Pauline Lucas, PT, DPT, WCS, NBC-HWC, PYT, CMMI is the is the author and instructor of the Mindfulness and Meditation for Pelvic Health course. Pauline works as an integrative physical therapist, specializing in pelvic health, at the Mayo Clinic in Arizona. As faculty member at the Mayo Clinic Alix School of Medicine she is director of the Health Coaching course and teaches Introduction to Lifestyle Medicine. Additionally, she is the creator and instructor of a successful meditation program for Mayo Clinic employees and patients. Pauline is a frequent presenter for local, regional, and national medical conferences on topics related to mindfulness, women’s health, and integrative medicine. She presented twice at CSM, both on the therapeutic use of yoga for chronic pain as well as the use of mindfulness and meditation in rehabilitation. She is the owner of Phoenix Yoga and Meditation, www.phoenixyogaandmeditation.com
In 2014, JAMA published the findings of a systematic review on the use of mindfulness meditation programs for stress-related outcomes like anxiety, depression, and pain, in diverse groups of adults.1 The evidence suggested that mindfulness meditation programs could help reduce anxiety, depression, and pain in some clinical populations. The authors, therefore, concluded that clinicians should be prepared to talk with their patients about the role that a meditation program could have in addressing psychological stress.
As pelvic health providers, we frequently work with patients dealing with significant psychological stress, both the result of their condition, but often also a contributor to their symptoms. What is our role in addressing those stressors? And how do we manage our own well-being when providing care for patients with high-stress levels and sometimes strong emotions?
Colleagues sometimes ask me when I use mindfulness during my workday. My answer is that I aim to use mindful awareness all day; when I wash my hands, when I greet my patient, as I listen to their story, when holding space for a patient with strong emotions, when touching during an exam or treatment, and while staying present for myself at the same time.
The science is clear: when we as healthcare providers practice mindfulness, both we and our patients benefit. A mindful therapist helps the patient feel safe and heard, which improves the therapeutic relationship; one of the factors determining a positive or negative treatment outcome.2 Of course we need to have good clinical skills, but the therapist’s mindful presence is like “the secret sauce” that enhances everything else they provide in their interactions.
There are many studies on the effects of mindfulness training on mental health providers. Outcomes such as increased compassion, better counseling skills, less stress, and better quality of life, likely apply to pelvic health rehabilitation professionals as well. 3
These days we can easily learn the basics of mindfulness through various Apps, online classes, books, and podcasts. But with mindfulness has many aspects, and even some contra-indications, learning to create a personal practice and skillfully navigate the integration of mindfulness practices in patient care requires more in-depth training with a qualified instructor.
Would you like to learn about the origins of and the science behind mindfulness, create a personal mindfulness and meditation practice, explain mindfulness to your patients (without ever using the word mindfulness), what techniques to choose, and when to limit or avoid mindfulness practices with your patient? Join me for Mindfulness and Meditation for Pelvic Health on October 22-23.
References:
- Goyal M, Singh S, Sibinga EMS, et al. Meditation Programs for Psychological Stress and Well-being: A Systematic Review and Meta-analysis. JAMA Intern Med.2014;174(3):357–368. doi:10.1001/jamainternmed.2013.13018
- Brito, G. Rethinking Mindfulness in the Therapeutic Relationship. Mindfulness5, 351–359 (2014). https://doi.org/10.1007/s12671-012-0186-2(accessed August,31, 2022)
- https://www.apa.org/monitor/2012/07-08/ce-corner (accessed August,31, 2022)
Mindfulness and Meditation for Pelvic Health
Course Dates:
October 22-23, 2022
Price: $360
Experience Level: All
Contact Hours: 12
Description: This 2-day virtual course is geared toward the pelvic rehabilitation professional to enhance both their personal and professional life satisfaction and serve their patients in a more mindful way. You will learn how chronic stress impacts health and well-being and the latest research on the benefits of mindfulness training for both patients and healthcare providers. You will personally experience various mindfulness practices such as body scan, breath awareness techniques, mindful movement, and meditation, so you can experience the power and benefits first-hand. We will explore how to apply mindful awareness in clinical practice to improve your patients’ experience and treatment outcomes, in addition to making your day more peaceful and productive as you enhance your ability to stay focused and become less reactive to triggering situations. You will return to your clinic with the ability to explain mindful awareness and its benefits to your patients and introduce mindfulness into your patient care. You will be able to begin or deepen your own mindfulness practice and apply practical mindfulness skills to a busy workday and personal life to promote your own happiness and well-being.
This week the interviewer becomes the interviewee as Stacey Futterman Tauriello sits down to interview Holly Tanner on the Male Pelvic Floor course.
Stacey Futterman reached out to Holly Tanner back in 2007 through a phone call to see if they could partner on a lecture covering male pelvic pain. The two had never met in person but decided to collaborate on the three-hour APTA National Conference lecture. Holly shares "I still recall the frequent glances I made to match the person behind the voice I had heard for so many long phone calls.”
This presentation was developed into a two-day education course for Herman & Wallace and contained lectures on male anatomy, post-prostatectomy urinary incontinence, pelvic pain, and sexual health and dysfunction. The big question of the time was “should we allow men to attend?” Holly puts this in perspective, “As strange as this question now seems, it speaks volumes about the world of pelvic health at that time; mostly female instructors taught mostly female participants about mostly female conditions.”
The Male Pelvic Floor course was first taught in 2008 and has since been expanded to include 22 contact hours. This current content includes 7 pre-recorded lectures and 2 full days of live lectures and labs, allowing more time for hands-on skills in examination and treatment. The schedule still covers bladder, prostate, sexual health, and pelvic pain, and further discusses special topics like post-vasectomy syndrome, circumcision, and Peyronie’s disease.
Because the course often has providers in attendance who have not completed prior pelvic health training, instruction in basic techniques is included. For the experienced therapists, there are multiple lab “tracks” that offer intermediate to advanced skills that can be practiced in addition to the basic skills. Holly adds, “One of the more valuable conversations that we have in the course is how to create comfort and ease in when for most us, we were raised in a culture (and medical training) where palpation of the pelvis was not made comfortable. Hearing from the male participants about their bodies, how they are affected by cultural expectations, adds significant value as well.”
In 2017 Herman & Wallace faculty member, Heather Radar submitted a blog where she wrote about a note that was left on her doorstep by the wife of an older gentleman who had chronic male pelvic pain. When looking into writing this blog I kept coming back to this past blog by Heather, and I have decided to share an abridged version today to accompany Holly Tanner's short interview discussing the Male Pelvic Floor Satellite Lab Course.
Recently, a note was left at my doorstep by the wife of an older gentleman who had chronic male pelvic pain. His pain was so severe, that he could not sit, and he lay in the back seat of their idling car as his wife, having exhausted all other medical channels available to her, walked this note up to the home of a rumored pelvic floor physical therapist who also treated men. The note opened with how she had heard of me. She then asked me to contact her about her husband’s medical problem. It ended with three words that have vexed me ever since…we are desperate. We Are Desperate.
Unlike so many men with chronic pelvic pain, he had at least been given a diagnostic cause of his pain, pelvic floor muscle dysfunction, rather than vaguely being told it was just a prostate issue. However, the therapists that had been recommended by his doctor only treated female pelvic dysfunction.
My first thought after reading the note was, “I bet shoulder or knee therapists don’t get notes like this on their doorstep.” My next thought, complete with facepalm, “THIS HAS TO STOP! Pelvic floor rehab has got to become more accessible”.
Pelvic floor therapists see all people including men, women, and transgender. They treat the pediatric, adult, and geriatric populations. They treat pelvic floor disorders in the outpatient, home health, and SNF settings. They treat elite athletes and those with multiple co-morbidities using walkers. They can develop preventative pelvic wellness programs and teach caregivers how to better manage their loved one’s incontinence. This is due to one simple fact: No matter the age, gender, level of health, or practice setting, every patient has a pelvic floor.
The pelvic floor should not be regarded as some rare zebra in clinical practice when it is the workhorse upon which so many health conditions ride. It interacts with the spine, the hip, the diaphragm, and vital organs. It is composed of skin, nerves, muscles, tendons, bones, ligaments, lymph glands, and vessels. It is as complex and as vital to function and health as the shoulder or knee is, and yet students are lucky if they get a “pelvic floor day” in their PT or OT school coursework.
I call for every therapist, specialist, and educator to learn more about the pelvic floor. If you only treat pelvic dysfunction in women, please consider expanding your specialty to include men. The guys really need your help. You literally may be the only practitioner around that has the skills to treat these types of problems. Yes, the concerns you have about privacy and feeling comfortable are valid. But, you are not alone in this. Smart people like Holly Tanner have figured all that stuff out for you and can guide you on how to expertly treat in the men’s health arena.
The Silver Lining. Thanks to the champions of pelvic floor rehab education, we’ve come a long way. The good news in this story is that this man’s doctor recognized early that he had pelvic floor muscle dysfunction and recommended that he see a pelvic floor physical therapist. The bad news-it took 2 years before he could find one. The ball is in our court, therapists. Let’s do better. Until there are no more men in the back seat, we still need to #LearnMoreAboutThePelvicFloor.
We need to continue to create more coursework and more clinical training opportunities so that the representation of those treating male patients improves. If you feel ready to take your training to the next level in caring for male pelvic dysfunction, join us for an upcoming Male Pelvic Floor Satellite Lab Course.

Male Pelvic Floor Satellite Lab Course is scheduled on several dates and satellite locations for 2022, including self-hosted course options. Dates include:
- April 23-24
- June 12-13
- September 24-25
- October 22-23
- December 3-4
In a 2018 article by Holly Tanner, she explains how managing a medical crisis such as a cancer diagnosis can be overwhelming for an individual. ‘Faced with choices about medical options, dealing with disruptions in work, home, and family life often leaves little energy left to consider sexual health and intimacy. Maintaining closeness, however, is often a goal within a partnership and can aid in sustaining a relationship through such a crisis.” Research shows that cancer treatment is disruptive to sexual health. Intimacy is a larger concept that may be fostered even when sexual activity is impaired or interrupted.
Prostate cancer treatment can change relational roles, finances, work-life, independence, and other factors including hormone levels. (1) Exhaustion (on the part of the patient and the caregiver), role changes, changes in libido, and performance anxiety can create further challenges. (1, 3, 4) Recovery of intimacy is possible, and reframing of sexual health may need to take place. Most importantly, these issues need to be talked about, as a renegotiation of intimacy may need to take place after a diagnosis or treatment of prostate cancer. (2)
If a patient brings up sexual health, or the practitioner encourages the conversation, many research-based suggestions can be provided to encourage recovery of intimacy including:
• Redefining sex to include other sexual practices beyond penetration, such as massage or touching, cuddling, talking, use of vibrators, medication, aids such as pumps (5)
• Participation in couples therapy to understand their partner’s needs, address loss, be educated about sexual function (7)
• Participation in “sensate focus” activities (developed by Masters & Johnson in the 1970s as “touch opportunities”) with appropriate guidance (6)
Holly continues to share that “Within the context of this information, there is an opportunity to refer the patient to a provider who specializes in sexual health and function. While some rehabilitation professionals are taking additional training to be able to provide a level of sexual health education and counseling, most pelvic health providers do not have the breadth and depth of training required to provide counseling techniques related to sexual health - we can, however, get the conversation started, which in the end may be most important.”
Courses of Interest:
- A colorectal or male pelvic cancer diagnosis has multiple systems that are affected by cancer treatment. The rehabilitation professional that works with the pelvic oncology patient needs to competently navigate treatment techniques for all of these systems, as well as be confident in treating a patient in a personal area. This two-day course will address specific cancer types including prostate cancer, penile cancer, and testicular cancer. Additional cancer types covered include colorectal cancer and anal cancer.
Trauma Awareness for the Pelvic Therapist - Remote Course - Apr 9-10, 2022
- Bring their increased awareness of trauma to the successful, holistic treatment of patients with pelvic pain, sexual dysfunction, bowel dysfunction, and bladder dysfunction.
Sexual Medicine in Pelvic Rehab - Remote Course - Apr 9-10, 2022
- This course provides a thorough introduction to pelvic floor sexual function, dysfunction and treatment interventions for males and females of all sexual orientations, as well as an evidence-based perspective on the value of physical therapy interventions for patients with chronic pelvic pain related to sexual conditions, disorders, and multiple approaches for the treatment of sexual dysfunction including understanding medical diagnosis and management.
Male Pelvic Floor Function, Dysfunction, and Treatment - Satellite Lab Course - April 23-24 2022
- Discuss sexual anatomy and physiology, prostate issues, and look at the research describing models of intimacy and what worked for couples who did learn to renegotiate intimacy after prostate cancer. Participants will be able to describe the relationships between pelvic muscle function and men’s sexual health, including the evidence that demonstrates pelvic muscle rehabilitation's positive impact on erectile function.
1. Beck, A. M., Robinson, J. W., & Carlson, L. E. (2009, April). Sexual intimacy in heterosexual couples after prostate cancer treatment: What we know and what we still need to learn. In Urologic oncology: seminars and original investigations (Vol. 27, No. 2, pp. 137-143). Elsevier.
2. Gilbert, E., Ussher, J. M., & Perz, J. (2010). Renegotiating sexuality and intimacy in the context of cancer: the experiences of carers. Archives of Sexual Behavior, 39(4), 998-1009.
3. Hawkins, Y., Ussher, J., Gilbert, E., Perz, J., Sandoval, M., & Sundquist, K. (2009). Changes in sexuality and intimacy after the diagnosis and treatment of cancer: the experience of partners in a sexual relationship with a person with cancer. Cancer Nursing, 32(4), 271-280.
4. Higano, C. S. (2012). Sexuality and intimacy after definitive treatment and subsequent androgen deprivation therapy for prostate cancer. Journal of Clinical Oncology, 30(30), 3720-3725.
5. Ussher, J. M., Perz, J., Gilbert, E., Wong, W. T., & Hobbs, K. (2013). Renegotiating sex and intimacy after cancer: resisting the coital imperative. Cancer Nursing, 36(6), 454-462.
6. Weiner, L., Avery-Clark, C. (2017). Sensate Focus in Sex Therapy: The Illustrated Manual. Routledge, New York.
7. Wittmann, D., Carolan, M., Given, B., Skolarus, T. A., An, L., Palapattu, G., & Montie, J. E. (2014). Exploring the role of the partner in couples’ sexual recovery after surgery for prostate cancer. Supportive Care in Cancer, 22(9), 2509-2515.
Holly Tanner, PT, DPT, MA, OCS, WCS, PRPC, LMP, BCB-PMB, CCI is a faculty member and the Director of Education at Herman & Wallace. She owns a private practice that focuses on pelvic rehabilitation and on chronic myofascial pain. Along with H&W faculty member Stacey Futterman, she co-authored the Male Pelvic Floor course.
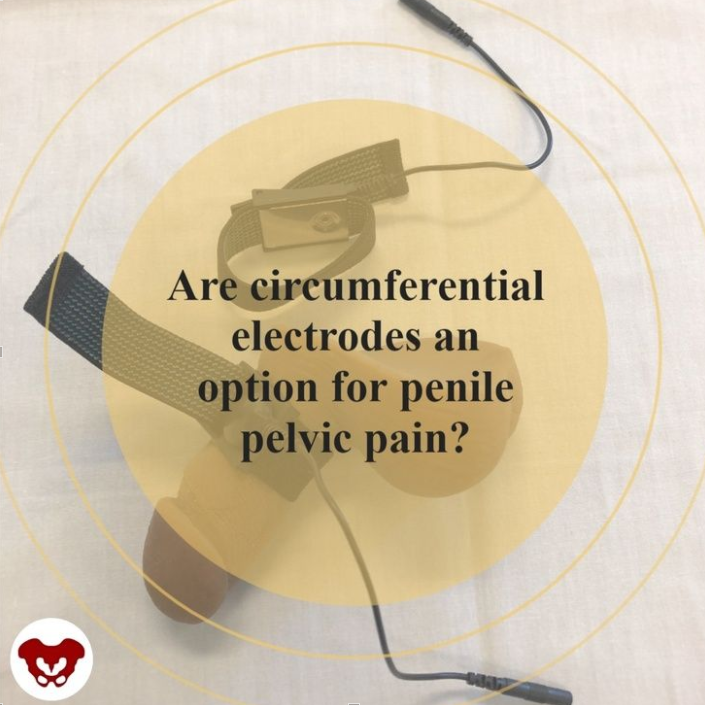
In the article by Schneider and colleagues (2013) “Refractory chronic pelvic pain syndrome in men: can transcutaneous electrical nerve stimulation help?” the authors conclude that TENS can be effective and safe as a treatment for pelvic pain. What is interesting about the technique they utilize in the intervention is that the electrodes are circumferential, designed to be worn around the penis itself. While this particular treatment may not be of interest for or applicable to all patients with pelvic pain, it may indeed be a valuable tool to add to the list of a comprehensive treatment approach, particularly for the patients who have penile pain or involvement of nerves such as ilioinguinal or the dorsal branch of the pudendal nerve that supplies the penis.
The patients in the report are defined as having “refractory pain” meaning that they have been treated and failed to improve. (Although the definition of “treated” would likely not include a comprehensive pelvic rehabilitation approach.) Patients treated themselves at home for 30 minutes, twice per day at 80 Hz, 150 µs at the sensory threshold level. Outcomes tools included a pain diary using a visual analog scale (VAS) and NIH-CPSI quality of life item at baseline, at 3 months after TENS use, and at last known follow-up appointment. 60 men aged 21-82 years were
Results included successful treatment after 12 weeks in 48% of subjects, and a positive effect was maintained in 21 patients after a mean follow-up of over 43 months. Success meant a greater than 50% reduction in pain VAS and a VAS less than or equal to 3. Pain visual analog scale decreased from 6.6 to 3.9, and QOL improved significantly as well. Fortunately, no adverse events were reported.
While circumferential electrodes are not the only type of electrodes that can be used in pelvic pain TENS application, these electrodes that have a stretchy band to help increased comfort and approximation of the treating surface can allow easy re-use of the electrode and direct placement over the penile tissues. in the image below, one electrode has been placed around the body of the penis and the other is left off simply for viewing the surface of the treatment surface of the electrode. One of 2 leads and electrodes could be used depending on location and extent of pain, and depending on patient preference. Current Medical Technologies carries circumferential electrodes if you are interested in purchasing them.
Although there is no one best treatment pathway for chronic pelvic pain, we can rely on the fact that most patients need multidisciplinary and multimodal support. For conditions that involve overactive nerves or referred pain into the penis, or even for distal treatment for more proximal discomfort, TENS may serve as one “tool in the toolbox” for chronic pelvic, and in particular, chronic penile pain. Pain in the glans, or end of the penis, can be a debilitating and frustrating aspect of pelvic pain (see prior blog post on Pain in the Glans Penis here (link: https://hermanwallace.com/blog/dysfunction-in-glans-penis), and the annoying, distracting sensation of clothing touching the penis can be a source of near-constant irritation. Neuromodulation can be one pathway to assist in moving beyond pain patterns, and it’s a pathway that can be relatively affordable and portable. Because TENS can be applied independently by many patients, TENS can also be a way to improve self-efficacy and provide one strategy for self-care that can be an adjunct to clinical care.
If you’d like to learn more treatment strategies for pelvic pain, the next Men’s Pelvic Health is taking place November 6-7, 2021. Click here (https://hermanwallace.com/continuing-education-courses/male-pelvic-floor-function-dysfunction-and-treatment-satellite-lab-course) to sign up for this course that will sell out! If you are unable to attend a Satellite location, you can easily sign up on your own by scheduling your own lab partner!
If you would like to purchase electrodes, you can find them on the CMT site here: https://www.cmtmedical.com/
Schneider, M. P., Tellenbach, M., Mordasini, L., Thalmann, G. N., & Kessler, T. M. (2013). Refractory chronic pelvic pain syndrome in men: can transcutaneous electrical nerve stimulation help?BJU Internationa
Holly Tanner, PT, DPT, MA, OCS, WCS, PRPC, LMP, BCB-PMB, CCI is a faculty member and the Director of Education at Herman & Wallace. She owns a private practice that focuses on pelvic rehabilitation and on chronic myofascial pain. Along with H&W faculty member Stacey Futterman, she co-authored the Male Pelvic Floor course.
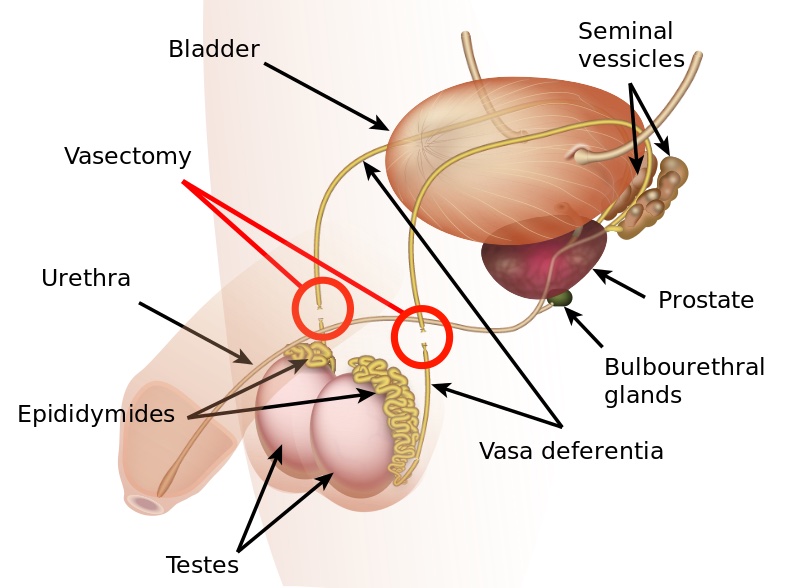
In the US, vasectomy is one of the most common procedures performed, and it is often completed in an outpatient setting with a local anesthetic. Fortunately for most folks, it’s well-tolerated and the advice to rest and ice is enough to allow full recovery. Unfortunately, there are those who don’t recover with ease and are left with chronic pain complications. This is a population that is often left out of the clinical rehabilitation setting, and there is not yet robust literature to catch up with the positive clinical results pelvic rehab providers observe when treating post-vasectomy pain.
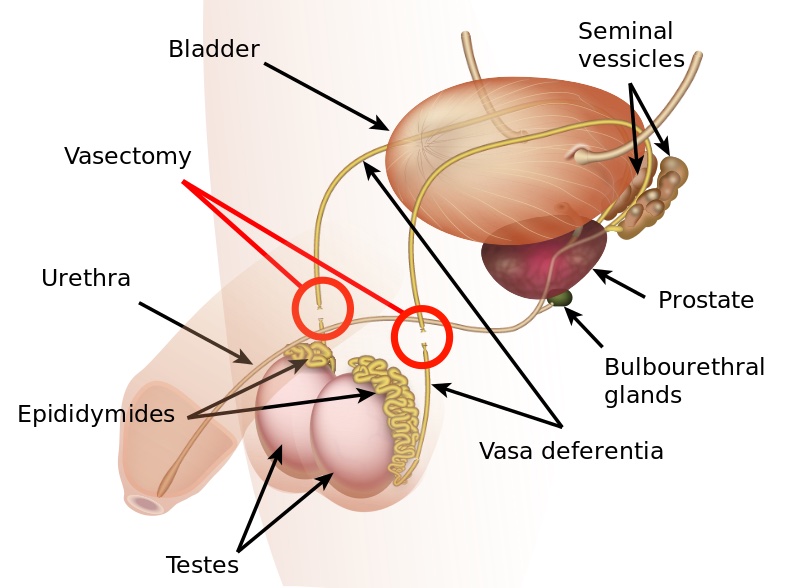
The Procedure
The goal of a vasectomy is typically contraception. The tube known as either the vas deferens or the ductus deferens is interrupted so that sperm does not travel to its typical destination outside the body via the urethra. This disruption in the tube takes place within the spermatic cord as it passes through the scrotum as this area is easily accessible. There are several techniques that can disrupt the tube where the sperm travels including, but not limited to, clamping, cauterization, or excision. The procedure leaves a small incision in the scrotal tissue.
Post-vasectomy Complications
Complications of a vasectomy may include bleeding and hematoma, infection, sperm granuloma (discussed below), chronic scrotal pain, seminal vesicle abscess (rare), and early or late canalization. (Sihra et al., 2007) Interestingly, some patients report less pain after vasectomy. (Leslie et al., 2007) Theories about the cause of post-vasectomy pain include interstitial fibrosis in the epididymal duct and perineurial fibrosis. (Lee et al., 2012) When we consider the anatomy, within the canal there may also be nerve irritation from the genitofemoral nerve, for example, or other connective tissues. If a patient had pain prior to the procedure in the low back, lower abdomen, or groin, the patient’s system may have been vulnerable to complications due to a sensitized system.
Examination & Rehab Efforts
When a patient presents with pain post-vasectomy, symptoms may worsen with prolonged sitting, with pressure from clothing, or in association with sexual or fitness activities. Because there has been a local insult to the tissues, it is logical to check the site of the procedure for any breakdown, signs of significant inflammation, swelling, and to examine for signs of infection such as fever. (Most patients have returned to their medical provider once pain develops, but if they haven’t, a referral is appropriate.) If the pain can be reproduced locally at the site of the procedure, the pain can often be managed by local treatment. You might find benefit in exam procedures such as a trunk or hip extension for the soft tissue tensioning as well as mechanical loading; palpation to the abdominal wall as well as within the spermatic cord. Treatment can address guarding of the area, general wellness (nutrition, movement, mental health), simple modalities such as heat, and gentle self-mobilization to the painful area.
Granulomas
Granulomas can form following a vasectomy, and while usually asymptomatic, a granuloma may be responsible for post-vasectomy pain. They are described as a “bag-like” structure with disintegrating spermatozoa that form at the cut ends of a vasectomy. (Chatterjee et al., 2001) If the granuloma is painful, very light manual mobilization of the thickened area may be done to alleviate pain (see image below). Mobilization of the spermatic cord itself via the testicle or more proximally may also prove helpful. Local modalities such as ultrasound or heat may improve symptoms as well, but clinically I have found that gentle manual therapy and movement exercises are enough to resolve the pain within a few weeks. Patients can be instructed to complete self-mobilization to the area of the granuloma, and as they often are scared to touch the area, helping alleviate this fear is useful in healing.

Post-vasectomy syndrome is very challenging for patients to manage, as they are often dismissed once the procedure is completed. Patients will share that they have been told “everything looks healed” and that the pain should go away on its own. Most providers are unaware of the role of pelvic rehab clinicians, and many pelvic rehab providers are less knowledgeable about conditions related to the scrotum and spermatic cord. For patients who do not respond to conservative intervention, vasectomy reversals have been found to be significantly helpful in reducing pain, though it’s often undesired due to the goal of contraception that inspired the vasectomy. (Herrel et al., 2015; Polackwith et al., 2015). Ideally, patients will be provided with an early recommendation to pelvic rehab so that further procedures or undoing of the vasectomy is avoided.
If you’d like to learn more about post-vasectomy syndrome and many other conditions that can go unrecognized and under-treated, the next opportunity to take the Male Pelvic Floor course is coming up July 9-10,2021!
Chatterjee, S., Rahman, M. M., Laloraya, M., & Pradeep Kumar, G. (2001). Sperm disposal system in spermatic granuloma: a link with superoxide radicals. International journal of andrology, 24(5), 278-283.
Herrel, L. A., Goodman, M., Goldstein, M., & Hsiao, W. (2015). Outcomes of microsurgical vasovasostomy for vasectomy reversal: a meta-analysis and systematic review. Urology, 85(4), 819-825.
Lee, J. Y., Chang, J. S., Lee, S. H., Ham, W. S., Cho, H. J., Yoo, T. K., ... & Lee, S. W. (2012). Efficacy of vasectomy reversal according to patency for the surgical treatment of postvasectomy pain syndrome. International journal of impotence research, 24(5), 202-205.
Leslie, T.A., R.O. Illing, D.W. Cranston, J. Guillebaud (2007). “The incidence of chronic scrotal pain after vasectomy: a prospective audit.” BJU International 100: 1330-1333.
Polackwich, A. S., Tadros, N. N., Ostrowski, K. A., Kent, J., Conlin, M. J., Hedges, J. C., & Fuchs, E. F. (2015). Vasectomy reversal for postvasectomy pain syndrome: a study and literature review. Urology, 86(2), 269-272.
Megan Pribyl, PT, CMPT is a practicing physical therapist at the Olathe Medical Center in Olathe, KS treating a diverse outpatient population in orthopedics including pelvic rehabilitation. Megan’s longstanding passion for both nutritional sciences and manual therapy has culminated in the creation of her remote course, Nutrition Perspectives for the Pelvic Rehab Therapist, designed to propel understanding of human physiology as it relates to pelvic conditions, pain, healing, and therapeutic response. She harnesses her passion to continually update this course with cutting-edge discoveries creating a unique experience sure to elevate your level of appreciation for the complex and fascinating nature of clinical presentations in orthopedic manual therapy and pelvic rehabilitation.
As a course developer and instructor for the Herman & Wallace Pelvic Rehab Institute, it is a privilege to continue sharing my passion for nutrition and pelvic rehabilitation with professionals nationwide. Interest in the topic continues to grow, and many pelvic rehab providers have identified nutrition as the “missing link” in their clinical practice. Nutrition Perspectives for the Pelvic Rehab Therapist has helped hundreds of pelvic rehab professionals integrate nutrition-related information into their clinical practice since 2015.

In the realm of nutrition, few questions provoke discussion with the same fervor as our title question: Organic Food vs. Conventional: Is There Any Difference? This question deserves a multi-dimensional answer - not unlike many topics in nutrition - including accessibility concerns, ethical factors for farmers, socio-economic factors, and our unique agricultural construct here in the United States. But the question about organic vs. conventional might just be the most important one deserving a thoughtful discussion to unravel the complexities around the topic of food.
You see, the answer to this question has profound implications for us. As we expand our ability to identify potential root contributors to conditions commonly encountered in pelvic rehabilitation, we must factor in nutrition. At first glance, it might be a stretch to see how one might link organic foods and potential effects on conditions such as constipation, inflammatory bowel diseases, IBS, PBS, and endometriosis for example. However, looking at food in a functional way, we acknowledge there may be under-appreciated qualitative differences between foods grown organically or produced conventionally.
Take, for example, the recent article by Kesse-Guyot et.al., 2020. which discusses the prospective association between organic food consumption and the risk of type 2 diabetes. In this study of over 30,000 participants, those with the highest quintile of organic food consumption compared to those with the lowest quintile had a 35% lower risk of having type 2 diabetes. The conclusion made by the authors was that organic food consumption was inversely associated with the risk of type 2 diabetes.
Said a different way, the study described a phenomenon where, for example, you might eat an organic bowl of oatmeal for breakfast and I might eat the same serving size conventional bowl of oatmeal for breakfast. If we extrapolate the comparison over our entire dietary intake pattern, you would have a 35% lower risk for developing type 2 diabetes compared to me…..despite you and I “eating the same foods”. How can this be possible? And might this begin to explain the sheer exasperation and frustration that can evolve in persons trying to make positive dietary changes - only to find they have no notable effect? How many times do you hear someone say “I am trying to eat healthily but it doesn’t seem to make a difference”.

Keeping in the context of type 2 diabetes, it is very well established that reductions in the richness and diversity of healthy microbes inhabiting the large intestine (gut dysbiosis) are correlative to metabolic syndrome. In those with type 2 diabetes, microbiomes showed a decrease in anti-inflammatory, probiotic, and other [beneficial] bacteria that could be pathogenic. (Das et al, 2021) Appreciating the differences between organic vs conventional - it is also well established that organic foods do carry less residue of herbicides and pesticides. These residues - which are found in higher concentration in conventionally produced foods - have been implicated in the same reduction in richness and diversity of microorganisms in the gut - which is contributory to dysbiosis. (Rueda-Ruzafa et all, 2019) Therefore it now seems not just plausible - but probable that there is a distinguishable difference between organic and conventional diets - to a degree at which all health care providers would do well to take notice.
In a report on the history of organic agriculture, author George Kuepper points out that:
“Pioneers of the organic movement believed that healthy food produced healthy people and that healthy people were the basis for a healthy society.”
And if organic foods can be a part of that, our patients deserve to know that these scientifically documented differences exist.
As our awareness of the connection between nutrition and health grows, so does the need to follow the science to share evidence-based and evidence-informed information. It is now more important than ever to have a working knowledge of nutrition basics as a pelvic rehabilitation professional. Plan to join us at one of our upcoming remote offerings of “Nutrition Perspectives for the Pelvic Rehab Therapist”: June 19-20 where we will explore this and many additional - and fascinating facets of the nutrition discussion.
Das, T., Jayasudha, R., Chakravarthy, S., Prashanthi, G. S., Bhargava, A., Tyagi, M., . . . Shivaji, S. (2021). Alterations in the gut bacterial microbiome in people with type 2 diabetes mellitus and diabetic retinopathy. Sci Rep, 11(1), 2738. doi:10.1038/s41598-021-82538-0
Kesse-Guyot, E., Rebouillat, P., Payrastre, L., Alles, B., Fezeu, L. K., Druesne-Pecollo, N., . . . Baudry, J. (2020). Prospective association between organic food consumption and the risk of type 2 diabetes: findings from the NutriNet-Sante cohort study. Int J Behav Nutr Phys Act, 17(1), 136. doi:10.1186/s12966-020-01038-y
Kuepper, George. (2010) A Brief Overview of the History and Philosophy of Organic Agriculture. Kerr Center for Sustainable Agriculture. http://kerrcenter.com/wp-content/uploads/2014/08/organic-philosophy-report.pdf Accessed May 14, 2021.
Rueda-Ruzafa, L., Cruz, F., Roman, P., & Cardona, D. (2019). Gut microbiota and neurological effects of glyphosate. Neurotoxicology, 75, 1-8. doi:10.1016/j.neuro.2019.08.006
Images:Par, Cecilia for Unsplash.
USDA organic seal.svg. Public Domain.
Fears about treating men’s health conditions are limiting access to care or are creating potential for harm in the field of pelvic health. Many cisgender women (women whose gender identify matches the sex likely assigned at birth) express concerns about working with cisgender men beyond a lack of knowledge about conditions related to prostate issues, urinary leakage, or genital pain. Are these fears warranted, are they fair? Rather than assert that ciswomen should simply move beyond their concerns, the field of pelvic health and the patients with whom we work may be better served by digging in and talking more openly about such fears. Following are some of the concerns or comments I have heard expressed by cisgender women within the context of treating men’s health matters:

- (Regarding palpation of the penis:) “Is that legal?”
- “I worry about being alone in a room with a man.”
- “What if he gets an erection?”
- “My husband doesn’t want me to work with other men for pelvic health stuff.”
- “I’ve never seen a man’s genitals before and I’m not comfortable with it.”
- “My religion teaches that I should not touch a man other than my husband.”
- “I don’t know what to say when men make suggestive comments.”
- “My supervisor is forcing me to do this work with men when I don’t want to.”
- “I only treat them in side lying because then I don’t have to see their stuff.”
Rather than a reader making a judgement about the above comments, we should ask ourselves as a profession if the above topics have been properly addressed in our training or if we are encouraged to work through this area of professional and personal intersecting concerns. We could view the concerns expressed through the lens of providing equal care, in other words, are we discriminating against someone based on their genitals? Or through a lens of safety- is there an actual (as well as perceived) threat from a cisgender woman who is alone in a treatment room with a cisgender man? If that’s potentially true, how are we mitigating this risk? Where does the anatomical line end between personal beliefs such as “I can touch another man’s shoulder, but not perineal area”? Are we practicing ethically if we are denying access to care or providing less than comprehensive care? Is a therapist truly worried about their primary relationship by doing this work because their partner does not approve? And more importantly, can we provide needed guidance or support to address some of the above obstacles?
I commonly have the opportunity to work with men who have seen other self-identified female therapists first. Here is what I often hear:
- “I could tell that they weren’t comfortable talking to me about this issue.”
- “It didn’t seem like they knew what to do with me.”
- “I got switched over to another therapist after asking some questions about using a penile pump.”
- “I felt really shamed about my condition because they would change the subject.”
- “I called many places and they rejected seeing me because I’m a man.”
- “When I asked if they were going to examine where the pain is [genital area] they said it would be a last resort.”
- “No one ever examined me, just gave me a biofeedback sensor to put in.”
This information is not shared to shame the caring professionals in our field. What needs to happen, however, for elevating the inclusiveness of care, is a continual dialogue and recognition of the support needed to work with sensitive conditions and the vulnerabilities of both patients and providers. It is potentially harmful to reject patients based on gender, or to provide lesser care based on genitals. To further this conversation, the Institute has partnered with author and educator Leticia Nieto, who holds a degree in psychology and who wrote Beyond Inclusion, Beyond Empowerment: A Developmental Strategy to Liberate Everyone. Join Leticia and me (Holly Tanner) for our first 3-hour discussion that emphasizes talking, feeling, and thinking through some of the above concerns and challenges. The class will focus on discussion more than lecture, and will aim to provide a space within which we can speak openly about how to move forward with the goal of improving comfort when working with men’s health issues and improving access to much needed pelvic health care. Note: this class is welcoming to all people with any gender identification, however, the emphasis will be on the topics discussed in this post.
Often pelvic floor therapists see men for post-prostatectomy urinary leakage. However, at least for me, that quickly led to seeing male patients for pelvic pain and sexual dysfunction. Male sexual dysfunction is a broad category and can consist of erectile dysfunction (ED), ejaculation disorders including premature ejaculation (PE), and low libido -- often there is a pelvic floor muscle (PFM) dysfunction component. Conservative treatment frequently consists of pharmacological and lifestyle changes for this population.
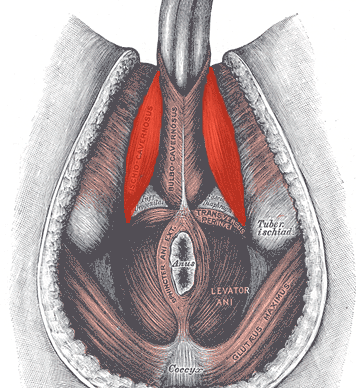
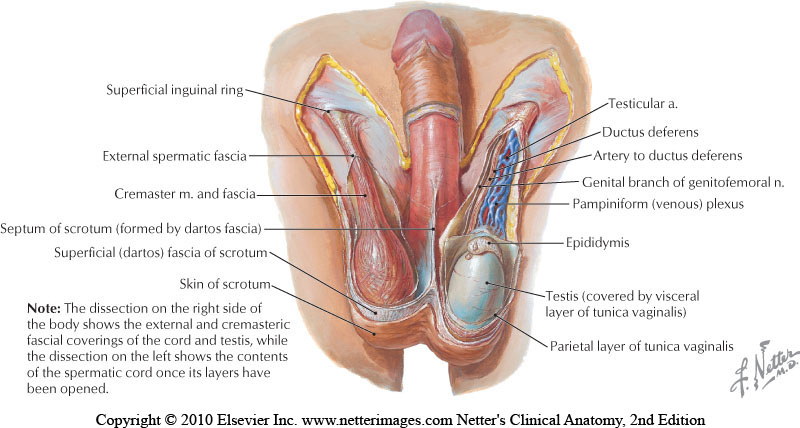
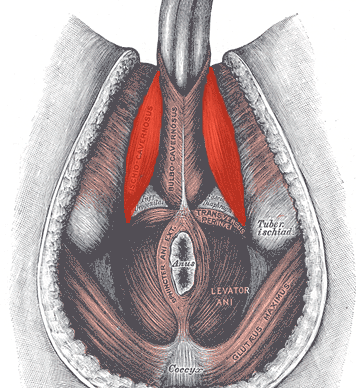
In normal sexual function, the male superficial pelvic floor musculature (bulbocavernosus and ischiocavernosus) work together to create increased intracavernosus pressure by limiting venous return, resulting in an erection. Ejaculation is created by rhythmic contractions of the bulbocavernosus muscle.
 The authors of this systematic review were curious if pelvic floor muscle training was effective for treating erectile dysfunction and premature ejaculation diagnoses, and if so to determine whether there is a treatment protocol. Ten studies were found that met the inclusion criteria, five that focused on ED and five that focused on PE. In total, there were 668 participants ranging in age from 30-59 years old. Studies were excluded if participants were post-prostatectomy and/or had a neurological diagnosis. The intervention was a pelvic floor program, and pelvic floor muscle contractions were either taught or supervised. Studies also included supportive treatment including biofeedback, lifestyle changes, and electrical stimulation.
The authors of this systematic review were curious if pelvic floor muscle training was effective for treating erectile dysfunction and premature ejaculation diagnoses, and if so to determine whether there is a treatment protocol. Ten studies were found that met the inclusion criteria, five that focused on ED and five that focused on PE. In total, there were 668 participants ranging in age from 30-59 years old. Studies were excluded if participants were post-prostatectomy and/or had a neurological diagnosis. The intervention was a pelvic floor program, and pelvic floor muscle contractions were either taught or supervised. Studies also included supportive treatment including biofeedback, lifestyle changes, and electrical stimulation.
The studies focused on erectile dysfunction listed a combination of hormonal, psychogenic, arteriogenic, and venogenic causes. The pelvic floor training ranged from 5-20 visits over 3-4 months and included a home exercise program. Pelvic floor training was similar in all studies and consisted of maximal quick contractions over one second and submaximal endurance holds over 6-10 seconds. Compliance to home exercise program was not assessed. Between 35% and 47% of participants reported a full resolution of symptoms. Subjective improvements were supported by improved maximal anal pressure and intracavernosus pressure. One study used the International Index of Erectile Function (IIEF) and showed significant improvement (p<0.05).
The studies focused on premature ejaculation noted participants had either lifelong or secondary PE. The pelvic floor training in these studies ranged from 12-20 sessions over 1-3 months. All studies used electrical stimulation as part of the pelvic floor muscle training. Four studies also used biofeedback. Only one study listed a home exercise program but did not report on compliance. The pelvic floor muscle training was compared to nothing in three studies, and to a selective serotonin reuptake inhibitor (SSRI) in the other two studies. Patient reported full resolution of symptoms was 55-83% in two studies, and there was a significant improvement in delay in heterosexual penetrative ejaculation (p<0.05) in three studies.
For both erectile dysfunction and premature ejaculation, pelvic floor muscle exercise prescription was 2-3 times per week with pelvic floor muscle contractions both maximal quick contractions and submaximal endurance holds. Significant results were shown with participants who were taught pelvic floor muscle contractions through a combination of verbal and physical means (typically biofeedback). Specific verbal cues were not reported. The authors suggest that electrical stimulation was helpful for training recruitment patterns; however, there was not a significant difference in outcomes for those with ED when using electrical stimulation. The authors suggest that pelvic floor muscle training can be part of a conservative treatment. It may be used with oral pharmacology for quick results, and may be beneficial with electrical stimulation and biofeedback, though more research is indicated.
If you are interested in learning more about treating male patients, consider attending Male Pelvic Floor: Function, Dysfunction, and Treatment!
Myers, C., Smith, M. “Pelvic floor muscle training improves erectile dysfunction and premature ejaculation: a systematic review” Physiotherapy 105 (2019) 235–243
As more and more patients seek care for pelvic floor dysfunction, the need for more qualified practitioners is becoming apparent. Many patients prefer to see a clinician who they identify with, which is why it is important for practitioners of all genders to learn to treat pelvic floor dysfunction. Because much of the public's awareness of pelvic rehab comes out of women's health, the vast majority of pelvic health practitioners are women.
There is currently a shortage of male pelvic health practitioners. To help us understand why it is so important to fix that, we reached out to several male clinicians who have attended the Male Pelvic Floor: Function, Dysfunction, and Treatment course to ask them about the need for more men in the field. Here are some answers to the question:
“Why is it important to have male providers available to treat male patients in the field of pelvic health?”
Grant Headley of Bridgetown Physical Therapy of Portland, Oregon (www.bridgetownpt.com)
While as PT’s we all approach our patients with interest in helping them as individuals, some of our patients feel more comfortable sharing certain details with a provider of the same gender. Many of the hang-ups some men have about receiving care from a female provider are related to an older generation, to certain traditional or religious cultural beliefs, or to certain beliefs about propriety related to receiving care.
As acknowledged in our coursework, generally men have cultural barriers that traditionally do not permit sharing of vulnerability or weakness, especially in the sexual domain. Here are a few unsolicited statements I feel encapsulate what my own male patients have told me: Some heterosexual men feel more comfortable sharing the details of their dysfunction with a man because they find it difficult to admit vulnerability in the presence of a female. Some men prefer not to relay the clinically pertinent details of dysfunctional sexual encounters with a female because they do not wish to make the female practitioner uncomfortable. Many men feel that they can relay more detail about the mechanics of the sexual dysfunction or signs of improvement to a male provider. Some men have told me that they felt their sexual dysfunction was minimized or that they have been treated with patronizing language by a female pelvic PT in the past. Unfortunately, these patients attribute this negative experience to the PT being female, and they are not comfortable having a second opinion with a female.
 Although we strive to present as open-minded and neutral to our patients, they may have an affinity for a male provider. This could foster a more constructive clinical partnership towards working on their goals if they perceive fewer communication barriers. I can offer my own experience as a past patient suffering with pelvic floor dysfunction; I was so desperate for help and I felt so grateful that there was a physical therapist in my city at all that was willing to help me. I did not care that she was female and that I had to receive treatment at a women's health clinic for new mothers in the University Hospital. Many female therapists reading this article have likely transferred lifesaving PT care to scores of men. This organization of H&W that does so much good for a sensitive aspect of men's care is dominated by women- this needs to be acknowledged as a net positive but also appreciated that much of the education and application of care is an adaptation from what has worked for women in the past. Many men will be so grateful to receive care and get better. Some men unfortunately will have barriers to receiving care and for those patients, we can seek out and encourage our male colleagues to get involved in pelvic rehab so we can all provide more access to care.
Although we strive to present as open-minded and neutral to our patients, they may have an affinity for a male provider. This could foster a more constructive clinical partnership towards working on their goals if they perceive fewer communication barriers. I can offer my own experience as a past patient suffering with pelvic floor dysfunction; I was so desperate for help and I felt so grateful that there was a physical therapist in my city at all that was willing to help me. I did not care that she was female and that I had to receive treatment at a women's health clinic for new mothers in the University Hospital. Many female therapists reading this article have likely transferred lifesaving PT care to scores of men. This organization of H&W that does so much good for a sensitive aspect of men's care is dominated by women- this needs to be acknowledged as a net positive but also appreciated that much of the education and application of care is an adaptation from what has worked for women in the past. Many men will be so grateful to receive care and get better. Some men unfortunately will have barriers to receiving care and for those patients, we can seek out and encourage our male colleagues to get involved in pelvic rehab so we can all provide more access to care.
Lance Frank of Flex Physical Therapy in Atlanta (www.flexptatl.com)
Personally, as a male provider in pelvic health, I find that the men I treat are much more comfortable and at ease discussing topics like erections (or lack thereof) and sexual dysfunction, as well as incontinence, or pelvic pain. In a female dominated sub-specialty of physical therapy, sometimes as a male it can be intimidating and even embarrassing for some men to discuss these topics at all, let alone with a female; so having the option to speak and be treated by another male who may better understand the changes, anatomy, and problems they’re experiencing may feel a bit less daunting. Our culture has made male masculinity fragile and I think some populations of men who need pelvic floor rehab may feel embarrassed to be treated by a female clinician if their perception of being seen by a female is emasculating. Ultimately, I think there needs to be more men in this field because there needs to be better visibility of male pelvic health providers in general, as well as better representation of men acknowledging that male pelvic floor disorders exist and are willing and able to treat them.
Eddie Gordon of Flow Rehab in Seattle (www.flowrehab.com)
There are far fewer male physiotherapists treating men with pelvic floor dysfunctions, but I am hopeful this will change for the better. Lack of access to male pelvic physios is a relative barrier to care because some men are more comfortable seeing a male pelvic provider the same way most women would prefer seeing a female pelvic physio. In general, men do not typically seek treatment as frequently or early enough the way most women do. If male pelvic physios are not available, then men may more likely delay treatment, which could potentially worsen their problem. Ironically, when it comes to men with pelvic floor dysfunctions, men are underrepresented, but I am hopeful that more male PT’s will be joining the movement to educate the male population.
Milan Patel of Comprehensive Therapy Services in San Diego (comprehensivetherapy.com)
I believe it's important to have male providers in the pelvic health field for many reasons, one being the opportunity for connection. I think we connect best with reflections of ourselves and for men seeking out a pelvic health provider that can be hard to find. In my experience, pelvic physical therapy works best when your patient can be open and honest, and establishing a strong connection between therapist and patient is the first step. Another reason is that people should have options for the provider they want. In San Diego I am the only male pelvic physical therapy provider which means most men seeking pelvic floor therapy have no choice but to see a female. If you switched the genders in the last sentence you could see how that is problematic. Many women prefer to have their pelvic PT be a female, I just think guys should get the same choice.
Steven Lavender of The Physical Therapy Practice NYC in New York (thephysicaltherapypractice.nyc)
In my experience as a gay male practitioner practicing pelvic floor physio on only men:
Gay male patients usually prefer a gay provider because they feel like they don’t have to explain lifestyle issues and choices, they may be unused to being touched by women, and maybe misogynistic.
Some straight men have told me that they think a male practitioner would know more about their pelvic issues than a woman. Some men don’t think women are strong enough nor have long enough fingers to get to the places they need to be. Some straight men report they might be attracted to a female therapist and get an erection or feel embarrassed about appearing unmanly with their particular pelvic condition.
For some men being touched by a woman is a religious issue so many males of the Jewish and Muslim faiths prefer to see a male practitioner.
Some men could not care less who sees them as long as they get better.
One woman called me for advice or for an appointment from some distance because they "figured a gay man in New York City just might know more about my ass and ass pain than any local jack-assed doctor in my neck of the woods." True story.
If you are interested in learning to treat male patients, the Male Pelvic Floor: Function, Dysfunction, and Treatment course is a great place to start! The course is taking place twice more in 2019, this September 13-15, 2019 in Pasadena, CA, and again in Fort Myers, FL on October 19-21, 2019. We are already booked four times in 2020 as well, so be sure to check out the full course schedule for all available dates.
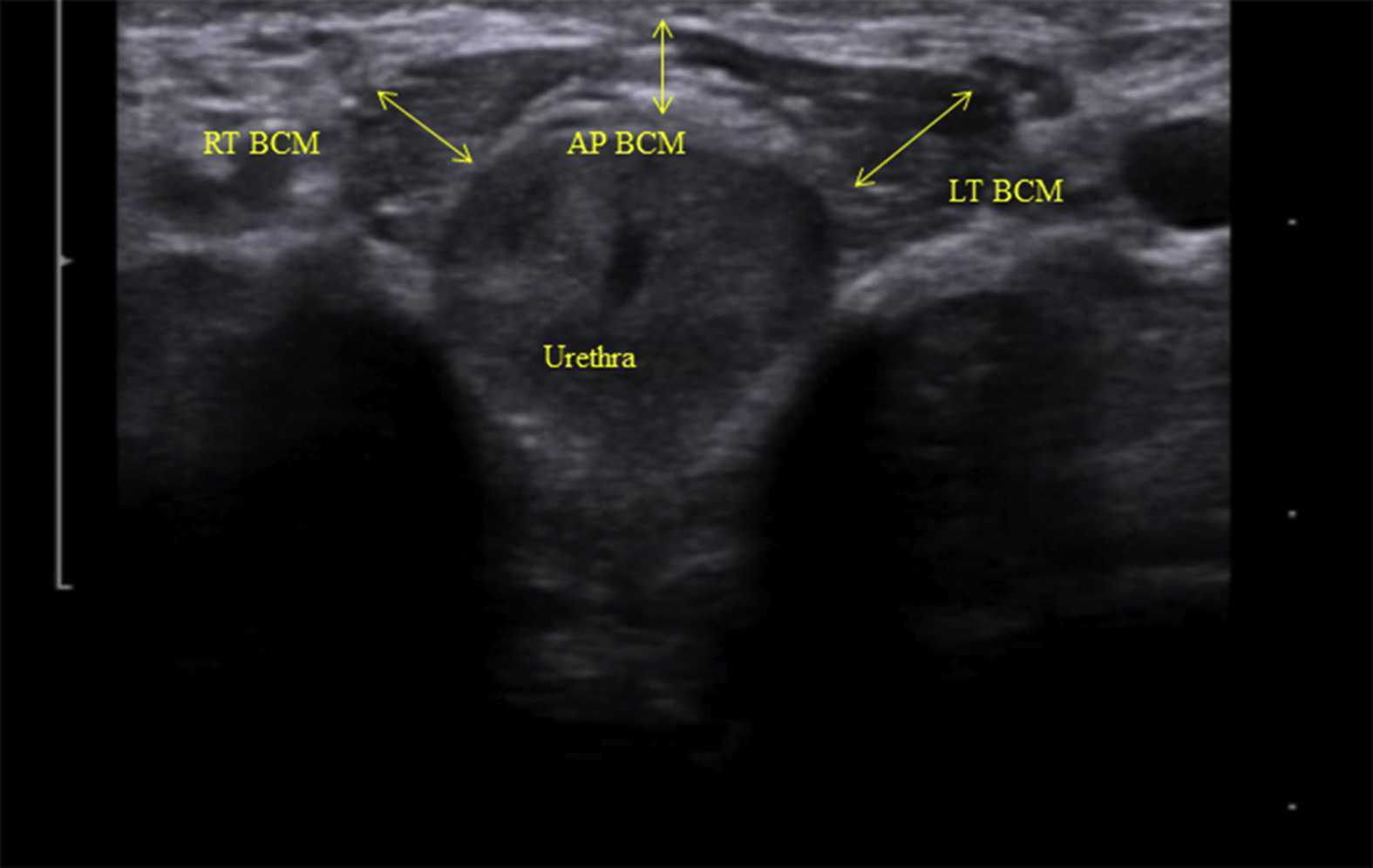
Rehabilitative ultrasound imaging has been used in clinical practice for well over a decade now. It has been used for core stabilization, as well as with female incontinence patients. In recent years, transperineal ultrasound imaging has emerged as a useful tool for assessing prolapses and identifying other women’s health issues in the anterior compartment.
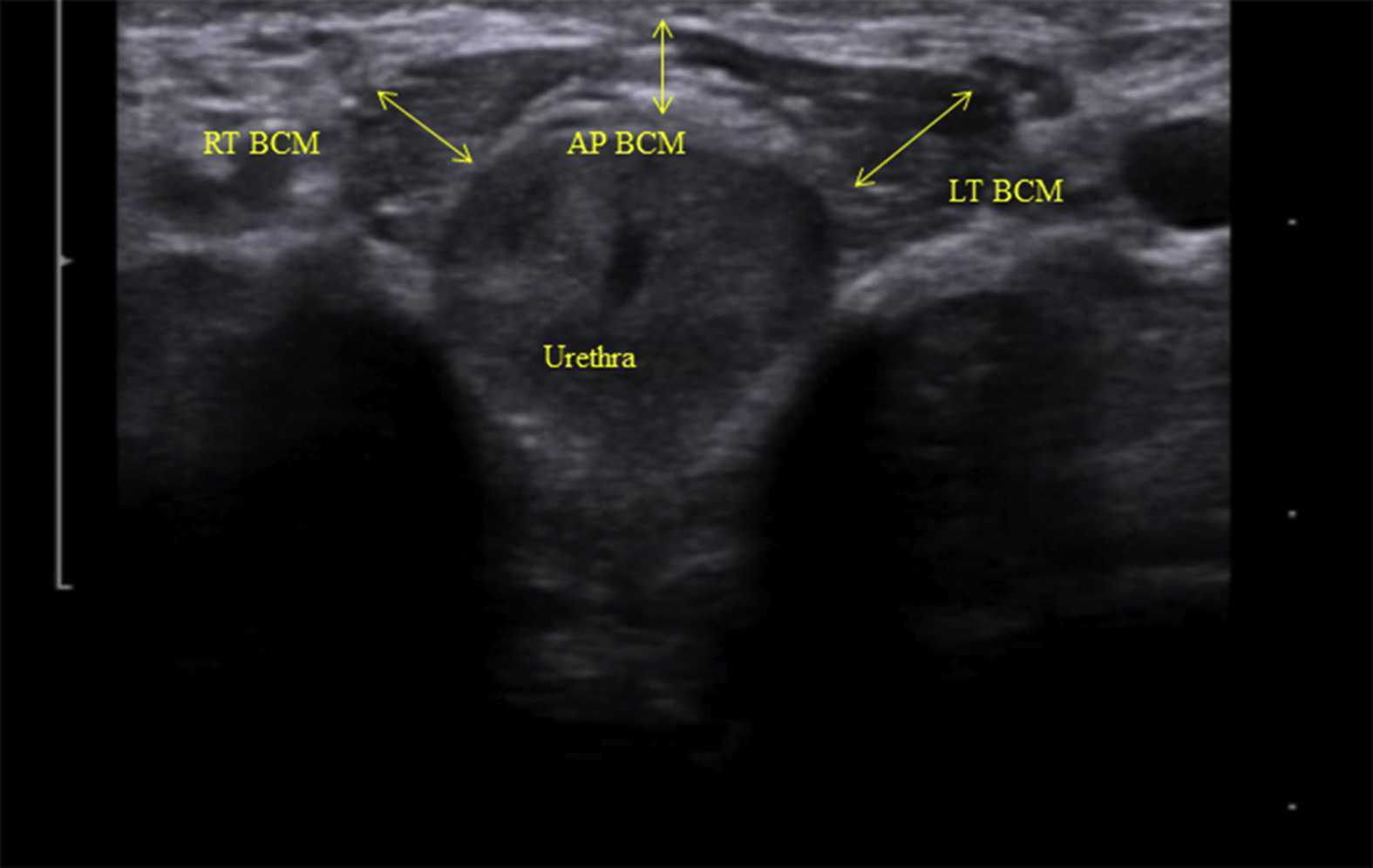 Like other things in men’s pelvic health, the use of ultrasound imaging for rehabilitation has lagged behind that in women’s pelvic health. Ryan Stafford is a researcher that is working to change that. In 2012, Stafford began looking at the normal responses to pelvic floor contractions and what is seen on ultrasound in men. He has since taken his research further to examine differences in men that present with post-prostatectomy incontinence. Stafford, van den Hoorn, Coughlin, and Hodges performed a study looking at the dynamic features of activation of specific pelvic floor muscles, and anatomical parameters of the urethra. The study included forty-two men who had undergone prostatectomy. Some of these men were incontinent and others remained continent. Transperineal ultrasound imaging was used to obtain images of the pelvic structures during a cough, and a sustained maximal contraction. The research team calculated displacements of pelvic floor landmarks with contraction, as well as anatomical features including urethral length, and resting position of the ano-rectal and urethra-vesical junctions.
Like other things in men’s pelvic health, the use of ultrasound imaging for rehabilitation has lagged behind that in women’s pelvic health. Ryan Stafford is a researcher that is working to change that. In 2012, Stafford began looking at the normal responses to pelvic floor contractions and what is seen on ultrasound in men. He has since taken his research further to examine differences in men that present with post-prostatectomy incontinence. Stafford, van den Hoorn, Coughlin, and Hodges performed a study looking at the dynamic features of activation of specific pelvic floor muscles, and anatomical parameters of the urethra. The study included forty-two men who had undergone prostatectomy. Some of these men were incontinent and others remained continent. Transperineal ultrasound imaging was used to obtain images of the pelvic structures during a cough, and a sustained maximal contraction. The research team calculated displacements of pelvic floor landmarks with contraction, as well as anatomical features including urethral length, and resting position of the ano-rectal and urethra-vesical junctions.
The data was analyzed and combinations of variables that best distinguished men with and without incontinence were reported. Several important components were identified in the study. Striated urethral sphincter activation, as well as bulbocavernosus and puborectalis muscle activation were significantly different between men with and without incontinence. When these two parameters were examined together, they were able to correctly identify 88.1% of incontinent men. They further reported that poor function of the puborectalis and bulbocavernosus could be compensated for if the man had good striated urethral sphincter function. However, the puborectalis and bulbocavernosus had less potential to compensate for poor striated urethral sphincter function. This is important for a therapist that works with post prostatectomy patients to know. This can explain part of why some men improve and do so well after a prostatectomy and others don’t, even with therapy to help. If the striated urethra sphincter is damaged and its normal responses are changed during surgery, then incontinence after prostatectomy may be more likely.
Using ultrasound imaging, the therapist can examine and see exactly where a man is deficient in response; whether it is the puborectalis, or the striated urethra sphincter. It is exciting to see this new research and see how rehabilitative ultrasound imaging can influence men’s pelvic health! Come and learn how to use ultrasound imaging for your men’s pelvic health patients as well as your women’s health and back pain patients! You will see how ultrasound imaging can change your practice and how much your patients will enjoy seeing real-time images of their contractions! Thanks to our partnership with The Prometheus Group, this course includes hands-on training on the latest in pelvic ultrasound imaging.
1. Stafford R, Ashton-Miller J, Constantinou C, et al. Novel insights into the dynamics of male pelvic floor contractions through transperineal ultrasound imaging. J. Urol. 2012; 188: 1224-30.
2. Stafford RE, van den Hoorn W, Couglin G, Hodges P. Postprostatectomy incontinence is related to pelvic floor displacements observed with trans-perineal ultrasound imaging. Neurol and Urodyn. 2018; 37:658-665.
Image credit Gupta et al. 2016 https://doi.org/10.1016/j.ajur.2016.11.002 https://www.sciencedirect.com/science/article/pii/S2214388216300881#fig2