MBA in 2021, her RN license, and her master’s in nursing (MSN) in 2020. She will eventually complete a nurse practitioner certificate. Stacey has also appeared on World News Now in New York, was featured on Oprah, locally on TMJ4’s Morning Blend, and on several news shows and radio stations in the United States and Australia.
Surface EMG is the only modality that can isolate the active component of tone and is, therefore, a very valuable tool in the assessment of patients with altered tone conditions. However, it is the most misunderstood modality in pelvic health therapy. Rarely do practitioners see a topic so argued in pelvic rehabilitation as surface EMG biofeedback. Some practitioners boldly state they are for or against it on their social media accounts and clinic pages. Therapists are not questioning the use of biofeedback with neurologic or orthopedic applications, so why is it such a polarizing topic in pelvic health? The Pelvic Rehab Report sits down with faculty members Tiffany Lee and Jane Kaufman to discuss the tool they love. These two instructors have over 50 years of combined experience using biofeedback and have been teaching biofeedback board certification courses together for the past 16 years.
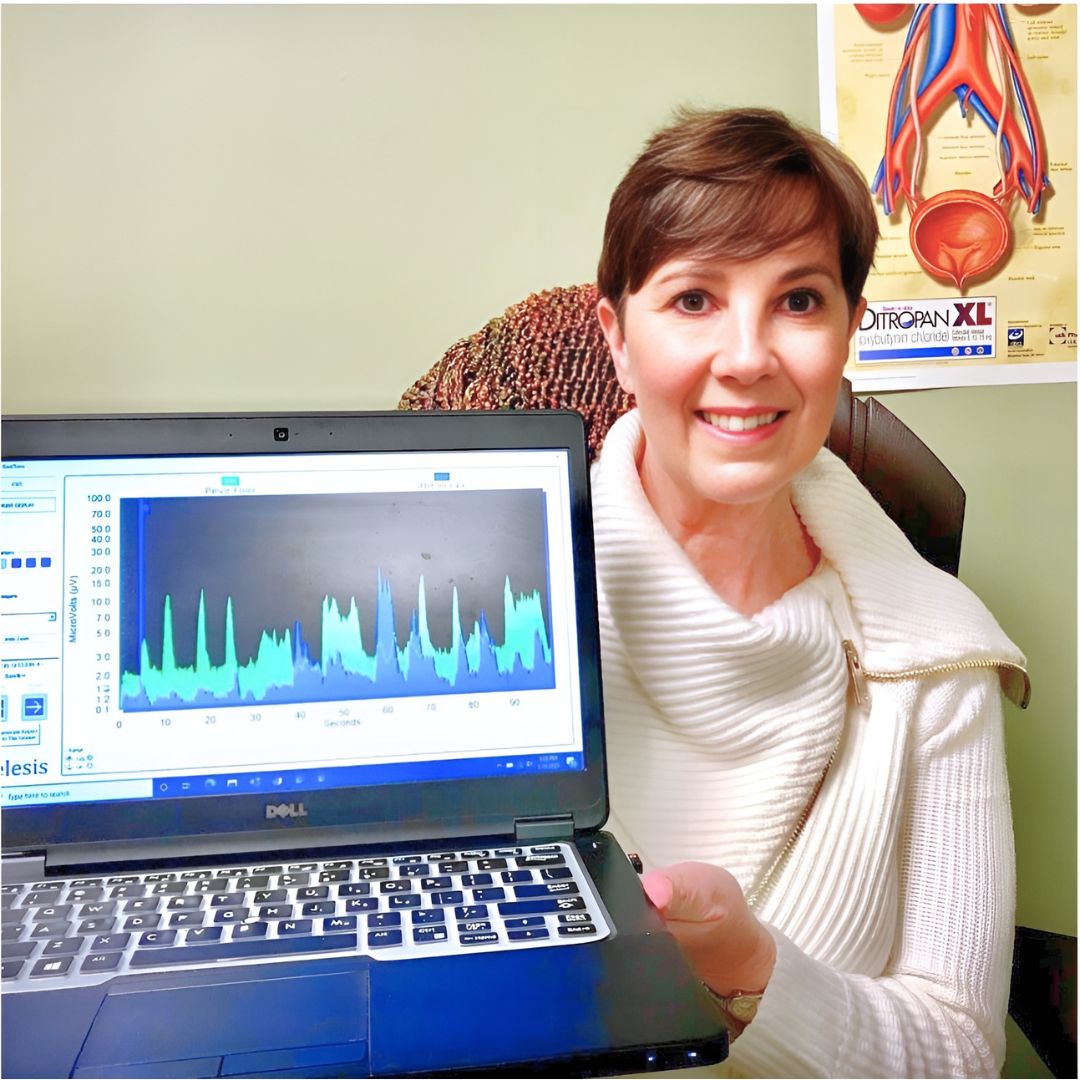
Biofeedback provides visual and auditory feedback of muscle activity and is a non-invasive technique that allows patients to adjust muscle function, strength, and behaviors to improve pelvic floor function. The small electrical signal (EMG) provides information about an unconscious process and is presented visually on a computer screen, giving the patient immediate knowledge of muscle function and enabling the patient to learn how to alter the physiological process through verbal and visual cues. Jane Kaufman explains “Many patients gain knowledge and awareness of the pelvic floor muscle through tactile feedback, but the visual representation helps patients hone in on body awareness and connect all the dots." Muscle evaluation through digital exam offers strength but does not appropriately address electrical activity such as resting tone and the ability to recruit or release tone in the muscle. The use of biofeedback addresses the specificity of muscle contraction and release, offering an additional view of muscle function.
In a 2020 research study by Pilkar et al., clinicians reported sEMG barriers of use, which included limited time and resources, clinically inapplicable sEMG system features, and the majority of clinicians' lack of training and/or confidence in the utilization of sEMG technology. This research also noted technical challenges, including the limited transfer of ever-evolving sEMG research into off-the-shelf EMG systems, nonuser-friendly intuitive interfaces, and the need for a multidisciplinary approach to accurately handling and interpreting data.
One barrier may be the price of a biofeedback unit. Tiffany Lee recommends using a 2-channel sEMG biofeedback hand-held unit with the software on a laptop or computer. In fact, to become board-certified in pelvic floor biofeedback, the Biofeedback Certification International Alliance (BCIA) requires a 2-channel EMG system with software. If you use a hand-held one-channel unit, the patient will have difficulty seeing the muscle activity and the coordination between the abdominals and pelvic floor. This prevents meaningful treatment as the patient cannot understand or interpret the LED bars on the machine (and often, the therapist cannot understand either). In truth, the benefits outweigh the cost of the equipment. You can cover the unit's cost and software to visualize muscle function and tone within a few treatments. Training is another issue; you need proper training in the modality to start utilizing biofeedback in your clinical setting. Most therapists have never been adequately trained. If they take a course where the instructor doesn’t believe in the benefits of biofeedback, they feel negatively toward a modality they have never personally explored. Biofeedback relies on a skilled clinician to interact with the patient, give verbal cues, ensure that the proper muscles are contracting and relaxing, and must be used in conjunction with their other skills and knowledge.
Think of sEMG biofeedback as one tool in your toolbox. Tiffany shares, "In a study by Aysun Ozlu MD et al., the authors conclude that biofeedback-assisted pelvic floor muscle training, in addition to a home exercise program, improves stress urinary incontinence rates more than a home exercise program alone." She continues, "Biofeedback is a powerful tool that can benefit your patient population and add to your skill set.
The acceptance of sEMG biofeedback in rehabilitation requires a unit (with software and sensors), training, and a multidisciplinary approach. Used correctly, it can positively impact patient performance and care in the clinic. Keep in mind that sEMG is a non-invasive technique. It has already shown great promise in neurorehabilitation and has been a widely utilized tool to assess neuromuscular outcomes in research. Jane Kaufman concludes, "Biofeedback treatment/training using the proper instrumentation provides the precise information necessary to change behaviors." This allows the patient to recognize that ‘yes, they are in charge of this muscle and that they can achieve success in overpowering the symptoms.’ Biofeedback routinely allows patients to understand that they are empowered to heal themselves with the tools you offer. They are in charge of their bodies and the outcome of treatment. It is also an important tool to use with patients who have experienced trauma and who are not ready to participate in manual therapy, and it is valuable for the pediatric population as well. Tiffany adds, “This modality can bring new business to your clinic. My local GI and colorectal providers often refer up to 5 new patients a week to my practice.
There is a long history of scientific evidence supporting the use of sEMG biofeedback in managing incontinence or pain symptoms. As a noninvasive, cost-effective, and powerful treatment modality, healthcare providers should consider this tool when managing pelvic floor dysfunction patients. Providers should be educated in the proper use of this valuable modality to gain the most out of the skills and knowledge that can be achieved through this intervention. For more information regarding courses and certification, please visit www.pelvicfloorbiofeedback.com.
Tiffany asked several PTs and OTs who have been to the board certification courses what they love about biofeedback. Here are a few answers
- “Biofeedback empowers my patients and gives them the confidence that they are actually doing their exercises and relaxing correctly! I’ve had nothing but positive feedback from patients, and it’s such a great tool to have as a pelvic floor therapist.”
- “My patients really love it, and they ask for it. I especially see the value for dyssynergia work on bearing down and learning eccentric abdominals and relaxed pelvic floor muscles. For men, I work on relaxing in standing and toileting postures if they can’t empty their bladder.”
- “Ultimately, the treatment needs to be meaningful to the patient. Biofeedback can complement other treatments. Their needs come before ours. We should offer all of our patients the ability to control their own muscles and SEE how to do it.”
- “After ONE session with a 5-year-old with constipation, mom called me in sheer excitement, screaming over the phone that he pooped on the potty!!! Something he has NEVER done before. Biofeedback helped him find and coordinate the potty muscles and tummy muscles, and this made a huge difference for him!”
- “Becoming certified in biofeedback has only been positive for me. My patients feel that the initial sEMG evaluation sets the stage for my care plan, and my discharge reassessment is a tangible reflection of their progress. Not to mention its strength as a marketing tool.”
Jane Kaufman adds “Biofeedback in treatment has been a game changer. Using this tool as a foundation for treatment in my clinic allowed my practice to grow, thrive, and achieve great acclaim in our region and beyond. It is not unusual for patients to travel several hours to seek treatment because of the empowering effect the biofeedback visual had on their understanding of their dysfunction.”
Biofeedback for Pelvic Floor Muscle Dysfunction is scheduled for July 28th and December 7th, 2024, and provides a safe space for clinicians to learn and practice this valuable tool. Registrants will need equipment to participate in this online course and will learn about the benefits of using this modality in their clinical practice.
In this course, Tiffany and Jane guide participants through learning to administer biofeedback assessments, analyze and interpret sEMG signals, conduct treatment sessions, and role-play patient instruction/education for each diagnosis presented during the many hands-on lab experiences.
References:
- Use of Surface EMG in Clinical Rehabilitation of Individuals With SCI: Barriers and Future Considerations Rakesh Pilkar, Kamyar Momeni, Arvind Ramanujam, Manikandan Ravi, Erica Garbarini, Gail F. Forrest. Front Neurol. 2020; 11: 578559. Published online 2020 Dec 18. doi: 10.3389/fneur.2020.578559 PMCID: PMC7780850
- Comparison of the efficacy of perineal and intravaginal biofeedback-assisted pelvic floor muscle exercises in women with urodynamic stress urinary incontinence. Aysun Ozlu MD, Neemettin Yildiz MD, Ozer Oztekin MD. Neurourol Urodyn. 2017 Nov;36(8):2132-2141. Epub 2017 Mar 27. doi: 10.1002/nau.23257 PMID: 28345778.
- Cram, J. R., & Kasman, G. S. (2011). The basics of surface electromyography. In E. Criswell (Ed.). Cram’s introduction to surface electromyography (2nd ed., pp. 3–7.) Jones and Bartlett.
- Kaufman, J., Stanton, K., & Lee, T. E. (2021). Pelvic Floor Biofeedback for the Treatment of Urinary Incontinence and Fecal Incontinence. Biofeedback, 49(3), 71-76.
- Shelly, Beth & Kaufman, Jane (2023). Foundations of Pelvic Floor Muscle Assessment Using Surface Electromyography. APTA Academy of Pelvic Health Physical Therapy.
AUTHOR BIOS
Tiffany Lee, OTR, OTD, MA, BCB-PMD, PRPC

Tiffany Lee holds a BS in OT from UTMB Galveston (1996), an MA in Health Services Management, and a post-professional OTD from Texas Tech University Health Sciences Center. In 2004, she received her board certification in Pelvic Muscle Dysfunction from the Biofeedback Certification International Alliance. She is a Herman & Wallace Pelvic Rehab Institute faculty member and teaches biofeedback courses. She has been treating pelvic health patients for 25 out of her 30-year career. Her private practice in San Marcos, Texas, is exclusively dedicated to treating urinary and fecal incontinence and pelvic floor disorders. Her continuing education company, Biofeedback Training & Incontinence Solutions, offers clinical consultation and training workshops. She also enjoys mentoring healthcare professionals working toward their BCIA certification.
Jane Kaufman, PT, M.Ed, BCB-PMD
Jane has been practicing PT for more than fifty years. She is a graduate of the Ithaca College Physical Therapy program and earned her master’s degree at the University of Vermont. In her early career, she practiced in outpatient settings, skilled nursing, and acute rehabilitation. Jane’s career began at Columbia Presbyterian Medical Center and progressed to the University of Vermont Health Network where she supervised the Department of Physical Therapy’s outpatient services. In the late 1990s, Jane became intrigued with pelvic floor muscle dysfunction, evolving to a quarter-century career in this highly specialized field.
In 2001 she began her career as a sole practitioner in pelvic floor muscle dysfunction and in 2003 established Phoenix Physical Therapy, PLC with a staff of clinicians specializing in the treatment of pelvic floor dysfunction, incontinence, and pelvic pain for all genders and all ages. In 2005, Jane became certified in the use of surface EMG biofeedback for pelvic floor muscle dysfunction (BCB-PMD ) from the Biofeedback Certification International Alliance. She sold her practice in 2022, having established a renowned reputation in Vermont, upstate New York, regionally, nationally, and internationally. Post Phoenix, Jane continues to offer workshops for other healthcare providers in the use of biofeedback for pelvic muscle dysfunction, and mentors healthcare professionals around the world toward certification in this field through the Biofeedback Certification International Alliance. Jane teams with Tiffany Lee, OTR, OTD through Biofeedback Training and Incontinence Solutions (www.pelvicfloorbiofeedback.com).
Jane has recently begun a consulting practice helping adults with pelvic floor muscle dysfunction issues and has continued helping children/teens through her new practice, PottyTime Physical Therapy (www.pottytimephysicaltherapy.com). In addition to her practice and teaching, Jane has participated in research through the University of Vermont Health Network on pelvic organ prolapse, incontinence, and sexual dysfunction. She has authored an article published in the online international journal Biofeedback and was a co-author in the APTA self-study manual for Foundations in Pelvic Floor Muscle Assessment using Surface Electromyography with Dr. Beth Shelley, PT, DPT, WCS, BCB-PMD. She is a Herman & Wallace Pelvic Rehabilitation Institute faculty member and teaches biofeedback courses through this company. Jane may be reached by email at: This email address is being protected from spambots. You need JavaScript enabled to view it.

Congratulations on completing Pelvic Function Level 1 (PF1) and entering the world of pelvic rehabilitation. Are you ready for your next course but not quite sure which one to take? Well, you’re not alone. Everyone’s pelvic health educational journey is different based on their interests and patient demographics and there are a lot of course options available.
I’m going to zero in on the intermediate-level courses in the Pelvic Function Series for you as HW does recommend that practitioners take at least one or two of these. If you’ve looked at the course page you’ve noticed that there are three courses with a Level 2 designation – as well as a lab course. What does this mean? These courses are designed to be a progression of knowledge and skills learned in the foundational course Pelvic Function Level 1.
Here are the intermediate courses:
- Pelvic Function Level 2A (PF2A) - Colorectal Pelvic Health, Pudendal Neuralgia, and Coccyx Pain
- Labs provide an introduction to internal anorectal examination for all genders.
- Pelvic Function Level 2B (PF2B) Urogynecologic Examination and Treatment Interventions
- Labs provide external abdominal and pelvic and internal vaginal approaches.
- Pelvic Function Level 2C (PF2C) Men’s Pelvic Health and Rehabilitation
- Labs provide external abdominal, gluteal, perineal, and internal anorectal approaches.
- Modalities and Pelvic Function (PFMOD) The Pelvic Health Toolkit
- Labs provide supervised instruction to practice modalities.
Ready for a more in-depth look at the courses? Here is a more detailed breakdown:
Pelvic Function Level 2A (PF2A) Colorectal Pelvic Health, Pudendal Neuralgia, and Coccyx Pain
This course is intended for the pelvic health clinician who treats patients with common functional gastrointestinal (GI) dysfunctions and is interested in learning internal anorectal examination and the use of balloon re-training.
In this course, you will learn about common functional gastrointestinal (GI) dysfunctions including irritable bowel syndrome, fecal incontinence, and constipation. Course topics provide an introduction to nutrition for bowel health, colorectal conditions, and oncology. Participants will be educated on how diagnoses such as hemorrhoids, fistulas, fissures, and anorectal pain including pudendal neuralgia and coccygodynia may be improved with pelvic rehabilitation.
Practical, trauma-aware, hands-on labs provide supervised instruction of pelvic function evaluation with external observation, palpation, and internal anorectal examination of pelvic skeletal and soft tissues. These labs include an external perineal and internal anorectal approach as well as education in the use of balloon re-training.
Pelvic Function Level 2B (PF2B) Urogynecologic Examination and Treatment Interventions
This course is intended for the pelvic health clinician who treats patients with conditions including urinary incontinence, chronic pelvic pain (CPP), and pelvic organ prolapse.
In this course, you will learn, with increased specificity, evaluation for urogynecologic conditions as well as an overview of medical management, and multi-disciplinary pelvic healthcare. Course topics provide a more in-depth understanding of urinary incontinence, chronic pelvic pain (CPP), and pelvic organ prolapse. Participants will be educated on how diagnoses such as interstitial cystitis/painful bladder syndrome (IC/PBS), urinary tract infections, vaginismus, vulvar pain, dyspareunia, polycystic ovarian syndrome (PCOS), and endometriosis may be improved with pelvic rehabilitation.
Practical, trauma-aware, hands-on labs provide supervised instruction of pelvic structures in relationship to the vaginal canal and surrounding structures such as the lumbopelvic nerves, the uterus, urethra, bladder, and rectum. Interventions instructed will include patient management of trunk and pelvic pressure, relaxation training, breathing, and manual therapies for a variety of pelvic dysfunctions. These labs include an external abdominal and pelvic and internal vaginal approach.
Pelvic Function Level 2C (PF2C) Men’s Pelvic Health and Rehabilitation
This course is intended for pelvic health clinicians who are interested in treating male pelvic health conditions.
In this course, you will learn critical detailed information about men’s pelvic health conditions including post-prostatectomy urinary incontinence, erectile dysfunction, and chronic pelvic pain (CPP). Participants will be educated on how diagnoses such as hard/flaccid, urgency/frequency, scrotal, testicular, and penile pain may be improved with pelvic rehabilitation.
Practical, trauma-aware, hands-on labs provide supervised instruction of pelvic health evaluation with external observation, palpation, and internal anorectal examination of pelvic structures and soft tissues. These labs include an external abdominal, gluteal, perineal, and internal anorectal approach.
Modalities and Pelvic Function (PFMOD) The Pelvic Health Toolkit
This course is for the pelvic health clinician who has the opportunity to use modalities as an adjunct to their patient's care and goes beyond the "Big 3" (E-Stim, Biofeedback, and Ultrasound).
In this course, you will learn about and practice a variety of modalities. Modalities in PFMOD include biofeedback, cold laser/light therapy, electrotherapy, real-time ultrasound imaging, belts, braces, supports, lubricants, myofascial tools/techniques, and “special topics” that can be used to assist in relaxation, bowel and bladder health, and sexual function. Specialized knowledge from experts in different subjects will be shared throughout the course.
Certain modalities that are impractical to practice live will be shared and demonstrated via video. These Interventions include shockwave, rehabilitative ultrasound imaging, dry needling, and light therapy.
Practical, trauma-aware, hands-on labs provide supervised instruction to practice utilizing biofeedback and other modalities to allow kinesthetic learning before prescribing and recommending them to patients.
Previous course sponsors who have provided samples and products have included:
- Nix
- Flyte
- OhNut
- Replens
- RockTape
- Bellies Inc.
- Ice Soothers
- BabyBellyBand
- Intimate Rose
- The Pro Group
- Good Clean Love
- Cushion Your Assets
If you are interested in taking an intermediate-level Pelvic Function Course but still have questions, then please contact us.
Have you ever heard the phrase “In one ear and out the other?” I sure have, I have vivid memories of my grandmother scolding me for just that. She could never understand how when she said things to me, particularly a list of tasks to do, I could never seem to remember. Funnily enough, my grandfather’s nickname for me was “rabbit ears” because he swore I could pick up on a conversation from anywhere in close proximity so it wasn’t my hearing. Pretty conflicting and confusing, right? I had trouble processing things I heard or remembering them long enough to do them. Years of Catholic school helped to give me structure and tools to keep myself and my fun little brain organized and on task, and I ended up being able to keep up with the rest of my class.
The older and more self-aware I got, the more I realized my brain doesn’t work the way everyone else’s does. The more I worked with kiddos with autism and ADHD, the more I realized my brain worked similarly to theirs. When I first heard the term “neurodivergent” I felt immediately like I had found the answer to a question I didn’t even know existed for myself. This was why I wasn’t the same as other people in processing all things! This is why I had to touch everything to learn about it. This is why I had to rewrite all my notes from professors instead of just being able to absorb what they said. This is why I needed mnemonics, stories, acronyms, and other little “hacks” to learn things.
There are many different ways people can learn. The most common forms of learning consider if a person learns best through visual, aural/ auditory, reading/writing, or kinesthetic movement. Individuals can be any combination of these, which can vary as they grow through life. Someone may start out learning better kinesthetically and learn to process information better visually as they age. In our COVID era, a new format of teaching became more prevalent, bringing “at distance” learning in to save the day in many instances.
The prevalence of distance learning via forums such as Google Meet or Zoom brought up some questions about how well students could learn. Did students learn as well virtually? Did different types of learners have different results? Did how students felt they learned correlate with the outcome measures of learning? Distance education provides the ability for some populations to get education they would not be able to attain otherwise. In a study by Wakahiu & Kangethe, 2014, “participants described learning experiences with profound statements that endorsed online learning as an excellent strategy for fulfilling their dreams to acquire an education.”
Distance learning has many benefits including the ability to learn new materials and achieve new intellectual goals in most locations on a flexible time schedule. Another benefit is the access to visual resources and the potential to be able to rewatch. The decreased cost of transport and the safety (and hopefully less stress) of staying home were also huge benefits. Some disadvantages include not being able to guarantee effective learning, the ability to stay attentive, or be successful with materials. There can be connection and technological problems as well as some students not having the best learning environment in their home (Masalimova et al, 2022). When I think of learning and pelvic health, I think not having face-to-face interaction, accountability, and reinforcement of practicing the skills can hinder some student’s learning ability.
A report by the U.S. Department of Education compared the exam grades for online and face-to-face versions of the same course from 1996 to 2008 and concluded that “online learning could produce learning outcomes equivalent to or better than face-to-face learning (Zheng, 2021).” Cacault et al., 2021 also assessed the effects of online lectures finding that having access to a live-streamed lecture in addition to an in-person option “improves the achievement of high-ability students, but lowers the achievement of low-ability students.”
How does this apply to Herman and Wallace? The pelvic institute has a variety of ways to learn including online courses, self-hosted options, satellite in-person classes with TAs, and in-person classes with instructors. They have made sure to account for different scenarios in order to make pelvic health learning accessible for all they can. The newest addition to the categories of “in person” and “with instructors” is Modalities and Pelvic Function. I had the pleasure of being on the curriculum team for this class and also being one of the instructors for the first run.
I thought people would like the stuff. I thought they would be excited to try biofeedback and electrical stimulation. I thought they would be pleasantly surprised by prizes and goodie bags full of awesome takeaways. I knew it would be a novel learning experience.
What I did not expect was the overwhelming feedback from participants stating things like“this course was one of the best I have met for my learning style.” The curious part is that when they were asked what their preferred learning style was, they were all different! Some liked to see, some needed to hear it, and some just were there to touch and feel and touch again. Varied practitioners, varied experience levels, varied treatment settings and population and one very consistent point of feedback…”This class just gets me.”
If you’re on the hunt for a class that “puts it all together” when it comes to the tools and toys that can be used for the pelvic floor, check out Modalities and Pelvic Function. Not only are there SO MANY samples (think three shipping crates full - sorry UPS) BUT this class shows you how much is out there to treat pelvic health patients, the pros/cons, the indications, contraindications, and relative precautions as well as the language on how to educate your patient on the use of these items in the clinic or as part of their home self-care routine. Join me this summer either in Raleigh NC on July 13-14 or in Manchester NH on August 24-25!

Don’t believe me…here are two testimonials from our inaugural class!
“Of all of the pelvic floor courses I have taken up to date, this is by far the most enjoyable one! not only did it include how to efficiently treat patients, but it was well organized, exciting content, and everyone was lovely! the instructors were so personable and taught in a way to benefit any learning style. I will be recommending this to all of my fellow PF PTs!” - Rachel Biek, PT, DPT
“I loved the in-person portion of this class! The instructors (Mora and Jenna) were perfect in their roles, we were relaxed and had so much fun exploring the variety of tools to use. The feel of the class was supportive and intimate, and we had adequate time to explore everything. Mora and Jenna did an excellent job, hard to believe this was their first time teaching this class!” - Allison M. Gannon, PT, DPT
REFERENCES:
- Cacault, Christian Hildebrand, Jérémy Laurent-Lucchetti, Michele Pellizzari, Distance Learning in Higher Education: Evidence from a Randomized Experiment, Journal of the European Economic Association, Volume 19, Issue 4, August 2021, Pages 2322–2372, https://doi.org/10.1093/jeea/jvaa060
- Masalimova, A. R., Khvatova, M. A., Chikileva, L. S., Zvyagintseva, E. P., Stepanova, V. V., & Melnik, M. V. (2022, March). Distance learning in higher education during COVID-19. In Frontiers in Education (Vol. 7, p. 822958). Frontiers Media SA.
- Wakahiu, J., & Kangethe, S. (2014). Efficacy of online distance learning: Lessons from the Higher Education for Sisters in Africa Program. European Journal of Research and Reflection in Educational Sciences, 2(1), 1-25.
- Zheng, M., Bender, D. & Lyon, C. Online learning during COVID-19 produced equivalent or better student course performance as compared with pre-pandemic: empirical evidence from a school-wide comparative study. BMC Med Educ 21, 495 (2021). https://doi.org/10.1186/s12909-021-02909-z
AUTHOR BIO:
Mora Pluchino, PT, DPT, PRPC

I am a graduate from Stockton University with my BS in Biology (2007) and Doctorate of Physical Therapy (2009). I have experience in a variety of areas and settings, working with children and adults, including orthopedics, bracing, neuromuscular issues, vestibular issues, and robotics training. I began treating Pelvic Health patients in 2016 and now have experience treating women, men, and children with a variety of Pelvic Health dysfunction. There is not much I have not treated since beginning this journey and I am always happy to further my education to better help my patients meet their goals.
I strive to help all of my patients return to a quality of life and activity that they are happy with for the best bladder, bowel, and sexual functioning they are capable of at the present time. In 2020, I opened my own practice called Practically Perfect Physical Therapy Consulting to help meet the needs of more clients. I have been a guest lecturer for Rutgers University Blackwood Campus and Stockton University for their Pediatric and Pelvic Floor modules since 2016. I have also been a TA with Herman and Wallace since 2020 and have over 150 hours of lab instruction experience.

There are currently two scheduled course offerings available for Modalities and Pelvic Function: Philadelphia PA in April 6-7 and Manchester NH in August 24-25. If neither of these work for your location or schedule then consider hosting! The hosting requirements and interest form can be found on the Host a Course page.
The new Modalities and Pelvic Function - Pelvic Health Clinical Toolkit is an in-person two-day continuing education course targeted to pelvic health clinicians covering frequently used modalities in pelvic health, including biofeedback and EStim. This course was designed to answer the clinician’s need to understand how to choose and access the right tools, both for in-clinic care and for patient self-care application.
One of the course co-creators, Mora Pluchino shared “This class will be unlike one you've taken before. The H&W curriculum team sat down and thought about how we could make this the most interactive, hands-on, and practical course while still staying evidence-based and professional. This will be an in-person learning opportunity with 2 days of lab, demonstration, and interactive learning opportunities. If there is a modality that exists in pelvic health, it will likely have a debut here. This class is made for anyone who wants to learn to apply modalities in the variety of uses possible for pelvic health!"
Biofeedback and electrical stimulation are covered in this course, as are introductions to understanding tools such as shockwave, dry needling, real-time ultrasound, laser, and electrotherapies. With hands-on lab time and learning modules grouped into tools specific to pelvic health conditions such as bowel dysfunction and sexual health challenges, practitioners will have the opportunity to trial various tools and applications that previously may have only been available as an image in a presentation.
When our popular Pelvic Function Level 1 course, which introduces participants to the world of pelvic health, was transitioned to a satellite lab course one of the content pieces that was left out was the modalities focus - simply because the equipment was too difficult to ship to multiple satellite locations around the country. Herman & Wallace is thrilled to announce that not only have we solved this issue, but designed a way for clinicians to learn about dozens of modalities in an environment that allows the clinician to move beyond theoretical and soundly into the practical delivery of a variety of technologies and tools.
Current Medical Technologies will be in-person with us as we design this learning experience and will be available to answer your questions about products and clinical set-up. The interactive environment has been designed to be stimulating and allow the clinician to apply a variety of learning strategies including tactile opportunities to try things on themselves or a lab partner. This is a unique course that provides a foundational understanding of technology and tools, clinical practice research, and recommendations in an in-person environment. Many equipment providers have been generous in providing sample products for trial and even some giveaways to take home!
We believe this Modalities course is so foundational to our skillset in pelvic health that we have added it to our core Pelvic Function Series. This course is intended to be taken after Pelvic Function Level 1 and can be taken at any point following the introductory course as you work your way through the PF Series. If you’re wondering “When should I take this course?” the answer is “as soon as you can!”
Rehabilitative ultrasound imaging has been used in clinical practice for well over a decade now. It has been used for core stabilization, as well as with female incontinence patients. In recent years, transperineal ultrasound imaging has emerged as a useful tool for assessing prolapses and identifying other women’s health issues in the anterior compartment.
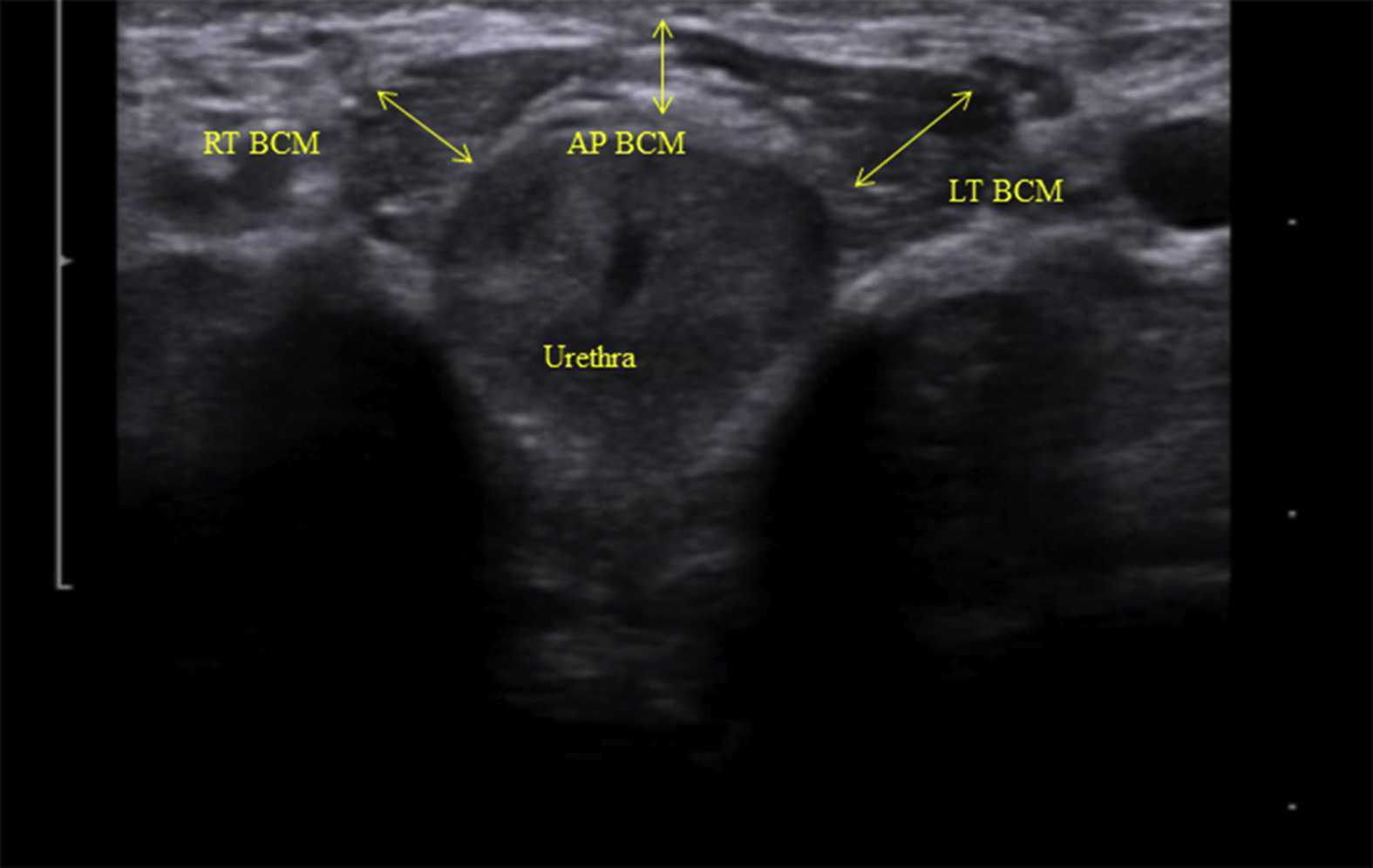
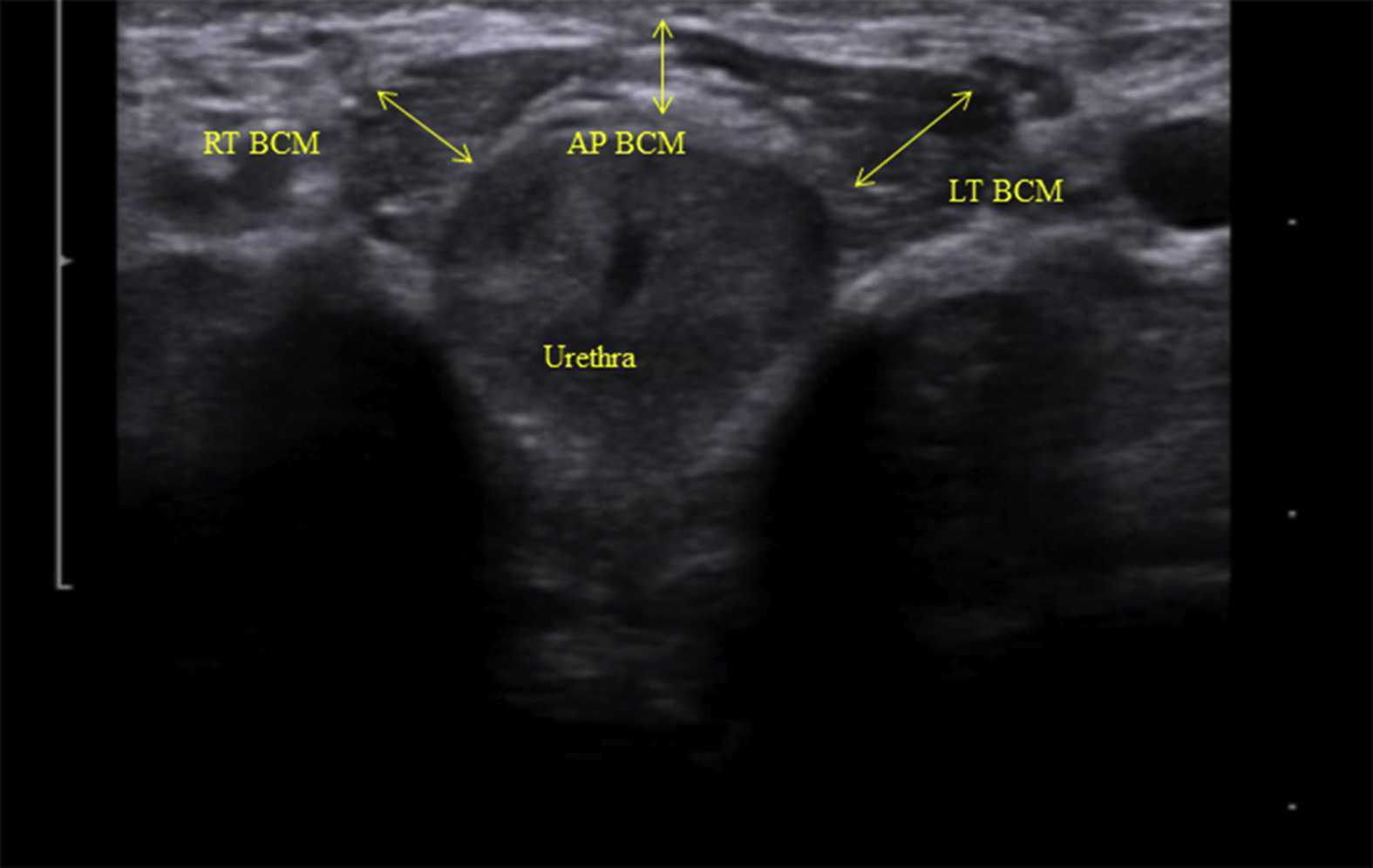 Like other things in men’s pelvic health, the use of ultrasound imaging for rehabilitation has lagged behind that in women’s pelvic health. Ryan Stafford is a researcher that is working to change that. In 2012, Stafford began looking at the normal responses to pelvic floor contractions and what is seen on ultrasound in men. He has since taken his research further to examine differences in men that present with post-prostatectomy incontinence. Stafford, van den Hoorn, Coughlin, and Hodges performed a study looking at the dynamic features of activation of specific pelvic floor muscles, and anatomical parameters of the urethra. The study included forty-two men who had undergone prostatectomy. Some of these men were incontinent and others remained continent. Transperineal ultrasound imaging was used to obtain images of the pelvic structures during a cough, and a sustained maximal contraction. The research team calculated displacements of pelvic floor landmarks with contraction, as well as anatomical features including urethral length, and resting position of the ano-rectal and urethra-vesical junctions.
Like other things in men’s pelvic health, the use of ultrasound imaging for rehabilitation has lagged behind that in women’s pelvic health. Ryan Stafford is a researcher that is working to change that. In 2012, Stafford began looking at the normal responses to pelvic floor contractions and what is seen on ultrasound in men. He has since taken his research further to examine differences in men that present with post-prostatectomy incontinence. Stafford, van den Hoorn, Coughlin, and Hodges performed a study looking at the dynamic features of activation of specific pelvic floor muscles, and anatomical parameters of the urethra. The study included forty-two men who had undergone prostatectomy. Some of these men were incontinent and others remained continent. Transperineal ultrasound imaging was used to obtain images of the pelvic structures during a cough, and a sustained maximal contraction. The research team calculated displacements of pelvic floor landmarks with contraction, as well as anatomical features including urethral length, and resting position of the ano-rectal and urethra-vesical junctions.
The data was analyzed and combinations of variables that best distinguished men with and without incontinence were reported. Several important components were identified in the study. Striated urethral sphincter activation, as well as bulbocavernosus and puborectalis muscle activation were significantly different between men with and without incontinence. When these two parameters were examined together, they were able to correctly identify 88.1% of incontinent men. They further reported that poor function of the puborectalis and bulbocavernosus could be compensated for if the man had good striated urethral sphincter function. However, the puborectalis and bulbocavernosus had less potential to compensate for poor striated urethral sphincter function. This is important for a therapist that works with post prostatectomy patients to know. This can explain part of why some men improve and do so well after a prostatectomy and others don’t, even with therapy to help. If the striated urethra sphincter is damaged and its normal responses are changed during surgery, then incontinence after prostatectomy may be more likely.
Using ultrasound imaging, the therapist can examine and see exactly where a man is deficient in response; whether it is the puborectalis, or the striated urethra sphincter. It is exciting to see this new research and see how rehabilitative ultrasound imaging can influence men’s pelvic health! Come and learn how to use ultrasound imaging for your men’s pelvic health patients as well as your women’s health and back pain patients! You will see how ultrasound imaging can change your practice and how much your patients will enjoy seeing real-time images of their contractions! Thanks to our partnership with The Prometheus Group, this course includes hands-on training on the latest in pelvic ultrasound imaging.
1. Stafford R, Ashton-Miller J, Constantinou C, et al. Novel insights into the dynamics of male pelvic floor contractions through transperineal ultrasound imaging. J. Urol. 2012; 188: 1224-30.
2. Stafford RE, van den Hoorn W, Couglin G, Hodges P. Postprostatectomy incontinence is related to pelvic floor displacements observed with trans-perineal ultrasound imaging. Neurol and Urodyn. 2018; 37:658-665.
Image credit Gupta et al. 2016 https://doi.org/10.1016/j.ajur.2016.11.002 https://www.sciencedirect.com/science/article/pii/S2214388216300881#fig2
Authors: Tamara Rial, PhD, CSPS, Kathleen Doyle-Elmer, PT, DPT and Rebecca Keller, PT, MSPT, PRPC
Tamara Rial, PhD, CSPS, co-founder and developer of Low Pressure Fitness will be presenting the first edition of Low Pressure Fitness and Abdominal Massage for Pelvic Floor Care Level 2 and 3 in Princeton, New Jersey in September, 2019. Rebecca Keller and Kathleen Doyle-Elmer are certified Low-Pressure Fitness specialists with training in rehabilitative ultrasound imaging. In this article, the authors discuss and explore the use of transabdominal ultrasound during Low Pressure Fitness on the abdominal and pelvic floor structures.
Real-time ultrasound imaging is a reliable and valid method to evaluate muscle structure, activity and mobility. Over the past few years, there has been increasing interest in the use of transabdominal ultrasound in the field of rehabilitation. The additional value of ultrasound imaging is that it allows for real-time analysis and visual feedback during the performance of pelvic floor and abdominal exercises (Hides et al., 1998). In the field of pelvic health, this is of notable importance when assessing proper movement of the deep abdominal and pelvic muscles during voluntary muscle actions. Transabdominal ultrasound has been found to be a safe, noninvasive, and accurate method to assess and observe muscular and fascial activity (Khorasani et al., 2012). When therapists learn how to properly use and apply ultrasound imaging, this technique can be a comprehensive tool for the clinician and a comfortable procedure for the patient. Moreover, it may be the method of choice for some patients who don’t want to have an internal pelvic examination (Van Delft, Thakar & Sultan, 2015). In this regard, a cross-sectional study found a moderate-to-strong correlation between ultrasound measurements and both digital examination and perineometry for the assessment of pelvic floor muscle actions (Volløyhaug et al., 2016).
Recently, Low Pressure Fitness has gained popularity as a pelvic floor training program aimed at reducing pressure on the pelvic structures while engaging the stabilizing muscles through postural and breathing exercises. In order to evaluate proper execution of Low-Pressure Fitness exercises as well as abdomino-pelvic muscle function during this type of training, real-time transabdominal ultrasound can be a clinically relevant tool.
Sagittal and Transverse Pelvic Floor/Urinary Bladder Assessment
The amount of movement of the bladder base on transabdominal ultrasound is considered an indicator of pelvic floor muscle mobility during pelvic floor muscle exercises (Khorasani et al., 2012). When properly executed, the Low-Pressure Fitness technique will allow the bladder to lift and the pelvic floor muscles to contract. These observed actions can be cued and progressed due to the real-time imaging biofeedback of the ultrasound. Because of the postural activation and diaphragm lift occurring during Low Pressure Fitness, the bladder fascial support system is tensioned resulting in a desirable bladder lift.
For example, we used a Pathway® Musculoskeletal Rehabilitative Ultrasound Imaging unit with a curvilinear transducer and Prometheus Pathway® rehabilitative ultrasound software utilizing the pre-set parameters (Abdominal Wall 7.5MHz and Bladder 5.0MHz) during a Low-Pressure Fitness basic supine posture. A standardized bladder filling protocol was used before imaging to ensure sufficient bladder filling to allow clear imaging of the base of the bladder and pelvic floor muscles.
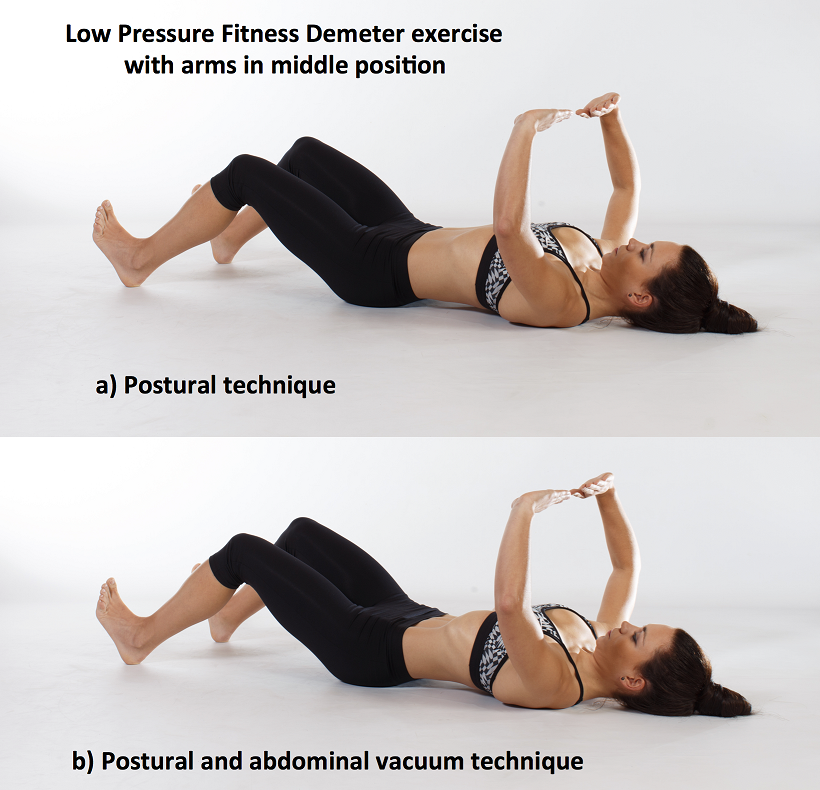
For the transverse view, radiologic standards were used, and the ultrasound transducer was placed in the transverse plane suprapubically and angled in a caudal/ posterior direction to obtain a clear image of the inferior-posterior aspect of the bladder. The participant was asked to perform the Low-Pressure Fitness Demeter exercise in the supine position with a neutral pelvis and knees flexed (Figure 1).
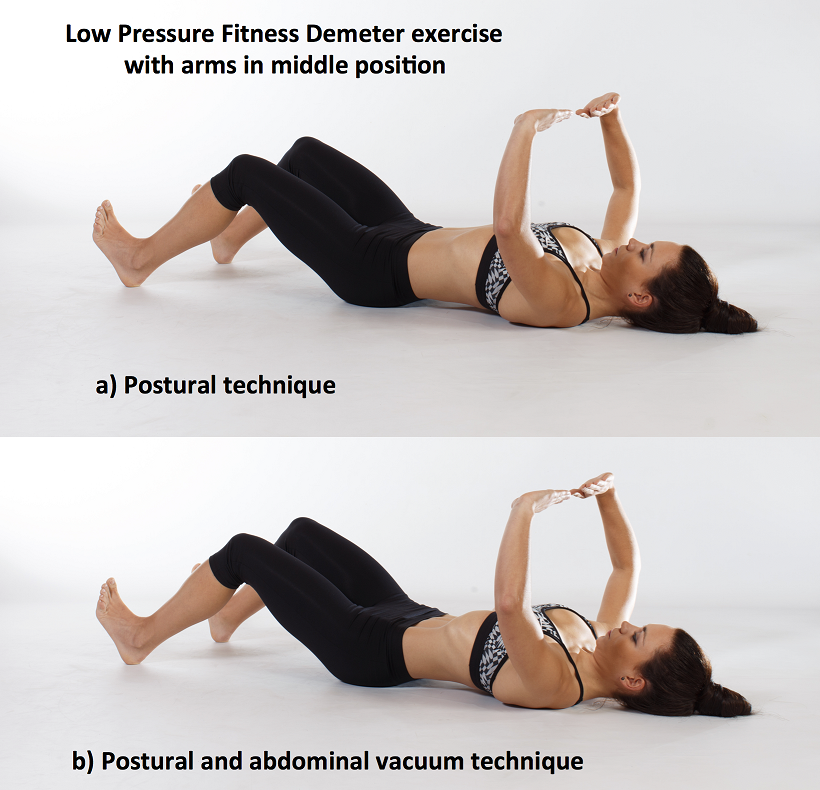
Figure 1. Demeter exercise with postural technique and with postural and abdominal vacuum technique combined.
The following video illustrates the pelvic floor/urinary bladder during: a) resting position; b) active pelvic floor contraction; c) Low Pressure Fitness Demeter exercise and; d) Low Pressure Fitness Demeter exercise combined with a voluntary pelvic floor muscle contraction. It is noticeable a greater bladder lift and pelvic floor activation with the postural and breathing cueing added to an active pelvic floor contraction than with the pelvic floor contraction alone.
Video of the behavior of the pelvic floor muscles in a sagital and transversal view during the supine position of Low Pressure Fitness and with the combination of an active pelvic floor muscle contraction.
Lateral Abdominal Wall Assessment
The lateral abdominal muscle ultrasound assessment allows us to observe the structural changes produced in the transversal section of the abdominal muscles in the midpoint between the anterior iliac crest and the costal angle. At low levels of contraction, the extent of transverse abdominis thickening measured using ultrasound is reported to be a valid method of assessment compared with either fine wire electromyographic measures of transverse activity (McMeeken et al., 2004). It is well established in the scientific literature that the lateral abdominal muscles provide stability to the trunk in different functional activities. Therefore, the assessment of the size, thickness and sliding of the abdominal wall is important for patients who present with lumbo-pelvic and/or pelvic floor dysfunctions. In this regard, patients with low back pain show different abdominal wall muscle activation patterns (i.e. less slide of the abdominal fascia and muscle thickness) than those without low back pain (Gildea et al., 2014; Unsgaard-Tondel et al., 2012).
Figure 2 shows the three muscle layers of the lateral wall in the resting position. The superficial layer corresponds to the external oblique, the middle layer to the internal oblique and the deep layer to the transverse abdominal muscle.
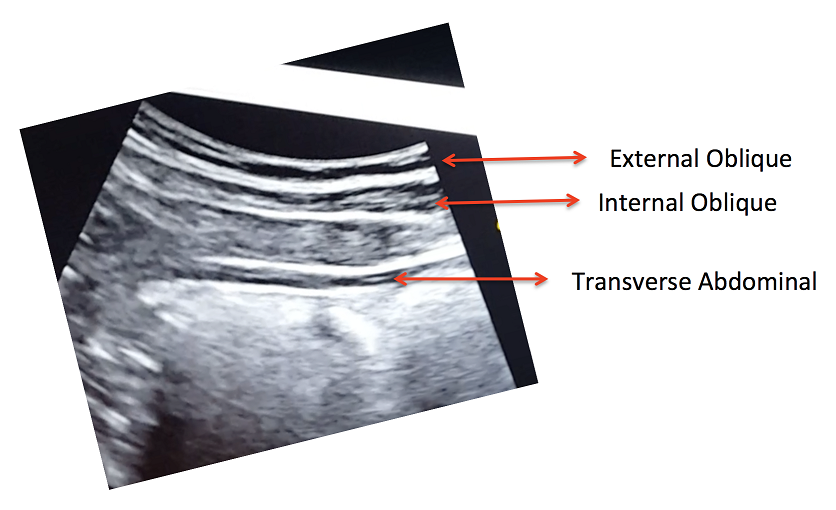
Figure 2. View of the right lateral abdominal wall at rest.
A key breathing component of the Low-Pressure Fitness program is the abdominal vacuum which manipulates intra-abdominal, intra-thoracic and intra-pelvic pressures during the breath-holding phase. Another key aspect of Low-Pressure Fitness is the shoulder girdle activation, spine elongation and ankle-dorsiflexion (Rial & Pinsach, 2017). Of note, previous studies have demonstrated greater transverse abdominis activation when performing ankle dorsi-flexion (Chon et al., 2010). We used transabdominal ultrasound to assess the lateral abdominal wall response during ankle dorsiflexion, shoulder girdle activation and the abdominal vacuum during Low Pressure Fitness.
In the following video, a voluntary (active) abdominal contraction is performed in order to distinguish this action from the involuntary abdominal contractions during Low Pressure Fitness. Afterwards, the postural technique of ankle dorsiflexion and shoulder girdle activation are performed in the Demeter exercise with arms in middle position (Figure 1). Lastly, an abdominal vacuum maneuver is added to the postural technique. If the exercises are properly executed, the progressive sliding and thickness of the abdominal muscles throughout exercise sequence should be observable (Figure 3).
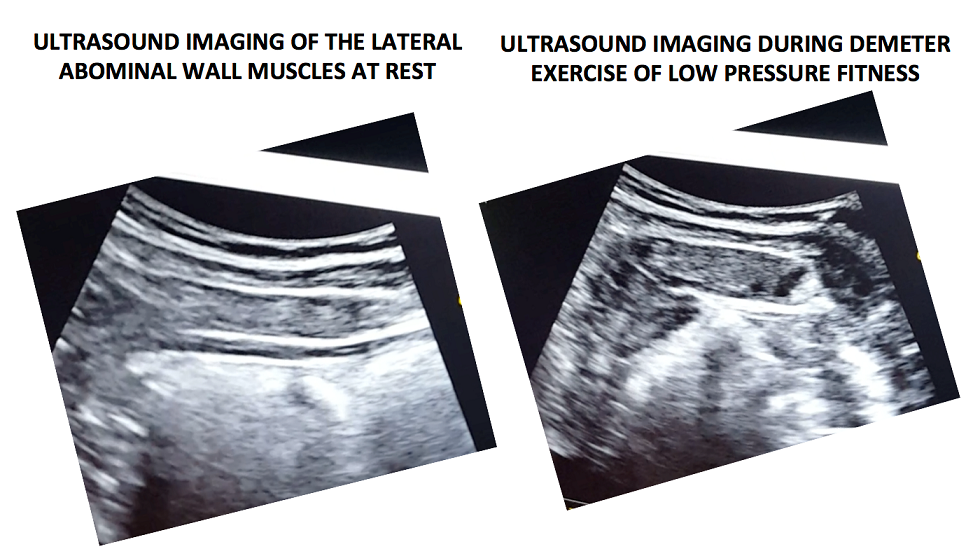
Figure 3. Ultrasound imaging at rest and during the complete LPF technique.
Video of a voluntary (active) abdominal contraction or draw-in maneuver is performed in order to distinguish this action from the involuntary abdominal contractions that occur during Low Pressure Fitness in a supine position
Muscle thickness of the transverse and internal oblique as well as a noticeable slide of the anterior abdominal fascia are observable during the Demeter exercise of Low-Pressure Fitness. This exercise pattern reflects an abdominal draw-in maneuver and a “corseting effect”. In this regard, notice the lateral pull or displacement of the edge of the anterior fascial insertion of the transverse the internal oblique muscle.
Navarro et al., (2017) used transabdominal ultrasound to assess the muscular responses of the pelvic floor and abdominal muscles in a group of women who underwent pelvic physiotherapy over two months. They found a significant increase in the transversal section of the transverse abdominis, external oblique, and internal oblique muscles when compared to resting in the supine position. Similar to the position assessed by Navarro et al. (2017), we also assessed the pelvic floor and abdominal muscle responses during a Low-Pressure Fitness supine exercise.
Transabdominal ultrasound can provide a noninvasive and informative visual biofeedback when training patients with Low Pressure Fitness. This ultrasound imaging can be a valuable tool to both the client and the clinician to objectify progress, assist with validating correct Low-Pressure Fitness form with positioning and vacuum/hypopressive maneuver as well as a motivational technique for the client. As demonstrated during our rehabilitative ultrasound imaging, observable bladder lift, pelvic floor activation and desirable lateral abdominal muscular corseting (slide and thicking) occurs during Low Pressure Fitness postural exercises and breathing. Since Low Pressure Fitness is a progressive exercise program, qualified instruction, technique driven progression and understanding pelvic floor health are needed to optimize patient outcomes.
Chon SC, Chang KY, You JS. Effect of the abdominal draw-in manoeuvre in combination with ankle dorsiflexion in strengthening the transverse abdominal muscle in healthy young adults: a preliminary, randomised, controlled study. Physiotherapy 96: 130-6, 2017.
Gildea JE, Hides JA, Hodges PW. Morphology of the abdominal muscles in ballet dancers with and without low back pain: a magnetic resonance imaging study. J Sci Med Sport. 17(5): 452-6, 2014.
Khorasani B, Arab AM, Sedighi Gilani MA, Samadi V, Assadi H. Transabdominal ultrasound measurement of pelvic floor muscle mobility in men with and without chronic prostatitis/chronic pelvic pain syndrome. Urology, 80: 673-7, 2012.
McMeeken JM, Beith ID, Newham DJ, Milligan P, Critchley DJ. The relationship between EMG and change in thickness of transversus abdominis. Clin Biomech 19: 337–342, 2004.
Hides JA, Richardson CA, Jull GA. Use of real-time ultrasound imaging for feedback in rehabilitation. Man Ther. 3:125-131,1998.
Navarro B, Torres M, Arranz B, Sanchez O. Muscle response during a hypopressive exercise after pelvic floor physiotherapy: Assessment with transabdominal ultrasound. Fisioterapia 39: 187-94, 2017.
Rial T, Pinsach P. Practical Manual Low Pressure Fitness Level 1. International Hypopressive & Physical Therapy Institute, Vigo, 2017.
Unsgaard-Tøndel M, Lund Nilsen TI, Magnussen J, Vasseljen O. Is activation of transversus abdominis and obliquus internus abdominis associated with long-term changes in chronic low back pain? A prospective study with 1-year follow-up. Br J Sports Med, 46(10): 729-34, 2012.
Van Delft K, Thakar R, Sultan AH. Pelvic floor muscle contractility: digital assessment vs transperineal ultrasound. Ultrasound Obstet Gynecol, 45: 217-22, 2015. Volløyhaug I, Mørkved S, Salvesen Ø, Salvesen KÅ. Assessment of pelvic floor muscle contraction with palpation, perineometry and transperineal ultrasound: a cross-sectional study. Ultrasound Obstet Gynecol 47: 768-73, 2016.