With PF1 Durham just around the corner, and PF1 Seattle in January sold-out with a 20-person wait list, our next PF1 is filling up quickly.
PF1 in Maywood, IL from March 1-3 is over half-full, and additional registrations are rolling in each day. If you are interested in joining us for PF1 in Maywood, do not hesitate to register. We expect this course to fill up before the holidays are upon us, so act quickly.
Once PF1 in Maywood is full, the next available PF1 is in Houston, TX in early May 2013. If you'd like to take this popular course before May of 2013, we suggest registering for the Maywood course today!
Stay tuned this week for a big announcement that we have coming up. We are adding a new highly requested feature to our website, which we are confident women's health physical therapists will find very helpful!
A big thanks to everyone who completed our PTPC Job Task Analysis Survey over the past few weeks. We received over 400 responses, which is more than enough data that we will need to perform the necessary analysis.
On May 2nd, we drew the names of our two lucky participants, who will each received a free course registration of their choosing. Congratulations to Christy Kline, PT and Kate Middleton, PT on winning the drawing!
Over the next few weeks, our subject matter experts and test development partner, Kryterion, will work together to finalize the quantitative blue print. This blue print will determine the relative amount of exam items that will be devoted to various sub-topics within pelvic rehabilitation. While not a "study guide", those interested inpursuing PTPC could use this test blue print to determine the topicson which to focus their studying efforts.
Our test developers will also use this test blue print to begin writing exam items. Similar to the JTA survey, we will need to beta test exam items in order to measure their validity for the actual exam.
Thanks again to everyone who participated, and please stay tuned for updates as we continue to work towards offering the PTPC exam for the first time. Also, if you completed the JTA survey, and have yet to redeem your $50 credit, let us know when you are ready to apply your credit to an upcoming course that you'd like to attend.
In a study from the Center for Aging at the University of Alabama, Birmingham and the Birmingham/Atlanta Veterans Affairs Geriatric Research, Education, and Clinical Center, researchers determine that physical therapy, bladder control strategies, and biofeedback significantly reduced the incidence of urinary incontinence in post-radical prostatectomy males when compared to a control group.
Check out the abstract of the study here.
The Institute is sponsoring a radio show hosted by Dr. Melanie Barton and featuing Amy Stein, MPT, BCB-PMD. Amy will talk about Interstitial Cystitis and Pelvic Pain and the role of physical therapy in treating these problems
Tune in on April 28th or visit Dr. Melanie's site to download the podcast.
Earlier this month, Datamonitor released a report on Urinary Incontinence in the 7 major global markets (The US, Japan, France, Germany, Italy, Spain, and the UK). Check out the highlights here. The whole report is pretty expensive, but they touch on a point that we have long emphasized: the prevalence of urinary incontinence will grow over the next ten years, with the most cases occurring in the United States.
Demand for innovative and effective treatments for urinary incontinence will continue to increase for years to come. Therapists with extensive clinical experience treating urinary incontinence will be well positioned for this demographic trend.
On April 18th, a group of German and Italian researchers published this article on the impact of episiotomy on pelvic floor dysfunction. The paper found that "Episiotomy appears to be a protective factor for women's wellness. Women who had episiotomy and who experienced perineal symptoms have a better psycho-physical health status in the 12.79 months follow-up."
Available for download is a 15 page PDF of "Impact of episiotomy on pelvic floor disorders and their influence on women's wellness after the sixth month postpartum: a retrospective study". The PDF contains research highlights (including Abstract, Background, Methods, Results and Conclusion)
Much has been made of the research indicating that a Caesarean section has a protective effect on the pelvic floor, with some women requesting a CS in order to avoid pelvic floor dysfunction (PFD). This practices raises concern about an elective approach to CS versus natural vaginal birth, as CS are by no means without risk to the mother, the fetus, and to the neuromusculoskeletal system. Recent research contributes to this discussion by assessing several variables including quality of life factors and pelvic dysfunction following either a CS or natural vaginal birth. Twenty one women who had given birth in the prior 36 months were recruited from daycare facilities. Subjects were categorized into normal vaginal delivery (NVD) or Caesarean section (CS). Subjects were only included if they gave birth to singletons, had not previously participated in pelvic rehabilitation, or if they did not had a history of pelvic surgery, neurologic issues or trauma that affected bowel and bladder function. Outcomes tools included the SF-36, and the Pelvic Floor Distress Inventory (PFDI). Within the PFDI, outcomes tools assessed urinary, colorectal, prolapse, and pelvic floor functional impact.

Nearly 70% of the women in the group studied were between the ages of 30 and 39, with ages ranging from 21-45. The number of subjects who had given birth vaginally was 16, by Caesarean section, 5. The authors report that approximately 75% of their subjects were Caucasian, had a household income of 70,000 or more, and nearly 80% had at least a four-year degree. The women in the CS group reported higher rates of urinary incontinence and pelvic pain (90% and 67%, respectively) when compared to the NVD group (50% and 23%). Women who gave birth via CS also had higher mean scores on the Urinary Distress Inventory, Colorectal-Anal Distress Inventory, and the Pelvic Organ Prolapse Distress Inventory. The authors also noted a correlation between pelvic organ prolapse and body mass index (BMI) greater than 25.
This research contributes to the literature about birth mode and pelvic dysfunction, and the study conflicts with other data that describes a protective effect of Caesarean birth mode on the pelvic floor. While avoiding vaginal delivery may indeed help reduce some injury to the pelvic floor, this study, even though the sample size was not large, reminds us that CS delivery can be associated with pelvic dysfunction and symptoms. This study was different from many prior reports in that the subjects were surveyed in the chronic rather than immediate postpartum period. If you are interested in learning more about postpartum rehabilitation, check out the Institute's offerings on this page: http://hermanwallace.com/postpartum.

With words like jumping, diving, spiking, hitting, and blocking making up the game's activities, volleyball is clearly a sport that requires a healthy pelvic floor. We know that athletes are at risk for pelvic dysfunction, with symptoms ranging from tension to leakage, but what happens when the pelvic floor is reeducated? In a study addressing volleyball players, researchers assess the effectiveness of a pelvic muscle rehabilitation program on symptoms of urinary incontinence. 32 female athletes were divided evenly between a control group and an experimental group. Inclusions criteria for the sample was nulliparity, symptoms of stress urinary incontinence, age between 13 and 30, and leakage amount more than 1 gram on the pad weight test. Exclusion criteria is as follows: treatment time of less than six months, sport practice for less than two years, urinary tract infections (either current or repeated prior infections), intervention adherence less than 50%, or body mass index outside of the range of 18-25.
Before and after intervention, the athletes were given a baseline questionnaire, a pad test (in the first 15 minutes of volleyball practice), and they completed seven days of a bladder diary to track leakage. The treatment group were instructed in anatomy and physiology of the lower urinary tract, about urinary incontinence (UI) and UI in athletes, and in leakage prevention strategies. A 3-day bladder diary was completed to improve awareness of fluid intake and bladder habits. Pelvic muscle awareness and correct contractions, doing protective pre-contractions of the pelvic floor, and a home exercise program of quick and endurance pelvic muscle contractions in different positions were also instructed.
The results of the intervention include a significant decrease in urinary leakage in the treatment group. The education provided also allowed for prevention of negative coping strategies that were reported in the subjects: the athletes would conceal leakage by wearing a menstrual pad, decreased their fluid intake, or empty their bladder more frequently. This study contributes to the growing body of evidence linking sport to pelvic dysfunction, and more importantly, rehabilitation efforts to improvement. If you want to learn more about pelvic dysfunction in athletes, come to The Athlete and the Pelvic Floor with Michelle Lyons. This 2-day continuing education course took place recently in New York City and your next opportunity to take the class is in Denver in October!
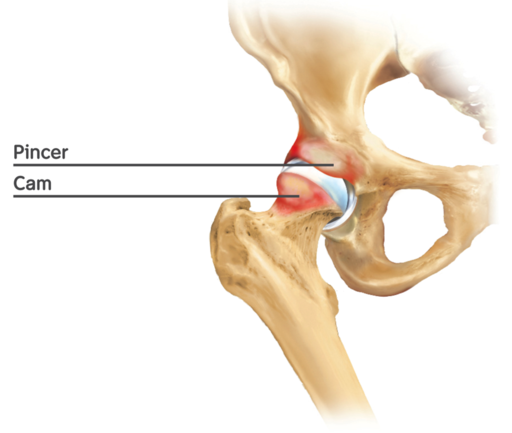
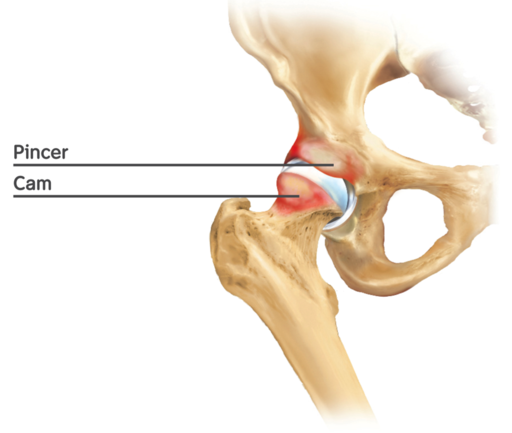
In the treatment of pelvic dysfunction, collaboration among physicians and pelvic rehabilitation providers creates an optimal care situation for the patient. In a research article that will be published in the July issue of Journal of Lower Genital Tract Disease, physical therapist and Herman & Wallace Institute faculty member Stacey Futterman demonstrates how a partnership between disciplines provides information valuable to the field of pelvic rehabilitation. Stacey and physicians Deborah Coady, Dena Harris, and Straun Coleman hypothesized that persistent vulvar pain may be generated by femoroactebular impingement (FIA) and the resultant effects on pelvic floor muscles. Through the research, the authors attempted to determine if hip arthroscopy was a beneficial intervention for vulvar pain, and if so, which patient characteristics influenced improvements.
Twenty six patients diagnosed with generalized, unprovoked vulvodynia or clitorodynia underwent arthroscopy for femoroacetabular impingement. For 3-6 months following hip repair, patients were treated with physical therapy that included surgical postoperative rehabilitation combined with rehabilitation for vulvodynia. Time period for follow-up data collection ranged from 36-58 months. Six patients reported improvements in vulvar pain following surgery and did not require further treatment, and it is noted that these patients were all in the youngest age bracket (22-29). Among the patients who did not report sustained relief, relatively older ages (33-74) were noted, along with a tendency to have vulvar pain for 5 years or longer.
The relationship between hip and pelvic pain may come from the bony structures, hip muscles including but not limited to the obturator internus, and nerves such as the pudendal. The authors conclude that "All women with vulvodynia need to be routinely assessed for pelvic floor and hip disorders…" and if needed, treatment should be implemented to address the appropriate tissue dysfunctions. If you are interested in learning more about hip dysfunction so you can better screen for dysfunction such as femoroacetabular impingement, check out faculty member Steve Dischiavi's continuing education course. Biomechanical Assessment of the Hip & Pelvis: Manual Movement Therapy and the Myofascial Sling System takes place next in Durham, North Carolina in May.
Patients diagnosed with colorectal cancer may undergo a procedure called mesorectal excision as part of their oncology management. In this procedure, a significant portion of the bowel is removed along with the tumor. Total mesorectal excision refers to the entire rectum and mesorectum (peritoneum that connects the upper rectum.) The rectum is removed up to the level of the levator muscles, and this procedure is indicated for tumors of the middle and lower rectum. In a study published in the World Journal of Oncology, the authors report on female urogenital dysfunction following total mesorectal excision (TME).
Questionnaires were returned by 18 women (age range 34-86) who had undergone TME for rectal cancer. Results of the study are summarized in the chart below. (All patients had reported vaginal childbirth, and five had undergone total abdominal hysterectomy and oophrectomy.)
| Presurgical
|
Postsurgical
|
Sexual function
| 5/18 (28%) were sexually active (with no complaints of dyspareunia) | Sexually active patients remained active but all reported discomfort with penetration 2 patients reported decreased libido due to stoma |
Urinary function
| 3/18 (17%) reported urinary urgency and frequency | Of patients with urinary symptoms, 80% persisted longer than 3 months post-surgery |
| 7/18 (39%) reported stress urinary incontinence | |
| New onset symptoms: 61% developed nocturia, 20% developed stress urinary incontinence, 1 patient required permanent catheter |
The authors conclude that rectal cancer treatment can worsen urinary symptoms of nocturia and stress incontinence. Patients who had also been treated with a hysterectomy were found to have more significant symptoms. A proposed mechanism of this increase in symptoms in women who had undergone a hysterectomy is the prior nerve dissection which, when added to the nerve dissection of the inferior hypogastric plexus and the hyogastric nerves for the total mesorectal excision, may have an additive effect. This study which is available full-text, free access, describes further the relationship between the autonomic nervous system in the female pelvis, pelvic function, and the surgery for rectal cancer. Data such as the information provided in this study allow medical providers and their patients to make well-informed decisions about surgeries and quality of life risk factors that may guide medical management of colorectal cancer.
If you would like to feel better prepared to manage post-surgical issues that arise following treatments for colorectal cancer in women, check out the Institute’s Oncology and the Female Pelvic Floor course taught by faculty member Michelle Lyons. This continuing education course happens next in May in Torrance, California.