Ramona C. Horton MPT, DPT is a rock star in the realm of pelvic rehabilitation! What you may not know about Ramona is that she has developed and instructs the Herman & Wallace visceral and fascial mobilization courses.
Most therapists have a variety of manual therapy techniques in their toolbox. Manual therapy often targets muscles, joints, and bones and encompasses a broad range of techniques for treating musculoskeletal pain and dysfunction. While visceral mobilization is a specialized type of manual therapy that focuses on the internal organs and their surrounding tissues and fascial mobilization, also known as myofascial release, focuses on the fascia, the connective tissue that surrounds and connects muscles, organs, and bone.
Ramona's Mobilization course series includes four courses, three of which have upcoming course dates this year:
- Mobilization of the Myofascial Layer: Pelvis and Lower Extremity
- Future course dates for 2026 TBD
- Mobilization of the Visceral Fascia: The Gastrointestinal System
- June 27th-29th
- Mobilization of the Visceral Fascia: The Urinary System
- November 14th-16th
- Mobilization of the Visceral Fascia: The Reproductive System
- October 17th-19th
- Herman & Wallace works with clinics across the nation to make these courses accessable for you! This year, satellites are available in 16 different states across 7 regions. To find out more information and specific city and state locations, go to the Fascial Based Treatment for Pelvic Dysfunction - Home Page.
- Mid-Atlantic

- New Jersy
- New York
- Pennsylvania
- South East
- Florida
- Georgia
- Great Lakes
- Illinois
- Michigan
- Ohio
- Wisconsin
- Great Plains
- Nebraska
- South Central
- Louisiana
- Texas
- South West
- Arizona
- California
- Pacific Northwest
- Washington
- Oregon
-
All four of the mobilization courses all have the prerequisite of having previously attended Pelvic Function Level 1 or equivalent. In addition, the most advanced course, Mobilization of the Visceral Fascia: The Reproductive System, requires that you have previously taken Mobilization of the Visceral Fascia: The Urinary System.
-
-
Not sure if these are the courses for you? Check out Ramona's article in The Pelvic Rehab Report titled The Top 5 Reasons to Learn Fascial Mobilization to see if anything she shares resonates with you.
We look forward to seeing you in a course soon!

This blog includes portions of an interview with Ramona Horton. Ramona serves as the lead therapist for her clinic's pelvic dysfunction program in Medford, OR. Her practice focuses on patients with urological, gynecological, and colorectal issues. Ramona has completed advanced studies in manual therapy with an emphasis on spinal manipulation, and visceral and fascial mobilization. She developed and instructs her visceral and fascial mobilization courses for the Herman & Wallace Pelvic Rehabilitation Institute, and presents frequently at local, national, and international venues on topics relating to women’s health, pelvic floor dysfunction, and manual therapy.
How did you start in pelvic rehabilitation and visceral mobilization?
My PT training was through the Army-Baylor program, I was all in for orthopedics and sports medicine until October of 1990. I gave birth to my second child, an adorable, but behemoth, 9lb 9oz baby boy. His delivery, a VBAC (vaginal birth after cesarean) was very traumatic on my pelvis, I sustained pudendal nerve injury and muscular avulsion. When I queried the attending OB-GYN about my complete lack of bladder control his response and I quote “do a thousand Kegels a day, and when you’re 40 and want a hysterectomy, we’ll fix your bladder then.” As for the desire to study visceral mobilization, that reflects back to my PT training through the US Army which was 30 years ago, when the MPT was just getting started. It was an accelerated program, to say the least. We received a master's in physical therapy with 15 months of schooling. Given the very limited timeline, which included affiliations and thesis, the emphasis in our training was on critical thinking and problem solving, not memorization and protocols which in 1985 was not the norm. I can still hear the words of our instructors “You have to figure it out, I am not going to give you a cookbook."
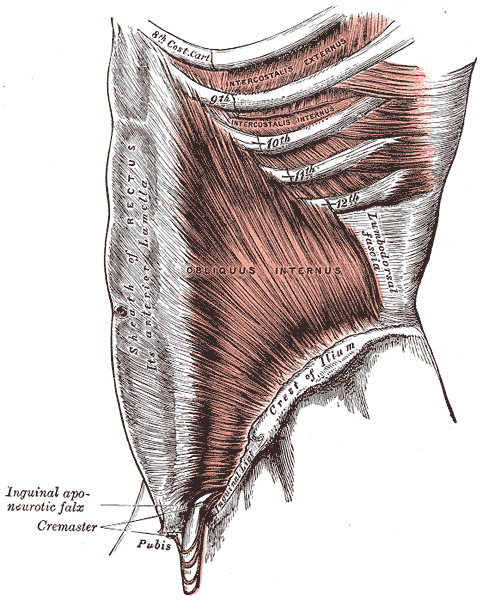
Following my initial training in the field of pelvic dysfunction in 1993 I started treating patients. I had a problem, I could not wrap my head around how I was to effectively treat bowel and bladder dysfunction…. without treating the bowel and bladder? I knew that there was more to this anatomy than just pelvic floor muscles and the abdominal wall, but at the time that is what was being treated. Once I started learning VM principles and applying the techniques to my patients I saw a vast improvement in my outcomes. I realized that the visceral fascia is a huge missing link in this field and that somewhere along the line the physical therapy community forgot one simple fact. We are not hollow; the visceral structures attach to the somatic frame through ligaments and connective tissue and have an influence on the biomechanics of said frame.
Why is the adoption of visceral mobilization so rare amongst practitioners who aren’t pelvic specialists?
Most likely several reasons, first they do not deal with dysfunctions that have visceral structures involved the way pelvic health therapists do. The second is a paucity of higher levels of evidence on the effectiveness of VM for musculoskeletal conditions. The third and most difficult issue to deal with is the broad-based claims that VM can be an effective treatment for issues ranging from acute trauma to emotional problems. One website called VM “bloodless surgery”. The problem simply is when anyone purports their technique to be a virtual panacea for all that ails mankind, without adequate evidence to back up the claims, the clinical world raises its collective antennae. These critical remarks are coming from a practitioner, published author, and educator in the VM field. The reality of evidence-based medicine is talk is cheap, research is not.
Why do you believe fascial mobilization is such an important aspect of clinical practice?
Most importantly because fascia is ubiquitous, it is EVERYWHERE throughout the body and it contains a vast neurological network to include nociceptors, mechanoreceptors, and proprioceptors just to name a few. The fascia was that stuff that we all dissected out of the way in anatomy lab so we could learn the assigned structures that soon would have a pin with a number stuck in it that we needed to know for a lab practical. We need to move beyond the “myofascia” and understand that the fascial system has multiple layers in the body starting at the panniculus which blends with the skin, the investing fascia surrounding muscles and forming septae, the visceral fascia which is by far the most complex and the deepest layer of fascia, the dura surrounding the central nervous system. All fascial structures, regardless of layer or location have their origin in the mesoderm of early embryologic development.
Ramona Horton's Fascial Mobilization Series 2022 Course Schedule
Mobilization of the Myofascial Layer: Pelvis and Lower Extremity Satellite Lab Course
Mobilization of Visceral Fascia: The Urinary System Satellite Lab Course
Mobilization of Visceral Fascia: The Gastrointestinal System Satellite Lab Course
September 30 - October 2, 2022
Mobilization of Visceral Fascia: The Reproductive System Satellite Lab Course
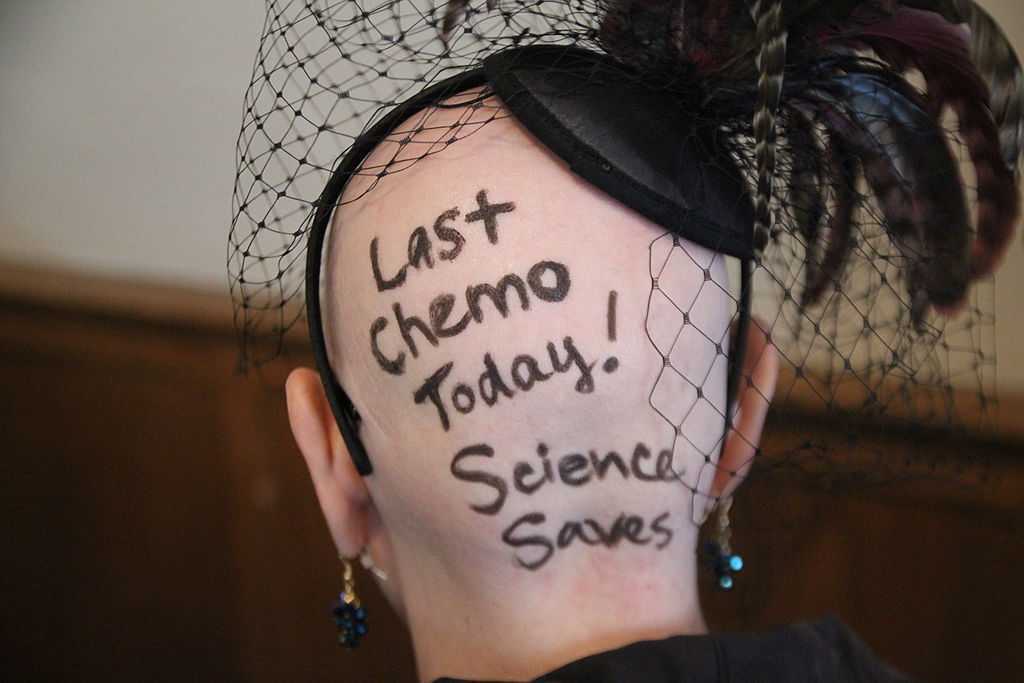
When a woman is given a cancer diagnosis, her entire world is turned upside down and inside out. There are so many things to think about; medical treatments, financial concerns, family concerns, and emotional upheaval. Sex may be the last thing that a woman may think about when she is actively going through treatment. However, at what rate are survivors having issues after treatment is complete?
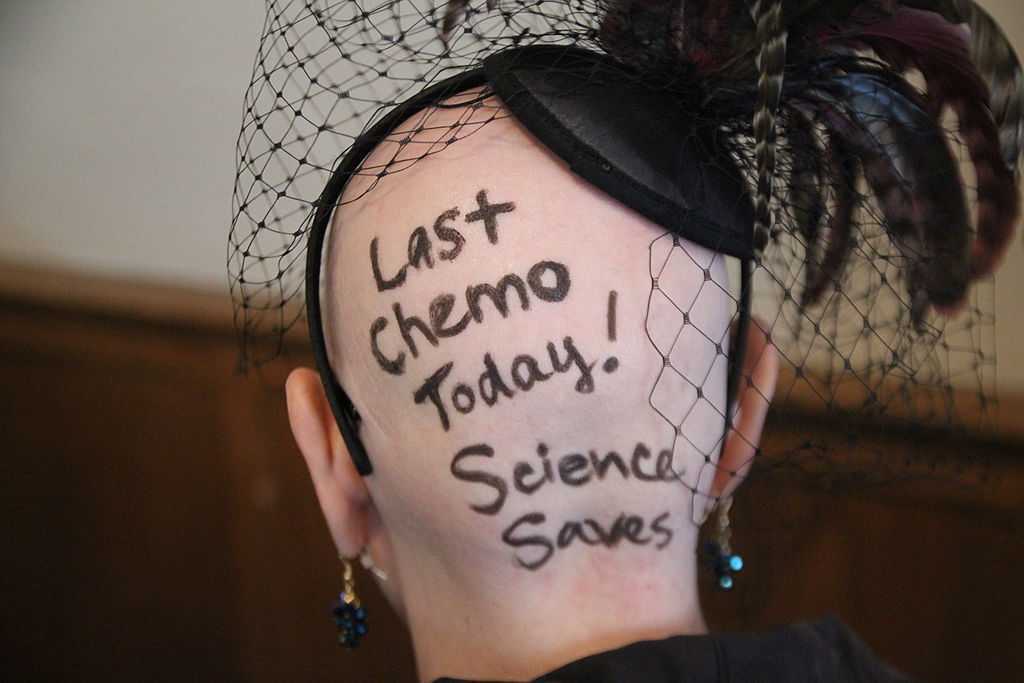 A recent study published in the journal Cancer looked at just this. A 2-year longitudinal study was performed that tracked young adults (18-39 years old) through and after their cancer diagnosis. The most common cancers seen in the samples were leukemia, breast cancer, soft-tissue sarcoma, and non-Hodgkin lymphoma. The patients completed the Medical Outcomes Study Sexual Functioning Scale at 4 months, 6 months, and 24 months after diagnosis. At 2 years after diagnosis over 50% of the patients surveyed reported some degree of sexual dysfunction. Women that were in a committed relationship had an increased likelihood for experiencing sexual dysfunction; while men had increased rate of reporting sexual issues regardless of their relationship status.
A recent study published in the journal Cancer looked at just this. A 2-year longitudinal study was performed that tracked young adults (18-39 years old) through and after their cancer diagnosis. The most common cancers seen in the samples were leukemia, breast cancer, soft-tissue sarcoma, and non-Hodgkin lymphoma. The patients completed the Medical Outcomes Study Sexual Functioning Scale at 4 months, 6 months, and 24 months after diagnosis. At 2 years after diagnosis over 50% of the patients surveyed reported some degree of sexual dysfunction. Women that were in a committed relationship had an increased likelihood for experiencing sexual dysfunction; while men had increased rate of reporting sexual issues regardless of their relationship status.
Women that undergo cancer treatment have several reasons that could be influencing their sexual function. Fatigue is a complaint that is often expressed by cancer patients. Their body image is often altered due to surgeries that have been performed. Chemotherapy and hormonal therapy often push women into menopause which then leads to vaginal dryness. Additionally, radiation and surgical treatment can lead to scar tissue, fibrosis, and stenosis of the vagina and pelvic floor muscles.
This is where physical therapy can help! In the Pelvic Floor Series Capstone course we teach advanced techniques that help treat pelvic floor issues by working on both the muscles, and the fascia. We also cover techniques that decrease the tenderness in the muscles that then allow you to stretch the muscle with less discomfort.
All of the techniques taught in Capstone are gentle but effective. The cancer survivor is the perfect population to use these gentle techniques on! Think of how rewarding our job will be when we help relieve the pain that may be associated with intercourse, and therefore improve intimacy of a cancer survivor with her partner!
Come join us for Capstone and learn techniques that will take your treatment skills to the next level!
Acquati, Zebrack, Faul, et al. Sexual functioning among young adult cancer patients: A 2-year longitudinal study. Cancer. 2018; 124(2): 398-405.
There has been a bit of buzz on the various news outlets and social media feeds about the “new organ” the interstitium. On March 27th an article appeared in Scientific Reports, an online peer-reviewed journal from the publishers of Nature. This work was presented by a team of researchers that utilized a new in vivo laser endomicroscopy technique that demonstrated this tissue is a matrix of collagen bundles and elastic fibers surrounded by fluid rather than the tightly packed layers of connective tissue that was previously observed on fixed slides . This submucosal layer was observed in the entire gastrointestinal tract, the urinary bladder, bronchus, dermis, bronchus and peri-arterial soft tissue and fascia. The authors state, “In sum, we describe the anatomy and histology of a previously unrecognized, though widespread, macroscopic, fluid-filled space within and between tissues, a novel expansion and specification of the concept of the human interstitium” Benias et al., 2018.
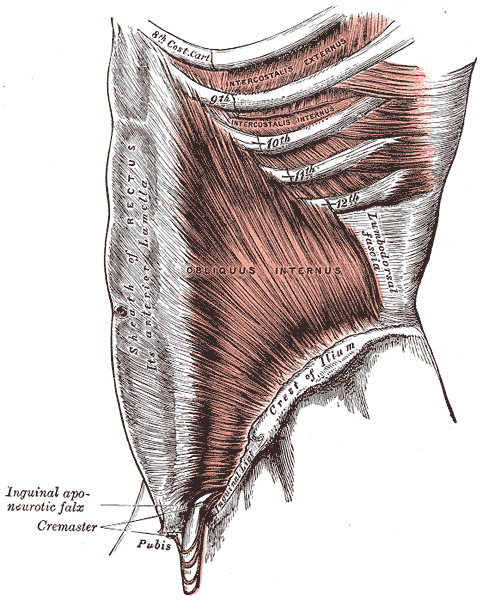 The only thing ‘new’ is the way that this group of scientists observed the tissue that until now has primarily been studied ex vivo. I find it rather humorous to note that it is mainstream news that histologists in the 21st century just realized that there is a difference in the architecture of living versus dead tissue. They noted a significant change in the appearance of tissue slides that were chemically fixed in the traditional manner when compared to studies of in vivo structures as well as fresh frozen samples. The researchers noted this tissue in the dermis as well as urinary system, gastrointestinal system and respiratory system. This further supports one of my favorite talking points presented in the visceral mobilization courses “fascia is fascia is fascia is fascia.”
The only thing ‘new’ is the way that this group of scientists observed the tissue that until now has primarily been studied ex vivo. I find it rather humorous to note that it is mainstream news that histologists in the 21st century just realized that there is a difference in the architecture of living versus dead tissue. They noted a significant change in the appearance of tissue slides that were chemically fixed in the traditional manner when compared to studies of in vivo structures as well as fresh frozen samples. The researchers noted this tissue in the dermis as well as urinary system, gastrointestinal system and respiratory system. This further supports one of my favorite talking points presented in the visceral mobilization courses “fascia is fascia is fascia is fascia.”
As an instructor that presents entire courses around the importance of the fascial system within all structures of the body including the dermis, epimysium, all organs, and the adventitia of vessels, I am thrilled to see this layer of the fascial system receive recognition and garner the attention it deserves. However, to refer to the interstitium as a new undiscovered organ is to ignore the work of the International Fascia Research Congress as well as many other notable scientists. These researchers see the fascial system as the dynamic mesenchymal tissue that unites every cell in the body and allows for fluid and tissue movement.
French hand surgeon Dr. Jean-Claude Guimrberteau has documented this tissue utilizing microendoscopy on living subjects for the past 20 years. Dr Guimberteau created a brilliant DVD called Strolling Under the Skin, you can view an excerpt available on YouTube. Following the success of several videos, he went on to co-author the book Architecture of Human Living Fascia: The extracellular matrix and cells revealed through endoscopy.
Another brilliant researcher is Orthopedic Surgeon Dr. Carla Stecco. Her paper The Fascia: the forgotten structure is an excellent review of the three-dimensional continuity of the myofascia. Following multiple publications, she also authored the book The Functional Atlas of the Human Fascial System. Her work is limited to the myofascial layer and does not include the visceral fascia although she notes its presence in her published works. For those that would like to know more about this tissue, I highly recommend both of these authors. If you wish to explore how a physical therapist can utilize this information in clinical practice, join me for one of my courses on fascial manipulation. The fascial based treatment for pelvic dysfunction series includes:
- Mobilization of the Myofascial Layer: Pelvis and Lower Extremity
- Mobilization of Visceral Fascia: The Gastrointestinal System
- Mobilization of Visceral Fascia: The Urinary System
- Mobilization of the Visceral Fascia: The Reproductive System of Men and Women
Benias, P. C., Wells, R. G., Sackey-Aboagye, B., Klavan, H., Reidy, J., Buonocore, D., ... & Theise, N. D. (2018). Structure and Distribution of an Unrecognized Interstitium in Human Tissues. Scientific Reports, 8(1), 4947. https://:doi.org/10.1038/s41598-018-23062-6, 2018.
Stecco, C., Macchi, V., Porzionato, A., Duparc, F., & De Caro, R. (2011). The fascia: the forgotten structure. Italian journal of anatomy and embryology, 116(3), 127.