In a case report published within the past year by physical therapist Karen Litos, a detailed and thorough case study describes the therapeutic progression and outcomes for a woman with significant functional limitation due to a separation of her diastasis recti muscles. The patient in the case is described as a 32-year-old G2P2 African-American woman referred to PT at 7 weeks postpartum. Delivery occurred vaginally with epidural, no perineal tearing, and pushing time of less than an hour. Primary concerns of the patient included burning or sharp abdominal pain when lifting, standing, and walking. Uterine contractions that naturally occurred during breastfeeding also worsened the abdominal pain and caused the patient to discontinue breastfeeding. The patient furthermore reported sensations that her insides felt like they would fall out, and abdominal muscle weakness and fatigue with activity.
Although many other significant details related to history, examination and evaluation were included in the case report, I will focus on the signs, interventions, and outcomes recorded in the paper. Diastasis was measured using finger width assessment and a tape measure. (Although ultrasound is more accurate and valid, palpation of diastasis has been demonstrated to have good intra-rater reliability as used in this study. Measures for interrecti distance (IRD) at time of evaluation were 11.5 cm at the umbilicus, 8 cm above the umbilicus, and 5 cm below the umbilicus. The patient also reported pain on the visual analog scale (VAS) of 3-8/10.
Interventions in rehabilitation included, but were not limited to: instruction in wearing an abdominal binder, appropriate abdominal and trunk strengthening (promotion of efficient load transfer and avoidance of exercises that may worsen separation), biomechanics training with functional tasks such as transfers, self-bracing of abdominals, avoiding Valsalva, postural alignment and symmetrical weight-bearing strategies. Plan of care was developed as 2-3x/week for 2-3 weeks, the patient was seen for 18 visits over a four month period. Therapeutic exercise was progressed to include general hip and trunk muscle strengthening towards a goal of stability during movement. Cardiovascular training progressed to light treadmill jogging and use of an elliptical.
After 18 visits, functional goals were all met and included picking up her baby, holding her baby for 30 minutes, standing or walking for at least an hour. VAS pain score progressed to 0 on the 0-10 scale. The diastasis was measured at discharge to be 2 cm at the umbilicus, 1 cm above the umbilicus, and 0 cm below the umbilicus. This case report is first an excellent example of a detailed case example. Second, while the separation dramatically improved, most importantly, the patient’s function improved and her goals were met. This case is a wonderful example of how sharing details of a patient’s rehabilitation efforts can be useful for other rehabilitation therapists to consider when developing a plan of care.
If you are interested in discussing more about postpartum care, check out the first in our peripartum series, “Care of the Pregnant Patient” taking place next in Boston in May with Institute co-founder Holly Herman.

Sexual dysfunction is a common negative consequence of Multiple Sclerosis, and may be influenced by neurologic and physical changes, or by psychological changes associated with the disease progression. Because pelvic floor muscle health can contribute to sexual health, the relationship between the two has been the subject of research studies for patients with and without neurologic disease. Researchers in Brazil assessed the effects of treating sexual dysfunction with pelvic floor muscle training with or without electrical stimulation in women diagnosed with multiple sclerosis (MS.) Thirty women were allocated randomly into 3 treatment groups. All participants were evaluated before and after treatment for pelvic floor muscle (PFM) function, PFM tone, score on the PERFECT scheme, flexibility of the vaginal opening, ability to relax the PFM’s, and with the Female Sexual Function Index (FSFI). Rehabilitation interventions included pelvic floor muscle training (PFMT) using surface electromyographic (EMG) biofeedback, neuromuscular electrostimulation (NMES), sham NMES, or transcutaneous tibial nerve stimulation (TTNS). The treatments offered to each group are shown below.
| Intervention
|
sEMG biofeedback PFMT: Use of intravaginal sensor and 30 slow, maximal-effort contractions followed by 3 minutes of fast, maximal-effort contractions in supine.
|
Sham NMES: sacral surface electrodes with pulse width of 50 ms at 2 Hz, on/off 2/60 seconds for 30 minutes
|
Intravaginal NMES: 200 ms at 10 Hz for 30 minutes using vaginal sensor.
|
TTNS: surface electrodes in the left lower leg with pulse width at 200 ms at 10 Hz for 30 minutes.
|
| Group 1, n = 6 | X | X | ||
| Group 2, n = 7 | X | X | ||
| Group 3, n = 7 | X | X |
The following factors made up some of the inclusion criteria for the study: age at least 18 years, diagnosis of relapsing-remitting MS, 4 month history of stable symptoms, currently participating in a sexually active relationship, and able to contract the pelvic floor muscles. Participants were excluded if they had delivered within the prior 6 months, had pelvic organ prolapse (POP) greater than stage I on the POP-Q, were perimenopausal or menopausal. Neurologic function symptoms were also monitored so that subjects could be evaluated for any potential flare-up. Home program instruction in PFMT included 30 slow and 30 fast PFM contractions to be completed in varied postures 3x/day.
Results included that all groups improved via the PERFECT scheme evaluation. Other specific indicators of improvement were noted for each group, and the use of the FSFI provided measures of sexual function. The authors conclude that pelvic floor muscle training (with or without electrostimulation) can produce positive changes in sexual arousal, vaginal lubrication, sexual satisfaction and sexual lives. The use of PFMT with intravaginal NMES "…appears to be a better treatment option than PFMT alone or in combination with PTNS in the management of the orgasm, desire and pain domains of [the FSFI]." You can find the abstract of the article by clicking here.
Patients who are managing disease symptoms of MS have many aspects of the disease that can interfere with sexual health, such as energy levels, neurologic impairment, and pain. Use of modalities such as biofeedback and/or electrotherapy may be useful adjuncts in the care of women who have MS. Prior research has identified the benefits of electrotherapy for urinary dysfunction in patients who have MS. The described research allows us to consider inclusion of these tools along with pelvic floor muscle training when working with women who experience sexual dysfunction as a part of MS.

In order to refer patients to needed care, it is vital that health care providers understand the roles that each provider plays. Within pelvic rehabilitation, this issue presents barriers and opportunities, as many providers do not know about pelvic rehabilitation, and about the wide scope of care that we can provide towards bowel, bladder, sexual dysfunction, and pelvic pain in men, women, and children. An article written by a physiotherapist and published in the British Journal of Midwifery highlights the issues such barriers can cause. Utilizing a focus group of seven 3rd year midwifery students, a researchers asked questions about student midwives' perceptions of the physiotherapist's role in obstetrics. Five distinct themes were proposed as a result of the focus group interviews:
1. Role recognition: in order to enable services for patients, understanding other professional roles is valuable.
2. Lack of knowledge: participants expressed a lack of knowledge about the physiotherapy role, and the students wondered if they should be seeking out that knowledge, or if the physiotherapists should be educating the midwives about their role. Prior inter professional education opportunities, which provides the students with potential for understanding other professions, were not viewed as positive by the students.
3. Perceived views existed: Although participants did not have a clear view of what a physiotherapist's role is in obstetrics, they had developed ideas (accurate or not) about the role.
4. Utilization of physiotherapy: Numerous barriers to utilization of physiotherapy in obstetrics rehabilitation were identified, and variations in referrals and utilization of PT were noted.
5. Benefits of physiotherapy: Participants' lack of knowledge, lack of feedback from patients, and issues such as waiting periods prior to getting care limited the stated benefits of physiotherapy care in obstetrics.
In order to avoid working independently of each other, physical therapists and midwives, along with other care providers for women, must understand the complementary roles we play. One of the best ways that we can create a shared understanding is through spending time in each other's educational or clinical environments. Each of us can take responsibility for providing some level of education towards teaching other providers what we do, what we know, and how we can collaborate. One of the ways that the Institute attempts to make this task easier is to provide you with presentations that are already created for this purpose. Our "What is Pelvic Rehab?" powerpoint presentation allows you to edit the slides created for referring providers. Within the presentation, basic information about pelvic therapy and specific research about pelvic rehabilitation for various conditions is combined. To check out the "What is Pelvic Rehab?" presentation and other patient and provider education materials, head to the Products and Resources page and see what information may help you (and your patients) share information about the role of the pelvic rehabilitation provider in collaboration with other health professionals.
Researchers using a community-based sample in the upper Midwest cities of Minneapolis/St. Paul surveyed 138 women between the ages of 18-49 with diagnosed vulvodynia. Vulvodynia was classified as primary (pain started with first tampon use or sexual penetration) or secondary pain started following a period of intercourse that was not painful. The authors aimed to determine the rates of remission of vulvar pain versus pain-free time periods. Remission was defined in this study as having at least one period of time that was pain-free for at least 3 months. Generalized vulvodynia categorization was made after clinical exam and was determined by the subject having pain at each point on the perineal “clock” with cotton swab provocation.
The authors reported that women diagnosed with primary vulvodynia were 43% less likely to report vulvar pain remission that women with a diagnosis of secondary vulvodynia. They also found that obesity and having generalized versus localized vestibulodynia was associated with reduced rates of remission. The theory was discussed that women who have different types of vulvodynia may have varied underlying mechanisms of pain that lead to differences in symptoms. Specifically, the paper reports on recent brain imaging work that suggests women who have primary vulvodynia demonstrate more characteristics of central pain processing.
In relation to health behaviors (such as seeking pain therapy), the authors state that the data may not be sufficiently powered to determine the influence of therapy on remission. They do agree that “…understanding of both spontaneous remission and improvement owing to therapy will ultimately provide guidance in developing more effective interventions.” Because a significant portion of women do not seek care for vulvar pain (for unknown reasons), a bias is created in the research through the lack of representation of those women who are not being studied through healthcare access.
The research concludes with a few familiar themes including the need for more research studying the clinical courses of primary versus secondary vulvodynia. We are also left with questions about which women seek care and why, how their clinical outcomes and remission history may differ based on intervention and other intrinsic variables such as body mass index, and how central pain processing affects pain duration and remission. If you are interested in learning more about vulvodynia, come to one of our newer courses offered by faculty member Dee Hartmann, Assessing and Treating Women with Vulvodynia. Two entire days are spent discussing vulvodynia theory and clinical skills for helping women optimize their health and function. You still have a few weeks to sign up for this course that takes place next in April in Minneapolis!

A report in The Canadian Journal of Human Sexuality describes the level of emphasis placed on particular sexual health topics in Canadian medical schools. Both the level of emphasis and the utilized teaching methods among 51 residency programs for obstetrics and gynecology (OBG), family medicine (FM), and undergraduate medicine (UGM) were evaluated. Program Directors and Associate Deans of the respective programs were electronically surveyed about the following topics: contraception, disease prevention, sexual violence/assault, childhood sexual abuse, sexual dysfunction, childhood and adolescent sexuality, role of sexuality in relationships, aging and sexuality, sexual orientation, gender identity, disability, and social and cultural differences.
The topic that received the most emphasis among the 3 program types was “information and skills for contraception.” Disease prevention for sexually-transmitted diseases was also a high-ranking topic.
The authors point out that while it seems understandable that OBG residencies may not include a significant amount of training in male sexual health, there was an absence of evidence on training in child sexual abuse and adolescent female sexuality in the OBG programs. The article notes other omissions of emphasis such as the lack of training among family practice residencies in transgender and gender identity issues, disability and sexuality, and cultural differences.
This article gives some insight into potential topics of training in human sexual health, and the lack of education in physicians regarding topics of sexual function and dysfunction. In addition to lacking knowledge of some topics in childhood, adolescent, and men’s and women’s health, we can be certain that most providers are not instructed in the role of pelvic rehabilitation providers for sexual dysfunction. How can we contribute to a provider’s knowledge of rehabilitation of sexual dysfunction?
Core lectures, including grand rounds and clinical training made up the primary modes of education for sexual health topics. What if each of us reached out to local training programs, or to local teaching hospitals, or even clinical groups and provided an educational platform about our role in sexual health?
In order to provide such training, you might feel as though you need additional resources and knowledge about sexual health and healing. If you would like to explore how we can maximize our contributions to men and women with sexual dysfunction, and explore your own thoughts and beliefs about sexual health, check out Herman and Wallace Pelvic Rehabilitation Institute co-founder Holly Herman’s course on Sexual Medicine for Men and Women taking place next in April in New Jersey.

Research in the field of sexual dysfunction has taught us several things about patients and healthcare visits. Most medical providers don’t ask about sexual function, most patients don’t bring it up, and women’s sexual health has a history of being undervalued and under-evaluated. Authors Maciel and Lagana describe the common myth that as women age, sexual interest decreases, and review literature to propose improved strategies. The study highlights the fact that there are positive physical health effects for older adults, and that by approaching sexual desire through a biopsychosocial method, further understanding of the issues can be gained.
Several factors have been found to be linked to healthy sex in older females. Having a positive attitude towards sex, an interesting an interested partner, good health, and a willingness to experiment sexually can all contribute to an active sex life. Women who are dealing with high stress, anxiety, and depression are known to be less sexually active. In this paper, the authors describe the work of Sobecki and colleagues, who found that older women have just as much interest in talking about sexual health as younger women, but that doctors aren’t usually asking about it. Sobecki et al. found that a patient reported feeling less embarrassed about bringing up sexual dysfunction if the medical provider demonstrated a professional demeanor, comfort with the topic, and a disposition that is kind and empathetic.
This last point seems worthy of pause and reflection in relation to the role of the pelvic rehabilitation provider. I would submit that most pelvic rehab therapists are highly capable of presenting a professional, kind, and empathetic demeanor. I wonder how many of us, however, had enough education regarding sexual health to demonstrate to patients a level of “comfort with the topic” that inspires a patient to bring up sexual concerns. The more comfortable we are with our own sexuality and the more knowledgeable we are about sexual health practices that are outside of our own experiences, the more we have to offer to our patients.
This excellent review article describes issues that older women often face: menopausal shifts in hormones and vaginal and perineal health, concerns about body image and self-worth. The authors also point out that the healthcare system has medicalized menopause, so that most women are offered little more than pharmaceuticals. One simple suggestion offered in the article is use of the Decreased Sexual Desire Screener that can help identify areas of concern in sexual health. If you are interested in learning more about sexual health and dysfunction, check out Institute founder Holly Herman’s Sexual Medicine for Men and Women continuing education course taking place next in April in New Jersey. If that date does not work for you, you could sign up early for the next course in San Diego in November!

The merriam-webster online dictionary defines reflex as "an action or movement of the body that happens automatically as a reaction to something" or as "something that you do without thinking as a reaction to something." This reflexive action ideally describes what the pelvic floor does when we perform an activity that increases intra-abdominal pressure- and that can help us tighten the pelvic floor protectively so that urine is not expelled from the bladder and out the urethra. A research article by Dietz, Bond, & Shek asked if childbirth interrupted the body's natural reflex of contracting the pelvic floor muscles during a cough.
84 women completed the study, which utilized ultrasound measurements to assess reflex contraction of the pelvic floor during a cough. The women were pregnant with their first child (a singleton) and were between 33-37 weeks gestation. Prior to childbirth, 98% of the subjects demonstrated a reflex contraction of the pelvic floor muscles. At a postpartum visit at least 3 months postpartum, the number of women completing a reflex contraction was reduced to 75%. In addition to fewer women demonstrating a shortening contraction during a cough in the postpartum women, the intensity of the contraction was also reduced.
To collect the data, the researchers prospectively completed 4D (4-dimensional) ultrasound (US) volume measurement of the pelvic floor during a cough. They used levator hiatus diameter changes to quantify reflex action of the pelvic floor muscles. From prenatal to postnatal visit, the magnitude of the reflex contraction decreased from 4.8 mm to 2.0 mm (the number represents the mean difference in midsaggital diameter between rest and maximal contraction.) In the antenatal visit, 26 of the 84 women complained of stress urinary incontinence, at the postpartum visit, 20 reported stress incontinence. An association was noted between a lower magnitude of reflex contraction and stress urinary incontinence.
The authors conclude that pelvic floor reflexes are altered by childbirth. The study offers theories as to why the reflexive contraction is interrupted, such as nerve injury or muscle damage, but did not make concrete conclusions about the causes of reflex interruption. Regardless of the mechanism that interrupts a reflexive contraction, this study highlights the value and importance of teaching women to retrain this importance reflexive contraction, and not only for a cough, but for any activity that may create a significant change in intra-abdominal pressure. If you are interested in learning more about postpartum rehabilitation, check out the Care of the Postpartum Patient, which will be offered next in Boston in May!

A US study published in the International Society for Sexual Medicine last year reports on the available evidence linking cycling to female sexual dysfunction. In the article, some of the study results are summarized in the left column of the chart below. On the right side of the column, we can consider ideas about how to potentially address these issues.
| Examples of Research Cited
|
Ideas for Addressing Potential for Harm |
| dropped handlebar position increases pressure on the perineum and can decrease genital sensation | encourage cyclists to take breaks from dropped position, either by standing up or by moving out of drops temporarily |
| chronic trauma can cause clitoral injury | encourage cyclists to wear appropriately padded clothing, to apply cooling to decrease inflammation, and to use quality shocks or move out of the saddle when going over rough roads/terrain when able |
| saddle loading differs between men and women | women should consider specific fit for bike saddles |
| women have greater anterior pelvic tilt motion | is pelvic motion on bike demonstrating adequate stability of pelvis or is there a lot of extra motion and rocking occurring? |
| lymphatics can be harmed from frequent infections and from groin compression | patients should be instructed in positions of relief from compression and in self-lymphatic drainage |
| pressure in the perineal area is affected by saddle design, shape | female cyclists with concerns about perineal health should work with a therapist or bike expert who is knowledgeable about a variety of products and fit issues |
| unilateral vulvar enlargement can occur from biomechanics factors | therapists should evaluate vulvar area for size, swelling, and evidence of imbalances in the tissues from side to side, and evaluate bike fit and mechanics, encouraging women to create more symmetry of limb use |
| genital sensation is frequently affected in cyclists, indicating dysfunction in pudendal nerve | therapists should evaluate female cyclists for sensory or motor loss, establishing a baseline for re-evaluation |
Because women tend to be more comfortable in an upright position, the authors recommend that a recreational (more upright) versus a competitive (more aerodynamic and forward leaning) position may be helpful for women when appropriate. Although saddles with nose cut-outs and other adaptations such as gel padding in seats are discussed in the article, the authors caution against making any distinct recommendations due to the paucity of literature that is available. The paper concludes that more research is needed, and particularly for considering the varied populations of riders ranging from recreational to racing.
Within a pelvic rehabilitation setting, applying all orthopedic and specific pelvic rehabilitation skills is necessary for women cyclists who present with pelvic dysfunction. Because injury to the perineal area including the pudendal nerve can have negative impact on function such as bowel, bladder, or sexual health, skills in helping a patient heal from compressive or traumatic cycling injuries is very valuable. To learn more about pudendal nerve health and dysfunction, the Institute offers a 2-day course titled Pudendal Neuralgia Assessment, Treatment and Differentials: A Brain/Pain Approach. This course is offered next in Salt Lake City in April, so sign up soon!

An important survey completed in Australia asked if prenatal pelvic floor function and dysfunction relates to postnatal pelvic floor dysfunction (PFD). Interestingly, the authors propose that "…damage to the pelvic floor is probably made before first pregnancy due to congenital intrinsic weakness of pelvic floor structures." Many of the patients involved in the study had dysfunction in more than one domain of pelvic health, with the authors recommending a comprehensive approach to the evaluation of pelvic floor dysfunction.
As part of the large study called the Screening for Pregnancy Endpoints study, or SCOPE, a prospective cohort study called Prevalence and Predictors of Pelvic floor dysfunction in Prenips, or 4P, was also completed. The 4P research (n = 858) contained 2 different studies including a questionnaire-based survey and a detailed clinical assessment. The survey utilized the Australian pelvic floor questionnaire which was administered at 15 weeks gestation and at 1 year postpartum. The Australian questionnaire scores items on domains of urinary dysfunction, fecal dysfunction, pelvic organ prolapse, and sexual dysfunction. When the participants answered the questionnaire the first time, all answers were directed to be answered for symptoms they experienced prior to being pregnant.
The results indicated that at 1 year postpartum, 90% of the women in this study reported pelvic floor dysfunction. Regarding the domains of bladder, bowel, prolapse and sexual symptoms, 71% of the participants reported symptoms from more than 1 of these domains, 31% from 2 domains, 24% from 3 sections of the survey, and 8% from all four sections. Other interesting statistics are as follows:
-of the 73% of participants reporting urinary dysfunction, 67% had these symptoms persisting from the prenatal period
-pre-pregnancy urinary dysfunction symptoms persisted in postpartum in 61% of participants
-for new onset bowel symptoms in the postpartum period, fecal incontinence or obstructed defecation were more likely to occur, while incontinence of gas (flatus) was more likely to occur as persisting symptoms
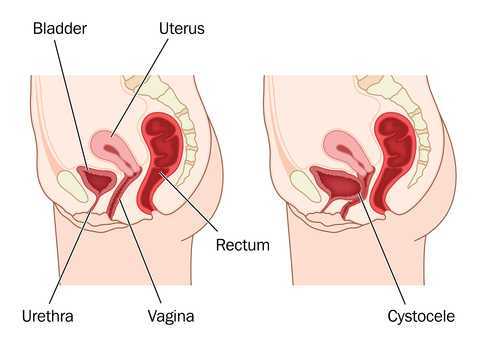
-prolapse symptoms were reported by 14% of women, with 20% of participants describing symptoms as severe and most common symptoms being vaginal pressure, heaviness, or a sensation of a lump being present
-symptoms of sexual dysfunction such as dyspareunia persisted postnatally in 59% and worsened in 12% compared to prenatal period
In women who delivered vaginally, the risk of pelvic floor dysfunction was increased, yet the authors caution against stating that c-sections are protective against pelvic floor dysfunction. They do theorize based on survey results that c-section may reduce the persisting PFD. Ideally, research such as this can help can assist in creating predictions for postpartum pelvic floor symptoms based on prenatal symptom history. Certainly it may be helpful to be aware of a patient's prenatal symptoms and include any new onset or persisting postpartum symptoms in her rehabilitation. If you are interested in learning more about pelvic floor dysfunction in pregnancy or postpartum, these topics are included in our Pregnancy and Postpartum course series that you can find on our main course page. The Care of the Pregnant Patient is happening in mid-March in Seattle, with a few seats still available! Care of the Postpartum Patient happens next in May in Boston. If you are interested in hosting Peripartum Special Topics, send us an email or give us a call!
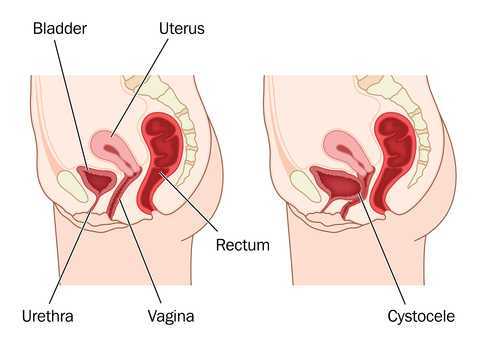
When considering rehabilitation of prolapse symptoms, therapists often implement an approach that addresses multiple factors related to pelvic health and function. Rehabilitation of prolapse symptoms may include bladder re-training, pelvic muscle strengthening, bowel health management, trunk and pelvic control strategies, avoidance of potential aggravating maneuvers such as bearing down, and education in management tools such as pessaries. As we have established in earlier posts in this 3-part series, each patient must be evaluated and treated with respect to her complaints and clinical findings. This post highlights a few of the many clinical research studies aimed at determining effectiveness of pelvic rehabilitation for prolapse symptoms.
In recent research, Hagen and colleagues completed a multi-center, randomized trial using parallel treatment groups to assess recovery from prolapse. Women with a stage I-III prolapse of any type confirmed by a physician using the POP-Q system and complaints of prolapse symptoms were the primary inclusion criteria. Women who had previously been treated by surgery for prolapse were excluded. The control group (n = 222) were given a prolapse lifestyle advice leaflet and no pelvic floor muscle training. The lifestyle advice included information about weight loss, constipation, avoidance of heavy lifting, coughing, and high-impact exercise. No information about pelvic floor muscle exercise was included.
The physiotherapy treatment group (n = 2250 received up to 5 individualized sessions of pelvic floor muscle training over 16 weeks. The first appointments were scheduled closer together to allow for proper training in muscle education, with the latter appointments being spread further apart. Rehabilitation began with instruction in pelvic muscle anatomy and function. Exercises were instructed based on results of a pelvic muscle assessment, and exercises were progressed with a goal of up to 10, 10-second holds, and up to 50 quick contractions completed three times per day. Women were also instructed in a pre-contraction of the pelvic floor muscles prior to increases in intra-abdominal pressure. (Electromyography, electrical stimulation, or pressure biofeedback were not allowed among the interventions.)
Outcomes tools included the pelvic organ prolapse symptom score (POP-SS) and several other tools to measure quality of life, level of bother from bowel and bladder symptoms, and a general health survey. Women in the physiotherapy treatment group reported more improvements in prolapse symptoms (POPP-SS). While degree of prolapse was also improved in the intervention group, the authors state that the differences were not significant when compared to the control group. Following are highlights from other research completed in prior years.
In this review of 5 randomized, controlled trials, Kari Bo describes the potential benefits demonstrated in the literature including improved pelvic organ prolapse (POP) stage, symptoms, and pelvic floor muscle morphology. The author summarizes that supervised and more intensive training is more effective than unsupervised training.
In this study the authors conducted 14 weeks of treatment with 7 clinic visits that included pelvic muscle awareness and proprioceptive training, education in home exercise program of strengthening.) Positive outcomes included improved anatomic measurements via POP-Q in anterior and posterior vaginal wall, and decreased prolapse symptoms. The intervention group demonstrated improved muscle strength, endurance, and surface EMG parameters. The study concluded that pelvic floor muscle training is effective in treating prolapse.
Compared with women in the control group, women in the pelvic floor muscle training group in this study demonstrated increased muscle thickness, decreased hiatal area, shortened muscle length, and elevated position of the bladder and rectum. Subjects also demonstrated decreased muscle length at maximum Valsalva, which the researchers indicated as a sign of increased muscle stiffness.
Following a 16 week physiotherapy program, women with stage I or II prolapse demonstrated significant improvement in stage of prolapse in this research. Women in the treatment group were more likely to report subjective improvement when compared to the control group.
The research indicates, although not consistently, that pelvic floor muscle training can improve the level of prolapse or descent in women with various types of prolapse. Many of the studies include not only pelvic muscle strengthening, but pelvic muscle awareness, protection, and training in functional activation to reduce the impact of straining when it does occur. Regardless of improvement in structural measures, women participating in pelvic muscle training consistently report decreased symptoms such as sense of heaviness when standing. In rehabilitation we are always concerned about function, level of bother, and quality of life of our patients. The bottom line appears to be that symptoms rule the day. We can tap into this fact by taking careful histories, by using outcomes tools, and by teaching our patients that over time they may benefit from continued rehabilitation efforts based on their home program. As with any home program, patients may benefit from a reevaluation and modification of a home program.
Although the research addressing perioperative pelvic rehabilitation is emerging, therapy in combination with surgical approaches may also help prepare women for successful management of prolapse symptoms. Evaluation and treatment of prolapse is instructed in the Institute's pelvic floor series, both in the Level 1 and in the Level 2B course. If you are interested in any series courses, please remember to plan ahead, as these courses fill up several months ahead of time! You can find all of our continuing education courses on the website by clicking here.